Introduction
Hip arthroscopy is an effective method for
diagnosing and treating hip joint diseases. Its indications include
acetabular impingement, hip synovial chondromatosis, glenoid labrum
injury, cartilage injury, hip joint infection and hip pain of
unknown origin. Its contraindications are joint stiffness,
superficial infection and heterotopic ossification (1,2).
Furthermore, hip arthroscopy is a technically demanding procedure
and difficult for surgeons to learn due to the thick subcutaneous
fat layer and muscles surrounding the hip joint, the high level of
congruency between the acetabulum and femoral head, and the special
instruments required to perform the procedure. Conventional methods
require precise hip puncture and adequate penetration of the
capsule, which is relatively difficult to perform due to direct
access to the central compartment being hindered by the
ball-and-socket morphology of the joint. Therefore, the risk of
chondral scuffing and labral penetration is high. During hip
arthroscopy, the operating space is available for the surgical
manipulations is insufficient, which may lead to inadequate
treatment of the lesions (3).
Arthroscopic capsulotomy may be utilized to expose
lesions in the hip joint and two methods are available to perform
this (4). One is the commonly used
interportal capsulotomy, in which the capsule is cut between the
two portals. The length of the interportal capsulotomy varies
depending on the individual surgeon's personal preference (5). Using this method, most lesions in the
central compartment may be sufficiently exposed, while the exposure
of lesions which lie distal to the femoral head is poor. The other
method is T-shaped capsulotomy, which was first described by
Horisberger et al (6) in
2009. This method comprises the generation of a space outside of
the capsule, followed by a T-shaped capsulotomy along the
iliofemoral ligament perpendicular to the intertrochanteric line.
This is often referred to as an ‘outside-to-inside’ technique,
which may provide adequate exposure to visualize the peripheral
compartment, as well as increased room for instrument
maneuverability. Compared with other joint puncture techniques, the
ability to perform this technique may be easily acquired by most
surgeons to achieve a satisfactory exposure and outcome. Certain
improvements to the method described by Horisberger et al
(6) were made, including suturing
the capsule and implementing different capsular management
strategies (4,7). The present study aimed to describe and
evaluate this technique.
Patients and methods
Patient selection
All patients who underwent hip arthroscopy at the
Third Affiliated Hospital of Sun Yat-sen University (Guangzhou,
China) between February 2012 and February 2016 were considered
eligible for the study and were retrospectively analyzed, excluding
those with infective hip arthritis. A total of 32 patients (18
cases with the left hip and 14 cases with the right hip affected),
including 19 males and 13 females, aged between 19 and 48 years
with a median age of 36, were included in the present study. The
cohort comprised 15 cases of hip synovitis, 9 cases of hip
impingement syndrome and 8 cases of hip joint synovial
chondromatosis.
Pre-operative bilateral anteroposterior hip X-ray
(AP view), frog leg view and Lequesne false profile X-ray images
were captured (8,9). Computed tomography of the hip joint was
also performed to analyze the morphology of the femoral head and
the acetabulum. Patients who were suspected of having labrum or
cartilage damage underwent magnetic resonance imaging (MRI)
examination.
Surgical technique: Extracapsular
arthroscopic approach
Standard equipment, including specific cannula,
shavers, a radiofrequency probe, 30 and 70° viewing arthroscope
(Smith & Nephew plc, London, UK), a C-arm fluoroscope and a
traction table were prepared. The patients were placed in the
supine position on the orthopaedic traction bed with the operating
leg immobilized at 20° hip flexion. The other, unaffected leg was
fixed with a leg holder and kept away from the operation field. A
well-padded bolster was placed under the perineum to prevent injury
to the genitalia and pudendal nerve.
The great trochanter and the anterior superior iliac
spine were marked with a sterile pen. The anterolateral portal
(ALP) was placed 1-2 cm proximal to the tip of the greater
trochanter and the AP view by C-arm was used to monitor the
arthroscope (blunt trocar) to reach the extracapsular position of
the femoral head-neck junction, just outside of the hip capsule
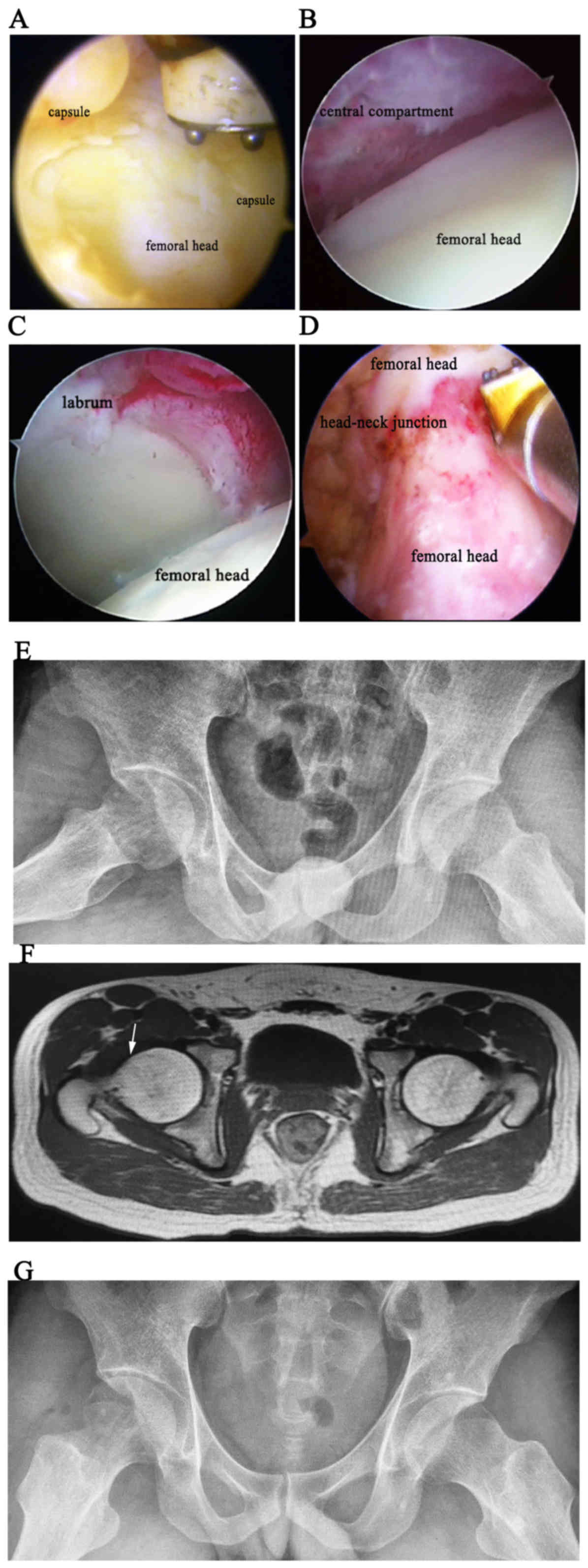
(Fig. 1). The distal anterolateral
accessory portal was set up ventrally and distal to the anterior
border of the trochanter. The blunt trocar was inserted into the
femoral head-neck junction under AP view. Subsequently, the
radiofrequency probe or shaver was placed into the femoral
head-neck junction through the trocar (Fig. 2). The adipose tissues between the
iliocapsularis tendon medially and the gluteus minimus tendon
laterally were removed under direct arthroscopic visualization and
the white capsular fibers were identified. The midanterior portal
was established if required. Capsulotomy was performed along the
fiber direction of the iliofemoral ligament. Partial cleaning of
the joint capsule near the acetabulum was performed. Probe hook may
also be used to improve the exposure by pushing joint capsules to
both sides. If more exposure was required, the medial or the
lateral limbs of the capsulotomy were retracted by pulling the
sutures placed on the section limbs. In patients who required
labrum repair or femoral head molding, a transverse cut along the
acetabular rim was performed. The capsulotomy was performed
parallel to the femoral neck to the labrum, and limited proximal to
the zona orbicularis to avoid injury to the terminal branch of the
lateral femoral circumflex artery (Fig.
3).
On a standard traction table, lower limb traction
was applied to facilitate the insertion of the arthroscope into the
central compartment. The acetabular labrum was located by
identifying the reflex portion of the rectus femoris muscle that
was visible on arthroscopy. Subsequently, diagnostic visualization
and treatment of any pathology in the central compartment was
performed. Following procedures including removal of synovial loose
bodies, debridement of delaminated cartilage, hip synovial biopsy
(Fig. 4) and repair of the labrum,
the traction was removed after the procedures in the central
compartments were completed so as to reduce injury to the nerve.
The arthroscope was then moved to the peripheral compartment of the
hip and the synovium was cleaned to observe the head-neck junction.
For cam-type femoroacetabular impingement patients, the bump of the
cam lesion was resected under the C-arm to achieve an
impingement-free range of movement (Fig.
5). This was performed carefully to prevent femur neck fracture
and injury to the ascending branch of the circumflex femoral
artery, which supplies blood to the femoral head.
In addition, excessive joint capsulotomy was avoided
and the capsule was not routinely sutured. However, for certain
patients with pre-operative anterior instability, ligamentous
laxity or acetabular dysplasia, a midanterior portal was
established. The hip was flexed to 30° and a sharp tissue
penetrating suture grasper (BirdBeak; Arthrex GmbH, Munich,
Germany) and Suture Lasso (Smith & Nephew plc) were used. The
Suture Lasso was used to pierce the proximal side of the
capsulotomy and a looped No. 2 nylon suture lasso was then shuttled
through the tissue. The grasper was used to retrieve the nylon
lasso through the distal side of the capsulotomy. A further No. 2
suture was shuttled into the lasso and pulled out. Finally, both
capsular limbs were sutured to achieve a side-to-side stitch, with
the knot tied outside of the capsule, to perform the capsule
closure (10). While Horisberger
et al (6) did not surture the
capsule.
Post-operative rehabilitation
Patients were routinely prescribed oral indomethacin
for prophylaxis of heterotopic ossification for 4 weeks. Those who
received femoroplasty were ambulated with crutches for 4 weeks as a
precautionary measure to prevent fracture of the femoroplasty site.
However, patients diagnosed with synovial chondromatosis and hip
synovitis were allowed immediate weight bearing post-operatively.
After 12 weeks, patients resumed their daily activities, and
gradually took up low-impact physical exercise, including jogging
and climbing stairs. After 6 months, the patients were allowed to
gradually return to sports (11–13).
Pre-operation and at the last follow-up activity and
functional levels were recorded using the modified Harris hip score
(MHHS) and The Visual Analogue Scale (VAS). MHHS is widely used to
assess the outcomes of hip arthroscopic procedures (14–17).
Patients were followed-up with telephone interviews. The details of
MHHS are listed in Table I. Unlike
the Harris hip score, the range of motion and absence of deformity
were not included in the MHHS. In addition, the VAS is a system
that measures the intensity of pain.
 | Table I.Modified-Harris hip scoring
system. |
Table I.
Modified-Harris hip scoring
system.
| Parameter | Points |
|---|
| I. Pain | 44 |
| None | 44 |
| Slight or
occasional, no activity compromise | 40 |
| Mild, no
effect on average activity, may take | 30 |
|
non-steroidal
anti-inflammatory agent |
|
| Moderate,
some average activity limitation, | 20 |
|
occasional narcotic use |
|
| Marked,
serious activity limitations | 10 |
| Totally
disabled, bedridden | 0 |
| II. Function | 47 |
| A.
Gait | 33 |
|
Walk with
limp |
|
|
None | 11 |
|
Slight | 8 |
|
Moderate | 5 |
|
Severe | 0 |
|
Support |
|
|
None | 11 |
|
Cane used for long
walks | 7 |
|
Cane used most of
the time | 5 |
|
One crutch | 3 |
|
Two canes | 2 |
|
Two crutches | 1 |
|
Not able to
walk | 0 |
|
Walking
distance |
|
|
>1 km | 11 |
|
500 m-1 km | 8 |
|
100-500 m | 5 |
|
Only inside the
house | 2 |
|
Confined to chair
or bed | 0 |
| B.
Activities | 14 |
|
Stair
climbing |
|
|
Normal, without
use of banister | 4 |
|
Normal, with use
of banister | 2 |
|
Stairs in any
manner | 1 |
|
Unable to climb
stairs | 0 |
|
Ability to put on
shoes and socks |
|
|
With ease | 4 |
|
With
difficulty | 2 |
|
Unable | 0 |
|
Ability to
sit |
|
|
Comfortably in
ordinary chair for 1 h | 5 |
|
On high chair for
half an hour | 3 |
|
Unable to sit for
half an hour in any chair | 0 |
|
Public
transport |
|
|
Able to enter
public transportion | 1 |
|
Unable to use
public transportation | 0 |
Statistical analysis
Statistical analysis was performed using SPSS 21.0
(IBM Corp., Armonk, NY, USA). MHHS and VAS score were expressed as
the mean ± standard deviation, and compared using a wilcoxon signed
rank test. P<0.05 was considered to indicate a statistically
significant difference.
Results
Complications
No complications including joint infection, perineal
skin compression, heterotopic ossification or injury of the lateral
femoral cutaneous nerve, sciatic nerve or pudendral nerve were
observed peri-operatively.
MHHS and VAS results
The follow-up duration was 18-32 months, with a mean
of 22.4±2.2 months. Of the total cohort, 31 patients were available
for follow-up, while 1 patient was lost to follow-up. MHHS was
66.2±6.0 and the Visual Analogue Score (VAS) was 6.5±1.1. At the
end of the follow-up period, the MHHS was 82.6±5.2 and the VAS was
1.2±0.7. While the modified Harris score was significantly
increased compared with the pre-operative score (P<0.05), the
VAS score at the end of the follow-up was significantly lower than
that at the pre-operative stage (P<0.05; Table II).
 | Table II.Comparison between pre- and
post-arthroscopy using MHHS and VAS. |
Table II.
Comparison between pre- and
post-arthroscopy using MHHS and VAS.
|
| Total cases | Pre-operative
score | Post-operative
score | P-value |
|---|
| VAS | 31 |
6.5±1.1 |
1.2±0.7 | P<0.05 |
| MHHS | 31 | 66.2±6.0 | 82.6±5.2 | P<0.05 |
Discussion
Anatomically, the hip capsule is reinforced by the
iliofemoral, pubofemoral and ischiofemoral ligament. The
iliofemoral ligament, which tightens with hip extension, is the
most important and strongest ligament in the hip. It is divided
into two branches and forms an inverted Y-shape anteriorly, and the
flat plane in front of the two branches separates the
iliocapsularis muscle and the gluteus minimus. The pubofemoral
ligament is on the medial and inferior side of the hip joint, and
the ischiofemoral ligament is on the posterior side (18). The hip joint may be divided into a
central compartment and a peripheral compartment. By identification
of the reflex portion of the rectus femoris muscle, the location of
the acetabular labrum may be determined. The insertion of the
rectus femoris on the pelvis starts from the upper edge of the
acetabulum at the 12 o'clock position, and the blood supply to the
femoral head is mainly from the medial femoral circumflex artery,
which arises near the base of the femoral neck, so that partial
capsulotomy is less likely to affect the blood supply of the
femoral head.
In the conventional method, due to the prominent
anterior acetabular wall and the tough capsule surroundings,
sufficient lower limb traction must be applied first to enlarge the
joint space. The surgeon may then use a needle to puncture the
central compartment under fluoroscopic guidance. Anitinol guide
wire is passed into the joint through the needle and metal tubes of
different diameters are consecutively placed to expand the tunnel.
Following this, the arthroscopic tube may be inserted into the
joint via the expanded tunnel. An interportal capsulotomy may be
used to enlarge the area for operation. Finally, the arthroscope
and a shaver may be placed into the joint. A major drawback of this
technique is that it may be difficult to perform for less
experienced surgeons. Furthermore, repeated puncturing may lead to
articular cartilage or labrum injury, as well as prolonged
operation and traction time. Prolongation of the traction time may
also lead to nerve injury and continued pressure between the
perineum column and the skin may cause skin compression (19). In addition, certain lesions lying
distal to the femoral head may not be sufficiently visualized due
to the overlying capsule and the relatively narrow operative area.
Due to the combination of these factors, treatment using the
conventional method may be insufficient, resulting in residual
deformity and patient dissatisfaction regarding the outcome.
Arthroscopic partial capsulotomy is an ‘outside to
inside’ method, which differs from the conventional puncture
method. Initially, the surgeon follows a Hueter approach at the
front of the joint, and once the partial capsulotomy has been
performed, the arthroscope may be inserted into the central
compartment from the outside to the inside under traction.
This method was first described by Horisberger et
al (6), and in the present
study, certain modifications have been applied. First, no adrenalin
solution was used to expand the joint capsule. In the beginning,
punctures were made directly outside the capsule. However, needle
puncture into the joint capsule is not necessary. By avoiding
repeated joint puncture, the operative duration may be reduced;
furthermore, the chances of labrum damage are reduced if performed
by a less experienced or unskillful surgeon. Furthermore, the
transverse cut along the acetabular rim is rarely required, as
partial cleaning of the joint capsule near the acetabulum is
usually performed at our department. By putting a probe hook to
push the section limbs of the capsule or pulling the sutures placed
on the section limbs of the capsule and passive rotation and
distraction of the lower limb, superior exposure was achieved in
most cases of the present study. This presents a difference from
the method described by Horisberger et al (6), which relied on the Wissinger rod or
Hohmann retractor over the proximal anterolateral portal. In
addition, the T-shaped cut was performed only in patients who
required labrum repair or femoral head-neck molding.
In addition, Horisberger et al (6) reported that, out of a total of 105
hips, dysesthesia/hypesthesia of the pudendal and lateral cutaneous
femoral nerves occurred in 9 cases. In the present study, not a
single case of lateral cutaneous nerve complications was
encountered. Injury to this nerve, which lies just below the
inguinal ligament and in front of the Sartorius and tensor fascia
latae (20), may occur during portal
establishment. In order to reduce the risk of nerve injury in the
present study, following the incision of the skin, the vascular
forceps were used to carefully separate the subcutaneous tissue,
and the trocar was then slowly inserted. Finally, Horisberger et
al (6) did not report whether
the capsule was repaired after capsulotomy. In the present study,
those patients with pre-operative anterior instability, ligamentous
laxity or acetabular dysplasia, the joint capsule was repaired with
absorbable sutures.
The partial capsulotomy used in the present study
has several advantages. One major benefit is that it prevents
possible iatrogenic cartilage and labrum damage from repeated
puncturing of the capsule, as all of the manipulations are
completed under direct visualization. This may also save time if
the operation is performed by a surgeon who is less experienced in
hip surgery. Only when partial capsulotomy is performed, the
surgeon may easily enter the joint, has a wider operative space and
improved visualization of the lesion, and is able to conveniently
fix the bone deformity. Furthermore, the traction time and strength
may be reduced, as it is only used after placing the portals and
performing the capsulotomy. Thus, the risk of sciatic or pudendal
nerve injury is reduced.
In addition, partial capsulotomy does not require
any special surgical instruments, including the hollow metal tube
or nitinol guide wire. The puncture method is also relatively
simple, and learning surgeons may quickly master this method.
Thaunat et al (21) regarded
capsulotomy as a simple and easy technique to master, which may be
performed using a 30° optic system, with the possibility of
reduction in the force and duration of traction, and with a lesser
risk of labral or chondral damage.
A shortcoming is that arthroscopic partial
capsulotomy inevitably causes damage to the ligaments of the hip
joint and part of the joint capsule. Indiscriminate capsulotomy
should also be avoided in case of iatrogenic hip pain and
instability after arthroscopy, particularly in patients with
potential joint laxity and developmental hip dysplasia (22). It is controversial whether the
capsule should be repaired after capsulotomy. Domb et al
(23) performed a systematic review
of ~4,000 cases of hip arthroscopic surgeries that used various
degrees of capsule resection treatment of femoroacetabular
impingement without patching or overlapping and identified no case
of iatrogenic instability. Strickland et al (24) reported that repaired and unrepaired
capsulotomy sites progressed to healing with a continuous
appearance on MRI by 24 weeks post-operatively. Dippmann et
al (25) performed a multicenter
study to compare capsular closure with non-capsular closure during
hip arthroscopy in Danish patients with femoroacetabular
impingement, and concluded that whether the hip capsule should be
closed during hip arthroscopy or not should be decided based on the
biomechanical pre-conditions of the patients.
No general consensus has been reached regarding
whether the capsule must be repaired, but undoubtedly, excessive
joint capsulotomy should be avoided. According to our experience,
which is based on individual situations with specific patients,
capsular repair may be recommended for patients with pre-operative
anterior instability, capsular hyperlaxity or hip development
dysplasia. An anatomic side-to-side repair of the capsule from the
distal to the proximal end may restore the native tension and
anatomy of the iliofemoral ligament. However, for certain patients
with adhesive capsulitis or limited external rotation prior to
surgery, capsular repair may not be necessary.
In addition, injury to the circumflexae femoris
lateralis artery may be avoided by paying full attention while
removing the adipose tissues between the gluteus minus laterally
and the iliocapsular medially. Excessive resection during
osteochondroplasty should also be avoided to prevent femoral neck
fractures (26).
Of note, the present study had several limitations.
The number of cases included in the study were limited.
Furthermore, the present study assessed only one treatment group,
without an additional treatment group for comparison. The VAS/MHHS
score were also not assessed at the same time-point for all
patients. Future studies should therefore address these issues and
include additional outcomes for patient characteristics and
clinicopathological data.
In conclusion, the arthroscopic partial capsulotomy
technique presented in the present study provides an alternative
option for exposure and treatment of hip joint disease. This method
yielded satisfactory clinical outcomes and without any significant
complications, and is easy to master for surgeons with limited
experience in hip arthroscopy.
Acknowledgements
Not applicable.
Funding
The present study was financially supported by the
Guangdong Medical Science and Technology Research Fund (grant no.
A2016066), the Guangdong Traditional Chinese Medicine Bureau
Research Fund (grant no. 20181061) and the Guangdong Medial
Scientific Research Fund (grant no. A2015115).
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
ZZ and DS conceived the study. ZZ performed the
literature search and wrote the manuscript. YC contributed to the
interpretation of data and review of the manuscript. KC contributed
to the analysis and interpretation of data, as well as language
editing. RH and TL collected and assembled the data. All authors
have read and approved the final manuscript.
Ethics approval and consent to
participate
Not required due to the retrospective nature of the
study.
Patient consent for publication
Patients have provided consent for publication.
Competing interests
The authors declare that they have no competing
interests
References
|
1
|
McCarthy JC and Lee JA: Hip arthroscopy:
Indications, outcomes, and complications. Instr Course Lect.
55:301–308. 2006.PubMed/NCBI
|
|
2
|
Sampson TG: Complications of hip
arthroscopy. Clin Sports Med. 20:831–835. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Mehta N, Chamberlin P, Marx RG, Hidaka C,
Ge Y, Nawabi DH and Lyman S: Defining the learning curve for hip
arthroscopy: A threshold analysis of the volume-outcomes
relationship. Am J Sports Med. 46:1284–1293. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Ekhtiari S, de Sa D, Haldane CE, Simunovic
N, Larson CM, Safran MR and Ayeni OR: Hip arthroscopic capsulotomy
techniques and capsular management strategies: A systematic review.
Knee Surg Sports Traumatol Arthrosc. 25:9–23. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Bedi A, Galano G, Walsh C and Kelly BT:
Capsular management during hip arthroscopy: From femoroacetabular
impingement to instability. Arthroscopy. 27:1720–1731. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Horisberger M, Brunner A and Herzog RF:
Arthroscopic treatment of femoroacetabular impingement of the hip:
A new technique to access the joint. Clin Orthop Relat Res.
468:182–190. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Forster-Horvath C, Domb BG, Ashberg L and
Herzog RF: A method for capsular management and avoidance of
iatrogenic instability: Minimally invasive capsulotomy in hip
arthroscopy. Arthrosc Tech. 6:e397–e400. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Clohisy JC, Carlisle JC, Beaulé PE, Kim
YJ, Trousdale RT, Sierra RJ, Leunig M, Schoenecker PL and Millis
MB: A systematic approach to the plain radiographic evaluation of
the young adult hip. J Bone Joint Surg Am. 90 Supp 4:47–66. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Hellman MD, Mascarenhas R, Gupta A,
Fillingham Y, Haughom BD, Salata MJ and Nho SJ: The false-profile
view may be used to identify cam morphology. Arthroscopy.
31:1728–1732. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Camp CL, Reardon PJ, Levy BA and Krych AJ:
A simple technique for capsular repair after hip arthroscopy.
Arthrosc Tech. 4:e737–e740. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Grzybowski JS, Malloy P, Stegemann C,
Bush-Joseph C, Harris JD and Nho SJ: Rehabilitation following hip
arthroscopy-a systematic review. Front Surg. 2:212015. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Enseki KR and Kohlrieser D: Rehabilitation
following hip arthroscopy: An evolving process. Int J Sports Phys
Ther. 9:765–773. 2014.PubMed/NCBI
|
|
13
|
Rath E, Sharfman ZT, Paret M, Amar E,
Drexler M and Bonin N: Hip arthroscopy protocol: Expert opinions on
post-operative weight bearing and return to sports guidelines. J
Hip Preserv Surg. 4:60–66. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Lavini F, Renzi-Brivio L, Aulisa R,
Cherubino F, Di Seglio PL, Galante N, Leonardi W and Manca M: The
treatment of stable and unstable proximal femoral fractures with a
new trochanteric nail: Results of a multicentre study with the
Veronail. Strategies Trauma Limb Reconstr. 3:15–22. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Harris WH: Traumatic arthritis of the hip
after dislocation and acetabular fractures: Treatment by
moldarthroplasty. An end-result study using a new method of result
evaluation. J Bone Joint Surg Am. 51:737–755. 1969. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Byrd JW and Jones KS: Prospective analysis
of hip arthroscopy with 2-year follow-up. Arthroscopy. 16:578–587.
2000. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Hung M, Hon SD, Cheng C, Franklin JD, Aoki
SK, Anderson MB, Kapron AL, Peters CL and Pelt CE: Psychometric
evaluation of the lower extremity computerized adaptive test, the
modified harris hip score, and the hip outcome score. Orthop J
Sports Med. 2:23259671145621912014. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Martin HD, Savage A, Braly BA, Palmer IJ,
Beall DP and Kelly B: The function of the hip capsular ligaments: A
quantitative report. Arthroscopy. 24:188–195. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Nakano N, Lisenda L, Jones TL, Loveday DT
and Khanduja V: Complications following arthroscopic surgery of the
hip: A systematic review of 36 761 cases. Bone Joint J.
99-B:1–1583. 2017. View Article : Google Scholar
|
|
20
|
Tomaszewski KA, Popieluszko P, Henry BM,
Roy J, Sanna B, Kijek MR and Walocha JA: The surgical anatomy of
the lateral femoral cutaneous nerve in the inguinal region: A
meta-analysis. Hernia. 20:649–657. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Thaunat M, Murphy CG, Chatellard R,
Sonnery-Cottet B, Graveleau N, Meyer A and Laude F: Capsulotomy
first: A novel concept for hip arthroscopy. Arthrosc Tech.
3:e599–e603. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Ranawat AS, McClincy M and Sekiya JK:
Anterior dislocation of the hip after arthroscopy in a patient with
capsular laxity of the hip. A case report. J Bone Joint Surg Am.
91:192–197. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Domb BG, Philippon MJ and Giordano BD:
Arthroscopic capsulotomy, capsular repair, and capsular plication
of the hip: Relation to atraumatic instability. Arthroscopy.
29:162–173. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Strickland CD, Kraeutler MJ, Brick MJ,
Garabekyan T, Woon JTK, Chadayammuri V and Mei-Dan O: MRI
evaluation of repaired versus unrepaired interportal capsulotomy in
simultaneous bilateral hip arthroscopy: A double-blind, randomized
controlled trial. J Bone Joint Surg Am. 100:91–98. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Dippmann C, Kraemer O, Lund B, Krogsgaard
M, Holmich P, Lind M, Briggs K, Philippon M and Mygind-Klavsen B:
Multicentre study on capsular closure versus non-capsular closure
during hip arthroscopy in Danish patients with femoroacetabular
impingement (FAI): Protocol for a randomised controlled trial. BMJ
Open. 8:e0191762018.PubMed/NCBI
|
|
26
|
Horner NS, Vikas K, MacDonald AE, Naendrup
JH, Simunovic N and Ayeni OR: Femoral neck fractures as a
complication of hip arthroscopy: A systematic review. J Hip Preserv
Surg. 4:9–17. 2017.PubMed/NCBI
|