Introduction
The treatment of urethral reconstruction has changed
considerably in recent decades. Although dilatation, internal
urethrotomy and end-to-end anastomosis of urethral margins are the
most widely used treatments, the choice of which to select should
be patient-centered (1).
Furthermore, these approaches are not recommended in long and
complex segments of urethral stricture due to a high rate of
failure (1). In recent decades, free
grafts including free skin (penile, scrotal, extragenital) flap,
bladder mucosa, oral (buccal and lingual) mucosa and colonic
mucosa, have been successfully applied to urethroplasty (2). Of these, oral mucosa graft is
considered to be an ideal substitute for the urethra, with high
success rates because of its characteristics of resistance to
infection and compatibility with a wet environment (3). Although oral mucosa grafts are now
widely applied in urethroplasty (2),
they are associated with certain early and late postoperative
complications, including oral pain, mouth tightness, speech and
chewing difficulties, altered sensation and reduced tongue
protrusion. Certain patients are unsuitable for undergoing
urethroplasty with oral mucosa graft due to difficulties with
harvesting sufficient oral mucosa (2,3).
Therefore, alternative grafts are important. Since bladder mucosa
was first used for urethra reconstruction by Memmelaar in 1947
(4), it has been demonstrated to be
feasible and safe in urethral reconstruction in several cases
(4–7). Therefore, bladder mucosa represents
alternative graft material in certain patients who are not
candidates for performing oral mucosa graft harvest.
To harvest bladder mucosa graft, patients undergo
conventional open surgery, which may be followed by numerous
complications (6,7). In the current study, a novel, minimally
invasive method is reported that has been applied to harvest
bladder mucosa graft though an endoscopic technique assisted by
water-jet. The safety, feasibility and efficacy of this approach
are discussed.
Patients and methods
Case data
Case 1 was a 35-year-old male patient with a
complaint of dysuria for 3 years. The patient was admitted to the
Department of Urology, Tongji Hospital (Wuhan, China) in April
2017. He had a history of straddle injury 3 years previously, and
had undergone internal urethrotomy twice and numerous instances of
urethral dilatation for the injury. Urethrography suggested that a
bulbar urethral stricture was present (Fig. 1A). At first, lingual mucosa was
recommended for urethral reconstruction. However, the patient
rejected this treatment once he understood the advantages and
disadvantages associated with urethral reconstruction with oral
mucosa. Eventually, urethral reconstruction with bladder mucosa
graft harvested via endoscopic sub-mucosal dissection assisted by
water-jet was adopted.
Case 2 was a 22-year-old male patient who had
suffered from dysuria for 1 year, in the absence of fever or
discomfort of the waist and abdomen. The patient was admitted to
the Department of Urology, Tongji Hospital (Wuhan, China) in May
2017. He had undergone urethroplasty surgery for hypospadias in
2001 and 2008. Physical examination indicated that the urethral
orifice was located at the middle of the penis (Fig. 1B). Preoperative cystography indicated
a segment of urethral stricture of ~1.5 cm (Fig. 1C). There was no residual urine under
bladder ultrasonography (Table
I).
 | Table I.Clinical and surgical
characteristics. |
Table I.
Clinical and surgical
characteristics.
| A, Clinical
characteristics |
|---|
|
|---|
| Characteristic | Patient 1 | Patient 2 |
|---|
| Age (years) | 35 | 22 |
| Sex | Male | Male |
| BMI
(kg/m2) | 22.0 | 23.9 |
| Medical history | Straddle injury;
internal urethrotomy twice and numerous instances of urethral
dilatation | Hypospadias; two
urethroplasty surgeries for hypospadias |
| Lesion location | Bulbous urethra | Penile urethra |
| Length of stricture
(cm) | 2.0 | 1.5 |
| Urethral orifice | Normal | Scrotum |
|
| B, Surgical
characteristics |
|
|
Characteristic | Patient 1 | Patient 2 |
|
| Stage of
urethroplasty | One-stage
approach | Two-stage
approach |
| Onlay of free bladder
mucosal | Dorsal onlay | – |
| Operative time
(min) | 167 | 156 |
| Operative time of
bladder mucosal harvest (min) | 35 | 30 |
| Blood loss (ml) | 120 | 100 |
| Severe
complications | No | No |
The two patients provided written, informed consent
for their inclusion in the current study.
Bladder mucosa graft harvest
The patients received ultrasonography and cystoscopy
to exclude urinary system diseases, including inflammatory and
neoplasm conditions, which would preclude harvest bladder mucosa
grafts. Routine urine examination, as well as urine culture, was
also necessary to determine whether urinary tract infection was
present.
The patient received general anesthesia and was
placed in the lithotomy position. The stricture was searched under
the guidance of catheter. The skin, the perineal superficial and
deep fascia and the corpus spongiosum were dissected layer by
layer. Before bladder mucosa was harvested, the length of the
stricture segment or position of hypospadias was measured, and then
the endoscope was placed into the bladder from the normal urethra
under direct vision (Fig. 2).
Subsequently, the surgical procedure of endoscopic sub-mucosal
dissection was performed using the water-jet hybrid knife system
(8) (I-Type; diameter, 2.3 mm;
length 1.9 m; Erbe China Ltd., Shanghai, China; Fig. 3).
The detailed endoscopic surgical procedure (Fig. 4) was as follows: Boundaries of
resection were marked by a series of electrical coagulation points;
a sub-mucosal ‘water pad’ was formed by the high-pressure water
column penetrating the mucous layer and gathering under the mucous
membrane to separate the mucosa and muscle layer; the mucosa
membrane was dissected along the edge of the marker points; active
bleeding was stopped via electrocoagulation and the bladder mucosa
graft was obtained.
Urethral reconstruction technique
The bladder mucosa graft was soaked in normal saline
at room temperature for 20 min prior to use. The thicker mucosa was
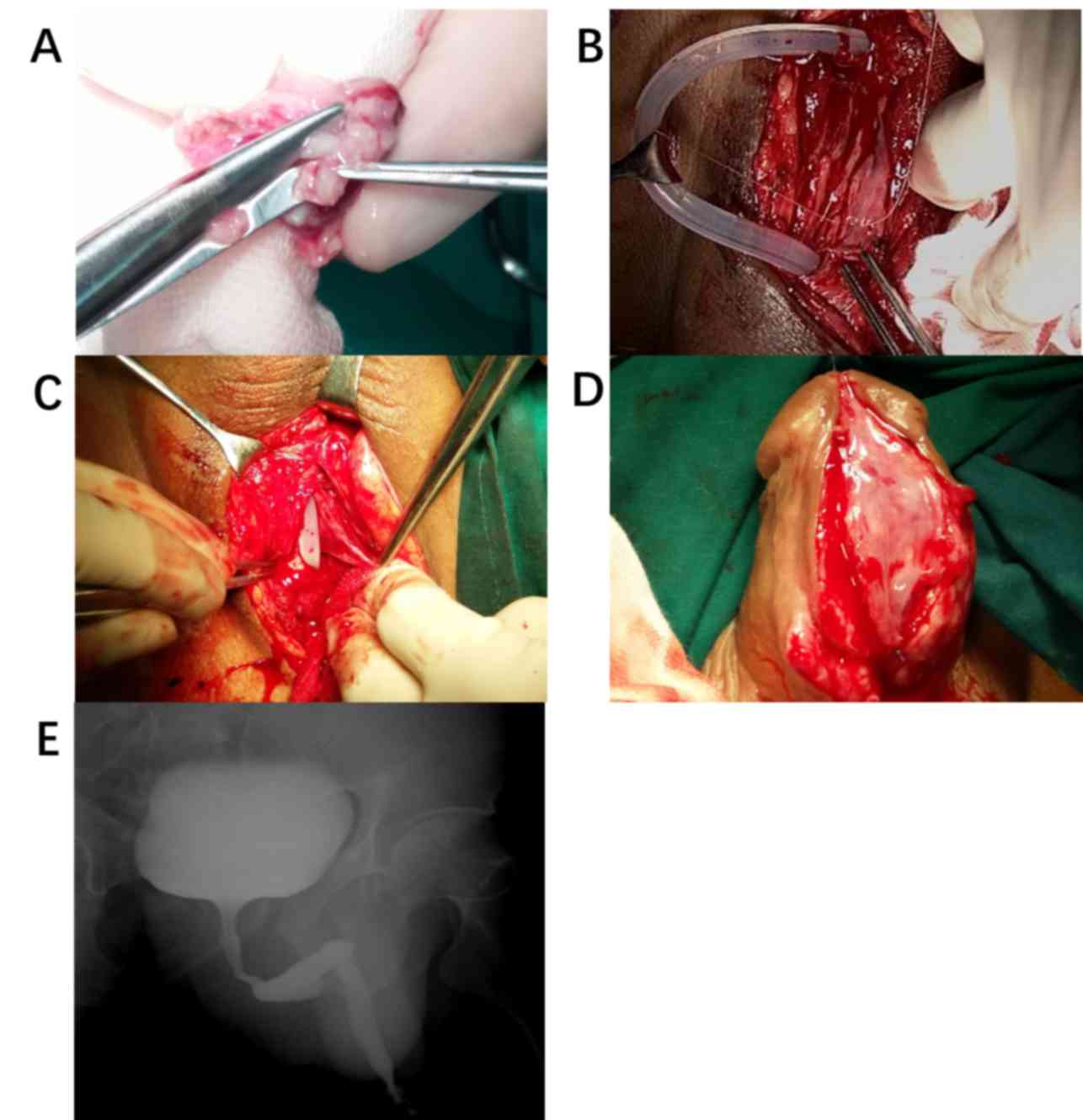
thinned and trimmed according to the size required (Fig. 5A). Dorsal onlay urethroplasty was
performed for case 1 (Fig. 5B and C)
and urethra plate reconstruction was performed for case 2. The
caliber of the reconstructed urethra should be spacious enough to
insert the 22Fr three cavity catheter for continuous bladder
irrigation postoperative. The incision was sewn up layer by layer.
Throughout the whole process, physiological saline and dilute
iodine were used to maintain a moist condition for the wound, and
electrocoagulation was generally not recommended except for massive
bleeding.
Bladder irrigation was stopped once hemorrhaging
disappeared. The catheter was removed 3–4 weeks later, then voiding
cystourethrogram was performed to check urethral condition.
Results
The surgeries were conducted successfully. One-stage
urethral reconstruction was performed in case 1, and the urethra
plate was reconstructed by first-stage in case 2 (Fig. 5D). No perforation, active
cysthemorrhagia or any other complication occurred during or
following surgery. Case 1 had unobstructed urination once the
catheter was removed at 1 month following surgery, and voiding
cystourethrogram indicated that the reconstructed zone was normal
(Fig. 5E). Within 4 months of
follow-up, there was no recrudescence. Case 2 is currently waiting
for the second-stage urethral reconstruction. The urethra plate
reconstructed by bladder mucosa graft has survived, and dysuria has
disappeared.
Discussion
Currently, urethral reconstruction with oral mucosa
graft is the most widely performed surgical approach in
urethroplasty, which has numerous advantages (2). These include the relative ease of
harvesting oral mucosa and minimal complications that may occur.
However, the drawbacks are the limited availability of tissue and
donor site morbidity (2,9,10).
Alternative grafts are also required for patients who are not
candidates for performing oral mucosa graft harvest, particularly
for long, narrow segments and for recurrent strictures following
prior operation using oral mucosa graft. Xu et al (11) reported a feasible procedure for
complex urethral strictures using circumferential colonic mucosa
grafts, which achieved a high success rate of 86%. Palmer et
al (12) reported a feasible,
safe and low morbidity technique for harvesting rectal mucosa graft
for urethral reconstruction via a transanal endoscopic
microsurgical technique. However, this technique carries a risk of
colonic perforation and requires an experienced surgeon, as well as
absence of bowel disease in the patient, which limit the extensive
use of rectal mucosa grafts among many institutions. To the best of
our knowledge, this is the first report of using bladder mucosa
graft harvested via endoscope assisted by water-jet for urethral
reconstruction, which is a minimally invasive approach compared
with conventional surgeries.
Bladder mucosa, with the advantage of providing long
segments, was first used for urethra reconstruction by Memmelaar in
1947 (4). Bladder mucosa is easy to
obtain and does not usually affect bladder function
postoperatively. For the current cases, recovery time was short
following the minimal invasive surgery. Bladder mucosa may be used
for long segment urethral stricture reparation, since it is easy to
obtain long segments of bladder mucosa. Furthermore, bladder mucosa
has similar characteristics to urethral epithelium (2,5–7,13).
Although complications, including meatal stenosis, prolapse and
shrinkage of bladder mucosa, may occur, a high success rate could
be achieved by selecting suitable cases (6,7).
Follow-up results in the current study suggest that the approach is
feasible and safe. Short-term successful outcomes have also been
described previously (4,6,12). In
order to avoid the potential complications following conventional
open surgery for bladder mucosa graft harvest, patients in the
current study underwent a minimally invasive approach of
transurethral endoscopic sub-mucosal dissection via water-jet to
harvest the bladder mucosa. This technique is performed on the
bladder, which is familiar to a urologist and easy to operate on,
and is relatively quick to learn (8). This novel minimally invasive technique
could potentially be provided to patients who are not suitable
candidates for oral mucosa graft.
The technique of endoscopic sub-mucosal dissection
assisted by water-jet in the treatment of digestive tract neoplasia
has been widely used in the clinic, and has been demonstrated to be
a safe and effective method in a minimally invasive operation
(8,14). Fritsche et al (8) presented the first prospective clinical
trial on the application of the technique in transurethral
dissection of the large bladder carcinoma in 2011. Compared with
the digestive tract and colon, the bladder mucosa and muscle layer
are thicker, which makes the surgery safer, with a low incidence of
vesical perforation and obturator nerve reflex). Furthermore,
bladder mucosa is less exposed to electrical damage and can be kept
alive more successfully once it is removed from the bladder
(8).
In terms of postoperative bleeding, complete
hemostasis intra-operative is critical for the success of
reconstructive surgery, because reoperation may destruct the
operative area. According to the data collected from patients who
underwent sub-mucosal dissection of bladder tumor via water-jet,
(which has a similar procedure to the harvest of bladder mucosa in
the present study), no cases of postoperative bleeding were
identified (8).
In conclusion, urethral reconstruction using bladder
mucosa graft harvested via transurethral endoscopic sub-mucosal
dissection assisted by water-jet is an alternative technique for
patients who are not deemed as suitable candidates for
urethroplasty with oral mucosa graft. However, further study of
cases with longer follow-up periods are required to demonstrate its
safety and feasibility.
Acknowledgements
Not applicable.
Funding
The present study was supported by Research Funds of
Tongji Hospital, HUST and Natural Science Foundation of Hubei
Provence to RC (grant no. 2017CFB714). This study was also
supported by Key Items of Health and Family Planning Commission of
Hubei Province to XZ (grant no. WJ2015MA015)
Availability of data and materials
Data sharing is not applicable to this article, as
no datasets were generated or analyzed during the current
study.
Authors' contributions
ZW, RC and XZ conceived and designed the present
study; RC and JH performed the experiments; TW, JL and SW analyzed
data; RC and ZW interpreted the results; ZW and RC prepared the
figures; and ZW, RC and XZ edited and revised manuscript. All
authors approved final version of manuscript.
Ethics approval and consent to
participate
Ethical approval was granted by the medical ethics
committee of Tongji hospital, Tongji medical college, Huazhong
University of Science and Technology (Wuhan, China).
Patient consent for publication
Written informed consent was obtained from the
patients for the publication of this article and any accompanying
images. The information used to identify patients was deleted.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Mangera A and Chapple C: Management of
anterior urethral stricture: An evidence-based approach. Curr Opin
Urol. 20:453–458. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Mangera A, Patterson JM and Chapple CR: A
systematic review of graft augmentation urethroplasty techniques
for the treatment of anterior urethral strictures. Eur Urol.
59:797–814. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Bhargava S and Chapple CR: Buccal mucosal
urethroplasty: Is it the new gold standard? BJU Int. 93:1191–1193.
2004. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Memmelaar J: Use of bladder mucosa in a
one-stage repair of hypospadias. J Urol. 58:68–73. 1947. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Monfort G, Bretheau D, Di Benedetto V and
Bankole R: Urethral stricture in children: Treatment by
urethroplasty with bladder mucosa graft. J Urol. 148:1504–1506.
1992. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Kinkead TM, Borzi PA, Duffy PG and Ransley
PG: Long-term followup of bladder mucosa graft for male urethral
reconstruction. J Urol. 151:1056–1058. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Ozgok Y, Ozgür Tan M, Kilciler M, Tahmaz L
and Erduran D: Use of bladder mucosal graft for urethral
reconstruction. Int J Urol. 7:355–360. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Fritsche HM, Otto W, Eder F, Hofstädter F,
Denzinger S, Chaussy CG, Stief C, Wieland WF and Burger M:
Water-jet-aided transurethral dissection of urothelial carcinoma: A
prospective clinical study. J Endourol. 25:1599–1603. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Chapple C, Andrich D, Atala A, Barbagli G,
Cavalcanti A, Kulkarni S, Mangera A and Nakajima Y: SIU/ICUD
consultation on urethral strictures: The management of anterior
urethral stricture disease using substitution urethroplasty.
Urology. 83 Suppl 3:S31–S47. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Barbagli G, Vallasciani S, Romano G,
Fabbri F, Guazzoni G and Lazzeri M: Morbidity of oral mucosa graft
harvesting from a single cheek. Eur Urol. 58:33–41. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Xu YM, Qiao Y, Sa YL, Zhang J, Fu Q and
Song LJ: Urethral reconstruction using colonic mucosa graft for
complex strictures. J Urol. 182:1040–1043. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Palmer DA, Marcello PW, Zinman LN and
Vanni AJ: Urethral reconstruction with rectal mucosa graft onlay: A
novel, minimally invasive technique. J Urol. 196:782–786. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Wessells H and McAninch JW: Use of free
grafts in urethral stricture reconstruction. J Urol. 155:1912–1915.
1996. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Schumacher B, Charton JP, Nordmann T,
Vieth M, Enderle M and Neuhaus H: Endoscopic submucosal dissection
of early gastric neoplasia with a water jet-assisted knife: A
Western, single-center experience. Gastrointest Endosc.
75:1166–1174. 2012. View Article : Google Scholar : PubMed/NCBI
|