Introduction
Meniscus injury is one of the most common injuries
in the knee joint. In general, men are more frequently affected
than women. Meniscus injury is manifested as joint swelling,
quadriceps muscle atrophy, localized pain, and tenderness. Among
them, the presence of localized tenderness in the internal and
lateral space are the most frequent symptoms (1). Arthroscopy is a minimally invasive
surgical method, which has been clinically applied for almost 50
years (2). In recent years,
arthroscopy has become the most applied surgical procedure for
treating meniscal injury.
The current concept of meniscus treatment considers
that the normal tissue of the meniscus should be retained to the
greatest extent, and the lesioned area should be surgically
repaired or removed (3).
Arthroscopic meniscus surgery mainly includes total meniscectomy,
meniscus plasty and perforation closure, of which total
meniscectomy is effective in the early remission of clinical
symptoms. However, total meniscectomy under arthroscopy can damage
the function of the knee joint in the clinical application, leading
to increased risk of degenerative knee disease. More seriously,
elevated tension required for articular cartilage after total
meniscectomy would easily progress into articular cartilage
degeneration or osteoarthritis (4).
For the elderly patients with meniscus injury, some
researchers recommend total meniscectomy since the dehydrated and
degenerative meniscus has already lost its function (5). Other researchers believe that the
meniscus injury in the majority of patients is relatively slight
and meniscus still retains a certain function. Total meniscectomy
would accelerate osteoarthritis process. They prefer meniscal
plasty to maximally retain the physiological function and alleviate
joint degeneration (6). Our study
enrolled 115 patients with meniscus injury treated in the First
People's Hospital of Wujiang District Suzhou (Suzhou, China). We
explored the pros and cons of meniscal plasty and total
meniscectomy, so as to provide new directions in treating
middle-aged meniscus patients.
Patients and methods
Basic characteristics
One hundred and fifteen middle-aged and elderly
patients with meniscal injury treated from May 2012 to October 2014
were enrolled. These patients all received complete follow-up.
Among them, 68 cases were male patients and 47 were females, with
the average age of 58.31±6.62 years (50–67 years). According to the
type of meniscus injury, there were 12 cases of traumatic meniscus
injury and 103 cases of non-traumatic meniscus injury. Ninety eight
patients experienced unilateral meniscus injury and 17 experienced
bilateral meniscus injuries. Ultimately, there were 70 patients (80
cases of knee joint) who received meniscus plasty under arthroscopy
and 45 patients (52 cases of knee joint) received total
meniscectomy under arthroscopy. All patients underwent preoperative
knee X-ray and MRI examination. No significant moderate-to-severe
osteoarthritis (7), and ligament
injury were observed. This study was approved by the Ethics
Committee of The First People's Hospital of Wujiang District
Suzhou. Signed informed consents were obtained from all
participants before the study.
Surgical procedure
Subjects received epidural anesthesia or general
anesthesia and were in the supine position. After routine
disinfection treatment, a 0.5 cm incision was cut on the lateral
patellar ligament and arthroscope was set. Saline was injected into
the joint cavity and we ultimately determined the surgical
procedure based on the location, type and injury degree.
Meniscus plasty under arthroscopy: Meniscus tissue
was kept approximately 5–6 mm in length. Meniscus tissue was
retained as much as possible. The remaining meniscus was repaired
using the radiofrequency knife to keep it intact (8).
Total meniscectomy under arthroscopy: The fragment
was morselized using basket forceps or a large tear was removed en
bloc. The anterior oblique tear was cut with arthroscopic scissors
and the fragment was removed using a grasper. The anterior and
posterior edges were trimmed of the meniscus to prevent stress
risers in the remaining meniscal rim.
Postoperative rehabilitation: Patients were
encouraged to exercise toes immediately after the surgery. Knee
flexion was gradually practiced one week after the surgery.
Weight-bearing exercise was encouraged 2–4 weeks later. After 12
weeks, daily activities could be restored and patients were allowed
regular physical activity 6 months later.
Observation indicators
Length of stay, operation time and visual analogue
score (VAS) between the two groups were compared. Knee function was
evaluated before the surgery and at the last follow-up using
international knee documentation committee subjective form (IKDC
2000) and Lysholm score. The differences of postoperative clinical
efficacy and improvement of knee function scores before and after
surgery in both groups were observed.
Statistical analysis
SPSS21.0 (Statistical Product and Service Solutions)
statistical software package (IBM Corp., Armonk, NY, USA) was used
for data analysis. Data were expressed as mean ± SEM. The t-test
was used to analyze the difference between two groups. The one-way
ANOVA was used to analyze the data among different groups, followed
by post-hoc LSD or SNK analysis. P<0.05 was considered to
indicate a statistically significant difference.
Results
Basic characteristics of subjects
One hundred and fifteen middle-aged and elderly
patients with meniscal injury treated in the hospital from May 2012
to October 2014 were enrolled. The average postoperative follow-up
of these patients was 2.6±0.3 years (2.3–3 years). There were 70
cases in experimental group with the average age of 57.26±7.82
years (50–65 years) and 45 cases in control group with the average
age of 59.43±6.33 years (50–67 years). No significant differences
were found in sex, age and meniscus injury site between the two
groups (P>0.05; Table I).
 | Table I.General data of the two groups. |
Table I.
General data of the two groups.
|
|
| Groups |
|
|---|
|
|
|
|
|
|---|
| Items | No. | Experimental | Control | P-value |
|---|
| Sex |
| Male | 68 | 43 | 25 | 0.5317 |
|
Female | 47 | 27 | 20 |
|
| Disease date |
| <2
months | 49 | 30 | 19 | 0.9464 |
| ≥2
months | 66 | 40 | 26 |
|
| Cause of disease |
|
Traumatic | 12 | 5 | 7 | 0.1498 |
|
Non-traumatic | 103 | 65 | 38 |
|
| Injured knee |
| Left | 51 | 32 | 19 | 0.6397 |
|
Right | 64 | 38 | 27 |
|
| Injured part |
| Anterior
horn | 23 | 15 | 8 | 0.793 |
| Somatic
part | 62 | 36 | 26 |
|
| Posterior
horn | 30 | 19 | 11 |
|
| BMI |
| <30
kg/m2 | 88 | 51 | 37 | 0.2475 |
| ≥30
kg/m2 | 27 | 19 | 8 |
|
| No. of
comorbidities |
| 0–1 | 94 | 59 | 35 | 0.3779 |
| 2 | 21 | 11 | 10 |
|
| Kellgren-Lawrence
grade |
| 0 | 13 | 8 | 5 | 0.6788 |
| 1 | 88 | 52 | 36 |
|
| 2 | 14 | 10 | 4 |
|
| Knee flexion |
|
<120° | 11 | 6 | 5 | 0.6513 |
|
≥120° | 104 | 64 | 40 |
|
| Swelling |
| No | 27 | 18 | 9 | 0.4804 |
| Yes | 88 | 52 | 36 |
|
Comparison of operation time, length
of stay and recovery time
We did not observe significant differences in length
of stay and recovery time between the two groups (P>0.05).
However, shorter operation time was found in control group than
that of experimental group, indicating smaller surgical risk of
total meniscectomy (P<0.05; Fig.
1).
Comparison of therapeutic
efficacy
Postoperative VAS in both groups was decreased
compared to the preoperative ones, which were decreased from 8.14
to 5.85 and 8.28 to 5.59 in experimental and control group,
respectively (P<0.001). However, no significant difference in
relieving postoperative pain between the two groups, indicating
that meniscus plasty and total meniscectomy have similar effect on
improving knee pain (P>0.05; Fig.
2).
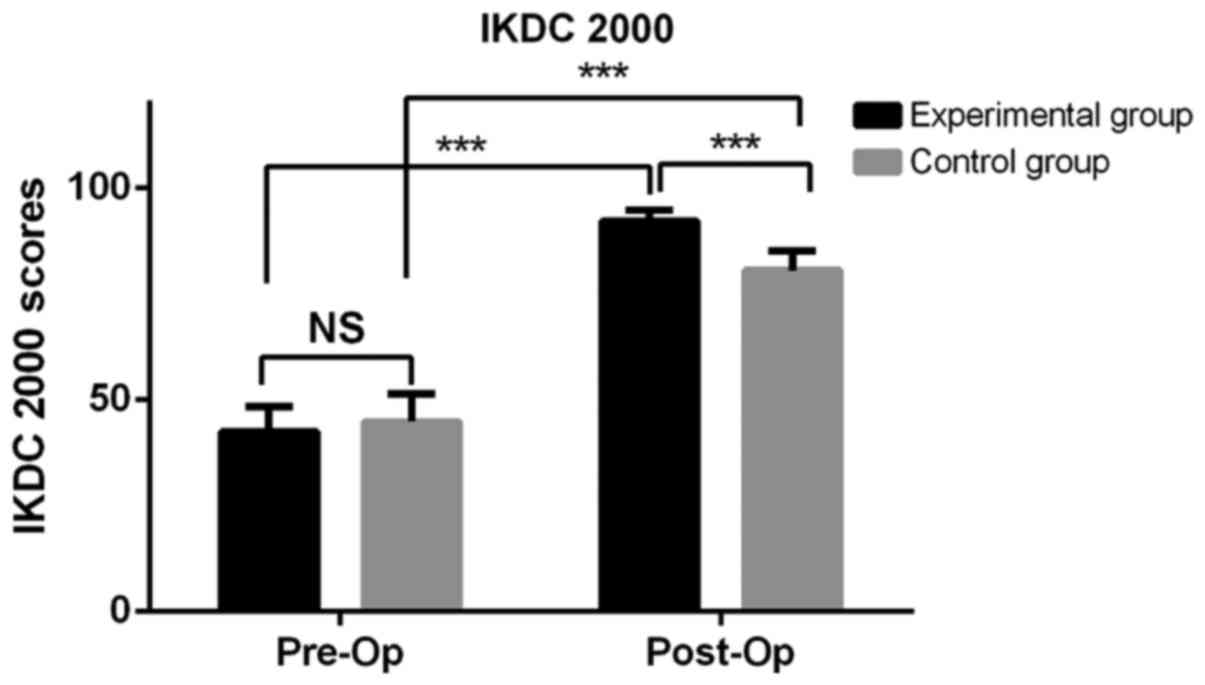
IKDC 2000 at the final follow-up were decreased from
92.22 to 42.42 and 80.53 to 44.89 in experimental group and control
group, respectively (P<0.001; Fig.
3). The improvement of IKDC 2000 was better in experimental
than that of control group.
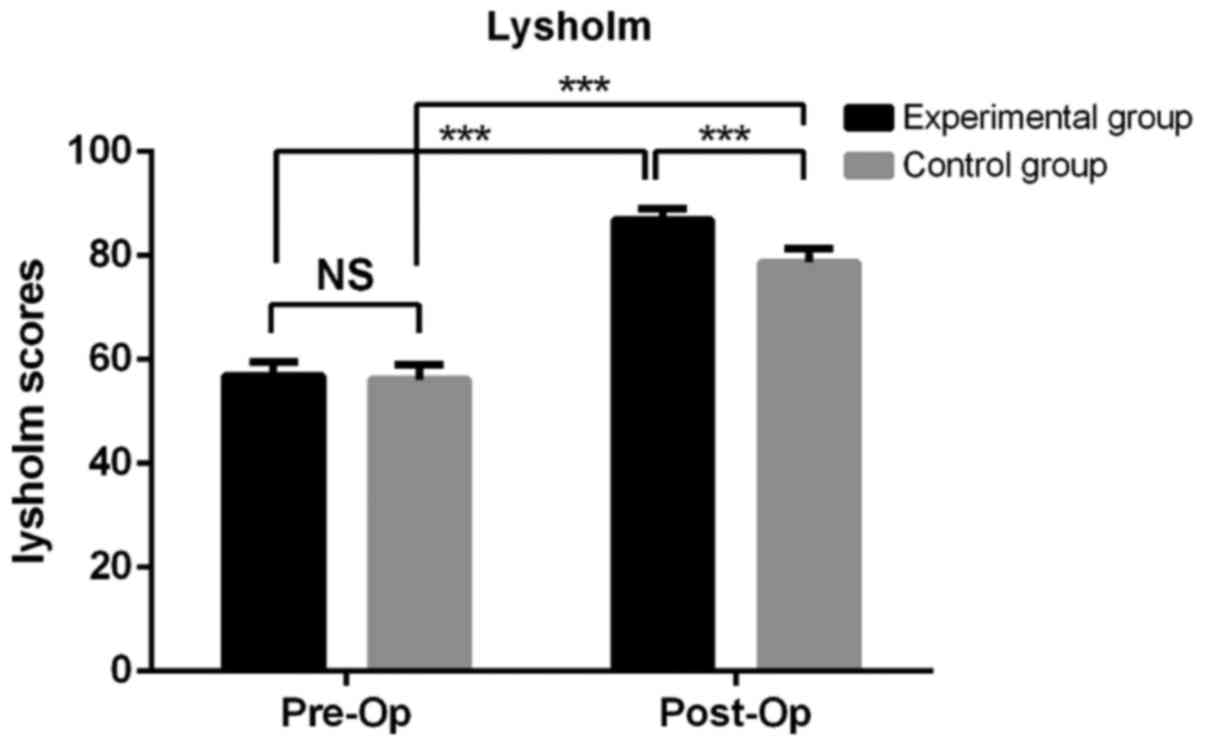
Postoperative Lysholm were elevated from 56.87 to
86.91 and 56.09 to 78.73 in experimental and control group,
respectively (P<0.001; Fig. 4).
Significant difference was found in Lysholm at the follow-up period
between the two groups, suggesting that the improvement of knee
function is better in experiment group.
Comparison of postoperative
complications
No infection occurred during the follow-up period in
the two groups. There were some patients experiencing deep venous
thrombosis, joint pain and swelling in the lower extremities within
three months after the operation. The above symptoms gradually
improved and the thrombus gradually disappeared after corresponding
treatment. No significant difference in postoperative complication
was found between the two groups (P>0.05; Table II).
 | Table II.Complications of the two groups. |
Table II.
Complications of the two groups.
|
|
| Groups |
|
|---|
|
|
|
|
|
|---|
| Items | No. | Experimental | Control | P-value |
|---|
| Deep venous
thrombosis | 3 | 1 | 2 | 0.9051 |
| Swelling | 18 | 8 | 10 |
|
| Pain | 8 | 3 | 5 |
|
| Swelling | 18 | 8 | 10 |
|
Discussion
Meniscus is the fibrocartilage between the femoral
condyle and the tibial plateau. Meniscus possesses important
functions, such as load transition, shock absorption, joint
stabilization and knee activity cooperation. Mechanical stability
of knee joint would be damaged if meniscus injury or meniscus tear
occurs, leading to early onset of osteoarthritis (9). Therefore, meniscal injury should be
repaired as much as possible. The advantages of arthroscopic
surgery for meniscus injury mainly include small incision, slight
trauma and quick recovery of daily activity. Besides, arthroscopy
could examine complex injuries related to cartilage and ligament
injuries. Arthroscopic surgery has replaced open surgery as the
best treatment for meniscal injury (10).
The vascularized area of meniscus can be classified
into the red-red zone (vascular portion that is located at 1–3 mm
away from meniscus synovium), red-white zone (blood supply is from
the end branch of capillaries in the red-red zone, which is located
3–5 mm inside of red-red zone), and white-white zone (non-vascular
portion that is located inside the red-white zone) according to the
degree of vascularity. The capillary plexus gradually decreases
with age. There are many great vessels in the meniscus before 14
years. However, 75% of great vessels gradually disappear from the
center of the meniscus after 14 years. The meniscus vascular area
is only 10–30% of the periphery of the meniscus in adulthood
(11,12). This special anatomy of meniscus makes
it difficult for repair of middle-aged patients with meniscal tear.
However, meniscus still retains its value since peripheral vascular
supply is functional. In the present study, meniscus tissue was
kept approximately 5–6 mm in length. We tried to retain the
meniscus function so as to reduce the sequelae after
meniscectomy.
Pathological changes of meniscus lesions in
middle-aged and elderly patients are remarkably different from
those of young adults. The majority of meniscal injuries in young
adults are caused by direct or indirect violence. Meniscus injuries
in middle-aged and elderly patients are commonly related to
meniscus degeneration. Loss of moist, thinner layer and decreased
elasticity all lead to adhesion and poor mobility of meniscus.
Moreover, decreased elastic strain and buffering effect further
exaggerate meniscus tear or wear (13). Patients with meniscus injury are
manifested as knee pain, pressure pain at the joint line, limited
range of knee flexure and knee swelling. In some severe cases,
locked joint and joint dysfunction are observed (14). In our study, only 12/115 patients
were traumatic meniscus injury cases. Other patients had no obvious
trauma history and their meniscus injuries resulted from chronic
strain and degenerative causes, which was consistent with other
reports (15). Among them, 104
(90.43%) cases presented limited knee extension function and 88
(76.52%) presented swelling knee joint. The diagnosis of meniscus
injury could be confirmed with other vital signs and MRI
examination (16).
Untimely treatment of meniscus injury would lead to
aggravated meniscus tear during repeated flexion and extension of
the knee joint. The torn meniscus also result in joint cartilage
damage to the femur and tibia due to the compressive force,
eventually leading to severe secondary articular cartilage injury
(17,18). Higuchi et al (19) performed a 12.2-year follow-up and
found that the amount of resected meniscus is one of the decisive
factors affecting the therapeutic effect. After the total
meniscectomy, axial alignment of the lower extremity was remarkably
changed, which was closely related to the resected area of
meniscus. Baratz et al (20)
found that the contact area of the femoral condyle articular
surface is reduced by 75%, and the articular surface contact stress
is increased to 235% after total meniscectomy. The role of the
meniscus in receiving and conducting the load disappears, resulting
in a significant change in the axial alignment of the lower
extremity. However, the contact area is only reduced by 10%, and
the contact stress is increased by 65% after partial meniscectomy
(20,21). Alterations of axial alignment of the
lower extremity result in damage to articular cartilage in the
non-weight-bearing region of the femur and tibia, and eventually
lead to osteoarthritis. The occurrence of osteoarthritis gradually
leads to swelling, pain and limited functional activities of the
knee joint, which further affects the daily life of affected
population. In the present study, IKDC 2000 and Lysholm scores were
better in the experimental group than those of the control group at
the final follow-up. Our data indicated that the partial meniscus
retained in the meniscus plasty can effectively alleviate the knee
joint degeneration and progress of arthritis to maintain knee
function.
Arthroscopy is an effective approach to treat knee
joint diseases. It has the advantages of high efficiency and
minimal invasiveness. Although the proportion of postoperative
complications of knee arthroscopic surgery is approximately 2%, it
is clinically significant due to the dramatic increase in the
number of knee arthroscopic surgeries. There are also many cases of
postoperative complications of knee arthroscopic surgery (22). Small (23) researched 10,262 cases of arthroscopic
surgery (of which, 8,741 cases underwent knee arthroscopy). The
incidence of postoperative complications was 1.68%. Among them,
joint hemostasis, infection and thromboembolism occurred most
frequently, which accounted for 60.1, 12.1 and 6.9%, respectively.
In our study, there were 3 (2.6%) cases of deep vein thrombosis, 8
(6.9%) of knee pain and 18 (15.6%) of knee swelling. No significant
adverse effect was found after anticoagulant local physiotherapy
was given.
Arthroscopic surgery, as a minimally invasive
surgery, and requires the operator to strictly control surgical
indications. Proficient in knee arthroscopy and careful procedures
can minimize the occurrence of postoperative complications and
comprehensively reflect the minimally invasive value of
arthroscopic knee surgery. Meniscus plasty and total meniscectomy
under arthroscopy can effectively improve knee joint pain symptoms
in a short period of time. In particular, meniscus plasty
remarkably alleviates the occurrence of knee osteoarthritis,
maintains the knee joint function, and improves the daily activity
of affected patients. Meniscus plasty should be the preferred
treatment for elderly patients with meniscus injury who do not have
significant moderate and severe osteoarthritis. Furthermore,
studies with large sample and long-term follow-up data are still
needed for the further exploration of the long-term knee function
changes in patients with meniscal injury.
In conclusion, both meniscal plasty and total
meniscectomy under arthroscopy can effectively relieve knee pain in
a short time. Meniscal plasty could remarkably alleviate the
progression of knee osteoarthritis, maintain knee function and
improve daily life of affected population. We consider that
meniscal plasty should be the preferred approach in treating
middle-aged and elderly patients with meniscus injury.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
All data generated or analyzed during this study are
included in this published article.
Authors' contributions
YS, ZT and JZh designed the study and performed the
experiments. LZ and JZe collected the data. ZT and RL analyzed the
data. YS and ZT prepared the manuscript. All authors read and
approved the final manuscript.
Ethics approval and consent to
participate
This study was approved by the Ethics Committee of
The First People's Hospital of Wujiang District Suzhou (Suzhou,
China). Signed informed consents were obtained from the patients or
the guardians.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Rohren EM, Kosarek FJ and Helms CA:
Discoid lateral meniscus and the frequency of meniscal tears.
Skeletal Radiol. 30:316–320. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Johnson MJ, Lucas GL, Dusek JK and Henning
CE: Isolated arthroscopic meniscal repair: A long-term outcome
study (more than 10 years). Am J Sports Med. 27:44–49. 1999.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Kollias SL and Fox JM: Meniscal repair.
Where do we go from here? Clin Sports Med. 15:621–630.
1996.PubMed/NCBI
|
|
4
|
Rangger C, Klestil T, Gloetzer W, Kemmler
G and Benedetto KP: Osteoarthritis after arthroscopic partial
meniscectomy. Am J Sports Med. 23:240–244. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Bin SI, Lee SH, Kim CW, Kim TH and Lee DH:
Results of arthroscopic medial meniscectomy in patients with grade
IV osteoarthritis of the medial compartment. Arthroscopy.
24:264–268. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Englund M: Meniscal tear - a feature of
osteoarthritis. Acta Orthop Scand Suppl. 75:1–45. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Hochberg MC, Altman RD, Brandt KD, Clark
BM, Dieppe PA, Griffin MR, Moskowitz RW and Schnitzer TJ: American
College of Rheumatology: Guidelines for the medical management of
osteoarthritis. Part II. Osteoarthritis of the knee. Arthritis
Rheum. 38:1541–1546. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Krych AJ, Bert JM and Levy BA: Treatment
of OA of the knee in the middle-aged athlete: The role of
arthroscopy. Sports Med Arthrosc Rev. 21:23–30. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
McDermott ID and Amis AA: The consequences
of meniscectomy. J Bone Joint Surg Br. 88:1549–1556. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Nepple JJ, Dunn WR and Wright RW: Meniscal
repair outcomes at greater than five years: A systematic literature
review and meta-analysis. J Bone Joint Surg Am. 94:2222–2227. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Arnoczky SP and Warren RF:
Microvasculature of the human meniscus. Am J Sports Med. 10:90–95.
1982. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Arnoczky SP and Warren RF: The
microvasculature of the meniscus and its response to injury. An
experimental study in the dog. Am J Sports Med. 11:131–141. 1983.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Maffulli N, Longo UG, Campi S and Denaro
V: Meniscal tears. Open Access J Sports Med. 1:45–54. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Levy IM, Torzilli PA and Warren RF: The
effect of medial meniscectomy on anterior-posterior motion of the
knee. J Bone Joint Surg Am. 64:883–888. 1982. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Englund M, Roemer FW, Hayashi D, Crema MD
and Guermazi A: Meniscus pathology, osteoarthritis and the
treatment controversy. Nat Rev Rheumatol. 8:412–419. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Bhattacharyya T, Gale D, Dewire P,
Totterman S, Gale ME, McLaughlin S, Einhorn TA and Felson DT: The
clinical importance of meniscal tears demonstrated by magnetic
resonance imaging in osteoarthritis of the knee. J Bone Joint Surg
Am. 85-A:4–9. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Krause WR, Pope MH, Johnson RJ and Wilder
DG: Mechanical changes in the knee after meniscectomy. J Bone Joint
Surg Am. 58:599–604. 1976. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
McCarty EC, Marx RG and DeHaven KE:
Meniscus repair: Considerations in treatment and update of clinical
results. Clin Orthop Relat Res. 402:122–134. 2002. View Article : Google Scholar
|
|
19
|
Higuchi H, Kimura M, Shirakura K, Terauchi
M and Takagishi K: Factors affecting long-term results after
arthroscopic partial meniscectomy. Clin Orthop Relat Res.
377:161–168. 2000. View Article : Google Scholar
|
|
20
|
Baratz ME, Fu FH and Mengato R: Meniscal
tears: The effect of meniscectomy and of repair on intraarticular
contact areas and stress in the human knee. A preliminary report.
Am J Sports Med. 14:270–275. 1986. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Ahmed AM and Burke DL: In-vitro
measurement of static pressure distribution in synovial joints -
Part I: Tibial surface of the knee. J Biomech Eng. 105:216–225.
1983. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Pierzchała A, Kusz D and Widuchowski J:
Complication of arthroscopy of the knee. Wiad Lek. 56:460–467.
2003.(In Polish). PubMed/NCBI
|
|
23
|
Small NC: Complications in arthroscopic
surgery performed by experienced arthroscopists. Arthroscopy.
4:215–221. 1988. View Article : Google Scholar : PubMed/NCBI
|