Introduction
The morbidity and mortality of atherosclerotic
coronary heart disease (CHD) have increased with the development of
economy and the improvement of human living standard, and heart
disease is ranked first of the diseases seriously threatening human
life and health at present (1).
Studies have shown that male incidence is higher than female, it is
not completely clear what the specific pathogenesis of CHD is, and
there are various theories, including endothelial dysfunction,
inflammatory reaction and lipid deposition hypothesis (2,3). In
addition to sex, age and blood lipid, the pathogenic factors
affecting CHD are mainly related to blood sugar, blood pressure,
obesity, smoking, and drinking. In recent years, a large number of
studies have proved that homocysteine (Hcy) is also one of the risk
factors for CHD (4–6).
Hcy, a non-essential amino acid, is converted mainly
from methionine intake in the diet (7). It has been reported that Hcy may damage
vascular endothelial cells and affect lipid metabolism,
contributing to the occurrence of atherosclerosis, thus inducing
cardiovascular and cerebrovascular diseases, but it is not
completely clear what the mechanism is (8,9).
Abnormal lipid metabolism is the most important risk factor in
atherosclerosis. Generally speaking, indicators of blood lipid
include total cholesterol (TC), triglyceride (TG), high-density
lipoprotein cholesterol (HDL-C) and low-density lipoprotein
cholesterol (LDL-C) (10). Studies
have found that Hcy participates in and speeds up the
auto-oxidation of LDL, while oxidized LDL cannot be recognized by
normal LDL receptors, leading to the occurrence and development of
acute coronary syndrome (11).
The purpose of this study is to compare the Hcy and
blood lipid level in serum of CHD patients with that of healthy
people and to perform statistical analysis on the risk factors for
CHD, to provide reference value for the assessment of disease and
the prevention and prognosis of CHD.
Patients and methods
General information
A total of 148 patients who were diagnosed as CHD
patients by coronary arteriography in Weifang People's Hospital
(Weifang, China) between January 2014 and December 2017 were
collected as study group using retrospective methods, including 89
male and 59 female with an average age of 56.42±9.84 years. The
study group was divided into 67 cases in angina pectoris group, 49
cases in acute myocardial infarction group and 32 cases in old
myocardial infarction group according to the clinical
characteristics. Another 120 healthy people in the same period were
selected as control group, including 64 males and 56 females with
an average age of 54.21±12.0 years. Exclusion criteria were:
Subjects who were pregnant, with lactation, tumors, liver and renal
insufficiency and various infections and immune diseases. No drugs
affecting Hcy metabolism were used and no steroid drug therapy was
received by the patients within the 2 months of the study. A total
of 268 subjects signed the informed consent. General information on
the candidates is shown in Table I.
The study was approved by the Ethics Committee of Weifang People's
Hospital.
 | Table I.General information [n (%)]. |
Table I.
General information [n (%)].
| Factors | Study group
(n=148) | Control group
(n=120) | χ2 | P-value |
|---|
| Age (years) |
| ≥54 | 102 (68.92) | 72
(60.00) | 2.315 | 0.128 |
|
<54 | 46
(31.08) | 48
(40.00) |
|
|
| Sex |
| Male | 89
(60.14) | 64
(53.33) | 1.252 | 0.263 |
|
Female | 59
(39.86) | 56
(46.67) |
|
|
| Long-term
smoking |
| Yes | 91
(61.49) | 32
(26.67) | 32.360 | <0.001 |
| No | 57
(38.51) | 88
(73.33) |
|
|
| Long-term
drinking |
| Yes | 35
(23.65) | 49
(40.83) | 9.094 | 0.003 |
| No | 113 (76.35) | 71
(59.17) |
|
|
| Hypertension |
| Yes | 87
(58.78) | 23
(19.17) | 42.980 | <0.001 |
| No | 61
(41.22) | 97
(80.83) |
|
|
| Diabetes |
| Yes | 43
(29.05) | 18
(15.00) | 7.445 | 0.006 |
| No | 105 (70.95) | 102 (85.00) |
|
|
| Hyperlipidemia |
| Yes | 59
(39.86) | 27
(22.50) | 9.170 | 0.003 |
| No | 89
(60.14) | 93
(77.50) |
|
|
| BMI |
|
<18.5 | 39
(26.35) | 23
(19.17) | 9.197 | 0.010 |
|
18.50–24.9 | 47
(31.76) | 60
(50.00) |
|
|
|
>25.0 | 62
(41.89) | 37
(30.83) |
|
|
Instruments and reagents
The DNM-9606 enzyme marker analyzer was purchased
from Beijing Plang New Technology Co., Ltd. (Beijing, China); Hcy
ELISA kit from Xiamen Huijia Biotechnology Co., Ltd. (Xiamen,
China); HI7100 biochemistry analyzer and its reagents from Hitachi,
Ltd. (Tokyo, Japan); blood lipid kit from Shanghai Yubo
Biotechnology Co., Ltd. (Shanghai, China).
Determination of Hcy and blood lipid
levels in serum
All subjects were fasting for >12 h on an empty
stomach before examination and no smoking, drinking and high-fat
food for 24 h. Venous blood (3 ml) was collected from patients on
an empty stomach in the study and control group, and Hcy and blood
lipid content in serum were determined using centrifugation at
8,000 × g for 20 min at 4°C. The Hcy level in serum was determined
quantitatively using enzyme-linked immunosorbent assay. TC was
determined using enzyme method, TG using glycerol phosphate oxidase
method and HDL-C and LDL-C using selective inhibition method. The
indicator of each group was determined 3 times and its average
value was taken. All steps were strictly in accordance with the
instructions.
Statistical analysis
Data analysis was performed using SPSS 17.0
statistical software (SPSS, Inc., Chicago, IL, USA). The
enumeration data were tested by χ2 test, the comparison of
measurement data between groups was tested by t-test, the
comparison among multiple groups was performed using one-way ANOVA,
and pairwise comparison between groups was performed using SNK-q
test. Analysis of risk factors for the disease was performed using
logistic regression. At P<0.05, the difference was considered
statistically significant.
Results
Comparison of Hcy and blood lipid
levels in serum between the two groups
Comparison of Hcy and blood lipid levels in serum
between the study and control group was performed. The HDL-C level
in the study group was significantly lower than that in control
group, while the levels of Hcy, TC, TG and LDL-C were significantly
higher than that in control group, and the differences were
statistically significant (P<0.001). Specific information is
shown in Fig. 1 and Table II.
 | Table II.Comparison of Hcy and blood lipid
levels in serum between the study and control group. |
Table II.
Comparison of Hcy and blood lipid
levels in serum between the study and control group.
| Groups | n | Hcy (µmol/l) | TC (mmol/l) | TG (mmol/l) | HDL-C (mmol/l) | LDL-C (mmol/l) |
|---|
| Study group | 148 | 21.06±5.28 | 4.64±1.06 | 1.96±0.33 | 0.85±0.13 | 2.29±0.57 |
| Control group | 120 | 12.03±3.95 | 4.21±0.62 | 1.18±0.27 | 1.41±0.26 | 2.01±0.50 |
| t |
| 15.540 | 3.931 | 20.840 | 22.910 | 4.223 |
| P-value |
| <0.001 | <0.001 | <0.001 | <0.001 | <0.001 |
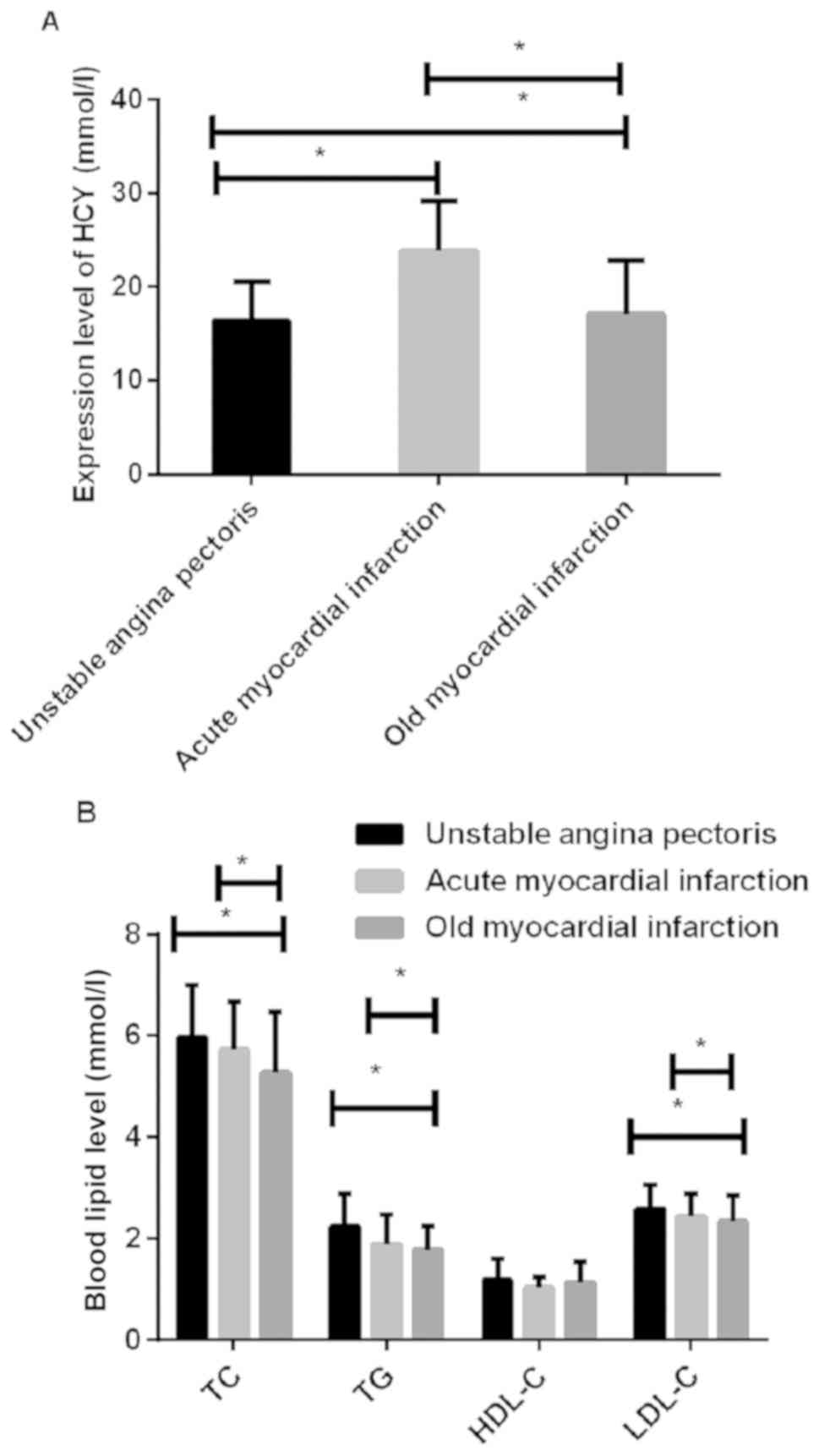
Comparison of Hcy and blood lipid
levels in serum in different types of CHD
The study group was divided into angina pectoris,
acute myocardial infarction and old myocardial infarction group
according to the clinical manifestations of CHD patients. The
difference was not statistically significant in the HDL-C level in
patients among the three groups (P>0.05), but the differences
were statistically significant in the levels of Hcy, TC, TG and
LDL-C in serum of patients among the three groups (P<0.05). The
Hcy level in acute and old myocardial infarction group was higher
than that in angina pectoris group, and in old myocardial
infarction group was lower than in acute myocardial infarction
group (P<0.05); the TC level in angina pectoris group was higher
than that in acute and old myocardial infarction group, and in
acute myocardial infarction group was higher than in old myocardial
infarction group (P<0.05); the TG level in acute and old
myocardial infarction group was lower than that in angina pectoris
group, and in old myocardial infarction group was lower than in
acute myocardial infarction group (P<0.05); the LDL-C level in
acute and old myocardial infarction group was lower than that in
angina pectoris group, and in old myocardial infarction group was
lower than in acute myocardial infarction group (P<0.05).
Specific information is shown in Fig.
2 and Table III.
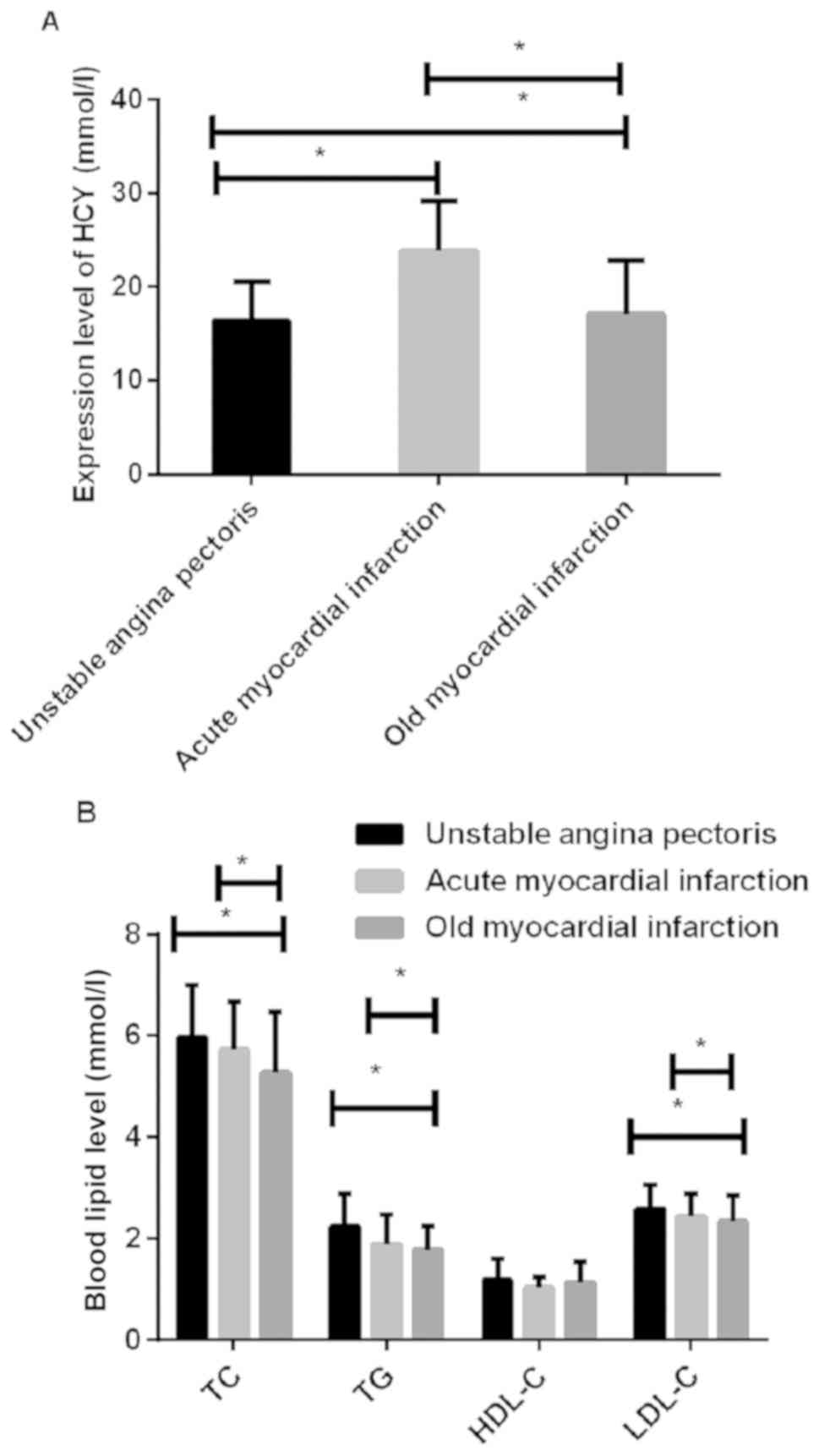 | Figure 2.Comparison of Hcy and blood lipid
levels in serum in different types of CHD. (A) The results of
enzyme-linked immunosorbent assay showed that there was a
significant difference in the Hcy level in patients among angina
pectoris, acute myocardial infarction and old myocardial infarction
group (*P<0.05). (B) TC was determined using enzyme method, TG
using glycerol phosphate oxidase method and HDL-C and LDL-C using
selective inhibition method. The results showed that there was no
significant difference in the HDL-C level in patients among angina
pectoris, acute myocardial infarction and old myocardial infarction
group (P>0.05). There was a significant difference in the levels
of Hcy, TC, TG and LDL-C in patients among the three groups
(P<0.05); the differences were statistically significant in the
levels of Hcy, TC, TG and LDL-C between acute and old myocardial
infarction and angina pectoris group (P<0.05); the differences
were statistically significant in the levels of Hcy, TC, TG and
LDL-C between old and acute myocardial infarction group
(*P<0.05). Hcy, homocysteine; CHD, coronary heart disease; TC,
total cholesterol; TG, triglyceride; HDL-C, high-density
lipoprotein cholesterol; LDL-C, low-density lipoprotein
cholesterol. |
 | Table III.Comparison of Hcy and blood lipid
levels in serum in different types of CHD. |
Table III.
Comparison of Hcy and blood lipid
levels in serum in different types of CHD.
| Diseases | n | Hcy (µmol/l) | TC (mmol/l) | TG (mmol/l) | HDL-C (mmol/l) | LDL-C (mmol/l) |
|---|
| Angina pectoris | 67 | 16.42±4.16 | 5.97±1.02 | 2.24±0.65 | 1.18±0.42 | 2.59±0.47 |
| Acute myocardial
infarction | 49 |
23.81±5.37b |
5.72±0.95b |
1.89±0.58b | 1.03±0.21 |
2.42±0.46b |
| Old myocardial
infarction | 32 |
17.13±5.64a,b |
5.26±1.21a,b |
1.77±0.47a,b | 1.13±0.41 |
2.33±0.52a,b |
| F-value |
| 34.910 | 5.036 | 8.649 | 2.451 | 3.735 |
| P-value |
| <0.001 | 0.008 | <0.001 | 0.090 | 0.026 |
Analysis of risk factors for CHD
BMI>25 was considered as obesity, and logistic
regression analysis was performed on the factors with statistically
significant difference used as independent variables. The results
of univariate analysis showed that CHD was associated with Hcy,
hyperlipidemia, smoking, hypertension and diabetes (P<0.05), but
had no relationship with drinking and obesity (P>0.05). The
results of multivariate analysis showed that Hcy, hyperlipidemia,
hypertension and diabetes were independent risk factors for CHD,
and the difference was statistically significant (P<0.05).
Specific information is shown in Tables
IV and V.
 | Table IV.Univariate analysis of risk factors
for CHD. |
Table IV.
Univariate analysis of risk factors
for CHD.
|
| OR | 95% CI | P-value |
|---|
| Smoking | 1.463 | 1.064–2.013 | 0.031 |
| Drinking | 1.389 | 1.042–1.852 | 0.076 |
| Hypertension | 0.871 | 0.672–1.130 | 0.035 |
| Diabetes | 0.457 | 0.261–0.801 | 0.029 |
| Obesity | 0.192 | 0.056–0.661 | 0.054 |
| Hyperlipidemia | 0.893 | 0.772–1.108 | 0.027 |
| Hcy | 1.814 | 0.925–3.558 | 0.002 |
 | Table V.Multivariate analysis of risk factors
for CHD. |
Table V.
Multivariate analysis of risk factors
for CHD.
|
| OR | 95% CI | P-value |
|---|
| Smoking | 1.356 | 1.064–2.013 | 0.064 |
| Hypertension | 0.843 | 0.776–1.130 | 0.028 |
| Diabetes | 0.352 | 0.261–0.504 | 0.031 |
| Hyperlipidemia | 0.759 | 0.634–1.034 | 0.023 |
| Hcy | 1.736 | 0.925–3.687 | 0.022 |
Discussion
CHD is more common and even fatal in middle-aged and
elderly people, the main pathological manifestation of which is
cardiac insufficiency. Cardiac insufficiency is due to the coronary
atherosclerotic plaque causing stenosis and blockage of arteries,
thus inducing other clinical manifestations (12). A large number of previous reports
have shown that the cholesterol level is associated with heart
disease. However, in recent years, studies have shown that Hcy is
an independent risk factor for CHD (13,14). The
specific reason is not clear why Hcy and blood lipid levels in
serum are associated with CHD risk, but it has proved that CHD risk
increases with the increase of Hcy and blood lipid levels in serum
(15).
This study compared Hcy and blood lipid levels in
serum between the study and control group. The HDL-C level in the
study group was significantly lower than that in control group,
while the levels of Hcy, TC, TG and LDL-C were significantly higher
than that in control group, and the differences were statistically
significant (P<0.001). The study of Granberry et al
(16) was consistent with our
results that HDL-C had the effect of preventing atherosclerosis.
Generally, the decrease of HDL-C level in CHD patients may be the
result of the decrease of HDL-C content contributing to lipid
deposition in the inner wall of the vessel, leading to the
occurrence of CHD (17,18). The difference was not statistically
significant in the HDL-C level in patients among angina pectoris,
acute myocardial infarction and old myocardial infarction group
(P>0.05), but the differences were statistically significant in
the levels of Hcy, TC, TG and LDL-C in serum of patients among
angina pectoris, acute myocardial infarction and old myocardial
infarction group (P<0.05). The differences were statistically
significant in the levels of Hcy, TC, TG and LDL-C between acute
and old myocardial infarction and angina pectoris group
(P<0.05), and the differences were statistically significant in
the levels of Hcy, TC, TG and LDL-C between old and acute
myocardial infarction group (P<0.05). The study of Christensen
et al (19) was consistent
with our results, among which the Hcy level in patients in acute
myocardial infarction group was significantly higher than that in
the other two groups, suggesting that the cause of myocardial
infarction in patients may be the increase of Hcy contributing to
occurrence of thrombosis (20).
Analysis of risk factors for the disease was
performed using logistic regression. The results of univariate
analysis showed that CHD was associated with Hcy, hyperlipidemia,
smoking, hypertension and diabetes (P<0.05), but had no
relationship with drinking and obesity (P>0.05). The results of
multivariate analysis showed that Hcy, hyperlipidemia, hypertension
and diabetes were independent risk factors for CHD, and the
difference was statistically significant (P<0.05). Our results
are very similar to that of Menezes et al (21). According to statistics, smoking is
associated with the death of CHD and is a significant risk factor
for early onset of CHD, and especially the younger the smoker is,
the greater the risk is (22). This
is because long-term smoking speeds up the oxidation of LDL-C,
resulting in decreased antioxidant capacity and dysfunction of
blood vessel endothelium (23).
Studies have shown that the incidence of CHD in hypertensive
patients with high diastolic blood pressure is 5 times higher than
that in patients with low diastolic blood pressure. About 70% of
patients with type II diabetes die of CHD, the most important risk
factor is dyslipidemia. In addition to some uncontrollable risk
factors such as sex, age and genetic factors, people should
actively control and cooperate to improve these variable risk
factors (24,25).
In conclusion, the Hcy level increases and the HDL-C
level decreases in serum of CHD patients. Hcy, hyperlipidemia,
hypertension and diabetes are independent risk factors for CHD,
which can provide reference for the assessment of the disease and
for the early prevention and treatment.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the present
study are available from the corresponding author on reasonable
request.
Authors' contributions
WL drafted the manuscript. WL and TW were mainly
devoted to the determination of Hcy and blood lipid levels in
serum. PS and YZ was responsible for the statistical analysis. All
authors read and approved the final manuscript.
Ethics approval and consent to
participate
The study was approved by the Ethics Committee of
Weifang People's Hospital (Weifang, China). Signed informed
consents were obtained from the patients or the guardians.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Zhong Y, Wang N, Xu H, Hou X, Xu P and
Zhou Z: Ischemia-modified albumin in stable coronary
atherosclerotic heart disease: Clinical diagnosis and risk
stratification. Coron Artery Dis. 23:538–541. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Su Z, Zhang S, Hou Y, Zhang L, Liao L, Xia
Q, Xiao C, Meng H and Yan Y: A preliminary study of single
nucleotide polymorphisms of lipoprotein lipase gene in coronary
atherosclerotic heart disease. Zhonghua Yi Xue Yi Chuan Xue Za Zhi.
17:157–160. 2000.PubMed/NCBI
|
|
3
|
Lyu Y, Jiang X and Dai W: The roles of a
novel inflammatory neopterin in subjects with coronary
atherosclerotic heart disease. Int Immunopharmacol. 24:169–172.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Ozkan Y, Ozkan E and Simşek B: Plasma
total homocysteine and cysteine levels as cardiovascular risk
factors in coronary heart disease. Int J Cardiol. 82:269–277. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Mayer O Jr, Simon J, Holubec L, Pikner R,
Vobrubová I and Trefil L: Fibrate treatment and prevalence risk of
mild hyperhomocysteinaemia in clinical coronary heart disease
patients. Eur J Cardiovasc Prev Rehabil. 11:244–249. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Naureen A, Munazza B, Shaheen R, Khan SA
and Fatima F: Serum homocysteine as a risk factor for coronary
heart disease. J Ayub Med Coll Abbottabad. 24:59–62.
2012.PubMed/NCBI
|
|
7
|
Wang P, Liu J, Lv X, Liu Y, Zhao Y and Guo
W: A naphthalimide-based glyoxal hydrazone for selective
fluorescence turn-on sensing of Cys and Hcy. Org Lett. 14:520–523.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Nabipour I, Vahdat K, Jafari SM, Amiri M,
Shafeiae E, Riazi A, Amini AL, Pazoki R and Sanjdideh Z:
Correlation of hyperhomocysteinaemia and Chlamydia
pneumoniae IgG seropositivity with coronary artery disease in a
general population. Heart Lung Circ. 16:416–422. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Sainani GS and Sainani R: Homocysteine and
its role in the pathogenesis of atherosclerotic vascular disease. J
Assoc Physicians India. 50 Suppl:16–23. 2002.PubMed/NCBI
|
|
10
|
Zhang HJ, Han P, Sun SY, Wang LY, Yan B,
Zhang JH, Zhang W, Yang SY and Li XJ: Attenuated associations
between increasing BMI and unfavorable lipid profiles in Chinese
Buddhist vegetarians. Asia Pac J Clin Nutr. 22:249–256.
2013.PubMed/NCBI
|
|
11
|
Sierakowska-Fijalek A, Kaczmarek P, Pokoca
L, Smorag I, Wosik-Erenbek M and Baj Z: Homocystein serum levels
and lipid parameters in children with atherosclerosis risk factors.
Pol Merkur Lekarski. 22:146–149. 2007.(In Polish). PubMed/NCBI
|
|
12
|
Wenger NK, Shaw LJ and Vaccarino V:
Coronary heart disease in women: Update 2008. Clin Pharmacol Ther.
83:37–51. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Aronow WS: Association between plasma
homocysteine and vascular atherosclerotic disease in older persons.
Prev Cardiol. 3:89–91. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Doncheva N, Penkov A, Velcheva A, Boev M,
Popov B and Niagolov Y: Study of homocysteine concentration in
coronary heart disease patients and comparison of two determination
methods. Ann Nutr Metab. 51:82–87. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Isaacs A, Willems SM, Bos D, Dehghan A,
Hofman A, Ikram MA, Uitterlinden AG, Oostra BA, Franco OH, Witteman
JC, et al: Risk scores of common genetic variants for lipid levels
influence atherosclerosis and incident coronary heart disease.
Arterioscler Thromb Vasc Biol. 33:2233–2239. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Granberry MC, Smith ES III and Talley JD:
Raising HDL-C to prevent atherosclerotic events. J Ark Med Soc.
96:378–379. 2000.PubMed/NCBI
|
|
17
|
Asztalos BF, Roheim PS, Milani RL, Lefevre
M, McNamara JR, Horvath KV and Schaefer EJ: Distribution of
ApoA-I-containing HDL subpopulations in patients with coronary
heart disease. Arterioscler Thromb Vasc Biol. 20:2670–2676. 2000.
View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Paavola T, Kangas-Kontio T, Salonurmi T,
Kuusisto S, Huusko T, Savolainen MJ and Kakko S: Plasma levels of
antibodies against oxidized LDL are inherited but not associated
with HDL-cholesterol level in families with early coronary heart
disease. Atherosclerosis. 224:123–128. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Christensen B, Landaas S, Stensvold I,
Djurovic S, Retterstøl L, Ringstad J, Berg K and Thelle DS: Whole
blood folate, homocysteine in serum, and risk of first acute
myocardial infarction. Atherosclerosis. 147:317–326. 1999.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Huang T, Yuan G, Zhang Z, Zou Z and Li D:
Cardiovascular pathogenesis in hyperhomocysteinemia. Asia Pac J
Clin Nutr. 17:8–16. 2008.PubMed/NCBI
|
|
21
|
Menezes AR, Lavie CJ, Milani RV, Arena RA
and Church TS: Cardiac rehabilitation and exercise therapy in the
elderly: Should we invest in the aged? J Geriatr Cardiol. 9:68–75.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Bruce IN: ‘Not only…but also’: Factors
that contribute to accelerated atherosclerosis and premature
coronary heart disease in systemic lupus erythematosus.
Rheumatology (Oxford). 44:1492–1502. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Lynch J, Davey Smith G, Harper S and
Bainbridge K: Explaining the social gradient in coronary heart
disease: Comparing relative and absolute risk approaches. J
Epidemiol Community Health. 60:436–441. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Marijon E, Trinquart L, Jani D, Jourdier
H, Garbarz E, Mocumbi AO, Celermajer DS and Ferreira B: Coronary
heart disease and associated risk factors in sub-Saharan Africans.
J Hum Hypertens. 21:411–414. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Maas AH, van der Schouw YT, Beijerinck D,
Deurenberg JJ, Mali WP and van der Graaf Y: Arterial calcifications
seen on mammograms: Cardiovascular risk factors, pregnancy, and
lactation. Radiology. 240:33–38. 2006. View Article : Google Scholar : PubMed/NCBI
|