Introduction
Glaucoma is a leading cause of irreversible
blindness worldwide (1) and retinal
ganglion cell (RGC) degeneration is a major pathogenic
characteristic of glaucoma (2,3).
Furthermore, a number of magnetic resonance imaging (MRI) studies
have reported that glaucomatous damage only affects RGCs in the
eyes, but also extends across the central visual pathway, then
further affecting the optic tract, lateral geniculate nucleus (LGN)
and the optic radiation (4–8). Using high-resolution 7.0-T MRI, Lee
et al (4) identified that the
LGN volumes are significantly smaller in primary open-angle
glaucoma (POAG) patients compared with those in healthy subjects. A
similar MRI study by Chen et al (5) confirmed this result and further
indicated that the LGN atrophy is consistent with the damage of the
optic disc in POAG patients. Besides LGN atrophy, the fractional
anisotropy (FA) of POAG patients also exhibited significant
alterations, the degree of which was closely correlated with the
disease severity, indicating that the atrophy of the visual cortex
may be an important diagnostic index for POAG and may be utilized
to guide its treatment (6,7). In addition, radiological evidence of
neurodegeneration in the optic tract and optic radiation of POAG
patients was provided, and this neurodegeneration was associated
with the damage of the optic disc and the loss of visual function
(8). Thus, radiological studies of
POAG patients have yielded novel insight into the pathophysiology
of glaucoma. Another previous study has also confirmed that modern
MRI may be an effective and non-invasive tool for assessing the
extent of glaucomatous progression within the central nervous
system and provide complementary indicators of disease severity
(9). However, it has remained
elusive whether diffusion tensor imaging (DTI) parameters of
cortical nerve fibers and LGN size determined by MRI may be used as
sensitive and reliable indicators for distinguishing patients with
glaucoma from healthy subjects. Therefore, the aim of the present
study was to evaluate the diagnostic value of changes in DTI
parameters of the central visual pathway and in the size of the LGN
for differentiating glaucomatous eyes from healthy eyes, and to
determine the sensitivity and specificity (diagnostic power) of
these indicators in discriminating between severe glaucoma and mild
to moderate glaucoma.
Materials and methods
Study subjects
The present study was approved by the Ethics
Committee of Tongji Hospital (Tongji Medical College, Huazhong
University of Science and Technology, Wuhan, China) and performed
in accordance with the Declaration of Helsinki. Written informed
consent was obtained from each subject prior to the start of the
study.
The present study was performed at Tongji Hospital
between April 2016 and March 2017. A total of 24 patients with POAG
(age, 34.29±10.69 years; males/females, 19/5) and 24 age- and
sex-matched non-glaucomatous healthy controls (age, 34.38±11.17
years; males/females, 19/5) were recruited for the present
observational study. All of the study subjects underwent
comprehensive ophthalmological examinations, including best
corrected visual acuity, slit-lamp microscopy and indirect
ophthalmoscope examination, intraocular pressure (IOP) measurement,
anterior chamber angle examination using gonioscopy, visual field
test (Octopus perimeter), central corneal thickness, axial length
and retinal nerve fiber layer (RNFL) thickness (Heidelberg spectral
domain optical coherence tomography) measurements (5–8).
Subjects were included in the POAG group according to the following
selection criteria: i) The subject was ≥18 years of age; ii) a
cup-to-disc (C/D) ratio ≥0.6, or an interocular C/D ratio
difference of ≥0.2; iii) presence of an RNFL defect; iv)
glaucomatous visual field defects corresponding to optic nerve
changes and v) normal anterior chamber depth with an open angle.
Patients who had undergone prior ocular surgeries, had a history of
eye disease (except for POAG) or those with any neurological
diseases were excluded from participation. Patients with systemic
diseases were also excluded. Subjects were included in the normal
group according to the following selection criteria: i) The subject
was aged ≥18 years; ii) normal IOP and fundus; iii) no significant
RNFL defect; iv) normal visual field and v) normal anterior chamber
depth with an open angle. Potential normal control subjects were
excluded from participation if they had a family history of
glaucoma, a history of ophthalmic or neurological disease or
surgery, or any systemic disease. According to a study by Mills
et al (10), the glaucomatous
eyes were stratified into six stages, from 0 to 5, for each patient
with POAG, after which the cumulative stage for the two eyes in
each patient was calculated. Patients with a cumulative stage of
>7 were assigned to the severe glaucoma group and all others
were categorized into the mild to moderate glaucoma group.
MRI methodology
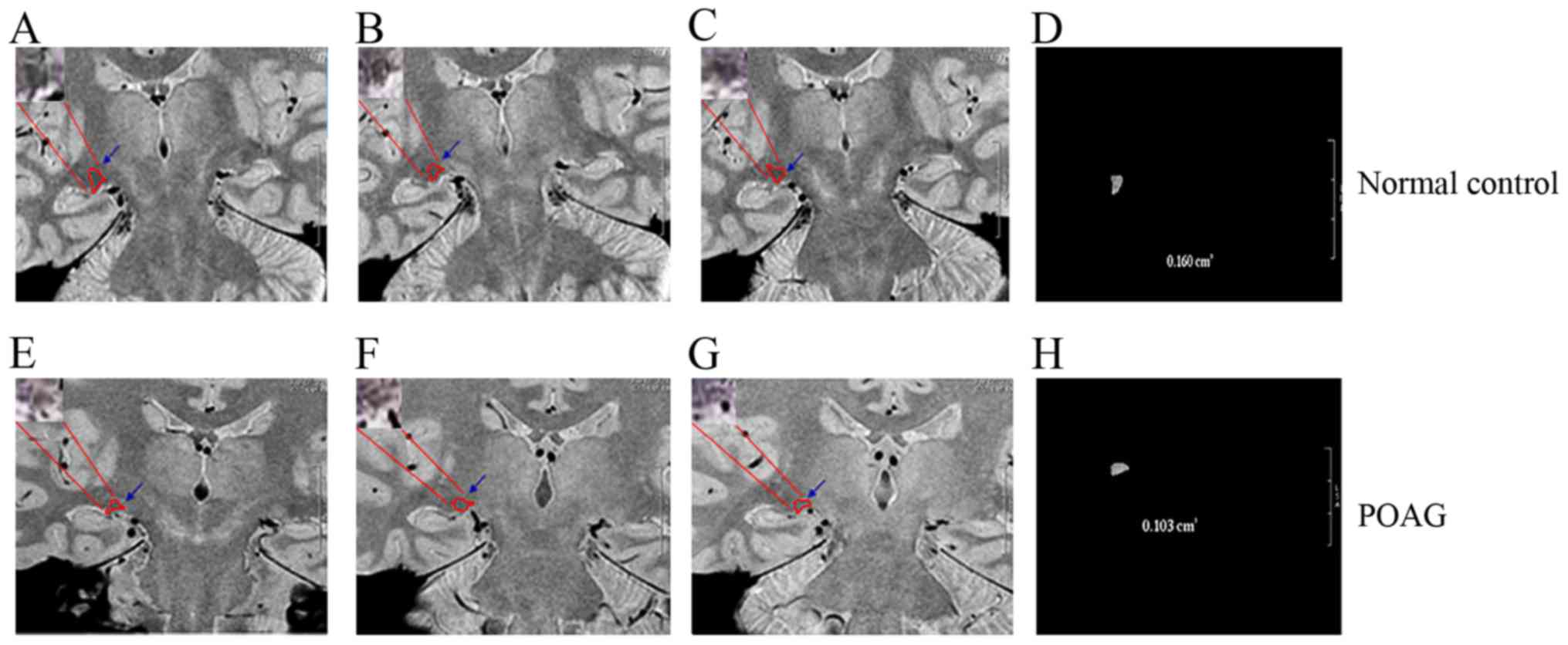
In accordance with previous studies (5,8), MRI was
performed within 7 days of the ophthalmological examinations. LGN
structural imaging (Fig. 1) and DTI
were performed using a 3.0 T General Electric MRI scanner (GE
Healthcare Life Sciences, Little Chalfont, UK) with an
eight-channel head coil. Three-dimensional-brain volume structural
imaging was performed with the following parameters: Echo time
(TE)=3.5 msec; repetition time (TR)=6.8 msec; inversion time=380
msec; slice thickness=1 mm with no gap; matrix=256×256; field of
view (FOV)=256×256 mm2; and number of excitations
(NEX)=1. For the proton density sequences, the parameters were as
follows: TE=22 msec; TR=3,400 msec; slice thickness=1.8 mm without
any gap; matrix=320×320; FOV=256×256 mm2; and NEX=4. LGN
height and volume measurements were performed offline on an
Advantage workstation (AW 4.4; GE Healthcare, Little Chalfont, UK).
Single-shot echo planar diffusion-weighted imaging was performed
with a bmax=800 sec/mm2, as well as 30
non-colinear gradient-encoding directions and one volume without
diffusion gradients. Other acquisition parameters were as follows:
TR=13,000 msec; ET=69 msec; matrix=128×128 zero-filled to 256×256;
FOV=24×24 cm2; slice thickness=2 mm with no gap; and
NEX=2. Voxel-wise statistical analysis of FA volumes was performed
using tract-based spatial analysis. Volume of interest (VOI)
analysis was performed to investigate the associations between
changes in FA and mean diffusivity (MD). For this, the VOI masks
were based on the voxels where differences in FA were detected.
Subsequently, these VOI masks were back-projected onto the original
images of each subject, and the MD was calculated.
Statistical analysis
All statistical analyses were performed using SPSS
software v.19.0 (IBM Corp., Armonk, NY, USA). Values are expressed
as the mean ± standard deviation where applicable. Receiver
operating characteristic (ROC) curves were constructed to assess
the ability of each parameter to distinguish subjects with glaucoma
from healthy controls and to differentiate between those with mild
to moderate glaucoma and those with severe glaucoma. The area under
the ROC curve was used to summarize the diagnostic accuracy of each
parameter. Spearman's correlation analysis was used to determine
the correlations between changes in DTI parameters and LGN size in
the glaucoma group. P<0.05 was considered to indicate a
statistically significant difference.
Results
Subject characteristics
A total of 24 patients with POAG and 24 age- and
sex-matched non-glaucomatous controls were included in the
analysis. There were no significant differences in age (34.29±10.69
vs. 34.38±11.17 years; P=0.979), sex ratio (male/female, 19/5 vs.
19/5; P=1.000), axial length (24.94±1.19 vs. 24.87±0.55 mm;
P=0.714) and central corneal thickness (537.50±35.35 vs.
533.56±30.11 µm; P=0.558) between the POAG and normal control
groups. The mean defect of the visual filed in the POAG group was
significantly higher than that in the normal control group
(14.38±9.43 vs. 0.84±0.68; P<0.001) and the RNFL in the POAG
group was significantly thinner than that in the normal control
group (61.89±21.71 vs. 111.25±9.99 µm; P<0.001; Table I).
 | Table I.Characteristics of POAG and normal
subjects. |
Table I.
Characteristics of POAG and normal
subjects.
| Variable | POAG subjects | Normal subjects | P-value |
|---|
| Age (years) | 34.29±10.69 | 34.38±11.17 | 0.979 |
| Sex
(male/female) | 19/5 | 19/5 | 1.000 |
| AL (mm) | 24.94±1.19 | 24.87±0.55 | 0.714 |
| CCT (µm) | 537.50±35.35 | 533.56±30.11 | 0.558 |
| MD | 14.38±9.43 | 0.84±0.68 | <0.001 |
| RNFL thickness
(µm) | 61.89±21.71 | 111.25±9.99 | <0.001 |
Diagnostic value of MRI
parameters
A ROC curve was generated to reveal the diagnostic
accuracies of the various parameters in discriminating patients
with POAG from normal control subjects. As presented in Table II, FA values of the optic tract and
the LGN volume exhibited the highest sensitivity and specificity
(FA values of the optic tract, at a cutoff of ≤0.412, had a
sensitivity of 79.2% and a specificity of 89.6%; and the LGN
volume, at a cutoff of ≤128 mm3, had a sensitivity of
79.2% and a specificity of 93.7%) for identifying patients with
POAG.
 | Table II.ROC curves of the LGN size and DTI
parameters of the central visual pathway for discriminating between
the normal (n=24) and glaucoma (n=24) groups. |
Table II.
ROC curves of the LGN size and DTI
parameters of the central visual pathway for discriminating between
the normal (n=24) and glaucoma (n=24) groups.
| Parameter | AUC | P-value | Cut-off value | Sensitivity (%) | Specificity (%) |
|---|
| LGN height | 0.814 | <0.001 | 4.75 mm | 0.688 | 0.792 |
| LGN
volume | 0.915 | <0.001 | 128
mm3 | 0.792 | 0.937 |
| FA-OT | 0.931 | <0.001 | 0.412 | 0.792 | 0.896 |
| FA-OR | 0.879 | <0.001 | 0.599 | 0.896 | 0.687 |
| MD-OT | 0.207 | <0.001 | None | None | None |
| MD-OR | 0.235 | <0.001 | None | None | None |
The severe glaucoma group contained 12 patients in
total. For discriminating between mild to moderate glaucoma and
severe glaucoma, the MD (cutoff, ≤0.001528 mm2/s;
sensitivity, 87.5%; specificity, 58.3%) and FA (cutoff, ≤0.341;
sensitivity and specificity, 75.0%) values of the optic tract
exhibited the highest sensitivity and specificity (Table III).
 | Table III.ROC curves of the LGN size and DTI
parameters of the central visual pathway for distinguishing the
severe glaucoma group (n=12) from the mild to moderate glaucoma
group (n=12). |
Table III.
ROC curves of the LGN size and DTI
parameters of the central visual pathway for distinguishing the
severe glaucoma group (n=12) from the mild to moderate glaucoma
group (n=12).
| Parameter | AUC | P-value | Cutoff value | Sensitivity (%) | Specificity (%) |
|---|
| LGN
height | 0.682 | 0.030 | 3.95 mm | 0.875 | 0.417 |
| LGN
volume | 0.698 | 0.019 | 67
mm3 | 0.958 | 0.208 |
| FA-OT | 0.801 | <0.001 | 0.341 | 0.750 | 0.750 |
| FA-OR | 0.719 | 0.009 | 0.593 | 0.583 | 0.792 |
| MD-OT | 0.802 | <0.001 | 0.001528
mm2/sec | 0.875 | 0.583 |
| MD-OR | 0.589 | 0.293 | None | None | None |
Correlation between changes in DTI
parameters and LGC size
The correlations between changes in DTI parameters
and the LGN size in glaucoma are presented in Table IV. The FA values of the optic tract
and the optic radiation were significantly correlated with the
height (r=0.395 and 0.452, respectively; P=0.005 and 0.001
respectively) and volume (r=0.286 and 0.348, respectively, P=0.049
and 0.015, respectively) of the LGN, while the MD values were not
(all P>0.05).
 | Table IV.Correlations between changes in DTI
parameters of the central visual pathway and parameters of the LGN
size in glaucoma. |
Table IV.
Correlations between changes in DTI
parameters of the central visual pathway and parameters of the LGN
size in glaucoma.
|
| LGN height | LGN volume |
|---|
|
|
|
|
|---|
| Parameter | r value | P-value | r value | P-value |
|---|
| FA-OT | 0.395 | 0.005 | 0.286 | 0.049 |
| FA-OR | 0.452 | 0.001 | 0.348 | 0.015 |
| MD-OT | −0.250 | 0.087 | −0.217 | 0.139 |
| MD-OR | −0.041 | 0.781 | −0.174 | 0.238 |
Discussion
The earliest MRI study of structural abnormalities
in glaucoma was published by Kashiwagi et al (11) in 2004. However, the majority of
relevant studies has been published within the last 5 years. Most
studies have determined significant anatomical degeneration within
the optic nerve, optic tracts, optic chiasm, optic radiations and
LGN (12–14), and these results were confirmed by a
meta-analysis (15). However, few
studies have focused on the diagnostic value of changes in DTI
parameters of the central visual pathway and in LGN size in POAG.
In a DTI study, Sidek et al (16) demonstrated that the FA of the optic
nerve had a high sensitivity and specificity in distinguishing mild
glaucoma from severe glaucoma. However, to date, how LGN height and
volume are associated with optic fiber changes has remained
elusive. Therefore, the present study aimed to provide this
information in order to improve the understanding of the
pathophysiological characteristics of glaucoma.
In the present study, the utility of changes in DTI
parameters of the central visual pathway and in LGN size for
diagnosing POAG was evaluated. It was observed that, among the
parameters determined, FA values of the optic tract had the highest
sensitivity and specificity, and were reliable biomarkers for
glaucoma evaluation. Furthermore, the FA values of the optic tract
and optic radiation exhibited significant correlations with LGN
size, providing novel insight into the central damage involved in
glaucoma.
For distinguishing glaucomatous eyes from healthy
eyes, measurements of the FA value of the optic tract and of the
LGN volume exhibited the highest sensitivity and specificity, with
cutoff values of ≤0.412 and ≤128 mm3, respectively.
Furthermore, for discriminating severe glaucoma from mild to
moderate glaucoma, the MD and FA values of the optic tract
exhibited the highest sensitivity and specificity. In the
evaluation of the central visual pathway based on DTI parameters
and LGN size, the FA of the optic tract was identified as the most
reliable and useful indicator for the clinical evaluation of
glaucoma. This result is in line with the results of previous
studies, indicating that FA may be more sensitive to glaucomatous
changes and may be an indicator of glaucomatous severity (9,16). From
a pathological viewpoint, these results imply that histological
lesions of the optic tract in glaucoma may be more marked compared
with LGN and optic radiation changes.
The correlation analysis performed to assess the
link between changes in the DTI parameters and LGN size revealed
that the FA values of the optic tract and optic radiation varied
consistently with the LGN size, indicating that certain
pathological features of central nervous system injury are
associated with POAG. To understand the reasons for these
correlations, it should be considered that the optic tract
represents the nerve endings of the RGCs in the retina, while the
optic radiation consists of the axons of LGN neurons; glaucoma is
characterized by the loss of RGCs, and the loss of LGN neurons has
also been indicated in pathological analyses of the brain in humans
and experimental primates with glaucoma (17,18).
Thus, the loss of the neuron soma also leads to fiber damage,
accounting for the abovementioned correlations. However, in terms
of the MD values, these exhibited no significant correlations. This
implies that the different MR signals (FA and MD of DTI) may
reflect different histological types of fiber damage (19,20), and
that, in the cohort of the present study, fiber damage may not have
led to sufficiently marked changes in MD values. However, this
hypothesis should be verified in further studies. The present
results also support that in DTI studies, the FA may have the
highest diagnostic value for identifying glaucoma.
LGN may serve a role in the function of perception
and cognition of humans, including visual attention and awareness
(21). Information on the LGN is
important for understanding glaucoma-associated perception and
cognition damage for future studies. The LGN scan and morphological
measurements from MRI scans are simple, but the slice thickness of
such a scan is 1.8 mm, while the diameter of a normal LGN is 4–5
mm, which may result in information dropout when examining the LGN.
Furthermore, the manual delineation of the LGN may also lead to
errors. Therefore, the methods used for determining the size of the
LGN require further improvement. DTI is a sensitive MR technique
that may detect microstructural changes in white matter (22). Compared with LGN measurements by MRI,
DTI scanning is time-consuming and requires more elaborate data
processing; however, it is more efficient as a diagnostic tool,
particularly in terms of the measurement of FA of the optic tract.
In addition, RGC axonal deficits in glaucoma appear to progress in
a distal to proximal manner (23);
thus, analysis of the FA value of the optic tract, which is the
fiber ending of the RGCs, may facilitate an earlier diagnosis of
glaucoma.
A limitation of the present study is that the study
population was relatively small. This may have affected the
statistical power, particularly in determining parameter
sensitivity and specificity in discriminating severe glaucoma.
Furthermore, older age has been significantly associated with POAG,
but in the present study, most participants were under 50 years of
age, which may have led to an age-associated bias. However, a
previous MRI study (24) reported
that in healthy volunteers, the FA and the MD of the bilateral
optic radiation and the bilateral optic nerve had no obvious
correlations with age and exhibited no obvious differences between
males and females. In future studies, participants aged >50
years should be assessed. In addition, more biochemical experiments
should be performed to verify and support the role of FA values in
discriminating POAG patients from healthy individuals.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
ML and YS performed the research and wrote the
manuscript. MK and KM performed the data analysis. HZ and ZC
designed the study and revised the manuscript. All of the authors
read and approved the final manuscript.
Ethics approval and consent to
participate
This study was approved by the Ethics Committee of
Tongji Hospital, Huazhong University of Science and Technology
(Wuhan, China). Informed consent was obtained from each subject
prior to the start of the study.
Patient consent for publication
Patient consent for publication of the MRI images
was provided.
Competing interest
The authors declare that they have no competing
interests.
References
|
1
|
Flaxman SR, Bourne RRA, Resnikoff S,
Ackland P, Braithwaite T, Cicinelli MV, Das A, Jonas JB, Keeffe J,
Kempen JH, et al: Global causes of blindness and distance vision
impairment 1990–2020: A systematic review and meta-analysis. Lancet
Glob Health. 5:e1221–e1234. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Quigley HA, Dunkelberger GR and Green WR:
Retinal ganglion cell atrophy correlated with automated perimetry
in human eyes with glaucoma. Am J Ophthalmol. 107:453–464. 1989.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Urcola JH, Hernández M and Vecino E: Three
experimental glaucoma models in rats: Comparison of the effects of
intraocular pressure elevation on retinal ganglion cell size and
death. Exp Eye Res. 83:429–437. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Lee JY, Jeong HJ, Lee JH, Kim YJ, Kim EY,
Kim YY, Ryu T, Cho ZH and Kim YB: An investigation of lateral
geniculate nucleus volume in patients with primary open-angle
glaucoma using 7 tesla magnetic resonance imaging. Invest
Ophthalmol Vis Sci. 55:3468–3476. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Chen Z, Wang J, Lin F, Dai H, Mu K and
Zhang H: Correlation between lateral geniculate nucleus atrophy and
damage to the optic disc in glaucoma. J Neuroradiol. 40:281–287.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Lu P, Shi L, Du H, Xie B, Li C, Li S, Liu
T, Feng H and Wang J: Reduced white matter integrity in primary
open-angle glaucoma: A DTI study using tract-based spatial
statistics. J Neuroradiol. 40:89–93. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Tellouck L, Durieux M, Coupé P,
Cougnard-Grégoire A, Tellouck J, Tourdias T, Munsch F, Garrigues A,
Helmer C, Malet F, et al: Optic radiations microstructural changes
in glaucoma and association with severity: A study using
3Tesla-magnetic resonance diffusion tensor imaging. Invest
Ophthalmol Vis Sci. 57:6539–6547. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Chen Z, Lin F, Wang J, Li Z, Dai H, Mu K,
Ge J and Zhang H: Diffusion tensor magnetic resonance imaging
reveals visual pathway damage that correlates with clinical
severity in glaucoma. Clin Exp Ophthalmol. 41:43–49. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Garaci FG, Bolacchi F, Cerulli A, Melis M,
Spanò A, Cedrone C, Floris R, Simonetti G and Nucci C: Optic nerve
and optic radiation neurodegeneration in patients with glaucoma: In
vivo analysis with 3-T diffusion-tensor MR imaging. Radiology.
252:496–501. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Mills RP, Budenz DL, Lee PP, Noecker RJ,
Walt JG, Siegartel LR, Evans SJ and Doyle JJ: Categorizing the
stage of glaucoma from pre-diagnosis to end-stage disease. Am J
Ophthalmol. 141:24–30. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Kashiwagi K, Okubo T and Tsukahara S:
Association of magnetic resonance imaging of anterior optic pathway
with glaucomatous visual field damage and optic disc cupping. J
Glaucoma. 13:189–195. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Chen WW, Wang N, Cai S, Fang Z, Yu M, Wu
Q, Tang L, Guo B, Feng Y, Jonas JB, et al: Structural brain
abnormalities in patients with primary open-angle glaucoma: A study
with 3T MR imaging. Invest Ophthalmol Vis Sci. 54:545–554. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Zhang YQ, Li J, Xu L, Zhang L, Wang ZC,
Yang H, Chen CX, Wu XS and Jonas JB: Anterior visual pathway
assessment by magnetic resonance imaging in normal-pressure
glaucoma. Acta Ophthalmol. 90:e295–e302. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Gupta N, Greenberg G, de Tilly LN, Gray B,
Polemidiotis M and Yücel YH: Atrophy of the lateral geniculate
nucleus in human glaucoma detected by magnetic resonance imaging.
Br J Ophthalmol. 93:56–60. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Li K, Lu C, Huang Y, Yuan L, Zeng D and Wu
K: Alteration of fractional anisotropy and mean diffusivity in
glaucoma: Novel results of a meta-analysis of diffusion tensor
imaging studies. PLoS One. 9:e974452014. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Sidek S, Ramli N, Rahmat K, Ramli NM,
Abdulrahman F and Tan LK: Glaucoma severity affects diffusion
tensor imaging (DTI) parameters of the optic nerve and optic
radiation. Eur J Radiol. 83:1437–1441. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Gupta N, Ang LC, Noël de Tilly L, Bidaisee
L and Yücel YH: Human glaucoma and neural degeneration in
intracranial optic nerve, lateral geniculate nucleus, and visual
cortex. Br J Ophthalmol. 90:674–678. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Sasaoka M, Nakamura K, Shimazawa M, Ito Y,
Araie M and Hara H: Changes in visual fields and lateral geniculate
nucleus in monkey laser-induced high intraocular pressure model.
Exp Eye Res. 86:770–782. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Nair SR, Tan LK, Mohd Ramli N, Lim SY,
Rahmat K and Mohd Nor H: A decision tree for differentiating
multiple system atrophy from Parkinson's disease using 3-T MR
imaging. Eur Radiol. 23:1459–1466. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Khong PL, Zhou LJ, Ooi GC, Chung BH,
Cheung RT and Wong VC: The evaluation of Wallerian degeneration in
chronic paediatric middle cerebral artery infarction using
diffusion tensor MR imaging. Cerebrovasc Dis. 18:240–247. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Kastner S, Schneider KA and Wunderlich K:
Beyond a relay nucleus: Neuroimaging views on the human LGN. Prog
Brain Res. 155:125–143. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Basser PJ, Mattiello J and LeBihan D:
Estimation of the effective self-diffusion tensor from the NMR spin
echo. J Magn Reson B. 103:247–254. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Crish SD, Sappington RM, Inman DM, Horner
PJ and Calkins DJ: Distal axonopathy with structural persistence in
glaucomatous neurodegeneration. Proc Natl Acad Sci USA.
107:5196–5201. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Sun HH, Wang D, Zhang QJ, Bai ZL and He P:
Magnetic resonance diffusion tensor imaging of optic nerve and
optic radiation in healthy adults at 3T. Int J Ophthalmol.
6:868–872. 2013.PubMed/NCBI
|