Introduction
Patients with episodes of angina are likely to
experience cardiac events in the next two years (1) and benefit from undergoing a
revascularization procedure (2).
Clinical research is required to be performed to improve the
assessment of the cause of chest pain in patients with suspected
angina to reduce the risk of cardiovascular events (3). At present, misdiagnosis occurs
frequently; for instance, individuals presenting with chest pain
diagnosed with non-cardiac conditions account for one-third of
cases diagnosed with cardiovascular disease in the follow-up time
(false-negative diagnosis of angina) (4). Therefore, diagnosis and risk
assessments require improvements to be reduce the rate of false
negative diagnosis (5).
In general, any patient referred to a cardiologist
with complaints of chest pain is subjected to 12-lead
electrocardiogram (ECG) to detect the possible presence of angina
(6). Further diagnostic assessment
includes exercise ECG (7). In
addition, conventional invasive coronary angiography is a
well-established and reliable method for the detection of angina
due to coronary heart disease, but this method is not recommended
in such patients due to contraindications, including access site
problems, severe allergies to intravenous contrast agents,
myocardial infarction, arrhythmia and stroke (8).
National Institute for Health and Care Excellence
clinical guidelines recommend the use of Computed Tomography
Coronary Angiography (CTCA) for acute chest pain (9). For the detection of coronary cardiac
disease(s), considering invasive coronary angiography is the
reference standard, CTCA has >95% specificity, >85%
sensitivity and acceptable positive (range, >93 and 81%) and
negative predictive rates (range, <2 and 9%) (8). Individuals with an arrhythmia, obesity
and/or coronary calcification, the image quality in CTCA is poor
(10). CTCA is associated with a
high radiation (20 mSv) exposure, which may induce cancer. Although
the radiation dose may be reduced to 2 mSv, a reduction of the
radiation dose always hampers the image quality (11). The diagnostic cost and duration of
hospital stay for an individual receiving CTCA are less than those
of the ‘standard diagnostic procedure’ (12). However, due to limited availability
of trained hospital staff and medical equipment at the Beijing
Anzhen Hospital, Capital Medical University (Beijing, China), it is
challenging to offer CTCA to all patients according to the National
Institute for Health and Care Excellence clinical guidelines.
The primary aim of the present study was to compare
the detection of angina due to coronary heart disease using CTCA
(CTCA and coronary artery calcium scoring) with the ‘standard
diagnostic procedure’ (clinical assessments, ECG and exercise ECG)
in Chinese patients with chest pain referred to the rapid access
chest pain clinic of Beijing Anzhen Hospital, Capital Medical
University (Beijing, China). The secondary endpoint of the study
was to investigate the sensitivity and accuracy of CTCA with regard
to the ‘standard diagnostic procedure’ at a level of evidence of 3
without any conflict of interest.
Materials and methods
Ethical approval and consent to
participate
The present study was registered in the research
registry (www.researchregistry.com; unique identifying no. 4232;
date, 11 January 2016). The protocol (no. BAH/CL/01/16 dated 15
December 2015) was approved by the review board of Beijing Anzhen
Hospital (Beijing, China). An informed consent form regarding
radiological images, pathology, clinical assessments and
publication of patient data and personal images (if any) in all
formats (hard copy and/or electronic format) irrespective of time
and language had been signed by all patients enrolled or their
relatives (legally authorized guardian). The present study adhered
to the law of China, the Standards for the Reporting of Diagnostic
Accuracy Studies (STARD) guidelines from 2015 (13) and the 2013 version of the Declaration
of Helsinki (14).
Inclusion criteria
Patients aged ≥18 years were included in the current
study if written informed consent was provided. Each patient
completed a patient information sheet on arrival at the hospital
(15). On the basis of the
information provided, patients with chest pain and suspected angina
due to coronary heart disease(s), referred (by medical officer of
emergency department and/or whole-body check-up department) to the
rapid access chest pain clinic of Beijing Anzhen Hospital, Capital
Medical University (Beijing, China) between 18 January 2016 and 1
December 2017, were included in the study. Demographic
characteristics of all of the enrolled patients are provided in
Table I.
 | Table I.Demographic characteristics of the
subjects (n=2,426). |
Table I.
Demographic characteristics of the
subjects (n=2,426).
| Characteristics | Value |
|---|
| Age (years) | 63.36±10.55 |
| Gender |
|
| Male | 1,457 (60) |
|
Female | 969 (40) |
| Smoking |
|
|
Currently | 480 (20) |
|
Previously | 505 (21) |
| Duration of chest
pain (months) |
|
|
<1 | 1,189 (49) |
| 1–6 | 775 (32) |
| 6–12 | 265 (11) |
|
>12 | 197 (8) |
| Body height (cm) | 161.09±3.89 |
| Body weight
(kg) | 61.02±4.54 |
| Body mass index
(kg/m2) | 23.55±2.1 |
| Arthritis | 218 (9) |
| Chronic obstructive
pulmonary disease and/or asthma | 314 (13) |
| Neuro and/or
psychological deficits | 194 (8) |
| Cancer | 72 (3) |
| Abnormality in the
gastrointestinal tract | 96 (4) |
| Family history of
angina due to coronary heart disease | 479 (19) |
| Rural
residence | 602 (25) |
| Income
quintile |
|
| 1
(lowest) | 698 (29) |
| 2
(low) | 612 (25) |
| 3
(moderate) | 545 (23) |
| 4
(high) | 491 (20) |
| 5
(highest) | 80 (3) |
Exclusion criteria
Patients who had refused to undergo CTCA, and those
with acute coronary syndrome (up to 100 days previously), chronic
kidney failure (or glomerular filtration rate ≤29.8 ml/min or serum
creatinine ≥251 µM/l) and female patients with pregnancies were
excluded from the current study. The patients who were greater than
the maximum height and weight range of the scanner were excluded
from the study. Patients with confirmed angina or high-density
lipoprotein (HDL) levels of <20 mg/dl and total cholesterol of
>600 mg/dl were excluded from the current study and subjected to
treatment directed by a cardiologist (16). Patients with gastroesophageal reflux,
gastroesophageal disease and diseases that are easily mistaken as
coronary heart disease were excluded from the study.
Experimental design
A total of 2,426 patients were included in the
present cross-sectional study. The STARD flow diagram of the study
is presented in Fig. 1. Patients had
undergone a clinical assessment with CTCA (16). At the rapid access chest pain clinic
of Beijing Anzhen Hospital, all patients were subjected to a normal
clinical assessment as outlined below subsequent to enrollment.
Clinical assessment
Determination of symptoms
Substernal chest pain provoked by emotional
stress/exertion and relieved by rest and/or nitroglycerin treatment
was defined as typical angina. Pain in the center of the chest that
was not associated with the heart, and accompanied with sleepiness,
weight gain, increased appetite, excessive sleep, mood changes,
fatigue and/or weakness, and that was not relieved by rest and/or
nitroglycerin was defined as atypical angina. Esophageal spasm pain
and/or cervical root compression pain that was relieved by rest
and/or nitroglycerin was defined as non-anginal pain (17).
The blood pressure was measured with a
sphygmomanometer (Omron 8712; Omron Healthcare, Jakarta,
Indonesia). Hypertension was defined as a diastolic blood pressure
of >90 mmHg and a systolic blood pressure of >140 mmHg
(18).
Blood tests
A blood sample was collected from all patients and
subjected to detection of total cholesterol, low-density
lipoprotein (LDL), HDL, blood serum creatinine, random plasma
glucose levels, hemoglobin, the percentage of glycated hemoglobin
(normal value, 6%) and troponin serum levels (normal value, 0.49
ng/ml) (16). Diabetes was defined
as random plasma glucose of >160 mg/dl. Hyperlipidemia was
defined as total cholesterol levels of >240 mg/dl, LDL of
>160 mg/dl and/or HDL of <40 mg/dl (18).
ECG
The chest, arms and lower legs were exposed and
electrodes were positioned, 12-lead ECG and exercised-ECG were
performed according to the Bruce protocol (16). If the heart was beating in a regular
sinus rhythm in the range of 60–100 (specifically 82) beats per
minute and waves and intervals had normal values [RR-interval,
0.6–1.2 sec; P-wave, 80 msec, PR-interval, 120–200 msec;
PR-segment, 50–120 msec; QRS-complex, 80–100 msec; ST segment,
80–120 msec; and T-wave, 160 msec (17)] were considered as normal ECG. The
Duke treadmill score was calculated according to the following
equation: Duke treadmill score=Exercise time-(5× ST segment
deviation in mm-(4× angina index score). Grading was performed
according to the Duke treadmill score with a score of ≥5 indicating
a low risk, −10 to +4 intermediate risk and ≤-11 high risk of
further cardiac events (19).
Coronary artery calcium score
All enrolled patients were subjected to a scan of
the heart by electron-beam CT (Philips Healthcare, Eindhoven, The
Netherlands). Radiological images were analyzed by experts
(radiologists with a minimum three years of experience in image
analysis) using Multi-Ethnic Study of Atherosclerosis software
(Collaborative Health Studies Coordinating Center, Seattle, WA,
USA) to determine the Agatston score and the presence of calcium
(18). The normal value of the
calcium score percentile with regard to age was estimated (Table II). The Agatston score and the
presence of calcium were interpreted by a radiologist (YH) who had
at least three years of experience.
 | Table II.Non-zero calcium score probability
estimation for a Chinese population. |
Table II.
Non-zero calcium score probability
estimation for a Chinese population.
|
| Males | Females |
|---|
|
|
|
|
|---|
| Age (years) | 25th | 50th | 75th | 90th | 25th | 50th | 75th | 90th |
|---|
| ≤45 | 0 | 0 | 3 | 50 | 0 | 0 | 0 | 0 |
| 46 | 0 | 0 | 4 | 56 | 0 | 0 | 0 | 0 |
| 47 | 0 | 0 | 6 | 63 | 0 | 0 | 0 | 0 |
| 48 | 0 | 0 | 8 | 71 | 0 | 0 | 0 | 2 |
| 49 | 0 | 0 | 11 | 80 | 0 | 0 | 0 | 6 |
| 50 | 0 | 0 | 14 | 89 | 0 | 0 | 0 | 12 |
| 51 | 0 | 0 | 17 | 98 | 0 | 0 | 0 | 17 |
| 52 | 0 | 0 | 21 | 110 | 0 | 0 | 0 | 23 |
| 53 | 0 | 0 | 25 | 124 | 0 | 0 | 0 | 30 |
| 54 | 0 | 0 | 29 | 136 | 0 | 0 | 1 | 38 |
| 55 | 0 | 0 | 34 | 150 | 0 | 0 | 2 | 47 |
| 56 | 0 | 0 | 38 | 163 | 0 | 0 | 5 | 57 |
| 57 | 0 | 0 | 43 | 176 | 0 | 0 | 7 | 66 |
| 58 | 0 | 1 | 49 | 194 | 0 | 0 | 10 | 77 |
| 59 | 0 | 3 | 58 | 215 | 0 | 0 | 14 | 90 |
| 60 | 0 | 5 | 67 | 242 | 0 | 0 | 18 | 105 |
| 61 | 0 | 7 | 279 | 273 | 0 | 0 | 23 | 122 |
| 62 | 0 | 10 | 91 | 304 | 0 | 0 | 28 | 144 |
| 63 | 0 | 13 | 102 | 329 | 0 | 0 | 34 | 160 |
| 64 | 0 | 15 | 112 | 350 | 0 | 0 | 39 | 178 |
| 65 | 0 | 18 | 121 | 372 | 0 | 0 | 45 | 194 |
| 66 | 0 | 21 | 132 | 397 | 0 | 0 | 51 | 211 |
| 67 | 0 | 24 | 143 | 427 | 0 | 0 | 55 | 220 |
| 68 | 0 | 28 | 154 | 450 | 0 | 2 | 59 | 229 |
| 69 | 0 | 32 | 166 | 470 | 0 | 3 | 64 | 235 |
| 70 | 0 | 34 | 174 | 487 | 0 | 5 | 70 | 243 |
| 71 | 0 | 37 | 183 | 503 | 0 | 7 | 76 | 262 |
| 72 | 0 | 40 | 191 | 522 | 0 | 9 | 83 | 276 |
| 73 | 1 | 45 | 201 | 546 | 0 | 11 | 89 | 287 |
| 74 | 2 | 49 | 216 | 570 | 0 | 13 | 96 | 300 |
| 75 | 3 | 53 | 229 | 599 | 0 | 16 | 103 | 314 |
| 76 | 5 | 58 | 241 | 629 | 0 | 18 | 111 | 332 |
| 77 | 6 | 63 | 254 | 659 | 0 | 22 | 119 | 347 |
| 78 | 8 | 70 | 273 | 695 | 0 | 25 | 128 | 361 |
| 79 | 9 | 75 | 288 | 735 | 0 | 28 | 137 | 377 |
| 80 | 11 | 81 | 305 | 769 | 0 | 32 | 146 | 398 |
| 81 | 13 | 88 | 325 | 808 | 2 | 35 | 158 | 416 |
| 82 | 15 | 95 | 344 | 855 | 3 | 40 | 167 | 436 |
| 83 | 18 | 103 | 369 | 913 | 5 | 44 | 177 | 456 |
| ≥84 | 20 | 112 | 391 | 971 | 6 | 50 | 190 | 483 |
CTCA
CTCA was performed using a 256-slice CT scanner
(Brilliance iCT; Philips Healthcare) by using the single
breath-hold protocol. Patients with a systolic blood pressure of
>110 mmHg and a heart rate of >60 beats/min received 0.5 mg
sublingual glyceryl trinitrate (Angised; Glaxo Smith Kline
Pharmaceuticals Ltd., Beijing, China) prior to CTCA (16). Coronary angiograms were interpreted
by clinicians (WZ, WL and SC) with at least three years of
experience using the scanner's workstation. In the case of a
disagreement between the clinicians, a consensus regarding the
revascularization procedure was reaching following an
interpretation by a cardiologist with at least three years of
experience. Significant stenosis and angina due to heart disease
were defined as per Table III
(20).
 | Table III.Interpretation of computed tomography
coronary angiography and coronary artery calcium score. |
Table III.
Interpretation of computed tomography
coronary angiography and coronary artery calcium score.
| Observation | Interpretation |
|---|
| Location | Degree of stenosis
(%) | Stenosis | Angina due to heart
disease |
|---|
| Luminal
cross-sectional area of at least 1 major epicardial vessel | <10 | Normal | No or minimal
coronary artery disease |
|
| 10–49 | Hemodynamically
insignificant | Non-obstructive
coronary artery disease/atherosclerotic plaque |
|
| 50–69 | Intermediate | Moderate
non-obstructive coronary artery disease/atherosclerotic plaque |
|
| ≥70 | Significant | Obstructive
coronary artery disease/atherosclerotic plaque |
| Left main stem | ≥50 | Significant | Mild
non-obstructive coronary artery disease/atherosclerotic plaque |
| Total/subtotal
occlusion | 100 | Significant | Obstructive
coronary artery disease/atherosclerotic plaque |
| Calcium score
>400 Agatston units | Inconclusive | Inconclusive | Non-obstructive
coronary artery disease/atherosclerotic plaque |
| Calcium score 90th
percentile for sex and age | Inconclusive | Inconclusive | Non-obstructive
coronary artery disease/atherosclerotic plaque |
The benefits score (the difference between the
possible benefit and the possible harm associated with each
procedure following the revascularization procedure) of diagnostic
modalities were evaluated by decision curve analysis according to
the following equation (21):
BS = AC − (BC XD1−D),
where BS is the benefit score of the adopted
diagnostic procedure for the detection of angina due to coronary
heart disease, A is the number of individuals with accurate
detection of angina, B is the number of individuals with no
accurate detection of angina, C is the total number of individuals
subjected to the procedure and D is the level of diagnostic
confidence; above this level, the revascularization procedure could
be recommended.
Cost
The cost of the diagnosis included the cost of
emergency department and/or whole-body check-up department
utilization, the cost of diagnostic modalities and pathology, and
expert charges (12).
Statistical analysis
InStat software (GraphPad Software Inc., La Jolla,
CA, USA) was used for statistical analysis. One-way analysis of
variance was performed to compare results and cost between the
‘standard diagnostic procedure’ and CTCA (22). Pearson correlation analysis
[considering the Pearson coefficient (r) in the range of
0.8543–0.8617 as significant] was performed to determine the
possible correlation between exercise ECG results and
interpretation of CTCA (23).
P<0.01 was considered to indicate statistical significance.
Results
Clinical assessment
In total, 776 patients (32%) were identified to be
abnormal on clinical assessment. According to anginal symptoms, 748
patients had non-anginal pain, 399 had typical angina and 988 had
atypical angina. By contrast, 12-lead ECG concluded that 401 (17%)
patients were abnormal. Exercised-ECG concluded that 356 (15%)
patients had a low risk, 266 (11%) patients had an intermediate
risk and 154 (6%) patients had a high risk of further cardiac
events (Table IV). A total of 1,420
patients (58%) were considered abnormal according to their coronary
artery calcium score and CTCA. CTCA concluded that 658 (27%)
patients had obstructive and 762 (31%) had non-obstructive coronary
artery disease (Table V). The
coronary artery calcium score and CTCA had a higher sensitivity
regarding the diagnosis of angina due to coronary heart disease
compared with the ‘standard diagnostic procedure’
(P<0.0001).
 | Table IV.Results of the standard diagnostic
procedure diagnostic procedure in the cohort (n=2,426). |
Table IV.
Results of the standard diagnostic
procedure diagnostic procedure in the cohort (n=2,426).
|
Characteristics | Value |
|---|
| Diabetesa | 515 (21) |
| Hypertensionb | 1,119 (46) |
|
Hyperlipidemiac | 848 (35) |
| Hemoglobin
(g/dl) | 13.88±1.89 |
| HbA1cd (%) | 6.15±1.31 |
| Serum creatininee
(µM/l) | 215.58±4.55 |
| Troponin serum
levelf (ng/ml) | 0.39±0.01 |
| Anginal
symptoms |
|
|
Non-anginal | 748 (31) |
|
Typical | 399 (16) |
|
Atypical | 988 (41) |
|
Inconclusive results | 291 (12) |
| 12 lead-ECG |
|
|
Normal | 1871 (77) |
|
Abnormal | 401 (17) |
|
Inconclusive results | 154 (6) |
| Exercise ECG |
|
|
Normalg | 1,551 (64) |
|
Abnormalh |
|
| Low
risk | 356 (15) |
|
Intermediate risk | 266 (11) |
| High
risk | 154 (6) |
|
Inconclusive results | 99 (4) |
 | Table V.Results of coronary artery calcium
score and computed tomography coronary angiography in the cohort
(n=2,426). |
Table V.
Results of coronary artery calcium
score and computed tomography coronary angiography in the cohort
(n=2,426).
| Characteristic | N (%) |
|---|
| Interpretation of
age- and sex-dependent coronary artery calcium score |
|
| No or
minimal coronary artery disease | 1,231 (51) |
|
Non-obstructive coronary
artery disease/atherosclerotic plaque | 1,195 (49) |
| Interpretation of
computed tomography coronary angiography |
|
| No or
minimal coronary artery disease | 1,006 (42) |
| Non-obstructive
coronary artery disease/atherosclerotic plaque |
|
|
Mild | 416 (17) |
|
Moderate | 346 (14) |
| Number of vessels
with obstructive coronary artery disease/atherosclerotic
plaque |
|
| 1 | 311 (13) |
| 2 | 241 (10) |
| 3 | 106 (4) |
| Other
cardiac-associated findings |
|
| Dilated
right atrium | 25 (1) |
| Aortic
valve calcification | 26 (1) |
| Left
ventricular wall thinning | 31 (1) |
| Mitral
valve calcification | 28 (1) |
| Left
ventricular hypertrophy | 33 (1) |
| Dilated
left ventricle | 35 (1) |
|
Hypertrophic obstructive | 46 (2) |
| Dilated
right ventricle | 47 (2) |
|
Cardiomyopathy | 25 (1) |
| Dilated
left atrium | 27 (1) |
| Non-cardiac
findings |
|
|
Parenchymal lung disease | 99 (4) |
| Liver
pathology | 27 (1) |
|
Pulmonary mass or nodule | 151 (6) |
|
Lymphadenopathy | 24 (1) |
|
Emphysema | 87 (4) |
|
Pulmonary embolism | 27 (1) |
| Hiatus
hernia | 25 (1) |
ECG results
The results of the 12-lead ECG were only considered
for patients with typical angina (Fig.
2), while for asymptomatic patients, ECGs were normal or did
not have any predictive value regarding angina (Fig. 3). The exercise ECG results were not
correlated with the interpretation of CTCA (r=0.8511; data not
shown).
 | Figure 2.12-leads electrocardiogram of a
patient with angina (age, 30 years). I, II, III, V1, V2, V3, V4, V5
and V6 are external leads. aVR, augmented vector right; aVL,
augmented vector left; aVF, augmented vector foot. |
 | Figure 3.12-leads electrocardiogram of an
asymptomatic patient (age, 32 years). The Sokolow index is in the
normal range. Normal regular sinus rhythm with hyperkalemia, which
caused left ventricular hypertrophy. No sign of angina. I, II, III,
V1, V2, V3, V4, V5 and V6 are external leads. aVR, augmented vector
right; aVL, augmented vector left; aVF, augmented vector foot. |
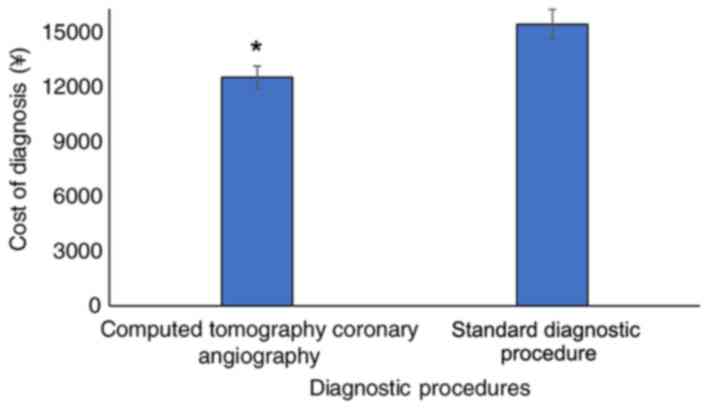
Cost
The cost of the ‘standard diagnostic procedure’ was
15,452±806 ¥/patient and that of CTCA with coronary artery calcium
scoring was 12,546±612 ¥/patient (Fig.
4).
The benefits score
The working area of the diagnosis that detected
angina due to coronary heart disease at one time among the adopted
diagnostic procedures was in the order of ECG <clinical
assessments <exercised ECG <coronary artery calcium score
<CTCA. Clinical assessment followed by 12-lead ECG and exercise
ECG had a level of confidence of only 5–35% for a revascularization
procedure and at >35%, there was a risk of overdiagnosis.
However, CTCA with the coronary artery calcium score had a level of
confidence of 5–64% for the revascularization procedure (Fig. 5).
Discussion
The present large-population study compares the use
of CTCA and the standard diagnostic procedure for diagnosing
patients presenting with chest pain with angina due to coronary
heart disease at an emergency unit specialized in Beijing Anzhen
Hospital, Capital Medical University. The standard diagnostic
procedure for the diagnosis is invasive and had more inconclusive
results (291 for anginal symptoms, 154 for ECG and 99 for exercise
ECG) than CTCA. If CTCA is unavailable to subjects with
inconclusive results of the standard diagnostic procedure for the
diagnosis of chest pain, the appropriate treatment is elusive and
the risk of cardiovascular events is increased (3,24). In
such cases, conventional CA may be performed; however, it is an
invasive procedure, with more complications and higher chances of a
false-negative diagnosis compared with CTCA (25). However, CTCA is a non-invasive method
of diagnosis and may be used to spare patients from further
stressful and invasive testing for angina (26). With respect to the results of CTCA,
it is a most desirable diagnostic modality for angina due to
coronary heart disease.
The present study analyzed the benefit of imaging
modalities by assessing anatomic testing vs. functional testing.
However, previous studies compare patient-centered and
clinician-centered outcomes (16,18,26).
Furthermore, certain studies reported on randomized controlled
trials adhering to the Consolidated Standards of Reporting Trials
guidelines with total populations sizes of 3,427 [sample size (n);
1,755 vs. 1,672; CTCA vs. standard diagnostic procedure] (1), 562 (n, 332 vs. 240) (12), 4,138 (n, 2,069 vs. 2,069) (16) and 4,146 (n, 2,073 vs. 2,073)
(26,27), and the studies were performed with
6-month follow-up periods with medication(s). Of note, in these
previous studies, the diagnostic methods were used for initial
diagnosis and diagnostic data were evaluated from a non-treatment
randomization design; however, it may not be possible to evaluate
the sensitivity and accuracy of any diagnostic method using two
groups, as the demographic parameters would be different between
the two groups, and randomization may only be appropriate for
treatment studies (28). If these
studies were still considered to be randomized trials, it may be
difficult to determine the phase, e.g. Phase I (on healthy
volunteers; sample size, 20–100), Phase II (diseased patients;
sample size, 100–300) or Phase III (diseased patients; sample size,
300–3,000) (29); according to the
sample size, these studies do not meet the criteria for any
randomized drug trial. Furthermore, the role of diagnostic
modalities in the initial diagnosis and during follow-up periods of
medication(s) is not clarified in these studies. With regard to the
design of the present study, the study provided an exact comparison
of CTCA and the ‘standard diagnostic procedure’ for the diagnosis
of angina due to coronary heart disease.
In 4% of subjects, the ECG results were
inconclusive. However, CTCA provided information on obstructive
(27%) and non-obstructive (31%) coronary artery disease, as also
reported previously (26). With
respect to the specificity of diagnostic modalities adopted by
clinicians for the diagnosis of patients with suspected angina, the
standard diagnostic procedure underestimated the possible risk of
cardiac events in patients with chest pain.
The cost of diagnosis using the standard diagnostic
procedure was higher than that of CTCA, as the former includes
clinical assessments, ECG and exercise ECG. Pathology includes
several types of tests, which are costly, time-consuming and
tedious. ECG is first-line test and international guidelines also
suggested this test for any possible angina due to heart diseases
(12). In consideration of cost
factors, exercise ECG increases the undesired financial burden on
low- and moderate-income patients.
Regarding the limitations of the present study, the
sensitivity and specificity of the diagnostic tests compared with a
reference standard (invasive CA) should have been assessed, which
is lacking in the present study. Without a reference standard, it
may be wrongly assumed that the best diagnostic test is the one
detecting the most anomalies in the population of the study.
Furthermore, it may not be appropriate to perform a head-to-head
comparison of CTCA, which exposes patients to radiation, with other
imaging modalities. In addition, the present study did not report
on cardiac events in the patients after diagnosis. The present
study has also not discussed the use of the diagnostic methods to
guide the selection of these drugs (β-blockers and/or glyceryl
trinitrate) in the follow-up period. The limited applicability of
coronary artery calcium score (45–84 years) is a further
limitation. The cost factor is not generalized and applies to the
P.R. China only. A huge number of patients arrived at the hospital
during the study period and were managed/treated by large number of
medical and paramedical staff; therefore, intra- and inter-observer
reliabilities are not granted. The study also lacks subgroup
analyses to identify any possible advantages of CTCA in patients
with typical or atypical chest pain.
The present study included 2,426 patients with chest
pain referred to the rapid access chest pain clinic of Beijing
Anzhen Hospital, Capital Medical University (Beijing, China). It
may be concluded that the diagnostic cost and the duration of the
hospital stay per individual are less for CTCA than those for the
‘standard diagnostic procedure’. The present study provided useful
information that may enhance the current knowledge regarding CTCA
and ‘standard diagnostic procedure’ for the diagnosis of angina due
to coronary heart disease. However, whether all chest pain patients
require CTCA examination remains controversial, particularly for
those with atypical chest pain. After all, the potential risk
associated with CTCA is higher than that of clinical assessments,
ECG and exercise ECG. Overall, the present study is of significance
for non-acute coronary syndrome patients presenting at chest pain
clinics, and may provide guidance on what diagnostic modality to
perform first, CTCA or ‘standard diagnostic procedure’.
In conclusion, according to the beneficial score
analysis curve, CTCA had a higher sensitivity for the diagnosis of
angina due to coronary heart disease and the cost was lower than of
the ‘standard diagnostic procedure’ diagnosis. Based on the results
of the present study, it may be recommended to only perform CTCA in
patients with suspected angina referred to a chest pain clinic and
to not subject them to the other stressful imaging modalities and
tedious pathological examination.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the present
study are available from the corresponding author on reasonable
request.
Authors' contributions
All authors read and approved the manuscript prior
to submission. ZW contributed to the design of the study and
project administration. YH contributed to data curation and formal
analysis. WL performed the statistical analysis. SC contributed to
data curation, and drafted, reviewed and edited the manuscript for
intellectual content.
Ethics approval and informed consent
The protocol of the present study (no. BAH/CL/01/16
dated 15 December 2015) was approved by the review board of Beijing
Anzhen Hospital (Beijing, China).
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Williams MC, Hunter A, Shah A, Assi V,
Lewis S, Mangion K, Berry C, Boon NA, Clark E, Flather M, et al:
Symptoms and quality of life in patients with suspected angina
undergoing CT coronary angiography: A randomised controlled trial.
Heart. 103:995–1001. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Bennell MC, Qiu F, Kingsbury KJ, Austin PC
and Wijeysundera HC: Determinants of variations in initial
treatment strategies for stable ischemic heart disease. CMAJ.
187:E317–E325. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Jordan KP, Timmis A, Croft P, van der
Windt DA, Denaxas S, González-Izquierdo A, Hayward RA, Perel P and
Hemingway H: Prognosis of undiagnosed chest pain: Linked electronic
health record cohort study. BMJ. 357:j11942017. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Sekhri N, Feder GS, Junghans C, Hemingway
H and Timmis AD: How effective are rapid access chest pain clinics?
Prognosis of incident angina and non-cardiac chest pain in 8762
consecutive patients. Heart. 93:458–463. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Boyle RM: Value of rapid-access chest pain
clinics. Heart. 93:415–416. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Parsonage WA, Cullen L and Younger JF: The
approach to patients with possible cardiac chest pain. Med J Aust.
199:30–34. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Nishimura RA, Otto CM, Bonow RO, Carabello
BA, Erwin JP III, Fleisher LA, Jneid H, Mack MJ, McLeod CJ, O'Gara
PT, et al: 2017 AHA/ACC focused update of the 2014 AHA/ACC
guideline for the management of patients with valvular heart
disease: A report of the American College of Cardiology/American
Heart Association Task Force on Clinical Practice Guidelines. J Am
Coll Cardiol. 70:252–289. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Sajjadieh A, Hekmatnia A, Keivani M,
Asoodeh A, Pourmoghaddas M and Sanei H: Diagnostic performance of
64-row coronary CT angiography in detecting significant stenosis as
compared with conventional invasive coronary angiography. ARYA
Atheroscler. 9:157–163. 2013.PubMed/NCBI
|
|
9
|
Dreisbach JG, Nicol ED, Roobottom CA,
Padley S and Roditi G: Challenges in delivering computed tomography
coronary angiography as the first-line test for stable chest pain.
Heart. 104:921–927. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Mowatt G, Cummins E, Waugh N, Walker S,
Cook J, Jia X, Hillis GS and Fraser C: Systematic review of the
clinical effectiveness and cost-effectiveness of 64-slice or higher
computed tomography angiography as an alternative to invasive
coronary angiography in the investigation of coronary artery
disease. Health Technol Assess. 12:iii–iv, ix-143. 2008. View Article : Google Scholar
|
|
11
|
Fuchs TA, Stehli J, Bull S, Dougoud S,
Clerc OF, Herzog BA, Buechel RR, Gaemperli O and Kaufmann PA:
Coronary computed tomography angiography with model-based iterative
reconstruction using a radiation exposure similar to chest X-ray
examination. Eur Heart J. 35:1131–1136. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Hamilton-Craig C, Fifoot A, Hansen M,
Pincus M, Chan J, Walters DL and Branch KR: Diagnostic performance
and cost of CT angiography versus stress ECG-a randomized
prospective study of suspected acute coronary syndrome chest pain
in the emergency department (CT-COMPARE). Int J Cardiol.
177:867–873. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Cohen JF, Korevaar DA, Altman DG, Bruns
DE, Gatsonis CA, Hooft L, Irwig L, Levine D, Reitsma JB, de Vet HCW
and Bossuyt PMM: STARD 2015 guidelines for reporting diagnostic
accuracy studies: Explanation and elaboration. BMJ Open.
6:e0127992016. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
World Medical Association: World medical
association declaration of helsinki: Ethical principles for medical
research involving human subjects. JAMA. 310:2191–2194. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Arnold J, Goodacre S, Bath P and Price J:
Information sheets for patients with acute chest pain: Randomised
controlled trial. BMJ. 338:b5412009. View
Article : Google Scholar : PubMed/NCBI
|
|
16
|
Newby DE, Williams MC, Flapan AD, Forbes
JF, Hargreaves AD, Leslie SJ, Lewis SC, McKillop G, McLean S, Reid
JH, et al: Role of multidetector computed tomography in the
diagnosis and management of patients attending the rapid access
chest pain clinic, The Scottish computed tomography of the heart
(SCOT-HEART) trial: Study protocol for randomized controlled trial.
Trials. 13:1842012. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Timmis A and Roobottom CA: National
institute for health and care excellence updates the stable chest
pain guideline with radical changes to the diagnostic paradigm.
Heart. 103:982–926. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Lennon SL, DellaValle DM, Rodder SG, Prest
M, Sinley RC, Hoy MK and Papoutsakis C: 2015 Evidence analysis
library evidence-based nutrition practice guideline for the
management of hypertension in adults. J Acad Nutr Diet.
117:1445–1458.e17. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Kim KH, Jeon KN, Kang MG, Ahn JH, Koh JS,
Park Y, Hwang SJ, Jeong YH, Kwak CH, Hwang JY and Park JR:
Prognostic value of computed tomographic coronary angiography and
exercise electrocardiography for cardiovascular events. Korean J
Intern Med. 31:880–890. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
National Institute for Health and Clinical
Excellence: Guidance: Chest pain of recent onset: Assessment and
diagnosis of recent onset chest pain or discomfort of suspected
cardiac origin [Internet]. National Clinical Guideline Centre for
Acute and Chronic Conditions (UK). London Royal College of
Physicians (UK); 2010
|
|
21
|
Fitzgerald M, Saville BR and Lewis RJ:
Decision curve analysis. JAMA. 313:409–410. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Blaha MJ, Budoff MJ, Tota-Maharaj R,
Dardari ZA, Wong ND, Kronmal RA, Eng J, Post WS, Blumenthal RS and
Nasir K: Improving the CAC score by addition of regional measures
of calcium distribution: Multi-ethnic study of atherosclerosis.
JACC Cardiovasc Imaging. 9:1407–1416. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
George RT, Arbab-Zadeh A, Miller JM,
Kitagawa K, Chang HJ, Bluemke DA, Becker L, Yousuf O, Texter J,
Lardo AC and Lima JA: Adenosine stress 64- and 256-row detector
computed tomography angiography and perfusion imaging: A pilot
study evaluating the transmural extent of perfusion abnormalities
to predict atherosclerosis causing myocardial ischemia. Circ
Cardiovasc Imaging. 2:174–182. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Holt T: Chest pain in primary care: What
happens to the undiagnosed majority? BMJ. 357:j16262017. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Xu Y, Tang L, Zhu X, Xu H, Tang J, Yang Z,
Wang L and Wang D: Comparison of dual-source CT coronary
angiography and conventional coronary angiography for detecting
coronary artery disease. Int J Cardiovasc Imaging. 26 (Suppl
1):S75–S81. 2010. View Article : Google Scholar
|
|
26
|
SCOT-HEART Investigators: CT coronary
angiography in patients with suspected angina due to coronary heart
disease (SCOT-HEART): An open-label, parallel-group, multicentre
trial. Lancet. 385:2383–2391. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Sabaté M and Ishida K: CT coronary
angiography increase diagnostic certainty in patients with stable
chest pain. Evid Based Med. 20:1872015. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Boutron I, Moher D, Altman DG, Schulz KF
and Ravaud P; CONSORT Group: Extending the CONSORT statement to
randomized trials of nonpharmacologic treatment: Explanation and
elaboration. Ann Intern Med. 148:295–309. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
US and Food and Drug Administration. Step
3. Clinical research. https://www.fda.gov/ForPatients/Approvals/Drugs/ucm405622.htm15–October.
2016
|