Introduction
Thromboembolism is a severe life-threatening disease
that comprises deep vein thrombosis and deep artery thrombosis and
is caused by vascular endothelial injury, platelet activation,
physiological coagulation processes, reduction of anticoagulant
activity, decreased fibrinolytic activity and abnormal flow in the
heart chamber, artery or vein (1,2).
Thromboembolism has been reported to significantly affect the
quality of life in patients with venous thrombosis (3,4) and has
also been indicated to lead to microcirculation dysfunction,
embolism of skin mucous membrane necrosis, organ dysfunction and
bleeding tendencies and pulmonary embolism (5,6).
Clinical investigation has revealed that atrial fibrillation and
thromboembolism significantly affects health (7). Furthermore, atrial fibrillation has
been demonstrated to cause sudden fatality in patients with
thromboembolism (7).
Previous studies have indicated that anticoagulation
treatments are the most commonly used and efficient therapeutic
agents for the prevention and treatment in adults and children who
have undergone catheter-associated thrombosis in the clinical
setting (8). Edoxabana, an inhibitor
of coagulation factor Xa, is a clinically prescribed
pharmacological agent for the treatment of non-atrial fibrillation
that reduces stroke and systemic embolism by targeting coagulation
factor Xa (9). A previous study
indicated that systemic inflammation was observed and detected in
patients with left atrial thrombus and non-rheumatic atrial
fibrillation (10). In addition,
previous findings indicated that the pathogenesis of chronic
inflammation may be associated with the promotion of thrombus
formation and dysfunction of platelet function, as determined by
in vivo imaging (11).
Furthermore, research has identified that apoptosis of vascular
endothelial cells (VECs) is an important indicator for the severity
of a venous thrombus (12).
Although the effects and safety profile of edoxaban
have been investigated in patients with non-atrial fibrillation in
previous reports, the application of edoxaban for patients with
atrial fibrillation has not been fully elucidated and the molecular
mechanism involved remains unclear (13). Previous results have indicated that
the activity of the protein C system is correlated with thrombus
formation and is involved in the inhibition of thrombin generation
in the platelet microenvironment (14,15). In
addition, Hadas et al (16)
suggested that methylglyoxal induces platelet hyperaggregation and
reduces thrombus stability through the upregulation of protein
kinase C activity and downregulation of the phosphoinositide
3-kinase (PI3K)/protein kinase B (AKT) signaling pathway.
Furthermore, Yi et al (17)
demonstrated that the PI3K inhibitor S14161 inhibits the modulation
of platelet activation and thrombus formation, which suggests that
PI3K may be a novel therapeutic target for the prevention of
thrombotic disorders.
In the present study, PI3K and AKT expression levels
in VECs from mice with atrial fibrillation and thromboembolism that
received treatment with edoxaban were investigated. In addition,
the efficacy of edoxaban on TSLP expression, Wnt-β phosphorylation
and integrin expression in platelets was explored. In the present
study, the effects of edoxabana on inflammation and apoptosis in a
mouse model of atrial fibrillation and thromboembolism were
investigated. The molecular mechanism of the edoxabana-mediated
signaling pathway in VECs was explored and the association between
edoxaban, the protein C system and atrial fibrillation and venous
thrombosis was determined.
Materials and methods
Ethics statement
Animal experiments were implemented legitimately
according to the Guide for the Care and Use of Laboratory Animals
of Xinjiang Medical University (Urumchi, China) and approved by the
Ethics Committee of The First Affiliated Hospital, Xinjiang Medical
University.
Cells culture and regents
VECs and platelet cells were isolated from C57BL/6J
mice (as described in the animal study section) with ferric
chloride-induced vein thrombus (18). VECs and platelet cells were cultured
in minimum essential medium (Sigma-Aldrich; Merck KGaA, Darmstadt,
Germany) supplemented with 12% fetal bovine serum (Invitrogen;
Thermo Fisher Scientific, Inc., Waltham, MA USA). All cells were
cultured in a 37°C humidified atmosphere containing 5%
CO2.
Small interfering (si)RNA
transfection
VECs were cultured to 80% confluence and transfected
with siRNA (0.12 µmol/l; cat. no. 6388; Cell Signaling Technology,
Inc., Danvers, MA, USA) that targeted Wnt-β (Si-Wnt-β) or scrambled
siRNA (Si-vector) using Lipofectamine RNAi MAX (Invitrogen; Thermo
Fisher Scientific, Inc.) according to the manufacturer's
instructions. siRNA-targeting Wnt-β and scrambled siRNA were
obtained from Shanghai GenePharma Co., Ltd. (Shanghai, China). The
time interval between transfection and subsequent experimentation
was 24 h.
Western blot analysis
VECs and platelet cells were isolated from
experimental mice, homogenized using a radioimmunoprecipitation
assay lysate buffer (Invitrogen; Thermo Fisher Scientific, Inc.)
containing protease-inhibitor and centrifuged at 1,000 × g at 4°C
for 10 min. The supernatant was used for protein analysis. Protein
concentration was determined using a BCA protein assay kit (Thermo
Fisher Scientific, Inc.). Western blotting was performed as
described previously (19). Equal
volumes of protein (50 µg) were loaded onto each well and separated
with 10% SDS-PAGE. Polyvinylidene fluoride membranes were then used
for immunoblotting. The membrane was blocked using 5% milk for 1 h
at room temperature. Primary antibodies were then incubated at 4°C
overnight. These were as follows: TSLP (1:1,000; cat. no. ab188166;
Abcam, Cambridge, UK), Protein C (1:1,000; cat. no. GTX87071),
Protein S (1:1,000; cat. no. GTX29027; both GeneTex, Inc., Irvine,
CA, USA), APCI (1:2,000; cat. no. 250212; Abbiotec inc., San Diego,
CA, USA), thrombomodulin (1:1,000; cat. no. ab230189; Abcam),
αIlbβ3 (1:1,000; cat. no. 10139-R012; Sinopharm Chemical Reagent
Co., Ltd., Shanghai, China), p-Wnt β (1:2,000; cat. no. 8655S; Cell
Signaling Technology, Inc.), Thrombin (1:1,000; cat. no. ab92621),
PI3K (1:1,000; cat. no. ab151549), AKT (1:1,000; cat. no. ab18785),
integrin (1:1,000; cat. no. ab52971), β-actin (1:2,000; cat. no.
ab8827; all Abcam). After washing using Tris buffered saline with
Tween-20 three times for 8 min, secondary antibodies were incubated
at room temperature for 1 h. GAPDH was used as an internal control.
The secondary antibodies utilized were as follows: horseradish
peroxidase conjugated Rabbit anti-mouse immunoglobulin G; 1:1,000;
cat. no. ab6728; Abcam). Immunoreactivity was determined by
enhanced chemiluminescent autoradiography using an ImageQuant
Las4000 (Thermo Fisher Scientific, Inc.) Protein expression was
analyzed using BandScan 5.0 software (Glyko, Inc.; BioMarin
Pharmaceutical Inc., San Rafael, CA, USA).
Animal study
A total of 40 C57BL/6J female mice (6–8 weeks old,
20–25 g in body weight) were purchased from Vital River Laboratory
Animal Technology Co. Ltd. Mice were housed in a
temperature-controlled facility at 23±1°C with a relative humidity
of 50±5% and 12 h light/dark cycle with free access to food and
water. To develop venous thrombosis, ferric chloride was used to
induce C57BL/6J mice according previous study (18). Mice with venous thrombosis and atrial
fibrillation (as confirmed via ECGs) were divided into two groups
(n=20) and received treatment with edoxaban (10 mg/kg, Simeiquan
Biological Technology Co., Ltd., Shenzhen, China) or the same dose
of phosphate-buffered saline (PBS) by gavage. The treatments were
continued for 42 days and were administered once a day. On day 60,
mice were sacrificed and the venous samples were obtained for
further analysis.
Histological analysis
Cardiac veins were isolated from experimental mice,
fixed with 4% paraformaldehyde for 2 h at 37°C and permeabilized by
incubating with 80% absolute ethanol, then embedded in paraffin and
cut into sections (5 µm). The sections then underwent microwave
antigen retrieval. After cooling, they were washed with distilled
water and blocked using normal goat serum (Invitrogen; Thermo
Fisher Scientific, Inc.) at room temperature for 30 min. The
cardiac vein sections were incubated with primary antibodies: anti
Thrombin (1:1,000, cat. no. ab92621; Abcam) for 12 h at 4°C.
Fluorescent-labeled AlexaFluor 488 horseradish peroxidase
conjugated rabbit anti-mouse immunoglobulin G (1:1,000; cat. no.
ab6728; Abcam) for 2 h at 37°C. The histologic sections were
subsequently scanned using a confocal microscope (Carl Zeiss AG,
Oberkochen, Germany; magnification, ×200).
ELISA
Following treatment for 60 days, the plasma
concentration of interleukin (IL)-1 (cat. no. ab100704), IL-4 (cat.
no. ab100710), IL-8 (cat. no. ab46032), tumor necrosis factor
(TNF)-α (cat. no. ab208348), prostacyclin (PGI2; cat. no.
ab120912), prostaglandin (PG)E2 (cat. no. ab133021; all Abcam),
PGD2 (cat. no. RJ17502; Shanghai Renjie Biotechnology Co., Ltd.,
Shanghai, China), PGF2α (cat. no. YS3501B; Shanghai Yaji
Biotechnology Co., Ltd., Shanghai, China) and Serotonin (cat. no.
ab133053; Abcam) in mice with venous thrombosis and atrial
fibrillation were analyzed using commercialized ELISA kits
according to the manufacturer's protocol. The operational
procedures were performed according to the manufacturer's
instructions. The results were analyzed using an ELISA reader
system (Bio-Rad Laboratories, Inc., Hercules, CA, USA).
Terminal
deoxynucleotidyl-transferase-mediated dUTP nick end labelling
(TUNEL) assay
Treated VECs were fixed with 4% neutral formaldehyde
for 20 min at 4°C. After washing with PBS, cells were permeabilized
on ice with 0.1% Triton X-100 in PBS for 2 min and mounted with
neutral resins. The TUNEL assay kit (Biotool LLC, Houston, TX, USA)
was used to determine the extent of apoptosis of VECs in
experimental mice following treatment with 10 mg/kg edoxaban or the
same dose of PBS. The procedures were performed as indicated in a
previous study (20). Cellular
nuclei were stained with DAPI (vector Laboratories, Inc.,
Burlingame, CA, USA). Images were captured with a ZEISS LSM 510
confocal microscope at 488 nm. Apoptotic cells were examined under
a laser confocal microscope (Fluoview 1000; Olympus, Tokyo, Japan;
magnification, ×200). The cellular nuclei and apoptotic cells were
counted in three fields of view from each sample.
Patelet aggregation test and platelet
release assay
Blood was collected and mixed with sodium citrate to
produce a final concentration of 0.38%. Citrated blood was then
mixed with an equal volume (5 ml) of PBS (pH 7.4). Platelet-rich
plasma (PRP) was obtained via centrifugation at a speed of 50 × g
for 10 min at 23°C with a refrigerated centrifuge (cat. no.
TGL-16A; Hunan Xiangli Scientific Instrument Co., Ltd., Changsha,
China). The PRP was then centrifuged a second time at 50 × g for 10
min at 23°C. The resultant suspension was further centrifuged at
750 × g for 10 min at 23°C to obtain the platelet pellet. The
platelet pellet was washed once in HEPES/Tyrode's buffer (10 mM
HEPES/NaOH, 5.56 mM glucose, 137 mM NaCl, 12 mM NaHCO3, 2.7 mM KCl,
0.36 mM NaH2PO4, 1 mM MgCl2, pH 7.4) in the presence of 1 mM EGTA
20. Following centrifugation at 750 × g for 10 min at room
temperature the platelet pellet was gently suspended in
HEPES/Tyrode's buffer and platelet concentrations were
2–3×108/ml. Washed platelets were then pre-incubated for
5 min at 37°C.
In vitro platelet aggregation was assessed in
citrated platelet rich plasma using a previously described method
(21). To minimize the loss of
denser platelets, the platelet agonists were as follows: Collagen
(4 µg/ml; Mascia Brunelli S.p.a., Milan, Italy), adenosine
diphosphate (5 µM), and ristocetin (1.5 mg/ml; each from
Sigma-Aldrich; Merck KGaA).
Platelet release was then induced for 10 min. by
adding collagen to a final concentration of 50 µg/ml. Prior to the
addition of collagen, CPsA (Shanghai Yaji Biotechnology Co., Ltd.)
was added to the washed platelets to obtain a final concentration
of 500 µg/ml. When reaction was completed, samples were centrifuged
at 10,000 × g for 2 min at room temperature. The supernatants were
then recovered and aliquoted. The levels of Serotonin were
determined using the aforementioned ELISA kits.
Statistical analysis
Data are presented as mean ± standard error of the
mean. Statistical differences between experimental groups were
analyzed using a Student's t-test. P<0.05 was considered to
indicate a statistically significant difference.
Results
Edoxaban affects the protein
expression levels of inflammatory factors and chemokines in the
sera of mice with atrial fibrillation and venous thrombosis
Inflammatory factor expression levels in the sera.
As indicated in Fig. 1A-D, the
expression levels of IL-1, −4, −8 and TNF-α were significantly
decreased in the sera of mice with fibrillation and venous
thrombosis that were treated with edoxaban when compared with mice
that received PBS treatment (P<0.01). Furthermore, edoxaban
therapy resulted in a significant increase in the expression levels
of chemokines PGI2, PGE2, PGD2 and PGF2α compared with PBS
treatment (P<0.01; Fig. 1E-H).
These results suggest that edoxaban may inhibit the expression of
inflammatory factors and promote the expression of chemokines in
the sera of mice with atrial fibrillation and venous
thrombosis.
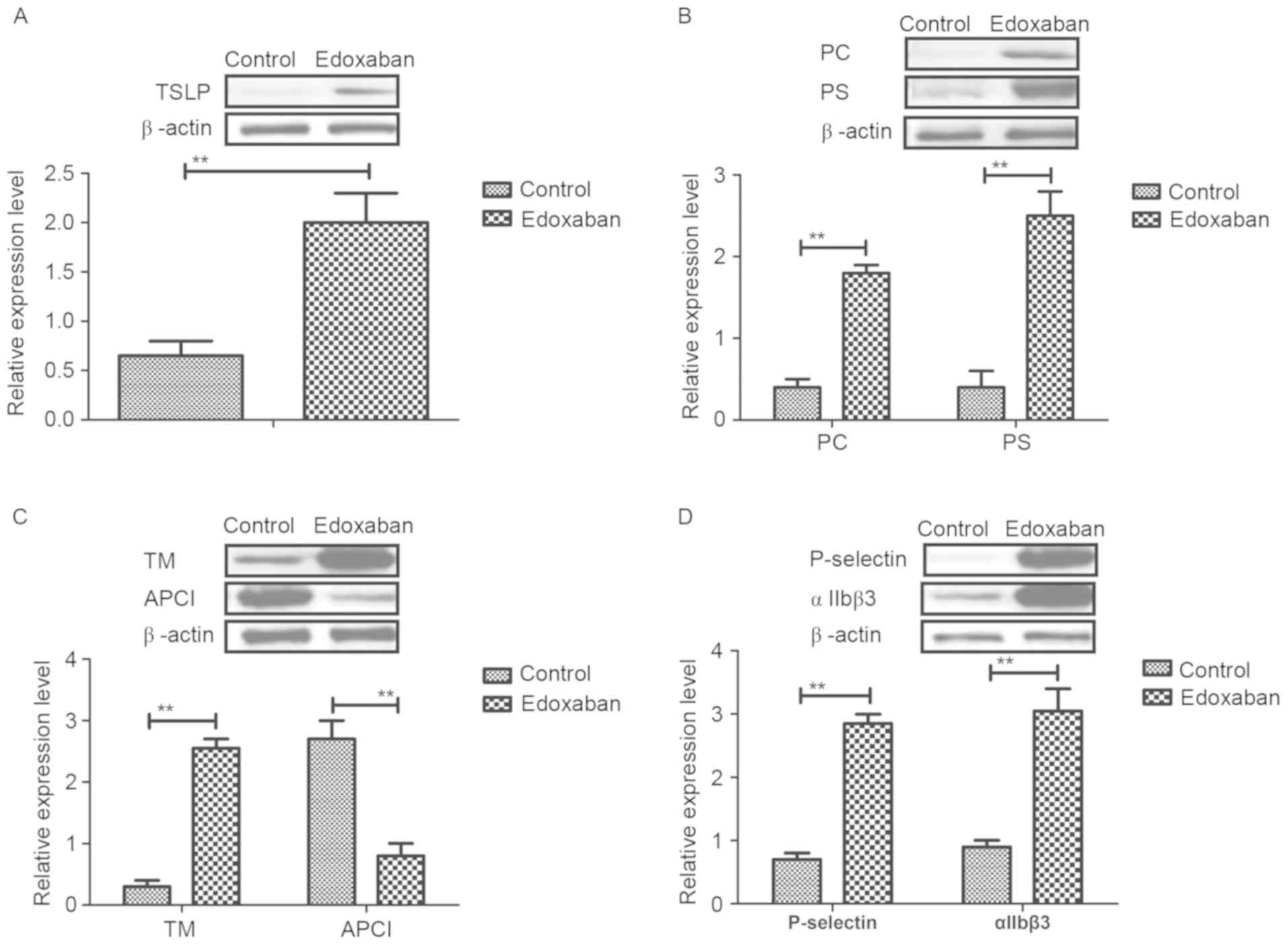
Edoxaban promotes the protein
expression levels of TSLP and activates the protein C system in
mice with atrial fibrillation and venous thrombosis
TSLP and activated protein C protein expression
levels were examined in mice with atrial fibrillation and venous
thrombosis using western blot analysis. As indicated in Fig. 2A, edoxaban significantly promoted
TSLP protein expression levels in platelets (P<0.01). In
addition, the expression levels of protein C system and APC
components were detected. Results indicated that protein C and
protein S expression levels were significantly upregulated in
experimental mice treated with edoxaban compared with those treated
with PBS (P<0.01; Fig. 2B).
Furthermore, the protein expression levels of thrombomodulin (TM)
were significantly upregulated, whereas the protein expression
levels of activated protein C inhibitor (APCI) were significantly
downregulated in edoxaban-treated mice with atrial fibrillation and
venous thrombosis (P<0.01; Fig.
2C). Furthermore, it was demonstrated that P-selectin and
integrin αIIbβ3 protein expression levels were significantly
increased in mice that received edoxaban therapy (P<0.01;
Fig. 2D). These results suggest that
edoxaban may stimulate TSLP expression and activate the protein C
system in mice with atrial fibrillation and venous thrombosis.
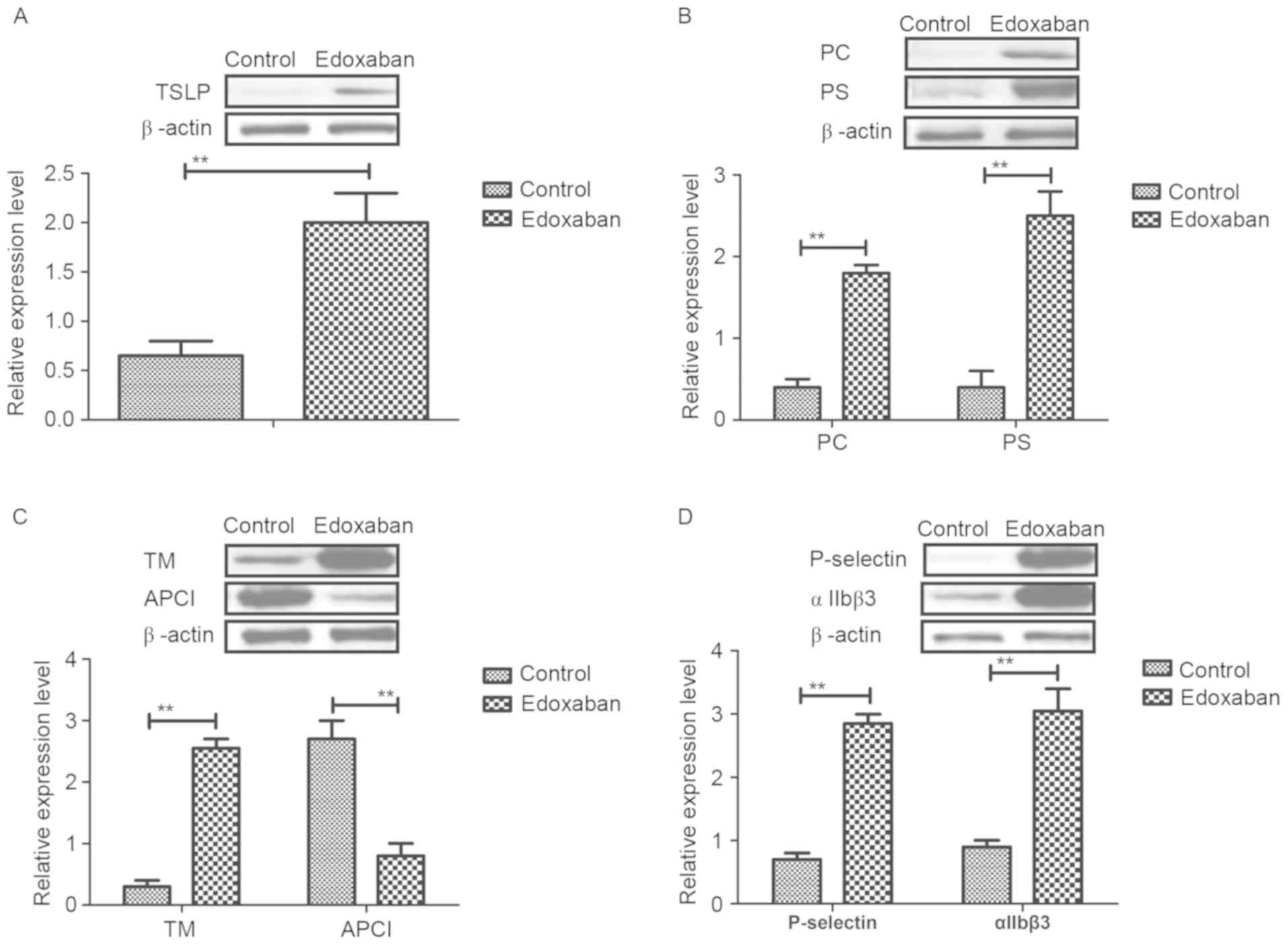 | Figure 2.Analysis of TSLP expression and
protein C system activity in mice with atrial fibrillation and vein
thrombus. (A-D) Protein expression levels of TSLP, PC, PS, TM,
APCI, P-selectin and integrin αIIbβ3 in experimental mice treated
with edoxaban or phosphate-buffered saline. Data are presented as
mean ± standard deviation of the mean. **P<0.01 as indicated.
TSLP, thymic stromal lymphopoietin; PC, protein C; PS, protein S;
TM, thrombomodulin; APCI, activated protein C inhibitor. |
Edoxaban activates Wnt-β
phosphorylation and inhibits platelet aggregation and secretion in
mice with atrial fibrillation and venous thrombosis
To investigate the mechanism of edoxaban-induced
upregulation of TSLP expression levels, Wnt-β phosphorylation and
integrin expression was detected in platelets in mice with atrial
fibrillation and venous thrombosis. The results in Fig. 3A indicated that edoxaban
significantly promoted Wnt-β phosphorylation in platelets
(P<0.01). In addition, it was observed that edoxaban treatment
significantly inhibited the aggregation of platelet cells and
significantly downregulated the protein expression levels of
thrombin compared with the control (P<0.01; Fig. 3B and C). Furthermore, results
indicated that platelet serotonin release was significantly
decreased in experimental mice treated with edoxaban compared with
the control (P<0.01; Fig. 3D).
Taken together, the results suggest that edoxaban may activate
Wnt-β phosphorylation and inhibit platelet aggregation and
secretion in mice with atrial fibrillation and venous
thrombosis.
Edoxaban regulates protein C system
through Wnt-β-mediated PI3K/AKT signal pathway in VECs
The edoxaban-mediated regulation of the protein C
system in VECs from experimental mice with atrial fibrillation and
venous thrombosis was further investigated. As indicated in
Fig. 4A, the protein expression
levels of PI3K and AKT were significantly upregulated following
edoxaban treatment (P<0.01). In addition, edoxaban significantly
upregulated Wnt-β protein expression levels in VECs (P<0.01;
Fig. 4B). Furthermore, results
indicated that inhibition of Wnt-β by siRNA (Si-Wnt-β) inhibited
the protein expression levels of PI3K and AKT in VECs (Fig. 4C). Additionally, it was observed that
Si-Wnt-β treatment significantly decreased the protein expression
levels of protein C and protein S (P<0.01; Fig. 4D). Expression levels of TM and APCI
were also significantly downregulated by Si-Wnt-β (P<0.01;
Fig. 4E). Furthermore, TSLP and
integrin protein expression levels were significantly suppressed by
Si-Wnt-β (P<0.01; Fig. 4F). Taken
together, these results suggest that edoxaban may regulate the
protein C system through the Wnt-β-mediated PI3K/AKT signaling
pathway in VECs.
Edoxaban improves atrial fibrillation
and venous thrombosis in a mouse model
In vivo therapeutic effects of edoxaban were
investigated in mice with atrial fibrillation and venous
thrombosis. As indicated in Fig. 5A,
data indicated that edoxaban improved apoptosis (as determined by
reduced staining) of VECs compared with control mice. Furthermore,
defective thrombus formation was significantly improved by edoxaban
compared with the control according to shear rates data (P<0.01;
Fig. 5B). In addition, results
indicated that stroke and blood velocity were significantly
improved in experimental mice treated with edoxaban (P<0.01;
Fig. 5C and D). Furthermore, data
indicated that atrial fibrillation was improved as the area of
venous thrombosis was markedly decreased in edoxaban-treated mice
with atrial fibrillation and vein thrombus (Fig. 5E and F). Taken together, the results
suggest that edoxaban may improve apoptosis, stroke, atrial
fibrillation and venous thrombosis in a mouse model.
Discussion
Venous thrombosis is a common disorder that is
associated with various molecular mechanisms and diverse processes
(22). Multiple factors may induce
the pathology of venous thromboembolism, including VEC injury,
blood flow state changes and increased blood clotting (22). Notably, venous thromboembolism may
induce a large number of other diseases, including pulmonary
embolism, neurologic diseases and skin disease (23–25).
Recently, atrial fibrillation and venous thrombosis has been
associated with significantly increased morbidity and mortality
rates in patients with cardiovascular disease in the clinical
setting (26). Anticoagulant therapy
is prescribed for millions of patients worldwide for the prevention
and treatment of venous thrombosis (27,28).
In the present study, edoxaban was administered for
the treatment of atrial fibrillation and venous thrombosis and the
efficacy and molecular mechanism of edoxaban was investigated.
Inflammatory factors and chemokine serum levels were studied in
experimental mice treated with edoxaban. In addition, the
association between edoxaban and the protein C system in VECs was
assessed in experimental mice. Furthermore, the Wnt-β-mediated
PI3K/AKT signaling pathway in VECs was also investigated. The
present results suggested that edoxaban inhibited the serum levels
of inflammatory factors, but also improved apoptosis, stroke,
atrial fibrillation and venous thrombosis through regulation of the
Wnt-β-mediated PI3K/AKT signaling pathway in a mouse model of
atrial fibrillation and venous thrombosis.
Serum levels of inflammatory factors are an
important measurement index in patients with cardiovascular disease
in the clinical setting (29).
Previous results identified that increased levels of inflammatory
markers were associated with disease severity of patients with
rheumatic mitral stenosis predisposed to left atrial thrombus
formation (30). In addition, Empana
et al (31) revealed that
inflammation contributed to thrombotic diseases based on
microparticles and sudden cardiac death due to coronary occlusion.
Furthermore, Sadowski et al (32) indicated that coronary thrombus
composition was associated with inflammation, and platelet and
endothelial markers. Notably, the expression levels of the
chemokines have been demonstrated to serve an essential role in
portal vein thrombosis (33). The
present results suggested that edoxaban significantly inhibited the
serum levels of inflammatory factors and upregulated the levels of
chemokines in mice with atrial fibrillation and venous thrombosis.
These regulations are beneficial for the treatment of atrial
fibrillation and venous thrombosis.
Protein C is important regulatory protein in the
progression of venous thrombosis (14,15). The
present study investigated the role of edoxaban on the protein C
system in a mouse model of atrial fibrillation and venous
thrombosis. It is well acknowledged that TSLP expression is
associated with the activity of the protein C system and may
predict the severity of patients with atrial fibrillation and
venous thrombosis (34,35). In addition, a previous report has
suggested that the levels of TM and APCI was also correlated with
venous thrombosis (36). The present
results indicated that edoxaban promoted TM expression and
inhibited APCI in the serum of mice with venous thrombosis.
Furthermore, previous reports have indicated that P-selectin and
integrin may inhibit thrombus resolution and prevent vein wall
fibrosis (37,38). In the present study, it was indicated
that P-selectin and integrin αIIbβ3 expression levels were
increased in mice following edoxaban therapy. These results suggest
that edoxaban may stimulate TSLP expression and activate the
protein C system in mice with atrial fibrillation and venous
thrombosis.
The PI3K/AKT signaling pathway is associated with
the progression of vein thrombus (16). However, to the best of our knowledge,
the effect of edoxaban on the PI3K/AKT signaling pathway has not
been previously studied. Guidetti et al (39) suggested that the PI3K/AKT signaling
pathway is stimulated by integrin engagement and further inhibits
activation of platelet in thrombus formation and stabilization.
These findings highlighted the possibility of novel venous
thrombosis and anti-thrombotic therapeutic strategies. In addition,
Su et al (40) also indicated
that human cathelicidin LL-37 inhibits the aggregation of platelets
and further lead to the inhibition of thrombosis via Src/PI3K/Akt
signaling. Notably, blood activity of platelets serve a crucial
role in hemostasis and formation of thrombosis (41). In the present analysis, it was
revealed that PI3K and AKT expression levels were significantly
upregulated by edoxaban through the Wnt-β-mediated PI3K/AKT
signaling pathway in a mouse model of atrial fibrillation and
venous thrombosis. However, inhibition of Wnt-β by its inhibitor
(Si-wnt-β) suppressed the protein expression levels of TM, TSLP and
integrin, which were also downregulated by Si-Wnt-β in VECs. Taken
together, these results suggest that edoxaban may regulate the
protein C system through the Wnt-β-mediated PI3K/AKT signal pathway
in VECs.
In conclusion, the present study identified that
edoxaban may be a potential oral anticoagulant in the acute
treatment of atrial fibrillation and venous thrombosis. The novel
findings suggest a potential insight to explore more efficient
preclinical mechanisms and therapeutic strategies of edoxaban for
treating atrial fibrillation and venous thrombosis. Notably, the
present findings demonstrated preclinical and experimental evidence
to support the efficacy of edoxaban, but also suggested the
molecular mechanism of edoxaban-mediated changes of Wnt-β,
P-selectin and integrin αIIbβ3 expression through the PI3K/AT
signaling pathway in VECs obtained from mice with atrial
fibrillation and venous thrombosis. Results identified that
edoxaban activated the protein C system by stimulation of the
PI3K/AT signaling pathway in VECs obtained from mice with atrial
fibrillation and venous thrombosis. Taken together, the present
outcomes suggest that edoxaban may improve the venous lesions by
regulation of apoptosis, stroke, atrial fibrillation and venous
thrombosis through the Wnt-β-mediated protein C system via the
PI3K/AKT signaling pathway, suggesting eoxaban may be an efficient
anti-thrombotic therapeutic agent for the treatment of atrial
fibrillation and venous thrombosis in the clinical setting.
Acknowledgements
Not applicable.
Funding
The present study was supported by the Xinjiang
Natural Science Fund (Efficacy and mechanism of protein C system in
progression of atrial fibrillation and vein thrombus, grant no.
2016D01C304).
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
XS and SM designed the present study and analyzed
the data; XS and ZL performed the experiments. MW analyzed the
data.
Ethics approval and consent to
participate
All animal procedures were reviewed and approved by
the Ethical Committee of The First Affiliated Hospital, Xinjiang
Medical University and the China Experimental Animal Protection
Association. All efforts were made to minimize the suffering of the
experimental mice.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Lim MS and Enjeti AK: Safety of
anticoagulation in the treatment of venous thromboembolism in
patients with haematological malignancies and thrombocytopenia:
Report of 5 cases and literature review. Crit Rev Oncol Hematol.
105:92–99. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Nagler M, Kremer Hovinga JA, Alberio L,
Peter-Salonen K, von Tengg-Kobligk H, Lottaz D, Neerman-Arbez M and
Lämmle B: Thromboembolism in patients with congenital
afibrinogenaemia. Long-term observational data and systematic
review. Thromb Haemost. 116:722–732. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Shlebak A: Antiphospholipid syndrome
presenting as cerebral venous sinus thrombosis: A case series and a
review. J Clin Pathol. 69:337–343. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Samoš M, Bolek T, Ivanková J, Stančiaková
L, Kovář F, Galajda P, Kubisz P, Staško J and Mokáň M: Heparin
induced thrombocytopenia presenting with deep venous thrombosis and
pulmonary embolism successfully treated with rivaroxaban: Clinical
case report and review of current experiences. J Cardiovasc
Pharmacol. 68:391–394. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
McKeage K and Keating GM: Parnaparin: A
review of its use in the management of venous thromboembolism,
chronic venous disease and other vascular disorders. Drugs.
68:105–122. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Pellegrini VD Jr: Prophylaxis against
venous thromboembolism after total hip and knee arthroplasty: A
critical analysis review. JBJS Rev. 3:01874474-201509000-00005.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Devlin R, Bonanno L and Badeaux J: The
incidence of thromboembolism formation following the use of
recombinant factor VIIa in patients suffering from blunt force
trauma compared with penetrating trauma: A systematic review. JBI
Database System Rev Implement Rep. 14:116–138. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Barco S, Atema JJ, Coppens M, Serlie MJ
and Middeldorp S: Anticoagulants for the prevention and treatment
of catheter-related thrombosis in adults and children on parenteral
nutrition: A systematic review and critical appraisal. Blood.
15:369–377. 2017.
|
|
9
|
Piazza G, Mani V, Goldhaber SZ, Grosso MA,
Mercuri M, Lanz HJ, Schussler S, Hsu C, Chinigo A, Ritchie B, et
al: Magnetic resonance venography to assess thrombus resolution
with edoxaban monotherapy versus parenteral
anticoagulation/warfarin for symptomatic deep vein thrombosis: A
multicenter feasibility study. Vasc Med. 21:361–368. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Maehama T, Okura H, Imai K, Saito K,
Yamada R, Koyama T, Hayashida A, Neishi Y, Kawamoto T and Yoshida
K: Systemic inflammation and left atrial thrombus in patients with
non-rheumatic atrial fibrillation. J Cardiol. 56:118–124. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Nishimura S: Pathogenesis of chronic
inflammation revealed by in vivo imaging: Thrombus formation and
platelet function. Rinsho Ketsueki. 51:620–624. 2010.(In Japanese).
PubMed/NCBI
|
|
12
|
Mo XR, Luo XJ, Li CP, Pan XF and Zhou LL:
Effect of mannitol injection by intravenous catheter on ear vein
endothelial cell apoptosis and venous thrombus in rabbits. Eur Rev
Med Pharmacol Sci. 19:491–497. 2015.PubMed/NCBI
|
|
13
|
Shirai Y, Noguchi T, Kita S, Nakamura A,
Tanimoto H, Ishigaki N, Aoyama K and Yoshida T: A study of
usefulness for portal vein thrombus with edoxaban. Nihon Shokakibyo
Gakkai Zasshi. 113:439–440. 2016.(In Japanese). PubMed/NCBI
|
|
14
|
Fei D, Meng X, Zhao M, Kang K, Tan G, Pan
S, Luo Y, Liu W, Nan C, Jiang H, et al: Enhanced induction of heme
oxygenase-1 suppresses thrombus formation and affects the protein C
system in sepsis. Transl Res. 159:99–109. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Lozano M, Escolar G, Schwarz HP, Hernández
R, Bozzo J and Ordinas A: Activated protein C inhibits thrombus
formation in a system with flowing blood. Br J Haematol.
95:179–183. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Hadas K, Randriamboavonjy V, Elgheznawy A,
Mann A and Fleming I: Methylglyoxal induces platelet
hyperaggregation and reduces thrombus stability by activating PKC
and inhibiting PI3K/Akt pathway. PLoS One. 8:e744012013. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Yi W, Li Q, Shen J, Ren L, Liu X, Wang Q,
He S, Wu Q, Hu H, Mao X and Zhu L: Modulation of platelet
activation and thrombus formation using a pan-PI3K inhibitor
S14161. PLoS One. 9:e1023942014. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Srivastava AK, Kalita J, Haris M, Gupta RK
and Misra UK: Radiological and histological changes following
cerebral venous sinus thrombosis in a rat model. Neurosci Res.
65:343–346. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Wai-Hoe L, Wing-Seng L, Ismail Z and
Lay-Harn G: SDS-PAGE-based quantitative assay for screening of
kidney stone disease. Biol Proced Online. 11:145–160. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Naganuma Y, Ichii O, Otsuka S, Hashimoto Y
and Kon Y: Analysis of TdT-mediated dUTP nick end labeling
(TUNEL)-positive cells associated with cardiac myogenesis in mouse
embryo. J Vet Med Sci. 75:283–290. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
González-Manchón C, Larrucea S, Pastor AL,
Butta N, Arias-Salgado EG, Ayuso MS and Parrilla R: Compound
heterozygosity of the GPIbalpha gene associated with
Bernard-Soulier syndrome. Thromb Haemost. 86:1385–1391. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Hawbaker S: Venous thromboembolism in the
cancer population: Pathology, risk, and prevention. J Adv Pract
Oncol. 3:23–33. 2012.PubMed/NCBI
|
|
23
|
Vitale C, D'Amato M, Calabro P, Stanziola
AA, Mormile M and Molino A: Venous thromboembolism and lung cancer:
A review. Multidiscip Respir Med. 10:282015. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Ungprasert P, Tanratana P and Srivali N:
Autoimmune hemolytic anemia and venous thromboembolism: A
systematic review and meta-analysis. Thromb Res. 136:1013–1017.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Fernandez MM, Hogue S, Preblick R and
Kwong WJ: Review of the cost of venous thromboembolism. Clinicoecon
Outcomes Res. 7:451–462. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Santin BJ, Lohr JM, Panke TW, Neville PM,
Felinski MM, Kuhn BA, Recht MH and Muck PE: Venous duplex and
pathologic differences in thrombus characteristics between de novo
deep vein thrombi and endovenous heat-induced thrombi. J Vasc Surg
Venous Lymphat Disord. 3:184–189. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Corral J, Huntington JA, González-Conejero
R, Mushunje A, Navarro M, Marco P, Vicente V and Carrell RW:
Mutations in the shutter region of antithrombin result in formation
of disulfide-linked dimers and severe venous thrombosis. J Thromb
Haemost. 2:931–939. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Vayá A, Gómez I, Mira Y, Ferrando F and
Corella D: Homocysteine levels in patients with deep vein
thrombosis lacking thrombophilic defects. Thromb Haemost.
99:1132–1134. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Dittmeier M, Wassmuth K, Schuhmann MK,
Kraft P, Kleinschnitz C and Fluri F: Dabigatran etexilate reduces
thrombin-induced inflammation and thrombus formation in
experimental ischemic stroke. Curr Neurovasc Res. 13:199–206. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Pulimamidi VK, Murugesan V, Rajappa M,
Satheesh S and Harichandrakumar KT: Increased levels of markers of
oxidative stress and inflammation in patients with rheumatic mitral
stenosis predispose to left atrial thrombus formation. J Clin Diagn
Res. 7:2445–2448. 2013.PubMed/NCBI
|
|
31
|
Empana JP, Boulanger CM, Tafflet M, Renard
JM, Leroyer AS, Varenne O, Prugger C, Silvain J, Tedgui A, Cariou
A, et al: Microparticles and sudden cardiac death due to coronary
occlusion. The TIDE (Thrombus and Inflammation in sudden DEath)
study. Eur Heart J Acute Cardiovasc Care. 4:28–36. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Sadowski M, Zabczyk M and Undas A:
Coronary thrombus composition: Links with inflammation, platelet
and endothelial markers. Atherosclerosis. 237:555–561. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Li N, Guo W, Shi J, Xue J, Hu H, Xie D, Wu
M and Cheng S: Expression of the chemokine receptor CXCR4 in human
hepatocellular carcinoma and its role in portal vein tumor
thrombus. J Exp Clin Cancer Res. 29:1562010. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Yadava K, Sichelstiel A, Luescher IF,
Nicod LP, Harris NL and Marsland BJ: TSLP promotes
influenza-specific CD8+ T-cell responses by augmenting local
inflammatory dendritic cell function. Mucosal Immunol. 6:83–92.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Janda J, Plattet P, Torsteinsdottir S,
Jonsdottir S, Zurbriggen A and Marti E: Generation of equine
TSLP-specific antibodies and their use for detection of TSLP
produced by equine keratinocytes and leukocytes. Vet Immunol
Immunopathol. 147:180–186. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Tate CM, Blosser W, Wyss L, Evans G, Xue
Q, Pan Y and Stancato L: LY2228820 dimesylate, a selective
inhibitor of p38 mitogen-activated protein kinase, reduces
angiogenic endothelial cord formation in vitro and in vivo. J Biol
Chem. 288:6743–6753. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Diaz JA, Wrobleski SK, Pechota AR, Hawley
AE, Roelofs KJ, Doornbos NK, Gabriel JE, Reynolds G, Lester P,
Londy F, et al: P-selectin inhibition therapeutically promotes
thrombus resolution and prevents vein wall fibrosis better than
enoxaparin and an inhibitor to von Willebrand factor. J Vasc Surg
Venous Lymphat Disord. 2:1142014. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Rossaint J, Vestweber D and Zarbock A:
GDF-15 prevents platelet integrin activation and thrombus
formation. J Thromb Haemost. 11:335–344. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Guidetti GF, Canobbio I and Torti M:
PI3K/Akt in platelet integrin signaling and implications in
thrombosis. Adv Biol Regul. 59:36–52. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Su W, Chen Y, Wang C, Ding X, Rwibasira G
and Kong Y: Human cathelicidin LL-37 inhibits platelet aggregation
and thrombosis via Src/PI3K/Akt signaling. Biochem Biophys Res
Commun. 473:283–289. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
McFadyen J and Peter K: Forget about
thrombosis: Platelets and Alzheimer's disease, yet another sticky
situation. Sci Signal. 9:fs92016. View Article : Google Scholar : PubMed/NCBI
|