Introduction
Cerebral stroke (CS) is an acute cerebrovascular
disease, it is the main cause of disability in adults, it has a
high incidence rate, high mortality rate and a high disability rate
(1). The incidence rate of ischemic
stroke in CS was higher than that of the hemorrhagic stroke
(2). Acute ischemic stroke (AIS) is
a circulatory disorder that seriously harms human health, and
commonly occurs in middle-aged and elderly individuals (3). AIS is caused by atherosclerosis and
thrombosis in patients, so it causes local brain tissue ischemia
and hypoxic lesions in patients. The treatment process is extremely
difficult (4). Currently, early
application of recombinant tissue plasminogen activator (rt-PA)
intravenous thrombolytic therapy can effectively improve the
treatment of AIS (3). The key to the
treatment of AIS is early intravenous administration of rt-PA
intravenous thrombolytic therapy, which recanalizes the damaged
blood vessels. Also the ischemic penumbra zone can be reperfused
(5). Therefore, early diagnosis
screening is critical for the treatment of AIS.
Guided by the American Heart Association/American
Stroke Association Early Management Guide for AIS in 2018, all
patients with suspected acute CA admitted to Liaocheng Brain
Hospital (Liaocheng, China) should have a brain imaging assessment
immediately after they arrive at Liaocheng Brain Hospital. In most
cases, CT scans [non-contrast CT (NCCT)] can provide the necessary
information for emergency assessment (6). A large number of documents have shown
that the CT perfusion (CTP) has an important effect in the
diagnosis of AIS (7,8). CTP uses continuous dynamic scanning for
selected levels of interest, with a non-ionic contrast agent to
reflect cerebral blood flow (CBF), cerebral blood volume (CBV),
mean transit time (MTT) and other blood perfusion parameters of
related brain tissue via calculation, that has been recognized
clinically (9). A large number of
reports have shown that CTP related parameters can detect cerebral
ischemic lesions at an early stage. This suggests that abnormal
brain tissue can provide an effective basis for clinical diagnosis
and the treatment of cerebrovascular diseases (10–12). In
this research, we studied the clinical value of brain CTP in
thrombolytic therapy of AIS patients and provided references for
the treatment of AIS patients.
Patients and methods
Basic patient information
A retrospective analysis of 185 patients diagnosed
with AIS in Liaocheng Brain Hospital from April 2012 to December
2017 was carried out. The age range was 59 to 81 years, the average
age was 71.15±5.22 years, and the average time from pathogenesis to
thrombolysis was 264.45±82.97 min. Inclusion criteria were: i)
pathogenesis duration <12 h; ii) ranked 4 to 24 points according
to the National Institute of Health Stroke Scale (NIHSS) before
treatment; iii) patients with effective treatment (2216) (NIHSS
score decreased 4 or more points compared with that before
treatment); iv) agree to receive relevant examinations and
treatments; v) patients with history of complete cases and
follow-up data; and vi) no related anticoagulation or thrombolytic
therapy was received in other hospitals. Exclusion criteria were:
i) patients who had allergic reactions or contraindications to the
medicines of our research; ii) patients during pregnancy or
lactation; iii) patients with acute gastrointestinal hemorrhage or
other hemorrhage disorders; iv) patients with other serious
diseases or tumors; v) patients with abnormal kidney, liver,
coagulation, blood pressure and blood sugar; and vi) patients with
communication or cognitive disorders. The subjects or their
families signed informed consent and cooperated with the medical
staff to complete the relevant medical treatment (Table I). The study was approved by the
Ethics Committee of Liaocheng Brain Hospital.
 | Table I.General information of patients in
clinics (n=185). |
Table I.
General information of patients in
clinics (n=185).
| Factors | n (%) |
|---|
| Age (years) |
|
<70 | 73
(39.46) |
| ≥70 | 112 (60.54) |
| Sex |
| Male | 124 (67.03) |
|
Female | 61
(32.97) |
| Married or
single |
|
Single | 62
(33.51) |
|
Married | 123 (66.49) |
| History of
smoking |
|
Smoking | 136 (73.51) |
|
Non-smoking | 49
(26.49) |
| History of drinking
alcohol |
|
Alcoholic | 118 (63.78) |
|
Non-alcoholic | 67
(36.22) |
| Eating habits |
|
Greasy | 147 (79.46) |
|
Light | 38
(20.54) |
| Type |
| Carotid
artery | 102 (55.14) |
| Vertebral
artery | 83
(44.86) |
NCCT, CTP inspection methods
Patients were requested to fast for 4–6 h before
examination, paralyzed patients were asked to remove metal objects
from the scanning range after the iodine allergy test became
negative. The Toshiba Aquilion 64-slice spiral CT machine was used
to scan the basal ganglia region for the level of interest. The
parameters are as follows: scanning layer thickness was 5 mm,
matrix 512×512, tube voltage 120 kV, tube current 210 mA, interval
time: 1 sec; scanning time: 16 sec, a total of 80 layers and
scanning range was 80 mm. The non-ionic iodine contrast agent of 50
ml of a venous injection (370 mg/ml) (iodoparin, cat. no.
60166-93-0; TargetMol, Boston, MA, USA) was injected through the
cubital vein at a flow rate of 4.5 to 5.0 ml/sec, and scanned at
the same time. The CT image data was transmitted to the treatment
workstation, and the treatment software of the system was used for
analysis and a series of brain perfusion parameter maps were
obtained. The abnormal area in the patient's CTP image was observed
and the CTP parameters were measured, namely CBF, CBV, and MTT.
rt-PA thrombolytic therapy and drug
schedule
The patients were connected to the monitor before
treatment (Wuhan Kaijin Medical Technology Co., Ltd., Wuhan, China)
and the changes in vital signs such as heart rate, blood pressure
and breathing were closely examined. Also 0.9 mg/kg of alteplase
(article no. RK20180329n; Boehringer Ingelheim Pharma GmbH &
Co. KG, Ingelheim, Germany) were given within 4.5 h of pathogenesis
for rt-PA thrombolytic therapy. The dosage was 0.9 mg/kg, and the
total dosage could not exceed 90 mg. Then, 10% of the total dose
was injected intravenously within 1 min, and the remaining drug was
continuously infused intravenously for more than 1 h. CT
examination was performed 24 h after rt-PA thrombolysis and if
hemorrhage did not occur in patients then routinely oral 100 mg
enteric-coated aspirin was applied, once per day.
Judging criteria
Early AIS signs of NCCT examination (13): blurred outline of the lenticular
nucleus or reduced density levels; increased density of internal
carotid artery in the brain (compact arterial sign); island
gray-white interface disappears (island sign). The ischemic
penumbra in CTP examination (14):
CBF decreased significantly while CBV remained normal, mildly
elevated or mildly decreased, and MTT was prolonged. The diagnosis
of AIS patients with NCCT and CTP was observed, the CTP parameters
in the abnormal perfusion zone and the mirror side zone of AIS
patients were recorded and compared; the NIHSS score was used to
investigate the correlation between the prognosis of NIHSS score
and CTP parameters after 3 months of thrombolytic therapy.
Statistical analysis
Statistical analysis was conducted by SPSS 17.3
(Beijing Net Counting Times Technology Co., Ltd., Beijing, China)
software system. Basic patient data counting were expressed as
percentage (%), using a Chi-square test. The CTP parameters of CBV,
CBF, and MTT were expressed as mean ± standard deviation and the
difference between the groups was analyzed by t-test. The
correlation between NIHSS scores and CTP parameters of CBV, CBF,
and MTT was analyzed by Spearman correlation analysis after 3
months of thrombolytic therapy. P<0.05 was considered to
indicate a statistically significant difference.
Results
Comparison between CTP and CTA
examinations in the diagnosis of AIS patients
In total, 177 patients were diagnosed with AIS by
clinical manifestations, biochemical tests and imaging. The
sensitivity level of CIS examination for diagnosis of AIS patients
was 96.61% and the sensitivity level of NCCT for diagnosis of AIS
patients was 63.28%. The sensitivity level of CTP examination for
diagnosis of AIS patients was significantly higher than that of the
NCCT examination and the difference was statistically significant
(P<0.050). The specificity level of CIS examination for
diagnosis of AIS patients was 50.00% and the specificity level of
NCCT for diagnosis of AIS patients was 25.00%. The specificity
level of patients with AIS diagnosed by CTP was significantly
higher than that of the NCCT, the difference was statistically
significant (P<0.050). The diagnostic compliance rate of
patients with AIS diagnosed by CTP was 94.59% and the diagnostic
compliance rate of AIS diagnosed by CT scan was 61.62%. The
diagnostic compliance rate of patients with AIS diagnosed by CTP
was significantly higher than that of NCCT and the difference was
statistically significant (P<0.050; Tables II and III and Fig.
1).
 | Table II.AIS effectiveness in CTP
diagnosis. |
Table II.
AIS effectiveness in CTP
diagnosis.
| CTP diagnosis | Clinical diagnosis
(+) | Clinical diagnosis
(−) | Total |
|---|
| CTP diagnosis
(+) | 171 | 4 | 175 |
| CTP diagnosis
(−) | 6 | 4 | 10 |
| Total | 177 | 8 | 185 |
 | Table III.AIS effectiveness in NCCT
diagnosis. |
Table III.
AIS effectiveness in NCCT
diagnosis.
| NCCT diagnosis | Clinical diagnosis
(SBI) | Clinical diagnosis
(Mild brain injury) | Total |
|---|
| NCCT diagnosis
(+) | 112 | 6 | 118 |
| NCCT diagnosis
(−) | 65 | 2 | 67 |
| Total | 177 | 8 | 185 |
Changes in CBV of CTP parameters and
correlation with NIHSS scores
The CBV in the abnormal perfusion zone of AIS
patients was 4.26±0.61 ml/100 g and in the mirror side zone was
5.95±0.84 ml/100 g. The CBV in the abnormal perfusion zone was
significantly lower than that of the mirror side zone, and the
difference was statistically significant (t=21.160, P<0.001).
NIHSS scores were obtained 3 months after thrombolytic therapy and
showed that the prognostic NIHSS score was negatively correlated
with CBV in patients with thrombolytic therapy (r=−0.912,
P<0.001; Fig. 2).
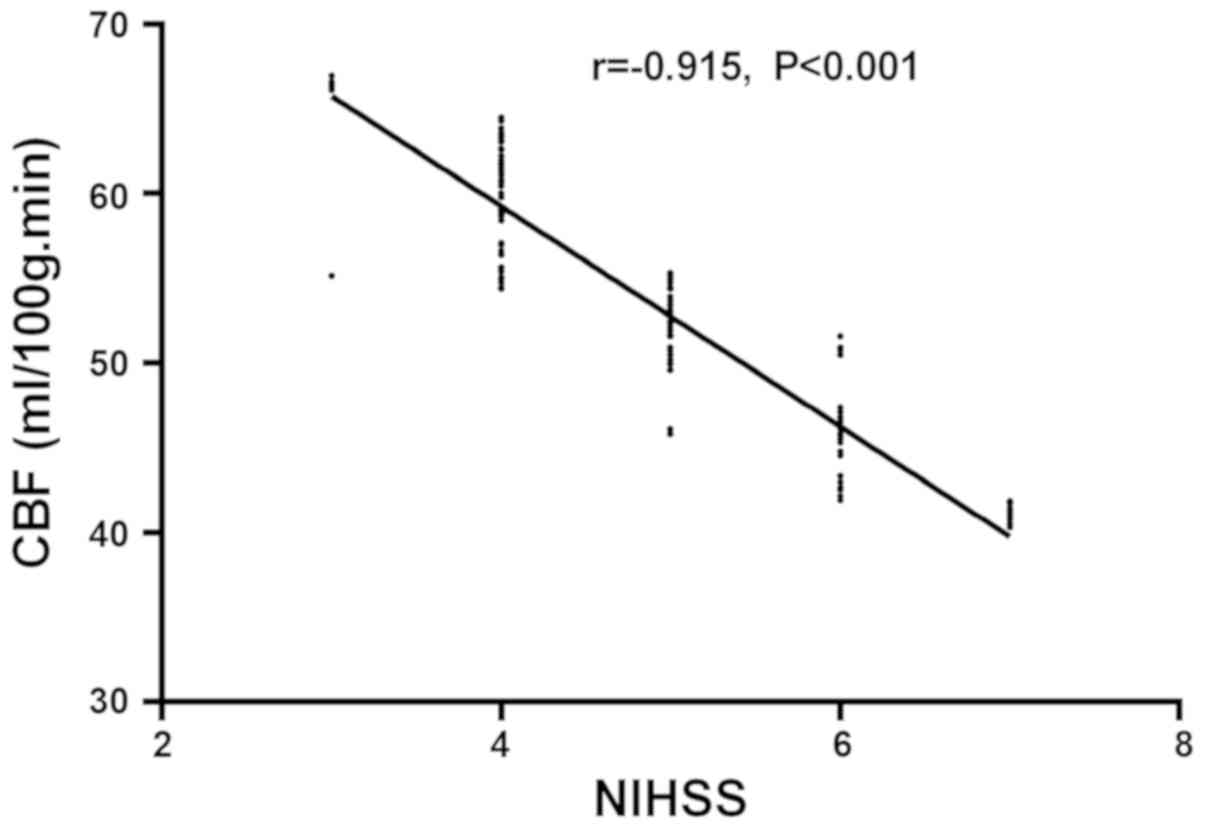
Changes in CBF of CTP parameters and
their correlation with NIHSS scores
The CBF in the abnormal perfusion zone of AIS
patients was 45.58±6.07 ml/100 g/min and in the mirror side zone
was 59.41±7.38 ml/100 g/min. The difference was statistically
significant (t=19.170, P<0.001). NIHSS scores were obtained 3
months after thrombolytic therapy and showed that the prognostic
NIHSS score was negatively correlated with CBF in patients with
thrombolytic therapy (r=−0.915, P<0.001; Fig. 3).
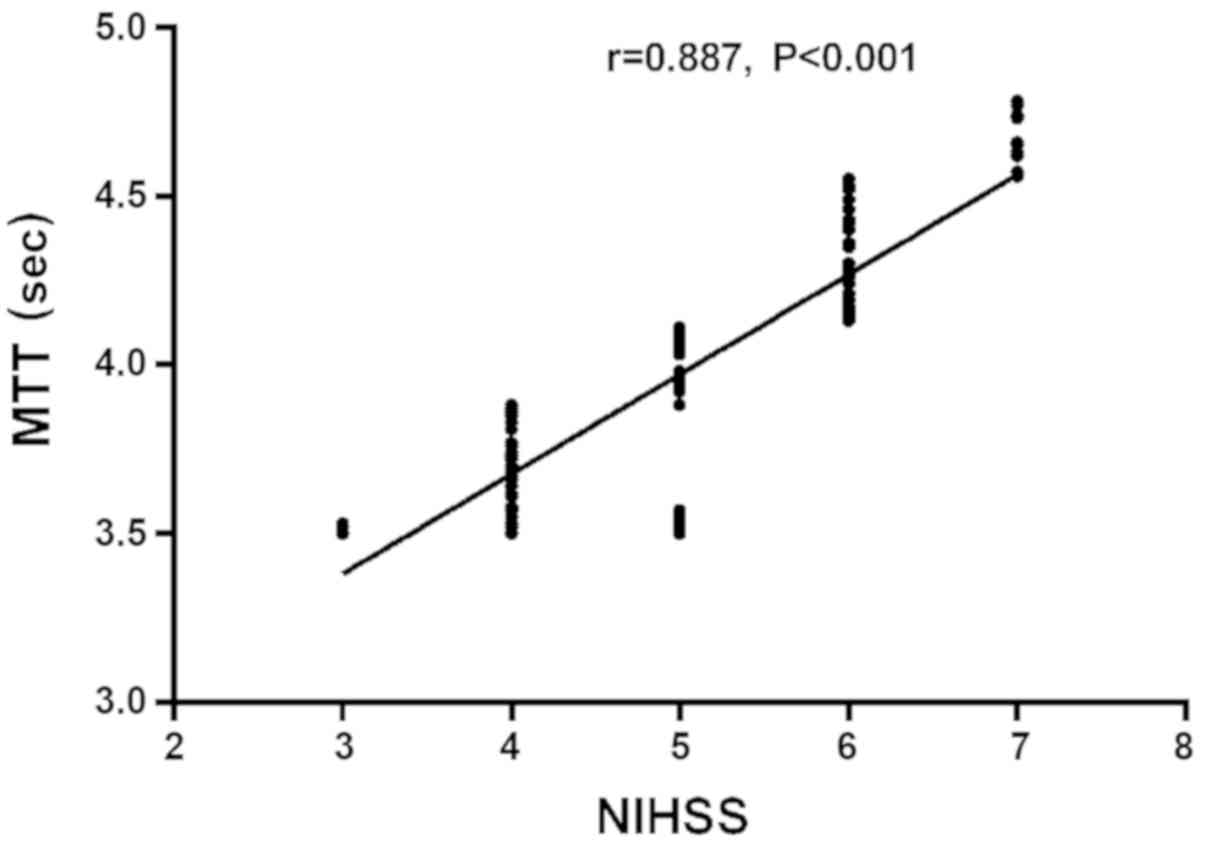
Changes in MTT of CTP parameters and
their correlation with NIHSS scores
The MTT in the abnormal perfusion zone of AIS
patients was 4.96±0.72 sec and the MTT in the mirror side zone was
4.02±0.56 sec. The MTT in the abnormal perfusion zone was higher
than that of the mirror side zone and the difference was
statistically significant (t=13.480, P<0.001). NIHSS scores were
obtained 3 months after thrombolytic therapy and showed that the
prognostic NIHSS scores were positively correlated with MTT in
patients with thrombolytic therapy (r=0.887, P<0.001; Fig. 4).
Discussion
According to statistics, in industrialized
countries, cerebrovascular disease is the leading cause of death
for women. Also it is the second cause of death for men and is an
important cause of cognitive impairment and dementia (15,16). CA
is the main cause of functional disability, and most CA patients
have neurological sequelae after treatment and it becomes
impossible to restore the same level of daily living activities as
before the disease (17). Currently,
the number of patients with global AIS is gradually declining due
to early control of risk factors. However, many patients still have
to take long-term care after treatment, causing a huge burden on
the patient's family and society. Therefore, early treatment is
very important (18). The first
choice for early treatment of AIS is rt-PA intravenous thrombolytic
therapy, and rt-PA is a highly selective thrombolytic drug for
fibrin (19). rt-PA is activated
once it binds to fibrin, this will induce the plasminogen convert
to fibrinolytic enzyme, which leads to the degradation of fibrin
and thrombosis in the body (20).
rt-PA thrombolytic therapy can restore blood supply to the
originally blocked blood vessels and reperfusion of brain tissue in
the ischemic penumbra. This improves the prognosis for life quality
of patients (21). This study
involved 185 patients diagnosed with AIS in Liaocheng Brain
Hospital, and the consistency of NCCT and CTP examination and
clinical diagnosis in AIS patients were analyzed. The correlation
of the prognosis of NIHSS scores between AIS patients and CBV, CBF,
MTT of CTP parameters were also analyzed. This study provided
references for clinical diagnosis and treatment of AIS
patients.
In this study, 177 patients were diagnosed with AIS
through clinical manifestations, biochemical tests and imaging.
Upon comparison of the detection results between the CTP and NCCT
of imaging, we revealed that the sensitivity, specificity, and
diagnostic compliance rates of AIS patients diagnosed by CTP were
higher than those of NCCT and the difference was statistically
significant. With the continuous development and progress of modern
medical CT scanning technology, CT has developed from morphological
imaging diagnosis to assessable hemodynamic changes that can be
assessed in vivo tissue (22). According to Yoo et al
(23), it was found that the safety
and efficacy of early NCCT for intra-arterial treatment has a
diagnostic value only for patients with small infarction, while
patients with large infraction require further examination for
diagnosis. However, Finlayson et al (24) showed that the diagnostic value of CTP
was higher than that of the NCCT and angiography in the diagnosis
of acute CA patients using NCCT, CT angiography and CTP, which
further approved our point of view. Later, we studied the CBV, CBF,
and MTT between the abnormal perfusion zone of AIS patients and the
mirror side zone. It was found that the CBV and CBF in the abnormal
perfusion zone were significantly lower than that of the mirror
side zone. Also the MTT in the abnormal perfusion zone was
significantly lower than that of the mirror side zone and the
difference was statistically significant. Relevant parameters of
CTP can reflect the collateral circulation of patients and the
abnormal perfusion of hemodynamics in brain tissues, so it provides
a basis for clinical treatment. If the CBF declines slightly, it
indicates that the cerebral circulation reserve is decompensated.
Also a significant reduction indicates that the patient may have
developed a cerebral infarction. Delayed MTT suggests a deduced
cerebral perfusion pressure as well as impaired perfusion reserve
and can indicate the condition of the patient's collateral
circulation (25). However, there is
no consistent conclusion on the optimal thresholds for CBV, CBF,
and MTT between the abnormal perfusion zone and the mirror side
zone. Therefore, we studied whether the prognosis of patients after
treatment was related to the pre-treatment CTP parameters. NIHSS
scores were obtained 3 months after thrombolytic therapy and the
prognosis of patients with thrombolytic therapy was negatively
correlated with CBV and CBF, while it was positively correlated
with MTT, and the difference was statistically significant.
According to van Seeters et al (26) in a study of patients with suspected
AIS, the parameters of CTP examination at admission have a strong
predictive effect on patients with poor prognosis and can be used
to predict long-term clinical outcomes. However, Ma et al
(27) also found that CTP parameters
are correlated with the evaluation index of patients' clinical
prognosis on the 14th and 90th day, which further supports our
research results.
In this experiment, due to the small number of
patients with AIS in Liaocheng Brain Hospital, we only have a small
base of selected subjects. Therefore, there may exist contingency
within our results and there were a large number of research
variables in AIS patients. Further study is still required.
Overall, brain CTP has a high diagnostic value for
rt-PA intravenous thrombolytic therapy in AIS. Also there is a
significant correlation with patients' prognosis score, which is
worthy of being promoted in the clinical diagnosis and treatment of
AIS patients.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the present
study are available from the corresponding author on reasonable
request.
Authors' contributions
SX wrote the manuscript. SX and LZ recorded and
analyzed NCCT and CTP inspection results. LW and LZ were
responsible for rt-PA thrombolytic therapy. All authors read and
approved the final manuscript.
Ethics approval and consent to
participate
The study was approved by the Ethics Committee of
Liaocheng Brain Hospital (Liaocheng, China). Signed informed
consents were obtained from the patients or guardians.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Sun Y, Zhang G, Zhang Z, Yu P, Zhong H, Du
J and Wang Y: Novel multi-functional nitrones for treatment of
ischemic stroke. Bioorg Med Chem. 20:3939–3945. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Amarenco P, Lavallée PC, Labreuche J,
Albers GW, Bornstein NM, Canhão P, Caplan LR, Donnan GA, Ferro JM,
Hennerici MG, et al TIAregistry.org Investigators, : One-year risk
of stroke after transient ischemic attack or minor stroke. N Engl J
Med. 374:1533–1542. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Jauch EC, Saver JL, Adams HP Jr, Bruno A,
Connors JJ, Demaerschalk BM, Khatri P, McMullan PW Jr, Qureshi AI,
Rosenfield K, et al American Heart Association Stroke Council;
Council on Cardiovascular Nursing; Council on Peripheral Vascular
Disease; Council on Clinical Cardiology, : Guidelines for the early
management of patients with acute ischemic stroke: a guideline for
healthcare professionals from the American Heart
Association/American Stroke Association. Stroke. 44:870–947. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Minnerup J, Wersching H, Teuber A,
Wellmann J, Eyding J, Weber R, Reimann G, Weber W, Krause LU, Kurth
T, et al REVASK Investigators, : Outcome after thrombectomy and
intravenous thrombolysis in patients with acute ischemic stroke: a
prospective observational study. Stroke. 47:1584–1592. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Joux J, Olindo S, Girard-Claudon A,
Chausson N, Saint-Vil M, Signate A, Edimonana M, Jeannin S,
Aveillan M, Cabre P, et al: Prehospital transfer medicalization
increases thrombolysis rate in acute ischemic stroke. A French
stroke unit experience. Clin Neurol Neurosurg. 115:1583–1585. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Powers WJ, Rabinstein AA, Ackerson T,
Adeoye OM, Bambakidis NC, Becker K, Biller J, Brown M, Demaerschalk
BM, Hoh B, et al American Heart Association Stroke Council, : 2018
guidelines for the early management of patients with acute ischemic
stroke: a guideline for healthcare professionals from the American
Heart Association/American Stroke Association. Stroke. 49:e46–e110.
2018. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Wintermark M: Brain perfusion-CT in acute
stroke patients. Eur Radiol. 15 (Suppl 4):D28–D31. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Lövblad KO and Baird AE: Computed
tomography in acute ischemic stroke. Neuroradiology. 52:175–187.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Wang XC, Gao PY, Xue J, Liu GR and Ma L:
Identification of infarct core and penumbra in acute stroke using
CT perfusion source images. AJNR Am J Neuroradiol. 31:34–39. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Borst J, Berkhemer OA, Roos YB, van Bavel
E, van Zwam WH, van Oostenbrugge RJ, van Walderveen MA, Lingsma HF,
van der Lugt A, Dippel DW, et al: MR CLEAN investigators: value of
computed tomographic perfusion-based patient selection for
intra-arterial acute ischemic stroke treatment. Stroke.
46:3375–3382. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Vagal A, Menon BK, Foster LD, Livorine A,
Yeatts SD, Qazi E, d'Esterre C, Shi J, Demchuk AM, Hill MD, et al:
Association between CT angiogram collaterals and CT perfusion in
the interventional management of stroke III trial. Stroke.
47:535–538. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Austein F, Riedel C, Kerby T, Meyne J,
Binder A, Lindner T, Huhndorf M, Wodarg F and Jansen O: Comparison
of perfusion CT software to predict the final infarct volume after
thrombectomy. Stroke. 47:2311–2317. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Demchuk AM, Menon BK and Goyal M:
Comparing vessel imaging: noncontrast computed tomography/computed
tomographic angiography should be the new minimum standard in acute
disabling Stroke. Stroke. 47:273–281. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Flottmann F, Broocks G, Faizy TD, Ernst M,
Forkert ND, Grosser M, Thomalla G, Siemonsen S, Fiehler J and
Kemmling A: CT-perfusion stroke imaging: a threshold free
probabilistic approach to predict infarct volume compared to
traditional ischemic thresholds. Sci Rep. 7:66792017. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Guidelines for diagnosis and management of
cardiovascular sequelae in Kawasaki disease (JCS 2003). J Cardiol.
43:263–283. 2004.(In Japanese). PubMed/NCBI
|
|
16
|
Kalaria RN: Cerebrovascular disease and
mechanisms of cognitive impairment: evidence from
clinicopathological studies in humans. Stroke. 43:2526–2534. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Allen CL and Bayraktutan U: Risk factors
for ischaemic stroke. Int J Stroke. 3:105–116. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Bergström L, Irewall AL, Söderström L,
Ögren J, Laurell K and Mooe T: One-year incidence, time trends, and
predictors of recurrent ischemic stroke in Sweden from 1998 to
2010: an Observational Study. Stroke. 48:2046–2051. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Ntaios G, Dziedzic T, Michel P,
Papavasileiou V, Petersson J, Staykov D, Thomas B and Steiner T;
European Stroke Organisation, : European Stroke Organisation (ESO)
guidelines for the management of temperature in patients with acute
ischemic stroke. Int J Stroke. 10:941–949. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Arba F, Inzitari D, Ali M, Warach SJ, Luby
M and Lees KR; STIR/VISTA Imaging Collaboration, : Small vessel
disease and clinical outcomes after IV rt-PA treatment. Acta Neurol
Scand. 136:72–77. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Akutagawa N, Sadashima S, Nakagaki H,
Nagano S and Yoshimura T: Intracerebral hemorrhage after
intravenous recombinant tissue plasminogen activator (rt-PA)
therapy for acute cerebral infarction in a patient with
ANCA-associated vasculitis. Rinsho Shinkeigaku. 57:454–456. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Wang J, Wu N, Cham MD and Song Y: Tumor
response in patients with advanced non-small cell lung cancer:
Perfusion CT evaluation of chemotherapy and radiation therapy. AJR
Am J Roentgenol. 193:1090–1096. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Yoo AJ, Berkhemer OA, Fransen PSS, van den
Berg LA, Beumer D, Lingsma HF, Schonewille WJ, Sprengers MES, van
den Berg R, van Walderveen MAA, et al: MR CLEAN investigators:
effect of baseline Alberta Stroke Program Early CT Score on safety
and efficacy of intra-arterial treatment: a subgroup analysis of a
randomised phase 3 trial (MR CLEAN). Lancet Neurol. 15:685–694.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Finlayson O, John V, Yeung R, Dowlatshahi
D, Howard P, Zhang L, Swartz R and Aviv RI: Interobserver agreement
of ASPECT score distribution for noncontrast CT, CT angiography,
and CT perfusion in acute stroke. Stroke. 44:234–236. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Yu Y, Han Q, Ding X, Chen Q, Ye K, Zhang
S, Yan S, Campbell BC, Parsons MW, Wang S, et al: Defining core and
penumbra in ischemic stroke: A voxel- and volume-based analysis of
whole brain CT perfusion. Sci Rep. 6:209322016. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
van Seeters T, Biessels GJ, Kappelle LJ,
van der Schaaf IC, Dankbaar JW, Horsch AD, Niesten JM, Luitse MJ,
Majoie CB, Vos JA, et al Dutch acute stroke study (DUST)
investigators, : The prognostic value of CT angiography and CT
perfusion in acute ischemic stroke. Cerebrovasc Dis. 40:258–269.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Ma QF, Jia JP, Wu J, Xu EH, Yu YY, Lu J
and Zhang M: Relationship between computed tomography perfusion
imaging and prognosis in hyperacute cerebral infarction. Zhonghua
Yi Xue Za Zhi. 91:3337–3340. 2011.(In Chinese). PubMed/NCBI
|