Introduction
As important parts of the inner ring of the
pharyngeal lymphatic ring, the tonsil and the adenoid are the first
immune line of defense for the upper respiratory tract of the human
body. When children's immune function is low, tonsil and adenoid
tissues cause hypertrophy and chronic inflammation once stimulated
by external pathogens (1). In recent
years, children with tonsil and adenoid hypertrophy are very common
(2). Tonsil hypertrophy leads to
upper respiratory tract infection in children, and local
inflammation, thereby resulting in systemic diseases (3). It also causes poor breathing in
children, and even obstructive sleep apnea syndrome, which affects
the growth and development of children (4). Adenoid hypertrophy oppresses the
auditory tube that results in secretory otitis media (5). The excessive secretion of ear canal
blocks the nostrils, and causes sinusitis, rhinitis and other
complications of a series of adjacent organs, seriously affecting
the physical and mental health of children. With the advancement of
medical technology, tonsil hypertrophy and adenoid hyperplasia have
been gradually valued by number of parents. The low-temperature
plasma radiofrequency ablation technique is the most commonly used
for excising the tonsil and the adenoid (6).
Children undergoing pediatric operation have poor
operative compliance. The low-temperature plasma radiofrequency
ablation technique requires endotracheal intubation, which has a
larger intensity of operative stimulation, so deeper general
anesthesia is required for operation (7). At present, respiratory inhalation
anesthesia, and muscle, intravenous anesthesia are two commonly
used general anesthesia. Both of them finally inhibit the central
nervous system (8). Inhalation
anesthesia is the most commonly used anesthesia for pediatric
clinical operations. Sevoflurane is a widely used
fluorine-containing volatile inhalation general anesthetic in
clinical practice (9), with a blood
and air partition coefficient approximately between 0.60±0.07 and
0.686±0.047. With easy operation, stability during operation and
good controllability, it is easy to control anesthesia depth, with
less stimulation to the respiratory tract, so it is increasingly
used in clinical practice (10).
However, sevoflurane has an irritating effect on the central
nervous system, leading to frequent postoperative agitation
(11). Agitation may cause the
tearing of the operative wound in children, and physical harm to
them. Desflurane is a third-generation halogen new gas inhalation
general anesthesia, commonly used in pediatric operations for
anesthesia (12). It has almost no
effect on the circulatory system. The liver and the kidney in the
body are hardly involved in its metabolism, which has little impact
on the liver and kidney (13).
However, desflurane for anesthesia induction has airway irritation,
and easily cause laryngeal spasm, cough, increase in secretion, and
pharyngitis during anesthesia (14).
Therefore, desflurane is clinically less used for the anesthesia
induction in clinical practice but commonly used in children to
maintain anesthesia.
In the management of general anesthesia, anesthesia
recovery occupies a very important position, and the anesthesia
recovery quality widely concerns anesthesiologists. Important
aspects of good anesthesia recovery quality include low
postoperative pain, high comfort degree in children, no obvious
adverse reactions during the extubation period, stable breathing
after anesthesia recovery, short recovery and extubation time
(15). Therefore, in this study, a
retrospective analysis was performed on the effects of desflurane
and sevoflurane on the postoperative recovery quality after
tonsillectomy and adenoidectomy in children, to find anesthetic
drugs more suitable for tonsillectomy and adenoidectomy in
children, and provide clinical references.
Patients and methods
General information
A retrospective analysis was performed on the
clinical medical records of 165 children who underwent
tonsillectomy and/or adenoidectomy and were admitted to the Xuzhou
Children's Hospital, Xuzhou Medical University (Xuzhou, China) from
February 2014 to May 2017. Among them, 79 children were
anesthetized with sevoflurane as the sevoflurane group, with an
average age of 5.34±1.52 years. Another 86 children were
anesthetized with desflurane as the desflurane group, with an
average age of 5.46±1.45 years. The study was conducted after
approval by the Medical Ethics Committee of Xuzhou Children's
Hospital, Xuzhou Medical University. Both the family and the
patients were informed and the parents signed an informed consent
form.
Inclusion and exclusion criteria
Inclusion criteria: with tonsil or adenoid
hypertrophy; aged 3–7 years; with a body weight of 10–30 kg; male
or female. Exclusion criteria: those with dysgnosia; those with
respiratory inhibition diseases or bronchial asthma; those with
severe circulatory system or blood system dysfunction; those with a
history of anesthesia allergy.
Experimental methods
Children in the two groups were treated with
intravenous general anesthesia for the operation. Venous blood
collection was performed before operation to detect leukocytes and
other blood routine indicators. Twenty-four hours before the
operation, the responsible nurse punctured the indwelling needle to
establish an intravenous infusion channel for intraoperative use.
Six hours before the operation, all children were fasted. Four
hours before the operation, they were disallowed to consume any
liquids. At the day of operation, parents were required to
accompany children into the operation waiting area. When waiting,
the parents embraced the children and actively communicated with
them to relieve their tension and reduce their psychological
burdens. Individual children with preoperative agitation who did
not cooperate with the nurse to enter the operating room were
intravenously infused with atropine (Hubei Xinghua Pharmaceutical
Co., Ltd., Hubei, China, guoyaozhunzi: H42020590) 0.01 mg/kg, and
immediately with ketamine (Xi'an Hanfeng Pharmaceutical Co., Ltd.,
Xi'an, China, guoyaozhunzi: H20054748) 1 mg/kg 60 sec later. After
they were unconscious and fell asleep smoothly, children were taken
into the operating room. After entering the operating room, the
mask was immediately substituted with oxygen supply, and the
monitoring device was connected to detect the HR, electrocardiogram
(ECC), NIBP and SpO2 of children. After the monitoring
device was properly connected, children were intravenously
administered fentanyl (Sinopharm Group Industrial Co., Ltd.
Langfang Branch, Langfang, China, guoyaozhunzi: H20123297) 2 µg/kg,
and given rocuronium bromide (Zhejiang Xianju Pharmaceutical Co.,
Ltd., Zhejiang, China, guoyaozhunzi: H20123188) 0.4 mg/kg and
atracurium (Zhejiang Xianju Pharmaceutical Co., Ltd., guoyaozhunzi:
H20090202) 0.1 mg/kg 60 min later for the anesthesia induction. The
tracheal intubation was performed after drugs were fully effective.
Children in the sevoflurane group continued to be given sevoflurane
(Jiangsu Hengrui Pharmaceutical Co., Ltd., Jiangsu, China,
guoyaozhunzi: H2004077) at a concentration of approximately 2–3%
for anesthesia maintenance, children in the desflurane group were
given desflurane (Baxter Healthcare, Guayama, Puerto Rico,
guoyaozhunzi: H20090201) at a concentration of 6–10% for anesthesia
maintenance. An anesthesia apparatus was connected to regulate
children's breathing, and the operation began after the minimum
alveolar anesthetic concentration was controlled at 1.0–1.6, the
oxygen flow at 1–2 l/min, the respiratory rate at 20–28 times/min,
and the end-tidal carbon dioxide partial pressure maintained at
30–38 mmHg. After the operation, children were immediately stopped
from medication and sent to the anesthesia recovery room. Their
respiratory tract and oral secretions were cleaned up, and they
were cared for by dedicated medical staff. When children had
spontaneous breathing, with a respiratory rate ≥18 times/min and an
inhaled air SpO2 ≥95%, and had spontaneous limb
activity, cough and swallowing, they were considered as anesthesia
recovery. At this time, the tracheal catheter was extubated. When
children were completely awake, with stable vital signs, they were
sent back to the intensive care unit.
Outcome measures
Time required for each project of
operation
The time required from injection-induced anesthesia
to be effective (onset time of anesthesia), residence time in the
operating room (operation time), time required from entering the
anesthesia recovery room to anesthesia recovery (recovery time),
time required from anesthesia recovery to extubate the tracheal
catheter (extubation time) and time spent in the anesthesia
recovery room (coincidence time) of children in the two groups were
recorded.
Operative monitoring indicators
The NIBP, HR and SpO2 of children in the
two groups were recorded at t0, t1, t2, t3, t4, t5 and t6.
Evaluation criteria for postoperative
recovery quality
Postoperative sedation evaluation: According to
Ramsay score (16), the sedation
degree of children in the two groups was evaluated at c1, c2, c3,
c4 and c5. Postoperative pain evaluation: According to the MOPS
(17) criteria, the pain of children
in the two groups was evaluated at b1, b2, b3, b4, b5 and b6.
Postoperative agitation evaluation: According to the PAED (18) criteria, the agitation of children in
the two groups was evaluated at a1, a2, a3, a4, a5 and a6.
Statistical analysis
SPSS17.0 [Yiyun (Shanghai) Information Technology
Co., Ltd., Shanghai, China] was used for statistical analysis.
Measurement data were expressed as mean ± standard deviation (mean
± SD), and analyzed by t-test. Enumeration data were expressed as
rate (%), and Chi-square test was also used. P<0.05 was
considered to indicate a statistically significant difference.
Results
Baseline data of children
There were no significant differences in the sex,
age, height, weight, preoperative leucocyte value, preoperative
erythrocyte value, preoperative platelet value and preoperative
hemoglobin value of children between the sevoflurane group and the
desflurane group (P>0.05) (Table
I).
 | Table I.Comparison of general clinical data of
children in two groups [n (%)] (mean ± SD). |
Table I.
Comparison of general clinical data of
children in two groups [n (%)] (mean ± SD).
| Category | Sevoflurane group
(n=79) | Desflurane group
(n=86) | χ2/t
value | P-value |
|---|
| Sex |
|
| 0.108 | 0.756 |
| Male | 36 (45.57) | 37 (43.02) |
|
|
|
Female | 43 (54.43) | 49 (56.98) |
|
|
| Age (years) |
5.34±1.52 |
5.46±1.45 | 0.519 | 0.605 |
| Height (cm) | 105.35±23.24 | 103.93±24.71 | 0.379 | 0.705 |
| Weight (kg) | 21.34±6.33 | 22.01±7.19 | 0.633 | 0.528 |
| Preoperative
leucocyte (×109/l) | 21.46±5.38 | 22.84±5.82 | 1.577 | 0.117 |
| Preoperative
erythrocyte (×1012/l) |
4.65±0.31 |
4.58±0.36 | 1.333 | 0.184 |
| Preoperative platelet
(×109/l) | 342.45±98.46 |
338.48±101.93 | 0.254 | 0.800 |
| Preoperative
hemoglobin (g/l) | 125.95±18.54 | 128.51±16.38 | 0.942 | 0.348 |
Time required for each project of
operation in two groups of children
There was no significant difference in the onset
time of anesthesia of children between the sevoflurane group and
the desflurane group (t=1.122, P=0.264). Children in the desflurane
group had shorter operation time than those in the sevoflurane
group (t=2.192, P=0.030); shorter recovery time than those in the
sevoflurane group (t=2.711, P=0.007); shorter extubation time than
those in the sevoflurane group (t=3.382, P=0.001); shorter
coincidence time than those in the sevoflurane group (t=2.975,
P=0.003) (Table II).
 | Table II.Comparison of time required for each
project of operation between two groups of children (mean ±
SD). |
Table II.
Comparison of time required for each
project of operation between two groups of children (mean ±
SD).
| Category (min) | Sevoflurane group
(n=79) | Desflurane group
(n=86) | t value | P-value |
|---|
| Onset time of
anesthesia | 8.45±3.53 | 8.96±2.21 | 1.122 | 0.264 |
| Operation time | 38.75±10.86 | 35.43±8.54 | 2.192 | 0.030 |
| Recovery time | 16.43±6.99 | 13.83±5.27 | 2.711 | 0.007 |
| Extubation
time | 9.52±4.65 | 7.43±3.21 | 3.382 | 0.001 |
| Coincidence
time | 25.95±11.64 | 21.26±8.48 | 2.975 | 0.003 |
Operative monitoring indicators of
children in two groups
The results of the study showed that at t0, there
were no significant differences in the NISBP and NIDBP of children
between the sevoflurane group and the desflurane group (P>0.05).
At t1, t2, t3, t4, t5 and t6, children in the sevoflurane had
higher NISBP and NIDBP than those in the desflurane group
(P<0.05). At t0 and t6, there was no significant difference in
the HR of children between the sevoflurane group and the desflurane
group (P>0.05). At t1, t2, t3, t4 and t5, children in the
sevoflurane group had lower HR than those in the desflurane group
(P<0.05). At t0, t4, t5 and t6, there was no significant
difference in the SpO2 of children between the
sevoflurane group and the desflurane group (P>0.05). At t1, t2
and t3, children in the sevoflurane group had lower SpO2
than those in the desflurane group (P<0.05) (Fig. 1).
 | Figure 1.Comparison of life monitoring
indicators of children between the sevoflurane and desflurane
groups. At t0, there were no significant differences in the NISBP
and NIDBP of children between the sevoflurane and desflurane groups
(P>0.05). At t1, t2, t3, t4, t5 and t6, children in the
sevoflurane group had higher NISBP and NIDBP than those in the
desflurane group (P<0.05). At t0 and t6, there was no
significant difference in the HR of children between the
sevoflurane group and the desflurane group (P>0.05). At t1, t2,
t3, t4 and t5, children in the sevoflurane group had lower HR than
those in the desflurane group (P<0.05). At t0, t4, t5 and t6,
there was no significant difference in the SpO2 of
children between the sevoflurane group and the desflurane group
(P>0.05). At t1, t2 and t3, children in the sevoflurane group
had lower SpO2 than those in the desflurane group
(P<0.05). *P<0.05, compared to the sevoflurane group, the
difference is statistically significant. |
Postoperative sedation of children in
two groups
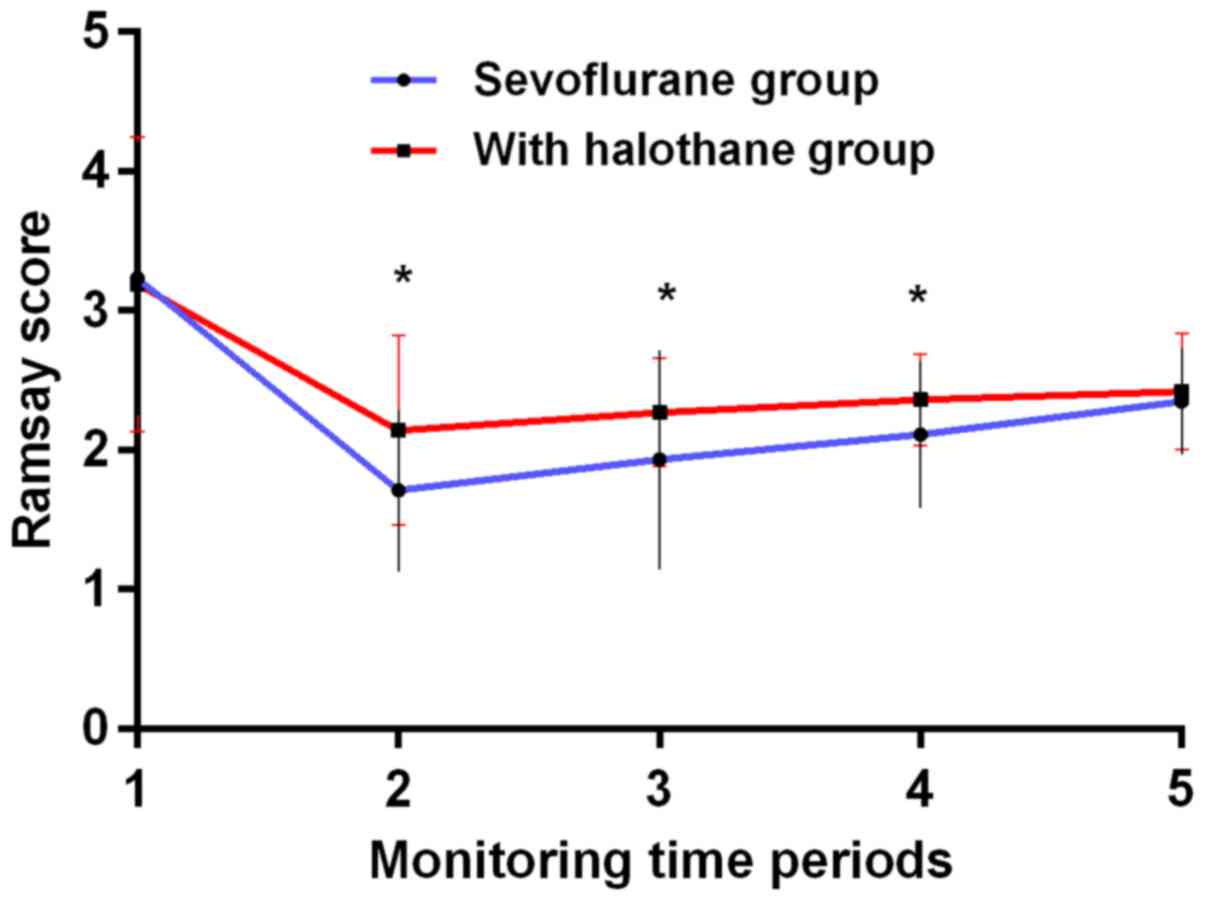
The results of the study showed that at c1 and c5,
there was no significant difference in the Ramsay scores of
children between the sevoflurane and desflurane groups (P>0.05).
At c2, the Ramsay score of children was (1.71±0.58) in the
sevoflurane group, lower than (2.14±0.68) in the desflurane group
(t=4.351, P<0.001). At c3, the Ramsay score of children was
1.93±0.79 in the sevoflurane group, lower than the 2.27±0.39 in
desflurane group (t=3.549, P=0.001). At c4, the Ramsay score of
children was 2.11±0.53 in the sevoflurane group, lower than the
2.36±0.33 in desflurane group (t=3.669, P<0.001) (Fig. 2).
Postoperative pain of children in the
two groups
The results of the study showed that at b1, b2 and
b6, there was no significant difference in the MOPS of children
between the sevoflurane group and the desflurane group (P>0.05).
At b3, the MOPS of children was 2.48±0.52 in the sevoflurane group,
higher than the 2.11±0.56 in the desflurane group (t=4.387,
P<0.001). At b4, the MOPS of children was 2.95±0.69 in the
sevoflurane group, higher than the 2.59±0.65 in the desflurane
group (t=3.451, P=0.001). At b5, the MOPS of children was 2.14±0.47
in the sevoflurane group, higher than the 1.65±0.38 in the
desflurane group (t=7.390, p<0.001) (Fig. 3).
Postoperative agitation of children in
the two groups
The results of the study showed that at a6, there
was no significant difference in the PAED scores of children
between the sevoflurane group and the desflurane group (P>0.05).
At a1, the PAED score of children was 2.99±1.23 in the sevoflurane
group, higher than the 2.04±1.03 in the desflurane group (t=5.394,
P<0.001). At a2, the PAED score of children was 4.72±1.79 in the
sevoflurane group, higher than the 3.53±1.28 in the desflurane
group (t=4.942, P<0.05). At a3, the PAED score of children was
3.47±1.36 in the sevoflurane group, higher than the 2.89±1.13 in
the desflurane group (t=2.988, P=0.003). At a4, the PAED score of
children was 2.87±0.59 in the sevoflurane group, higher than the
2.58±0.62 in the desflurane group (t=3.072, P=0.003). At a5, the
PAED score of children was 2.18±0.48 in the sevoflurane group,
higher than the 1.84±0.38 in the desflurane group (t=5.065,
P<0.001) (Fig. 4).
Discussion
In recent years, the number of children with tonsil
and adenoid hypertrophy has increased significantly. Clinically,
children with tonsil and adenoid hypertrophy are commonly treated
with resection. Children are in a critical period of body growth
and development, with poor compensation of the body and organ
system and have poor operative compliance. Therefore, they have
strong postoperative nociceptive stress response and emotional
response, with poor postoperative recovery quality. Failure to
obtain good postoperative recovery quality may lead to pain
aggravation in children, and a series of side effects such as
agitation, nausea, vomiting, and cerebral hypoxia, which may cause
irreversible long-term physical and mental damage to children and
prolong length of stay (19).
Clinically, the most commonly used inhalation
general anesthesia for the pediatric operation is desflurane and
sevoflurane. Desflurane, a fluoro-chlorinated compound of
isoflurane with low blood and air partition coefficient, low blood
solubility, quick recovery in children and good controllability, is
an ideal inhalation anesthetic in pediatric anesthesia (20). However, it is highly irritating to
the respiratory tract and cannot be used for anesthesia induction,
which is often used to maintain anesthesia clinically. Sevoflurane
has a fragrant smell, which is less irritating to the respiratory
tract, and has no inhibitory effect on the circulatory system.
Commonly used in younger children with poor treatment compliance,
it can be used for anesthesia induction and maintenance, widely
used in clinical practice (21).
However, postoperative agitation caused by sevoflurane in children
is very common (11). Sevoflurane is
also highly volatile, and the anesthetic waste gas pollutes the
environment, causing certain damage to the upper respiratory tract
health of medical staff (22).
The results of the current study showed that there
was no significant difference in the onset time of anesthesia of
children between the sevoflurane group and the desflurane group
(t=1.122, P=0.264). Children in the desflurane group had shorter
operation time than those in the sevoflurane group (t=2.192,
P=0.030); shorter recovery time than those in the sevoflurane group
(t=2.711, P=0.007); shorter extubation time than those in the
sevoflurane group (t=3.382, P=0.001); shorter coincidence time than
those in the sevoflurane group (t=2.975, P=0.003). This indicates
that children in the desflurane group have a smoother operation,
faster anesthesia recovery rate and better postoperative recovery
in the short-term than those in the sevoflurane group. At t0, there
were no significant differences in the NISBP and NIDBP of children
between the sevoflurane group and the desflurane group (P>0.05).
At t1, t2, t3, t4, t5 and t6, children in the sevoflurane group had
higher NISBP and NIDBP than those in the desflurane group
(P<0.05). The study by Lin et al (23) found that after tracheal intubation
with sevoflurane at a concentration of 8% for anesthesia
maintenance, patients' DBP increases significantly. This is similar
to our findings, indicating that sevoflurane has a certain impact
on human blood pressure. At t0 and t6, there was no significant
difference in the HR of children between the sevoflurane group and
the desflurane group (P>0.05). At t1, t2, t3, t4 and t5,
children in the sevoflurane group had lower HR than those in the
desflurane group (P<0.05). In the study by Ishibashi et
al (24), ketamine, sevoflurane
and propofol for pediatric anesthesia induction were compared. It
was found that the HR of children with sevoflurane for anesthesia
induction is lower than that of children with ketamine and
propofol. This is similar to our findings. Low HR can lead to a
decrease in myocardial oxygen consumption, thereby limiting the
contraction of peripheral blood vessels and resulting in
insufficient blood supply to the body, which is not conducive to
the postoperative recovery of children (25). At t0, t4, t5 and t6, there was no
significant difference in the SpO2 of children between
the sevoflurane group and the desflurane group (P>0.05). At t1,
t2 and t3, children in the sevoflurane group had lower
SpO2 than those in the desflurane group (P<0.05).
Pellis et al (26) monitored
patients who maintained anesthesia with desflurane and remifentanil
during laparoscopic gastric bypass surgery. No significant
fluctuation in the preoperative and postoperative SpO2
of patients was found. This is similar to our findings. In this
study, the SpO2 of children who maintained anesthesia
with desflurane was higher than that of children who maintained
anesthesia with sevoflurane. This indicates that desflurane has no
significant effect on the SpO2 level of children. The
World Health Organization stated that SpO2 less than 90%
can be regarded as hypoxemia in the body, which is not conducive to
the postoperative recovery of children (27). At c1 and c5, there was no significant
difference in the Ramsay scores of children between the sevoflurane
group and the desflurane group (P>0.05). At c2, c3 and c4,
children in the sevoflurane group had lower Ramsay scores than
those in the desflurane group (P<0.05). At a6, there was no
significant difference in the PAED scores of children between the
sevoflurane group and the desflurane group (P>0.05). At a1, a2,
a3, a4 and a5, children in the sevoflurane group had higher PAED
scores than those in the desflurane group (P<0.05). The
experimental results of Wang et al (28) show that if sevoflurane is used alone
for pediatric anesthesia, the incidence of pediatric agitation is
50%, and the excitement score is significantly higher than that of
children with propofol for anesthesia. Our results showed that
sevoflurane caused short-term agitation in children. However, with
their self-recovery, and the comfort of their parents and doctors
and nurses' care, their agitation gradually returned to normal. At
6 h after the tracheal catheter was extubated, the emotion of
children in the sevoflurane group was basically the same as that of
children in the desflurane group. Agitation during the
postoperative recovery will affect children's postoperative
recovery. Causing bleeding of the operative wound and physical
damage to children, children's struggle may even lead to asphyxia
and other serious life-threatening consequences. At b1, b2 and b6,
there was no significant difference in the MOPS of children between
the sevoflurane group and the desflurane group (P>0.05). At b3,
b4 and b5, children in the sevoflurane group had higher MOPS than
those in the desflurane group (P<0.05). It is speculated that
children in the sevoflurane group are more agitated after
operation, resulting in tearing of the wound and pain
aggravation.
In summary, more suitable as an anesthetic
maintenance drug for tonsillectomy and adenoidectomy in children,
desflurane has a better anesthetic effect and is safer. In
addition, children with desflurane anesthesia have high
postoperative recovery quality and quick recovery in the short
term, with better sedative and analgesic effects.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the present
study are available from the corresponding author on reasonable
request.
Authors' contributions
XW and CS were responsible for postoperative
recovery quality analysis. BP collected the patients' general data.
XS and FZ analyzed and interpreted NIBP, HR and SpO2. XW
and JC contributed to statistical analysis. All authors read and
approved the final manuscript.
Ethics approval and consent to
participate
The study was approved by the Ethics Committee of
Xuzhou Children's Hospital, Xuzhou Medical University (Xuzhou,
China). Patients who participated in this research, had complete
clinical data. Signed informed consents were obtained from the
parents of the child patients or the guardians.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Zagólski O: Why do palatine tonsils grow
back after partial tonsillectomy in children? Eur Arch
Otorhinolaryngol. 267:1613–1617. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Anuntaseree W, Rookkapan K, Kuasirikul S
and Thongsuksai P: Snoring and obstructive sleep apnea in Thai
school-age children: Prevalence and predisposing factors. Pediatr
Pulmonol. 32:222–227. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Gonzales R, Bartlett JG, Besser RE,
Hickner JM, Hoffman JR and Sande MA; Centers for Disease Control
and Prevention, : Principles of appropriate antibiotic use for
treatment of nonspecific upper respiratory tract infections in
adults: Background. Ann Emerg Med. 37:698–702. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Mitchell RB, Garetz S, Moore RH, Rosen CL,
Marcus CL, Katz ES, Arens R, Chervin RD, Paruthi S, Amin R, et al:
The use of clinical parameters to predict obstructive sleep apnea
syndrome severity in children: The Childhood Adenotonsillectomy
(CHAT) study randomized clinical trial. JAMA Otolaryngol Head Neck
Surg. 141:130–136. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Yazıcı H: Nasal mucociliary clearance in
adenoid hypertrophy and otitis media with effusion. Curr Allergy
Asthma Rep. 15:742015. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Karadağ S, Özkiriş M, Kubilay U and
Söyletir G: The effect of radiofrequency ablation on microbiology
of the tonsils. Int J Pediatr Otorhinolaryngol. 76:1654–1657. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Kim HJ, Park BK and Chung IS: Comparison
of general anesthesia and conscious sedation during computed
tomography-guided radiofrequency ablation of T1a renal cell
carcinoma. Can Assoc Radiol J. 69:24–29. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Wormald PJ, van Renen G, Perks J, Jones JA
and Langton-Hewer CD: The effect of the total intravenous
anesthesia compared with inhalational anesthesia on the surgical
field during endoscopic sinus surgery. Am J Rhinol. 19:514–520.
2005. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Kaskinoro K, Maksimow A, Georgiadis S,
Långsjö J, Scheinin H, Karjalainen P and Jääskeläinen SK:
Electroencephalogram reactivity to verbal command after
dexmedetomidine, propofol and sevoflurane-induced unresponsiveness.
Anaesthesia. 70:190–204. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Esper T, Wehner M, Meinecke CD and
Rueffert H: Blood/Gas partition coefficients for isoflurane,
sevoflurane, and desflurane in a clinically relevant patient
population. Anesth Analg. 120:45–50. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Guler G, Akin A, Tosun Z, Ors S, Esmaoglu
A and Boyaci A: Single-dose dexmedetomidine reduces agitation and
provides smooth extubation after pediatric adenotonsillectomy.
Paediatr Anaesth. 15:762–766. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Xu X, Zheng C, Li N, Shen H and Wang G:
The decrease of NMDAR subunit expression and NMDAR EPSC in
hippocampus by neonatal exposure to desflurane in mice. Behav Brain
Res. 317:82–87. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Demirel I, Ozer AB, Bayar MK and Erhan OL:
Anaesthesia management for acute appendicitis in cases with
Sjogren's syndrome accompanying autoimmune hepatitis. BMJ Case Rep.
2013(pii): bcr20120081112013.PubMed/NCBI
|
|
14
|
Yildirim H, Adanir T, Atay A, Katircioğlu
K and Savaci S: The effects of sevoflurane, isoflurane and
desflurane on QT interval of the ECG. Eur J Anaesthesiol.
21:566–570. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Zeng G, Zhao Z, Yang F, Zhong W, Wu W and
Chen W: Retrograde intrarenal surgery with combined spinal-epidural
vs general anesthesia: A prospective randomized controlled trial. J
Endourol. 29:401–405. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Hsu CW, Sun SF, Chu KA, Lee DL and Wong
KF: Monitoring sedation for bronchoscopy in mechanically ventilated
patients by using the Ramsay sedation scale versus auditory-evoked
potentials. BMC Pulm Med. 14:152014. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Buonsenso D, Barone G, Valentini P, Pierri
F, Riccardi R and Chiaretti A: Utility of intranasal Ketamine and
Midazolam to perform gastric aspirates in children: A double-blind,
placebo controlled, randomized study. BMC Pediatr. 14:672014.
View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Locatelli BG, Ingelmo PM, Emre S, Meroni
V, Minardi C, Frawley G, Benigni A, Di Marco S, Spotti A, Busi I,
et al: Emergence delirium in children: A comparison of sevoflurane
and desflurane anesthesia using the Paediatric Anesthesia Emergence
Delirium scale. Paediatr Anaesth. 23:301–308. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Yilmaz T, Koçan EG and Besler HT: The role
of oxidants and antioxidants in chronic tonsillitis and adenoid
hypertrophy in children. Int J Pediatr Otorhinolaryngol.
68:1053–1058. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Dalal KS, Choudhary MV, Palsania AJ and
Toal PV: Desflurane for ambulatory anaesthesia: A comparison with
sevoflurane for recovery profile and airway responses. Indian J
Anaesth. 61:315–320. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Amin AM, Mohammad MY and Ibrahim MF:
Comparative study of neuromuscular blocking and hemodynamic effects
of rocuronium and cisatracurium under sevoflurane or total
intravenous anesthesia. Middle East J Anaesthesiol. 20:39–51.
2009.PubMed/NCBI
|
|
22
|
Krenzischek DA, Schaefer J, Nolan M,
Bukowski J, Twilley M, Bernacki E and Dorman T: Phase I
collaborative pilot study: Waste anesthetic gas levels in the PACU.
J Perianesth Nurs. 17:227–239. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Lin TC, Lu CC, Kuo CK, Hsu CH, Huang GS,
Liu JY and Ho ST: Single vital-capacity and successive tidal-volume
breathing of sevoflurane in induction of anesthesia for tracheal
intubation in gynecologic patients. Acta Anaesthesiol Taiwan.
46:66–70. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Ishibashi H: More effective induction of
anesthesia using midazolam-butorphanol-ketamine-sevoflurane
compared with ketamine-sevoflurane in the common marmoset monkey
(Callithrix jacchus). J Vet Med Sci. 78:317–319. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Schaller BJ, Sandu N, Cornelius JF, Filis
A and Perez-Pinzon MA; Trigemino-Cardiac-Reflex-Examination-Group
(T.C.R.E.G.), : Oxygen-conserving implications of the
trigemino-cardiac reflex in the brain: The molecular basis of
neuroprotection? Mol Med. 15:125–126. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Pellis T, Leykin Y, Albano G, Zannier G,
Di Capua G, Marzano B and Gullo A: Perioperative management and
monitoring of a super-obese patient. Obes Surg. 14:1423–1427. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Yoder BA, Stoddard RA, Li M, King J,
Dirnberger DR and Abbasi S: Heated, humidified high-flow nasal
cannula versus nasal CPAP for respiratory support in neonates.
Pediatrics. 131:e1482–e1490. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Wang X, Jiang T and Zhao B: Effects of
different maintain doses of dexmedetomidine on plasma cortisol and
glucose during anesthesia recovery period in patients undergoing
uvulopalatopharyngoplasty under sevoflurane inhalation anesthesia.
Lin Chung Er Bi Yan Hou Tou Jing Wai Ke Za Zhi. 28:1154–1157.
2014.(In Chinese). PubMed/NCBI
|