Introduction
In cervical surgery, the pedicle screw technique has
demonstrated reliable biomechanical compatibility and a high rate
of bone fusion (1). However,
accurate placement of the screw is difficult, as the outer diameter
of the cervical pedicle is smaller than the thoracolumbar pedicle
(2). Furthermore, the cervical
pedicle has a large range of variation and adjoins the vertebral
artery, nerve root and spinal cord (3) Pedicle perforation from any direction is
associated with a considerable risk, intra-operative complications,
including the rupture of the bone wall, may decrease the clamping
force of the screw, and the rate of grade 2 and 3 screw perforation
is ~20% (4). A previous study has
demonstrated a low rate of intra-operative complications associated
with cervical pedicle screw fixation, but a high incidence of mild
to moderate screw deviation, which may cause complications
including the perforation of the pedicle wall, vertebral artery
injury, nerve root injury and spinal cord injury (5).
Therefore, the present study performed a detailed
applied anatomy investigation of the cervical pedicle and designed
a novel subaxial cervical pedicle screw placement device to
increase the accuracy of subaxial cervical pedicle screw placement
and to reduce the occurrence of complications during screw
placement.
Materials and methods
Structure of the guide device
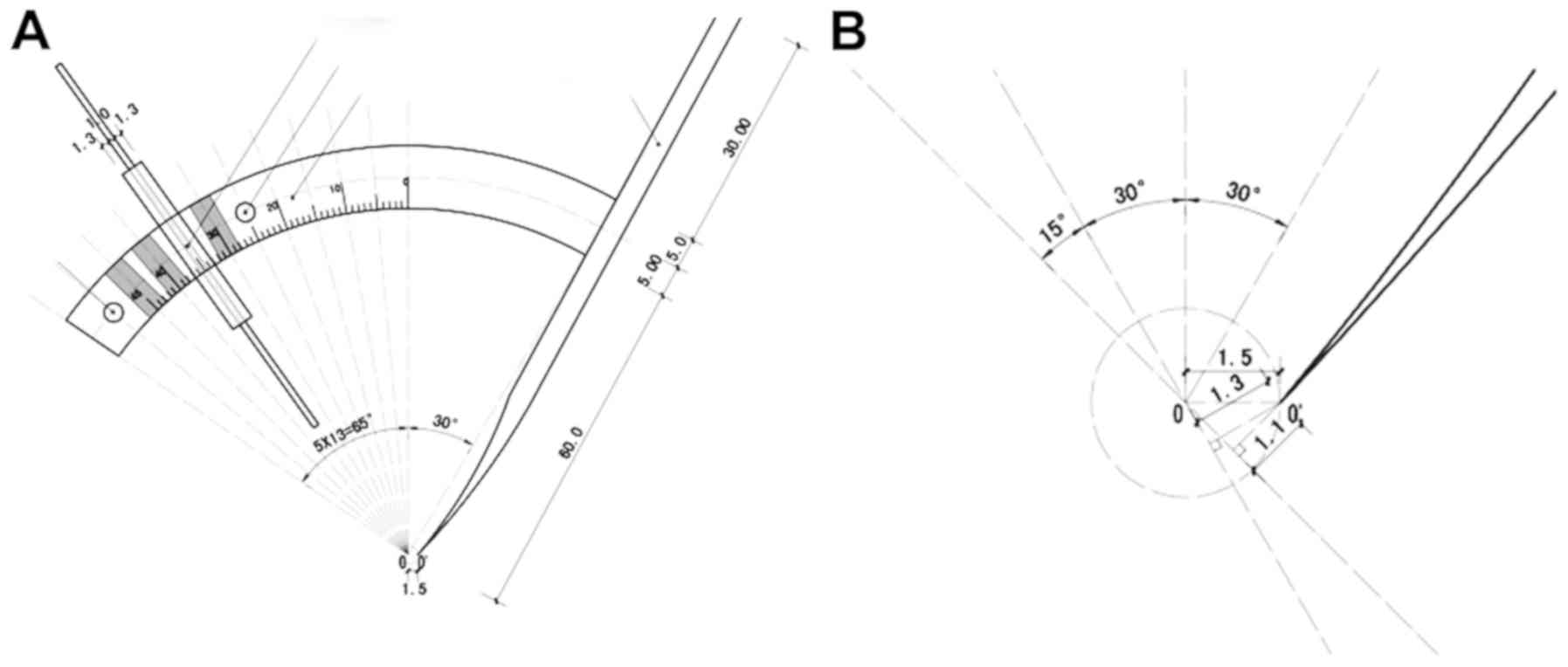
The subaxial cervical pedicle screw placement guide
device comprises two parts: The positioning and orientation. Its
structural features are presented in Fig. 1. The upper part of a fixed
positioning pin is connected to an arcuate sliding groove, the
center of which is located 1.5 mm from the tip of the fixed
positioning pin. The sliding groove is marked with a 0–45°
graduation, and two tightening screws are present at 30 and 45°,
respectively. These two tightening screws are used to tighten the
sliding groove and fix the working sleeve. Inside the sliding
groove, there are four working sleeve slots at 30, 35, 40 and 45°,
in which to place the working sleeve. The guide device is made of
surgical steel and produced by Suzhou Qingniu Medical Device Co.,
Ltd. (Suzhou, China) in strict accordance with the principles and
structural features of invention patent no. ZL200810123915.6.
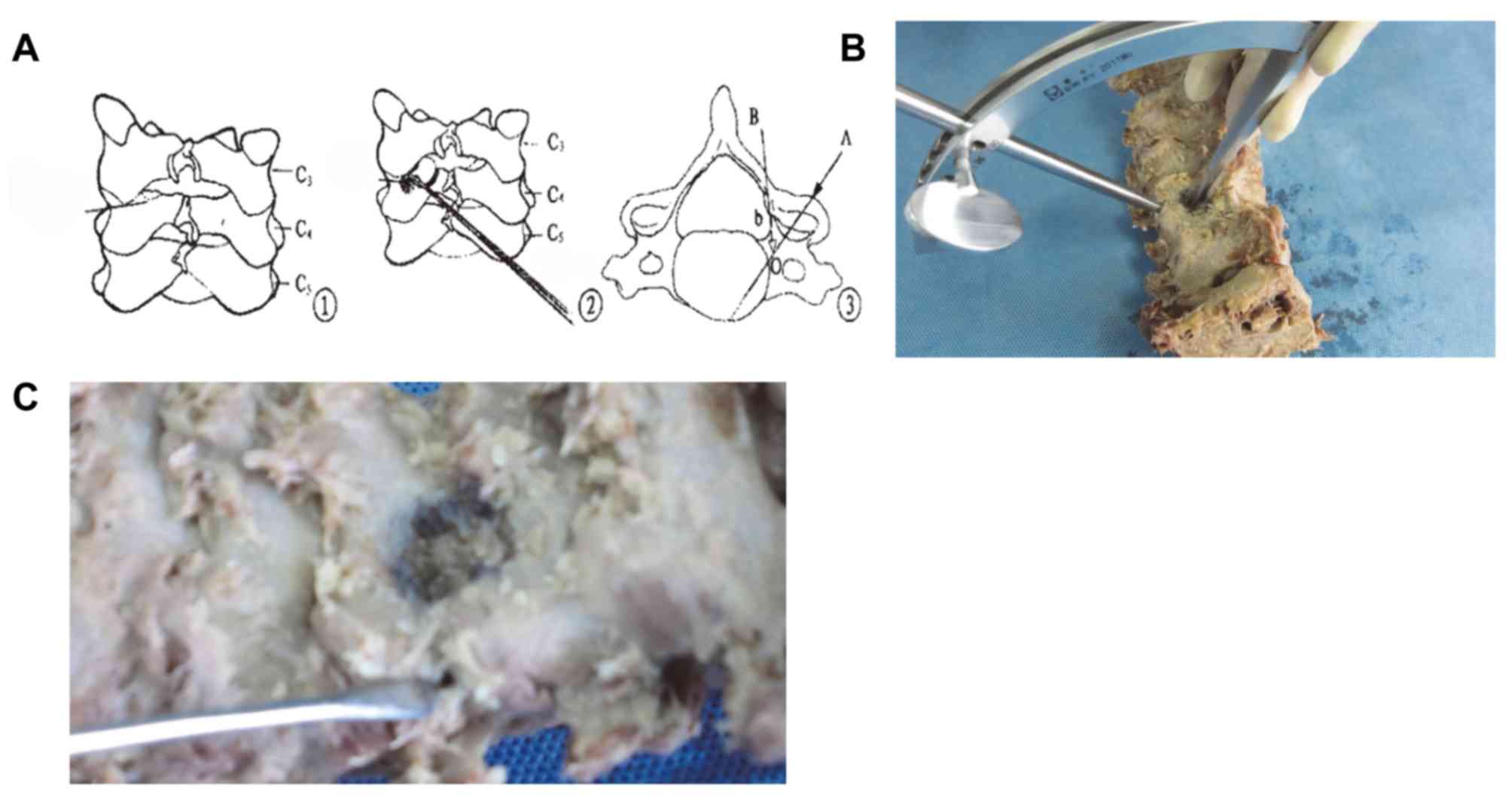
Preparation of specimens
Subaxial cervical specimens of 10 antiseptically
treated adult male human cadavers were selected (aged 60–80 years).
A longitudinal posteromedial incision was made to bilaterally
expose the outer edge of the facet joints. In total, 100 cervical
pedicles of 50 vertebral bodies (C3-C7) were measured. The
inclination and sagittal angles of the pedicle were measured via
the X-ray examination (Fig. 2). The
100 cervical pedicles were randomly divided into two groups
according to the different screw-setting techniques; in the guide
device group, the Subaxial Cervical Pedicle Screw Placement Guide
Device was used, and in the control group, the Abumi technique was
applied.
Subaxial cervical pedicle screw
placement guide device
The subaxial cervical pedicle screw placement guide
device (Fig. 3) was used in
combination with a keyhole partial laminectomy and tapping
technique (6). A keyhole
fenestration of ~5 mm was created between the fixed vertebral body
and adjacent vertebral plate for placement of the locator. After
identification of the medial, superior and inferior borders of the
pedicle, the positioning pin was fixed in the center of the medial
border of the pedicle. The direction of the working sleeve was
identified by regulating the direction of the fixed positioning pin
and the angle of the sliding groove. The inclination angle of the
working sleeve was 40–45° at C3-C6 and 30–40° at C7. The sagittal
angle of the working sleeve was parallel to the vertebral upper
endplate (caudally inclined to C3-C4 at an angle of ~10°,
resembling a pointed cone; cephalically inclined to C6-C7 at an
angle of ~10° and perpendicular to the posterolateral surface of
the C5 vertebral body). After the working sleeve had been fixed
with the tightening screw, the heading device of the pedicle was
rotated in the pedicle. Finally, a pedicle screw of suitable
diameter and length was implanted.
Abumi technique
After determining the position of the nail,
high-speed grinding is used to drill the bone cortex of the nail
point to create a suitable round hole. The diameter of the hole is
approximately equal to the screw neck, so that the entrance of the
pedicle canal may be seen directly. The small probe was moved into
the vertebral body by the pedicle of the medullary cavity under
X-ray C arm monitoring, after the pedicle screw entered slowly into
the pedicle. An inward tilt angle should be applied combined with
pre-operative computed tomography (CT) and intra-operative
assessment. Intra-operative lateral X-ray monitoring was used to
ensure that the probe is located in the pedicle and along the
probe, and inserted into the location and direction of tapping.
Combined with pre-operative CT, the distance of the pedicle to the
vertebral anterior, the pedicle medullary cavity diameter and
intraoperative examination were used select the appropriate pedicle
screw.
Statistical analysis
The success rate of the screw placement and the
incidence of bone wall, blood vessel, nerve root and spinal cord
injury were determined. The results were compared between the two
groups using the chi-square test. P<0.05 was considered to
indicate a statistically significant difference.
Results
Clinical outcomes
After the removal of the pedicle screws, the channel
wall of each pedicle screw was probed with a pedicle probe to check
the integrity of the screw channel wall. The vertebral body was
dissociated. The screw channel was directly observed after creation
of the incision (Fig. 4).
In the guide device group, 2 of the 50 pedicles (4%)
were perforated (C3 vertebral artery injury and C5 nerve root
injury, respectively). In the Abumi technique group, screw
placement failed in 8 of the 50 pedicles (16%; C3 nerve root
injury, C3 spinal cord injury, C4 nerve root injury, C4 vertebral
artery injury, C5 nerve root injury, C5 vertebral artery injury, C5
spinal cord injury and C6 nerve root injury, respectively; Table I).
 | Table I.Incidence of failure in the two groups
(n=50). |
Table I.
Incidence of failure in the two groups
(n=50).
| Type | Control group | Guide device
group |
X2 | P-value |
|---|
| Perforation of
pedicle wall | 8 (16) | 2 (4) | 4.00 | 0.046 |
| Vertebral
artery injurya | 2 (4) | 1 (2) |
|
|
| Nerve
root injurya | 4 (8) | 1 (2) |
|
|
| Spinal
cord injurya | 2 (4) | 0 (0) |
|
|
Statistical analysis
The chi-squared test revealed that the screws had
been correctly implanted. However, the success rate of screw
placement in the left pedicle (treated with the guide device) was
significantly higher than that in the right pedicle (treated
without the guide device; chi2=4.00, P<0.05).
The incidence of perforation of the pedicle wall, as
well as the vascular injury, nerve root injury and spinal cord
injury resulting from it, was recorded in Table I.
Discussion
Prior to the development of subaxial cervical
pedicle screw fixation, a large number of studies had assessed the
three-dimensional morphology of the subaxial cervical pedicle. For
instance, Reinhold et al (7)
indicated that the coronal plane of the subaxial cervical pedicle
is elliptical, and its inner width is shorter than its height. They
also reported that the internal width of the pedicle gradually
increased from C3 to C7. The width of C3, C4, C5 and C6 ranged from
4.2 to 5.6, 4.4 to 5.4, 4.7 to 5.6 and 4.7 to 6.5 mm, respectively.
However, the height of C3, C4, C5, C6 and C7 did not exhibit any
substantial variation. Karaikovic et al (8) identified that only a small proportion
of the subaxial cervical pedicles had no medullary cavity.
The front part of the subaxial cervical pedicle
connects to the upper posterolateral vertebral body, and the back
connects to the upper lateral mass. The entry site of the pedicle
screw is located at the intersection of the vertical center line
and horizontal midline through the upper 1/4 of the lateral mass
(9). The axis of the subaxial
cervical pedicle at the C3-C4 level is relatively close to the
upper endplate, but is slightly lower at C5-C7 (10). The anterior border of the upper
endplate of the subaxial cervical pedicle is a slope. If the
pedicle screw is too long, it may perforate the upper endplate when
implanted along the axis of the pedicle.
In a study by Yukawa et al (11), the inclination angle of the subaxial
cervical pedicle was 41.6–49.4°. The effective width of the screw
channel is maximal when the inclination angle of the subaxial
cervical pedicle screw channel is identical to the inclination
angle of the pedicle itself (12).
The medial wall of the subaxial cervical pedicle is
thin (13,14); thus, its resistance to external force
is relatively low (15). Previous
studies have suggested that the medial wall of certain subaxial
cervical pedicles has a nourishing vessel entrance that results in
congenital bone defects and reduced bone strength of the pedicle
(16).
The height and width of the transverse foramen
gradually increases from C3 to C6. The vertebral artery generally
originates from the subclavian artery and enters the transverse
foramen of C6, while some enter the transverse foramen at C3-C5 and
C7 (17). The ertebral artery is
surrounded by a venous sinus and distributes into the transverse
foramen. The portion of the transverse foramen that is not
traversed by the vertebral artery is relatively small (18).
The cervical nerve root tightly attaches to the
inferior border of the intervertebral foramina and distributes
forward and outward. The subaxial cervical pedicle, upper nerve
root, and dural sac mostly attaches to one another at 1.0–2.5 mm
from the lower nerve root. The cervical cord is packed within the
dural sac and surrounded by cerebrospinal fluid, resulting in a
great distance between the cervical cord and the pedicle (19). The anatomy of the subaxial cervical
pedicle is controversial among researchers worldwide due to
differences in ethnicity, sex and age, the dryness and storage
period of the specimens and the methods of measurement (20,21).
In 1991, Panjabi et al (22) determined the three-dimensional
anatomical morphology of the human cervical pedicle and reported
that pedicle screw fixation was successfully performed. In 1998,
Wang et al (13) provided the
measurement results of cervical specimens of 54 adult Chinese
patients. The inclination angle at C3, C4, C5, C6 and C7 was 42.97,
44.28, 44.80, 42.26 and 35.23°, respectively. The sagittal angle
(positive above the horizontal line and negative below the
horizontal line) at C3, C4, C5, C6 and C7 was −5.16, −0.32, 2.40,
5.00 and 5.47°, respectively. In 1994, Abumi (1) reported the application of pedicle screw
fixation in the treatment of subaxial cervical spine injury and
obtained satisfactory clinical outcomes. In 2000, Abumi (23) reported on various complications
associated with cervical pedicle fixation.
Ludwig et al (24) studied 67 pedicles at C3-C7 from 7
patients using the Abumi technique and obtained an overall pedicle
cortical penetration rate of 40.3% (mild, 28.4%; severe, 11.9%) and
an overall success rate of 88.0% (placement within pedicle, 59.7%;
slight penetration of cortex, 28.4%). Abumi et al (23) performed cervical pedicle screw
placement in 180 patients using a total of 669 screws.
Post-operative CT revealed that 45 screws (6.7%) penetrated the
pedicle; 1 patient developed vertebral artery injury and 2
developed neurological symptoms.
The standards of subaxial cervical pedicle screw
placement are not uniform. Five methods are currently utilized: The
Abumi technique, the standard pedicle screw method, the partial
laminectomy pedicle probe method, the dredging pipe method and
three-dimensional computer navigation. As the classic Abumi
technology has been used in our department for cervical screw
placement, a group treated with the Abumi technique was used in the
present study as a control. The Abumi technique involves partial
removal of cortical and cancellous bone from the back of the
lateral mass to expose the pedicle entrance, and the screw is then
inserted either by direct visualization or under X-ray
fluoroscopy.
The standard pedicle screw method involves
identification of the pin entrance site and direction of entry
according to anatomical landmarks. This technique may utilize a
variety of positioning methods, all of which have common features.
For instance, the pin entrance site is located within the outer
quadrant superior to the cervical lateral mass. The inclination
angle is 30–45°. The sagittal angle is negative at C3-C4, 0° at C5
and positive at C6-C7 (25).
The dredging pipe method was described in 2001 by
Karaikovic et al (8).
Specifically, the cortical bone of the lateral mass is removed at
the site of pin entrance by a rongeur or bone drill. The cancellous
bone is removed by a curette with a 2- to 3-mm diameter rotated
along the axis of the pedicle, exposing the flared pedicle
entrance. Cancellous bone in the pedicle tube is then scraped in a
rotating manner with the curette. The depth of the pedicle tube is
3–5 mm under direct visualization. If any resistance is
encountered, the direction may be slightly adjusted. If screwing is
still not possible, a new pin entrance site should be selected.
Upon penetration of the pedicle tube, the screw is inserted along
the medullary cavity. Ebrahein et al (26) first reported fenestration and
laminectomy in 1997. The vertebral plate was partially removed to
directly probe the position of or to expose the pedicle. Thus, the
pedicle may can be safely inserted under direct visualization.
Fenestration and laminectomy increases the accuracy of pedicle
screw placement, but exposes the cervical cord, which may then be
inadvertently injured. Three-dimensional computer navigation
includes computer processing of the results of three-dimensional
C-arm X-ray fluoroscopy and establishment of three-dimensional
dynamic images to navigate the pedicle screw placement during the
operation, thus increasing the safety of pedicle screw
placement.
The criteria to evaluate the screw position differ
among previous studies. Neo et al (15) classified the screw position into four
grades: Grade 0, correct entrance of the screw channel along the
axis of the subaxial cervical pedicle; grade 1, screw channel
displacement of <2 mm; grade 2, screw channel displacement of
>2 and <4 mm; and grade 3, screw channel displacement of
>4 mm. Yoshimoto et al (27) defined partial screw perforation as a
displacement distance of <0.5 times the screw diameter and
complete screw perforation as a displacement a distance of >0.5
times the screw diameter. Kast et al (28) defined correct screw placement as ≤1
mm penetration of the subaxial cervical pedicle into the cortex,
mild screw perforation as perforation that occurred lateral or
anterior to the vertebral body or occupied the spinal lateral
recess, did not contact the dural sac or extended outward to induce
vertebral artery stenosis, and was <1/4 the diameter, and severe
perforation as >25% involvement of the vertebral artery or the
occurrence of downward perforation-induced potential nerve
compression or injury. Reinhold et al (7) classified screw placement results into
four grades: Grade I, the subaxial cervical pedicle screw is
located at the center of the pedicle; grade IIa, the subaxial
cervical pedicle screw penetrates the medial wall of the pedicle,
but the displacement is <1/4 of the screw diameter; grade IIb,
the displacement distance of the subaxial cervical pedicle screw is
>1/4 of the screw diameter and the screw does not contact
peripheral nerves or blood vessels; and grade III, the displacement
distance is >1/4 of the screw diameter and the screw is attached
to peripheral nerves and blood vessels.
The subaxial cervical pedicle screw placement guide
device is able to probe the midpoint of the medial wall of the
cervical pedicle using the fixed positioning pin. The guide sleeve
was adjusted and fixed according to the angle measured by
pre-operative X-ray fluoroscopy and multi-slice spiral CT. The
working sleeve was connected to the sliding groove using the
tightening screw. The ability to individually regulate the pin
entrance angle for each vertebral body and guide the placement of
the fixed positioning pin greatly assists clinicians in overcoming
factors of uncertainty during screw placement. Thus, accurate and
relatively safe screw placement may be achieved using the subaxial
cervical pedicle screw placement guide device.
This guide device combined with the keyhole partial
laminectomy and tapping technique allows the medial wall of the
pedicle to be probed under direct visualization and facilitates
assessment of the pin entrance site and direction. The design core
concentrates on an arcuate sliding groove. The distance (OO′)
between the center of the sliding groove and the tip of the fixed
positioning pin is 1.5 mm (Fig. 5).
At various pin entrance angles, the vertical distance between the
tip of the fixed positioning pin and the line of the pin entrance
direction is ≥1.1 mm (it is precisely 1.1 mm when the pin entrance
angle is 45°). After measuring the thickness of the cortical bone
in the medial wall of the subaxial cervical pedicle, >1.1 mm was
the safest measurement that ensured the screw did not penetrate the
medial wall due to the junction of the different intensities of
cortical and cancellous bones in the pedicle. Only 2 cases of screw
perforation occurred in the guide device group of the present
study.
However, the design of the subaxial cervical pedicle
screw placement guide device has certain limitations. The direction
of the guide sleeve should be adjusted according to the angle
measured by pre-operative X-ray fluoroscopy and CT. The inclination
angle may be fixed by adjusting the position of the guide sleeve on
the sliding groove, but the sagittal angle must be artificially
adjusted according to the pre-operative evaluation. The outcomes
are associated with the experience of the surgeon and the accuracy
of the pre-operative CT evaluation. In addition, the precision of
the guide device affects the direction of the guide sleeve. The
midpoint of the medial wall of the pedicle is more readily
identified by surgeons with greater experience. Based on the
current study's operational experience in surgery, displacement may
interfere with the direction of the guide device.
In the present study, two pedicles (4%) in the guide
device group were perforated, causing external injury in one case
and inferior injury in the other. When the vertebral body was
horizontally cut after completion of the procedure, it was revealed
that the abovementioned injuries had been induced due to the
direction from which the pin had been inserted, i.e., the pin
entrance angle was too large. However, further in-depth studies are
still required to address these issues.
In conclusion, application of the subaxial cervical
pedicle screw placement guide device is more accurate and safer
than previous techniques. This guide device overcomes certain
anthropic factors during screw placement and ensures for an
individually optimal pin entrance. However, further in-depth
studies are required to reduce screw placement errors.
Acknowledgements
Not applicable.
Funding
No funding received.
Availability of data and materials
The analyzed data sets generated during the study
are available from the corresponding author on reasonable
request.
Authors' contributions
The final version of the manuscript has been read
and approved by all authors, and each author believes that the
manuscript represents honest work.
Ethical approval and consent to
participate
The current study was approved by the Medical Ethics
Board of Nanjing Hospital Affiliated to Nanjing Medical University
(Nanjing, China). Informed consent was obtained from the families
of the patients.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Abumi K, Itoh H, Taneichi H and Kaneda K:
Transpedicular screw fixation for traumatic lesions of the middle
and lower cervical spine: Description of the techniques and
preliminary report. J Spinal Disord. 7:19–28. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Nishizawa K, Mori K, Nakamura A and Imai
S: Novel landmark for cervical pedicle screw insertion point from
computed tomography-based study. Asian Spine J. 11:82–87. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Deng T, Jiang M, Lei Q, Cai L and Chen L:
The accuracy and the safety of individualized 3D printing screws
insertion templates for cervical screw insertion. Comput Assist
Surg (Abingdon). 21:143–149. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Uehara M, Takahashi J, Ikegami S, Kuraishi
S, Futatsugi T and Kato H: Screw perforation rates in 359
consecutive patients receiving computer-guided pedicle screw
insertion along the cervical to lumbar spine. Eur Spine J.
26:2858–2864. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Schnake KJ, Tropiano P, Berjano P and
Lamartina C: Cervical spine surgical approaches and techniques. Eur
Spine J. 25 (Suppl 4):S486–S487. 2016. View Article : Google Scholar
|
|
6
|
Wu Z, Wei Y and Yu L: Analysis and
prevention of the direction error of transpedicular fixation for
the cervical spinal fracture. Chin J Spine Spinal Cord. 14:178–179.
2004.(In Chinese).
|
|
7
|
Reinhold M, Magerl F, Rieger M and Blauth
M: Cervical pedicle screw placement: Feasibility and accuracy of
two new insertion techniques based on morphometric data. Eur Spine
J. 16:47–56. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Karaikovic EE, Yingsakmongkol W and Gaines
RW Jr: Accuracy of cervical pedicle screw placement using the
funnel technique. Spine (Phila Pa 1976). 26:2456–2462. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Bozbuga M, Ozturk A, Ari Z, Sahinoglu K,
Bayraktar B and Cecen A: Morphometric evaluation of subaxial
cervical vertebrae for surgical application of transpedicular screw
fixation. Spine (Phila Pa 1976). 29:1876–1880. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Chazono M, Soshi S, Inoue T, Kida Y and
Ushiku C: Anatomical considerations for cervical pedicle screw
insertion: The use of multiplanar computerized tomography
reconstruction measurements. J Neurosurg Spine. 4:472–477. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Yukawa Y, Kato F, Yoshihara H, Yanase M
and Ito K: Cervical pedicle screw fixation in 100 cases of unstable
cervical injuries: Pedicle axis views obtained using fluoroscopy. J
Neurosurg Spine. 5:488–493. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Richter M, Cakir B and Schmidt R: Cervical
pedicle screws: Conventional versus computer-assisted placement of
cannulated screws. Spine (Phila Pa 1976). 30:2280–2287. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Wang D, Tang T and Huang S: Anatomical
study and clinical application of pedicle screw fixation in lower
cervical spine. Chin J Orthop. 11:659–662. 1998.(In Chinese).
|
|
14
|
Cervical pedicle screw instrumentation is
more reliable with O-arm-based 3D navigation, . analysis of
cervical pedicle screw placement accuracy with O. European Spine
Journal. 27:2729–2736. 2018.PubMed/NCBI
|
|
15
|
Neo M, Fujibayashi S, Miyata M, Takemoto M
and Nakamura T: Vertebral artery injury during cervical spine
surgery: A survey of more than 5600 operations. Spine (Phila Pa
1976). 33:779–785. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Tse MS, Chan CH, Wong KK and Wong WC:
Quantitative anatomy of C7 vertebra in Southern Chinese for
insertion of lateral mass screws and pedicle screws. Asian Spine J.
10:705–710. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Sanelli PC, Tong S, Gonzalez RG and Eskey
CJ: Normal variation of vertebral artery on CT angiography and its
implications for diagnosis of acquired pathology. J Comput Assist
Tomogr. 26:462–470. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Bruneau M, Cornelius JF, Marneffe V,
Triffaux M and George B: Anatomical variations of the V2 segment of
the vertebral artery. Neurosurgery 59 (1 Suppl 1). ONS20–ONS24.
2006.
|
|
19
|
Simsek S, Uz A, Er U and Apaydin N:
Quantitative evaluation of the anatomical parameters for subaxial
cervical spondylectomy: An anatomical study. J Neurosurg Spine.
18:568–574. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Munusamy T, Thien A, Anthony MG,
Bakthavachalam R and Dinesh SK: Computed tomographic morphometric
analysis of cervical pedicles in a multi-ethnic Asian population
and relevance to subaxial cervical pedicle screw fixation. Eur
Spine J. 24:120–126. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Al-Saeed O, Marwan Y, Kombar OR, Samir A
and Sheikh M: The feasibility of transpedicular screw fixation of
the subaxial cervical spine in the Arab population: A computed
tomography-based morphometric study. J Orthop Traumatol.
17:231–238. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Panjabi MM, Duranceau J, Goel V, Oxland T
and Takata K: Cervical human vertebrae. Quantitative
three-dimensional anatomy of the middle and lower regions. Spine
(Phila Pa 1976). 16:861–869. 1991. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Abumi K, Shono Y, Ito M, Taneichi H,
Kotani Y and Kaneda K: Complications of pedicle screw fixation in
reconstructive surgery of the cervical spine. Spine (Phila Pa
1976). 25:962–969. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Ludwig SC, Kowalski JM, Edwards CC II and
Heller JG: Cervical pedicle screws: Comparative accuracy of two
insertion techniques. Spine (Phila Pa 1976). 25:2675–2681. 2000.
View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Aoude AA, Fortin M, Figueiredo R, Jarzem
P, Ouellet J and Weber MH: Methods to determine pedicle screw
placement accuracy in spine surgery: A systematic review. Eur Spine
J. 24:990–1004. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Ebraheim NA, Xu R, Knight T and Yeasting
RA: Morphometric evaluation of lower cervical pedicle and its
projection. Spine (Phila Pa 1976). 22:1–6. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Yoshimoto H, Sato S, Hyakumachi T,
Yanagibashi Y and Masuda T: Spinal reconstruction using a cervical
pedicle screw system. Clin Orthop Relat Res. 111–119. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Kast E, Mohr K, Richter HP and Börm W:
Complications of transpedicular screw fixation in the cervical
spine. Eur Spine J. 15:327–334. 2006. View Article : Google Scholar : PubMed/NCBI
|