Introduction
Cervical carcinoma is the second most common
malignant tumor type in females, accounting for 527,600 newly
diagnosed cases and 265,700 deaths worldwide in 2012 (1). The neoplasm is most frequently caused
by persistent infection with high-risk human papillomavirus (HPV),
leading to slow and progressive infiltration (2,3).
Usually, the process of cervical carcinogenesis takes 10 years or
longer (2,3). Regular and frequent cervical carcinoma
screening and early diagnostic approaches have become the most
critical tools for preventing the progression of pre-cancerous
lesions to cervical carcinoma (4).
Colposcopy is a visual technique that is extensively used to
collect cervical tissue samples and identify cervical lesions.
However, the application of colposcopy is limited by the skills and
experience of clinical staff (5).
Furthermore, the selection of the biopsy site is always subjective
and affects the determination of the histological type based on
visual changes (6). Due to the above
reasons, the accuracy rate of the determination of cell
morphological changes and mild nuclear abnormalities is limited. At
present, the predictive rate for severe pre-cancerous lesions is
<55% in the clinic (7). Aberrant
cell morphology and mild nuclear abnormalities always induce
atypical squamous cells of undetermined significance
(ASCUS)/atypical squamous cells-cannot exclude high-grade squamous
intraepithelial lesion (ASC-H)/low-grade squamous intraepithelial
lesion (LSIL). Furthermore, high-grade squamous intraepithelial
lesions (HSIL) are considered severe pre-cancerous lesions
(8).
The dynamic spectral imaging (DySI) colposcope is a
digital-video colposcope integrating standard colposcopy with
adjunctive DySI cervical mapping (9). DySI has a relatively higher sensitivity
for detecting severe pre-cancerous lesions [defined as lesions
covering >2/3 of the total uterine neck and cervical
intraepithelial neoplasia 2+ (CIN2+)] (10). Soutter et al (11) reported that the diagnostic efficacy
for CIN2+ lesions by DySI is significantly higher compared with
that of traditional colposcopy in patients with cytological
abnormalities. In 2013, the American Cancer Society updated their
screening guidelines for the early detection of cervical carcinoma
and pre-cancerous lesions (12), to
recommend the cytological technique as the discriminant diagnostic
tool for high-risk (hr)HPV-positive patients according to the World
Health Organization Guidelines (13). At present, the determination of hrHPV
is considered as an alternative method after the cytological
examination, while the colposcopy examination is performed directly
for those patients with severe cytological results (14).
In the present study, the diagnostic efficacy of
DySI, traditional colposcopy and their combination was first
evaluated. Subsequently, two different screening methods of
traditional colposcopy, namely hrHPV examination as the
pre-screening method and cytological examination combined with
determination of the hrHPV, were compared. The results revealed
that the combined application of the DySI technique and traditional
colposcopy exhibited a higher sensitivity compared with that of
traditional colposcopy alone for the detection of pre-cancerous
cervical lesions in subjects with an abnormal cytological
result.
Materials and methods
Patients
The present retrospective study included 146
patients diagnosed with cervical lesions and ASCUS on colposcopy
examination. The inclusion criteria were an age of >18 years,
and an abnormal screening test result [referral from cervical
screening to the colposcopy unit due to an abnormal cervical
cytological result]. Patients fulfilling the following criteria
were excluded: i) Known pregnancy, ii) human immunodeficiency virus
infection, iii) acquired immune deficiency syndrome, iv)
hysterectomy and v) radiation treatment or chemotherapy.
DySI examination
The DySI system used in the present study was a
DySIS v2.1 purchased from Forth Photonics Ltd. (Livingston, UK).
This technique allowed for visualization of the cervix during a
colposcopic examination and measurement or mapping the dynamics of
the acetowhitening effects for each point of the cervix, to finally
provide a per-point analysis of the acetowhitening effects.
Upon addition of 3% acetic acid, the evaluation of
acetowhitening effects by DySI commenced automatically. Although
the acquisition period continued for ~3 min, the acetowhitening
effects persisted for longer (15).
When the examination was completed, the DySI information was
concisely illustrated with a color-coded map. The color-coded map
was overlaid with the color images for the vertical tissues to
facilitate the identification of the location of cervical lesions
and determine the severity. The DySI procedure was performed
according to the manufacturer's protocols.
hrHPV screening
The patients were instructed to refrain from sexual
activity and washing of the vagina, and no drugs were applied and
no other surgeries of the cervix and vagina were performed for 3
days prior to the HPV screening. The cervix was exposed by with a
speculum and a HPV sampler was used to obtain the specimens. The
specimens were preserved in PBS and ready to be detected in the
laboratory. hrHPV was assessed in the cervical specimens by
employing the GP5+/6+ polymerase chain reaction enzyme immunoassay
according to the protocols of previous studies (16,17).
Evaluation of clinical presentation by
two different strategies
The patients of the present study were divided into
two groups that were subjected to different evaluation strategies
prior to colposcopy and/or DySI (18). First, hrHPV examination was used as
the pre-screening experiment. If the hrHPV test was positive, the
patients were separated and then subjected to the diagnostic
procedures. Meanwhile, the hrHPV negative patients were also
subjected to the diagnostic procedures for consistency.
Furthermore, hrHPV examination was used as the criterion for
classification examination. If patients had a critical cell
morphology or mild nuclear abnormalities and an hrHPV-positive
status, the patients were separated and then subjected to the
diagnostic procedures. The hrHPV negative patients were also
subjected to the diagnostic procedures. If the patients'
cytological results indicated a morphology of highly diseased
cells, the patients were selected directly and subjected to the
diagnostic procedures immediately.
Trial grouping
According to the presence of abnormal nuclear
morphology and the degree of pre-cancerous lesions, the patients
were divided into an ASCUS/ASC-H/LSIL group (n=93), HSIL group
(n=53) and HSIL/hrHPV-negative group (n=13). Furthermore, all three
groups were subdivided into a routine colposcopy group, DySI group
and combined diagnosis by DySI and routine colposcopy group. In
addition, the patients were divided into two groups that were
subjected to different evaluation strategies to examine the
clinical presentation prior to colposcopy. For the Method 1 group
(n=110), the hrHPV examination was used as the pre-screening
experiment, and for the Method 2 group (n=124), hrHPV examination
was used as a criterion for classification examination (cytology
analysis). Each of the two groups was sub-divided into a routine
colposcopy group, a DySI group and a combined diagnosis by DySI and
routine colposcopy group.
Statistical analysis
All of the data were analyzed by using SPSS software
19.0 (IBM Corp., Armonk, NY, USA). Quantitative data are expressed
as the mean ± standard deviation. Categorical variables, including
sensitivity and specificity (expressed as percentages, %), were
analyzed by using a Chi-square test. Receiver operating
characteristic curves were employed to evaluate the sensitivity and
specificity of the routine colposcopy method, DySI and the combined
diagnostic method, according to previously published studies
(19,20). All of the data were obtained from at
least six independent tests or experiments. P<0.05 was
considered to indicate a statistically significant difference.
Results
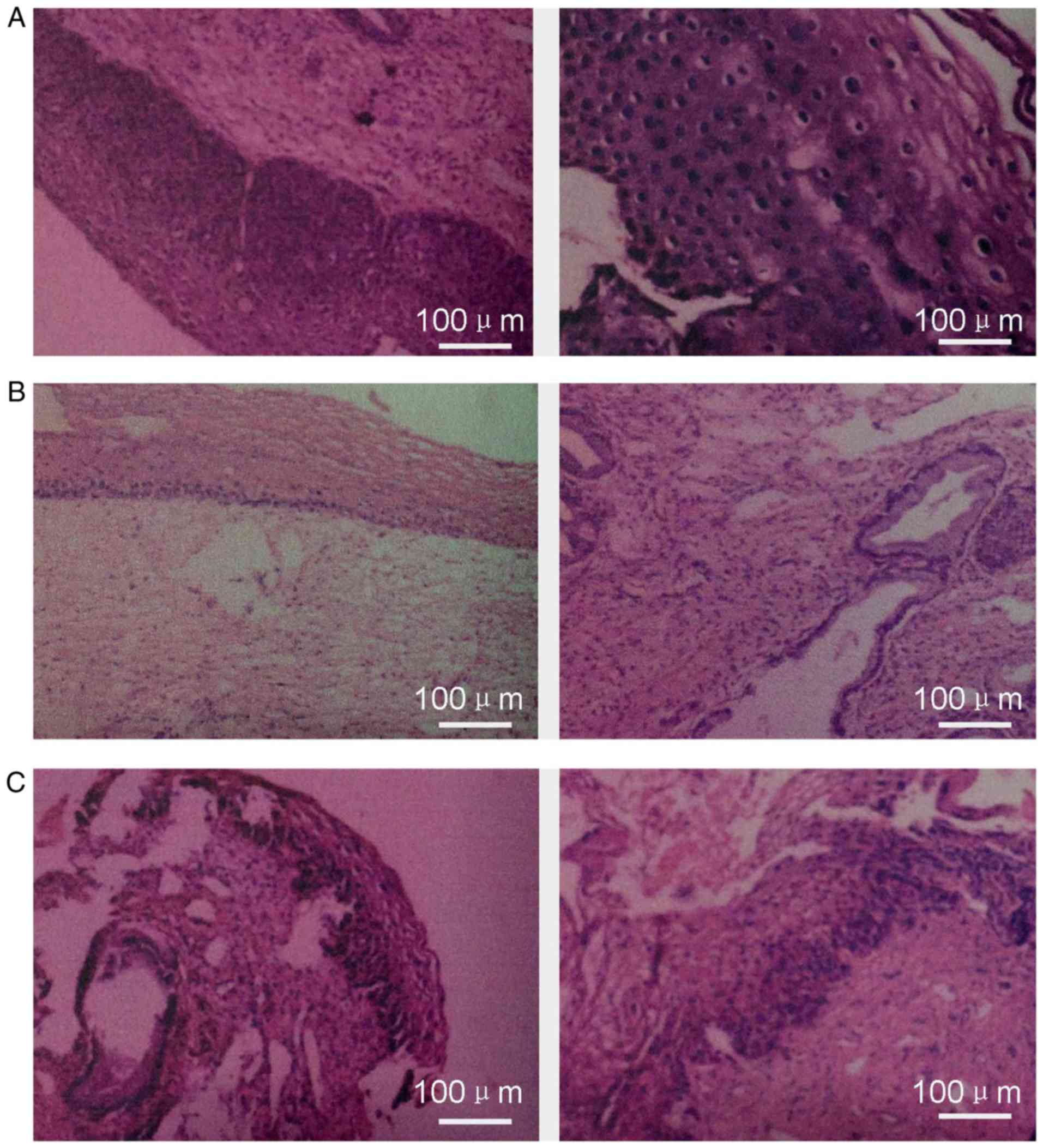
Histological results
The present study included 146 patients with
pre-cancerous lesions according to the patients' cytological
results. The histological samples were taken from the cervix of the
uterus using the colposcope prior to the analysis of the diagnostic
sensitivity and specificity according to a previously published
study (21). In the current study,
the gold standard for the cancer diagnosis was the histological
analysis. Histological analysis revealed that the patients either
exhibited focal advanced squamous intraepithelial lesions (CIN2,
CIN3; 66 patients; Fig. 1A),
low-grade squamous intraepithelial lesions (CIN1; 41 patients;
Fig. 1B) or low-grade
intraepithelial lesions (CIN0; 37 patients; Fig. 1C). There were also two patients with
adenocarcinoma of uterine cervix. Therefore, all of the patients
were included in the subsequent examinations.
Characteristics of the patients
A total of 93 patients (63.7%) were indicated to
have low cytological abnormalities and 53 patients (36.3%) had high
cytological abnormalities (Table I).
Furthermore, the lesions of 110 patients (75.3%) were
hrHPV-positive and those of 33 patients (22.6%) were
hrHPV-negative, while no results were obtained for 3 patients
(3.1%). Regarding the CIN grades, 37 patients were CIN0, 41 were
CIN1, 14 were CIN2 and 52 were CIN3 grade; furthermore, 2 patients
were diagnosed with adenocarcinoma of the cervix (Table I). Two biopsy specimens were
collected from each patient for the subsequent tests.
 | Table I.Clinicopathological characteristics of
the subjects (n=146). |
Table I.
Clinicopathological characteristics of
the subjects (n=146).
| Item | Value |
|---|
| Age (years) |
|
| Mean
(range) | 37.0 (18.7–62.6) |
|
Median | 35.4 |
| Cytological
detection |
|
|
ASCUS/ASC-H/LSIL | 93 (63.7) |
| HSIL | 53 (36.3) |
| hrHPV detection |
|
|
Positive | 110 (75.3) |
|
Negative | 33 (22.6) |
|
Ineffective detection | 3 (2.1) |
| Grade of
tumorigenicity |
|
| CIN0 | 37 (25.3) |
| CIN1 | 41 (28.1) |
| CIN2 | 14 (9.5) |
| CIN3 | 52 (35.6) |
| Adenocarcinoma of
uterine cervix | 2 (1.4) |
Combination of routine colposcopy and
DySI enhances the diagnostic sensitivity for pre-cancerous lesions
in subjects with abnormal cytological results
In patients classified as ASCUS/ASC-H/LSIL, the
diagnostic sensitivity in the DySI subgroup [69%; 95% confidence
interval (CI), 56–82%] was significantly higher compared with that
in the routine colposcopy subgroup (43%; 95% CI, 28–57%; P=0.01;
Table II). When the DySI method was
combined with routine colposcopy, the diagnostic sensitivity was
increased to 77% (95% CI, 65–88%), which was significantly higher
compared with that of routine colposcopy alone and DySI alone,
respectively (all P<0.05; Table
II). Furthermore, in the HSIL group, combined diagnosis by DySI
and routine colposcopy also demonstrated a higher diagnostic
sensitivity compared with that of in the routine colposcopy alone
or DySI alone group (P<0.05; Table
II). However, there were no significant differences in the
diagnostic sensitivity among the three subgroups for the HSIL and
hrHPV-negative group (P<0.05; Table
II).
 | Table II.Sensitivity and specificity of routine
colposcopy, DySI and their combination in the diagnosis of
intraepithelial cervical lesions of different histological types
(threshold, CIN2+) as pre-cancerous lesions. |
Table II.
Sensitivity and specificity of routine
colposcopy, DySI and their combination in the diagnosis of
intraepithelial cervical lesions of different histological types
(threshold, CIN2+) as pre-cancerous lesions.
| Group | N | Sensitivity (95% CI),
% | P-valuea | Specificity (95% CI),
% | P-valuea |
|---|
| ASCUS/ASC-H/LSIL | 93 |
|
|
|
|
| Routine
colposcopy |
| 43 (28–57) |
| 88 (81–95) |
|
| DySI |
| 69 (56–82) | 0.010 | 78 (68–88) | 0.210 |
| Combined
diagnosis |
| 77 (65–88) | 0.001 | 70 (59–80) | 0.001 |
| HSIL | 53 |
|
|
|
|
| Routine
colposcopy |
| 61 (48–74) |
| 55 (35–75) |
|
| DySI |
| 64 (51–76) | 1.000 | 63 (42–83) | 0.690 |
| Combined
diagnosis |
| 85 (75–95) | 0.001 | 25 (25–65) | 0.500 |
| HSIL and hrHPV
negative | 13 |
|
|
|
|
| Routine
colposcopy |
| 55 (22–87) |
| 46 (16–75) |
|
| DySI |
| 34 (4–65) | 0.690 | 65 (36–93) | 0.630 |
|
Combined diagnosis |
| 78 (52–100) | 0.500 | 36 (7–66) | 1.000 |
Cytological examination according to
Method 1
In Method 1 (a pre-screening strategy),
determination of the hrHPV status was used as the pre-screening
tool, and cytological examination was then employed to make a
definite diagnosis for patients with hrHPV-positive samples. In the
present study, 110 out of 146 patients (75.3%) were hrHPV-positive
and subjected to a cervical smear test. The results indicated that
71 patients (64.5%) had low cytological abnormalities and 39
patients (35.5%) had high cytological abnormalities (Table III).
 | Table III.Influence of different referral
strategies on the sensitivity and specificity of routine
colposcopy, DySI and their combination in the diagnosis of
intraepithelial cervical lesions (threshold, CIN2+) as
pre-cancerous lesions. |
Table III.
Influence of different referral
strategies on the sensitivity and specificity of routine
colposcopy, DySI and their combination in the diagnosis of
intraepithelial cervical lesions (threshold, CIN2+) as
pre-cancerous lesions.
| Method | N | Advanced lesions
under colposcopy, n (%) | Sensitivity (95%
CI), % |
P-valuea | Specificity (95%
CI), % |
P-valuea |
|---|
| 1 | 110 | 59 (53.3) |
|
|
|
|
| Routine
colposcopy |
|
| 52 (42–63) |
| 83 (74–91) |
|
|
DySI |
|
| 67 (57–77) | 0.040 | 68 (57–78) | 0.003 |
|
Combined diagnosis |
|
| 82 (73–90) | 0.001 | 63 (52–73) | 0.001 |
| 2 | 124 | 65 (52.4) |
|
|
|
|
| Routine
colposcopy |
|
| 53 (43–63) |
| 77 (68–85) |
|
|
DySI |
|
| 64 (54–73) | 0.100 | 67 (57–76) | 0.130 |
|
Combined diagnosis |
|
| 81 (74–89) | 0.001 | 60 (50–70) | 0.001 |
Cytological examination according to
Method 2
In Method 2 (a pre-screening strategy), the patients
with low cytological changes and hrHPV-negative status were
excluded from further analysis. Therefore, all of the patients with
high cytological changes and those with low cytological
abnormalities and hrHPV-positive status were subjected to
examination by colposcopy and/or DySI. The results indicated that
93 patients (76.4%) exhibited low cytological abnormalities and
were hrHPV-positive, and 53 patients exhibited high cytological
abnormalities (Table III).
Therefore, 124 patients (84.9% of all patients) were included in
Method 2; these patients included 71 hrHPV-positive patients and 53
patients who illustrated higher cytological abnormalities.
DySI enhances the diagnostic
sensitivity for subjects with ≥CIN2+ pre-screened with Method 1 or
2
If Method 1 was used for pre-screening, the
diagnostic sensitivity for detecting (pre-)cancerous lesions in
subjects with CIN2+ in the DySI group (67%; 95% CI, 57–77%) was
significantly higher compared with that in the routine colposcopy
group (52%; 95% CI, 42–63%; P=0.04; Table III). Furthermore, compared with
that in the groups using either diagnostic method alone, the
diagnostic sensitivity achieved by combination of routine
colposcopy with DySI was significantly increased to 82% (95% CI,
73–90%; P<0.05; Table III). If
Method 2 was used for pre-screening, no significant differences in
the diagnostic sensitivity were obtained between the DySI group
(64%; 95% CI, 54–73%) and the routine colposcopy group (53%; 95%
CI, 43–63%; P<0.05; Table III).
However, the diagnostic sensitivity in the combined diagnosis group
(81%; 95% CI, 74–89%) was significantly higher compared with that
in the groups using either diagnostic method alone (P=0.001;
Table III).
Discussion
Although cervical screening strategies have proven
to be successful in preventing cervical carcinoma, the diagnostic
accuracy also requires to be improved. Therefore, the diagnostic
accuracy of routine colposcopy combined with DySI was investigated
in the present study. It was revealed that DySI exhibited a higher
sensitivity, which is consistent with the result of a previously
published study (10). However, it
is uncommon that hrHPV-negative patients exhibit high cytological
changes; this may occur as the sequelae of un-associated risk
factors.
The finding of low cytological abnormalities
accounts for the overwhelming majority of abnormal cytological
morphologies in screening processes (22), and represents the patients who were
remained undiagnosed following the colposcopy. Due to a few
factors, such as difficulties in diagnosis and economic burden of
patients, international research to improve the screening process
and diagnostic methods for cervical carcinoma has been launched. In
fact, the implementation of the hrHPV examinations led to subjects
undergoing colposcopy screening in the clinic more frequently, a
certain amount of which may be unnecessary. Furthermore, potential
mistakes, including the relatively lower specificity of combined
diagnostic methods, or misdiagnosis (false-positive diagnoses or
identifying a low number of cytological abnormalities) may cause
unnecessary anxiety of patients, along with increased national
healthcare costs. However, it is important to perform preliminary
screenings prior to examination for cervical carcinoma using
combined diagnostic methods with enhanced sensitivity, while those
patients not fulfilling certain criteria may be excluded from
further examinations. In the present study, the data were analyzed
following DySI examination, and the results suggested that DySI
combined with routine colposcopy is able to significantly improve
the accuracy and sensitivity of cervical carcinoma diagnosis by
first subjecting the patients to hrHPV examination and/or
cytological examination (10,23).
In recent years, novel methods for diagnosing
pre-cancerous lesions have been proposed. Ni et al (24), used endoscopic diagnosis for
diagnosing pre-cancerous laryngeal lesions, which is also a
traditional method for examining laryngeal cancer lesions. DeNardis
et al (25), applied
adjunctive dynamic spectral imaging to detect pre-cancerous
cervical lesions. However, the secondary sensitivity and
specificity of the adjunctive dynamic spectral imaging on its own
are relatively low. Furthermore, in the present study, the strategy
of combining the DySI and routine colposcopy was applied for the
first time, to the best of our knowledge, which is also different
from the method described by DeNardis et al (25). In addition, three-dimensional power
Doppler ultrasound was previously utilized to diagnose
pre-cancerous lesions, but the sensitivity of this method is lower
(26) compared to the present study.
It is therefore indicated that the combination of DySI and routine
colposcopy is a promising strategy for diagnosing pre-cancerous
cervical lesions.
The present study had two possible limitations.
First, when the different screening methods and the referral method
were retrospectively simulated, certain deviations in the data
might occur. There is controversy regarding the correlation between
the characteristics of CIN2 and the clinical histological type,
however, CIN2 is also the threshold for excision treatment
(27,28). Furthermore, the number of biopsies
from the same patient were relatively small in the present study.
Increasing the amount of biopsies may increase the sensitivity of
the colposcopy examination (29).
However, in the present study, a mean number of specimens of 2
(ranging from 1 to 4) was selected, which is consistent with the
normal amount of biopsy specimens in the clinic. Therefore, it is
indicated that any potential effects of the amounts of selected
tissue biopsy specimens may be neglected.
In conclusion, the present study proved that the
DySI strategy has a higher diagnostic sensitivity compared with
that of routine colposcopy. Furthermore, adjuvant DySI improves the
accuracy of colposcopy examination in different setups. In
conclusion, combined DySI and routine colposcopy exhibited an
increased diagnostic sensitivity for the detection of pre-cancerous
lesions in patients with low or high cytological abnormalities,
compared with either method on its own.
Acknowledgements
Not applicable.
Funding
The present study was granted by the Science and
Technology Project of Jiangxi Education Department in 2017 (grant
no. GJJ170629).
Availability of data and materials
All data generated or analyzed during the present
study are included in this published article.
Authors' contributions
WLH designed the current study and provided the
fund. DL and WLH performed the experiments, collected the patients'
data, wrote the manuscript, and read and approved the final
manuscript.
Ethical approval and consent to
participate
The present study was approved by the Ethics
Committee of Jinggangshan University (Ji'an, China). All of the
patients provided their written informed consents to participate in
the present study.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
financial or commercial interests regarding the present study.
References
|
1
|
Torre LA, Bray F, Siegel RL, Ferlay J,
Lortet-Tieulent J and Jemal A: Global cancer statistics, 2012. CA
Cancer J Clin. 65:87–108. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Luo S, Li N, Yu S, Chen L, Liu C and Rong
J: MicroRNA-92a promotes cell viability and invasion in cervical
cancer via directly targeting Dickkopf-related protein 3. Exp Ther
Med. 14:1227–1234. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Li B, Shi H, Wang F, Hong D, Lv W, Xie X
and Cheng X: Expression of E-, P- and N-cadherin and its clinical
significance in cervical squamous cell carcinoma and precancerous
lesions. PLoS One. 11:e01559102016. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Wang JL, Yang YZ, Dong WW, Sun J, Tao HT,
Li RX and Hu Y: Application of human papillomavirus in screening
for cervical cancer and precancerous lesions. Asian Pac J Cancer
Prev. 14:2979–2982. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Ma L, Cong X, Shi M, Wang XH, Liu HY and
Bian ML: Distribution of human papillomavirus genotypes in cervical
lesions. Exp Ther Med. 13:535–541. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Wentzensen N, Zuna RE, Sherman ME, Gold
MA, Schiffman M, Dunn ST, Jeronimo J, Zhang R, Walker J and Wang
SS: Accuracy of cervical specimens obtained for biomarker studies
in women with CIN3. Gynecol Oncol. 115:493–496. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Ferris DG and Litaker MS; ALTS Group, :
Prediction of cervical histologic results using an abbreviated reid
colposcopic index during ALTS. Am J Obstet Gynecol. 194:704–710.
2006. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Wu Y, Zhao J, Hu J, Wu XW and Zhu LR:
Significance of p16/Ki-67 double immunocytochemical staining in
cervical cytology ASCUS, LSIL and ASC-H. Zhonghua Fu Chan Ke Za
Zhi. 52:734–739. 2017.(In Chinese; Abstract available in Chinese
from the publisher). PubMed/NCBI
|
|
9
|
Kaufmann A, Founta C, Papagiannakis E,
Naik P and Fisher A: Standardized digital colposcopy with dynamic
spectral imaging for conservative patient management. Case Rep
Obstet Gynecol. 2017:52692792017.PubMed/NCBI
|
|
10
|
Louwers J, Zaal A, Kocken M, Ter Harmsel
W, Graziosi G, Spruijt J, Berkhof J, Balas C, Papagiannakis E,
Snijders P, et al: Dynamic spectral imaging colposcopy: Higher
sensitivity for detection of premalignant cervical lesions. BJOG.
118:309–318. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Soutter WP, Diakomanolis E, Lyons D,
Ghaem-Maghami S, Ajala T, Haidopoulos D, Doumplis D, Kalpaktsoglou
C, Sakellaropoulos G, Soliman S, et al: Dynamic spectral imaging:
Improving colposcopy. Clin Cancer Res. 15:1814–1820. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Saslow D, Solomon D, Lawson HW, Killackey
M, Kulasingam SL, Cain J, Garcia FA, Moriarty AT, Waxman AG, Wilbur
DC, et al: American cancer society, American Society for colposcopy
and cervical pathology, and American society for clinical pathology
screening guidelines for the prevention and early detection of
cervical cancer. CA Cancer J Clin. 62:147–172. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Santesso N, Schunemann H, Blumenthal P, De
Vuyst H, Gage J, Garcia F, Jeronimo J, Lu R, Luciani S, Quek SC, et
al: World Health Organization Guidelines: Use of cryotherapy for
cervical intraepithelial neoplasia. Int J Gynaecol Obstet.
118:97–102. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Kelly RS, Patnick J, Kitchener HC and Moss
SM; NHSCSP HPV Special Interest Group, : HPV testing as a triage
for borderline or mild dyskaryosis on cervical cytology: Results
from the sentinel sites study. Br J Cancer. 105:983–988. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Li W, Venkataraman S, Gustafsson U, Oyama
JC, Ferris DG and Lieberman RW: Using acetowhite opacity index for
detecting cervical intraepithelial neoplasia. J Biomed Opt.
14:0140202009. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Snijders PJ, van den Brule AJ, Jacobs MV,
Pol RP and Mejier CJ: HPV DNA detection and typing in cervical
scrapes. Methods Mol Med. 119:101–114. 2005.PubMed/NCBI
|
|
17
|
van den Brule AJ, Pol R,
Fransen-Daalmeijer N, Schouls LM, Meijer CJ and Snijders PJ:
GP5+/6+ PCR followed by reverse line blot analysis enables rapid
and high-through identification of human papillomavirus genotypes.
J Clin Microbiol. 40:779–787. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Rijkaart DC, Berkhof J, van Kemenade FJ,
Coupe VM, Hesselink AT, Rozendaal L, Heideman DA, Verheijen RH,
Bulk S, Verweij WM, et al: Evaluation of 14 triage strategies for
HPV DNA positive women in population based cervical screening. Int
J Cancer. 130:602–610. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Pepe M: The statistical evaluation of
medical tests for classification and prediction. Oxford: Oxford
University Press; 2003
|
|
20
|
Greiner M: Serodiagnostische tests.
Berlin: Springer; 2003, View Article : Google Scholar
|
|
21
|
Hanaoka M, Ishikawa T, Ishiquro M, Tokura
M, Yamauchi S, Kikuchi A, Uetake H, Yasuno M and Kawano T:
Expression of ATF6 as a marker of pre-cancerous atypical change in
ulcerative colitis-associated colorectal cancer: A potential role
in the management of dysplasia. J Gastroenterol. 53:631–641. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Bulkmans NW, Rozendaal L, Snijders PJ,
Voorhorst FJ, Boeke AJ, Zandwijken GR, van Kemenade FJ, Verheijen
RH, v Groningen K, Boon ME, et al: POBASCAM, a population based
randomized controlled trial for implementation of high-risk HPV
testing in cervical screening: Design, methods and baseline data of
44, 2012 women. Int J Cancer. 110:94–101. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Zaal A, Louwers JA, Berkhof J, Kocken M,
Ter Harmsel WA, Graziosi GC, Spruijt JW, Balas C, Papagiannakis E,
Snijders PJ, et al: Agreement between colposcopic impression and
histological diagnosis among human papillomavirus type 16 positive
women: A clinical trial using dynamic spectral imaging colposcopy.
BJOG. 119:537–544. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Ni XG, He S, Xu ZG, Gao L, Lu N, Yuan Z,
Lai SQ, Zhang YM, Yi JL, Wang XL, et al: Endoscopic diagnosis of
laryngeal cancer and precancerous lesions by narrow band imaging. J
Laryngol Otol. 125:288–296. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
DeNardis SA, Lavin PT, Livingston J,
Salter WR, James- Patrick N, Papagiannakis E, Olson CG and Weinberg
L: Increased detection of precancerous cervical lesions with
adjunctive dynamic spectral imaging. Int J Womens Health.
9:717–725. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Belitsos P, Papoutsis D, Rodolakis A,
Mesogitis S and Antsaklis A: Three-dimensional power Doppler
ultrasound for the study of cervical cancer and precancerous
lesions. Ultrasound Obstet Gynecol. 40:576–581. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Moscicki AB, Ma Y, Wibbelsman C, Darragh
TM, Powers A, Farhat S and Shiboski S: Rate of and risks for
regression of CIN-2 in adolescents and young women. Obstet Gynecol.
116:1373–1380. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Dina R and Argamosa D: The NHS cervical
screening programme criteria for evaluating cervical cytology:
Comparison of the new with the old. Cytopathology. 23:349–352.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Bekkers RL, van de Nieuwenhof HP, Neesham
DE, Hendriks JH, Tan J and Quinn MA: Does experience in colposcopy
improve identification of high grade abnormalities. Eur J Obstet
Gynecol Reprod Biol. 141:75–78. 2008. View Article : Google Scholar : PubMed/NCBI
|