Introduction
Retroperitoneal sarcoma is a lethal disease with a
generally poor prognosis, and retroperitoneal tumors are usually
secondary metastatic tumors from other organs. Numerous patients
are able to feel an abdominal mass or distension at the end-stage
of the disease. Traditional treatment strategies for locally
advanced retroperitoneal tumors include surgical resection
(1,2), radiation therapy (3,4) and
chemotherapy (5,6). The deep site of the retroperitoneum is
surrounded by gastrointestinal and urologic organs and large blood
vessels, which increases the difficulty of open surgery.
Irreversible electroporation (IRE) is a non-thermal ablative
technique, which destroys the lipid-bilayer structure of the cell
membrane to generate tiny nanopores using a series of high-voltage,
low-energy-current electrical pulses, resulting in apoptosis of the
target cells. Previous studies have reported on the progressive use
of IRE for the treatment of solid organs, including the pancreas
(7), liver (8), lung (9),
kidney (10) and prostate (11), and it is particularly suitable for
tumors located in large vessels, the hilar region, bile duct and
ureter (12). We ever reported the
novel use of IRE for the percutaneous local ablation of portal vein
tumor thrombus (PVTT) without heat-sink effect and thermal injury
to surrounding portal vein (PV) branches (13). However, this technique is not
generally suitable for patients with cardiopulmonary dysfunction,
arrhythmia or cardiac pacemaker.
The present study reports on 3 cases with metastatic
retroperitoneal tumors with the primary tumor originating from
other organs, who received IRE palliative therapy using 3–4
electrodes according to the tumor size, and on their short-term
follow-up.
Materials and methods
Patient selection
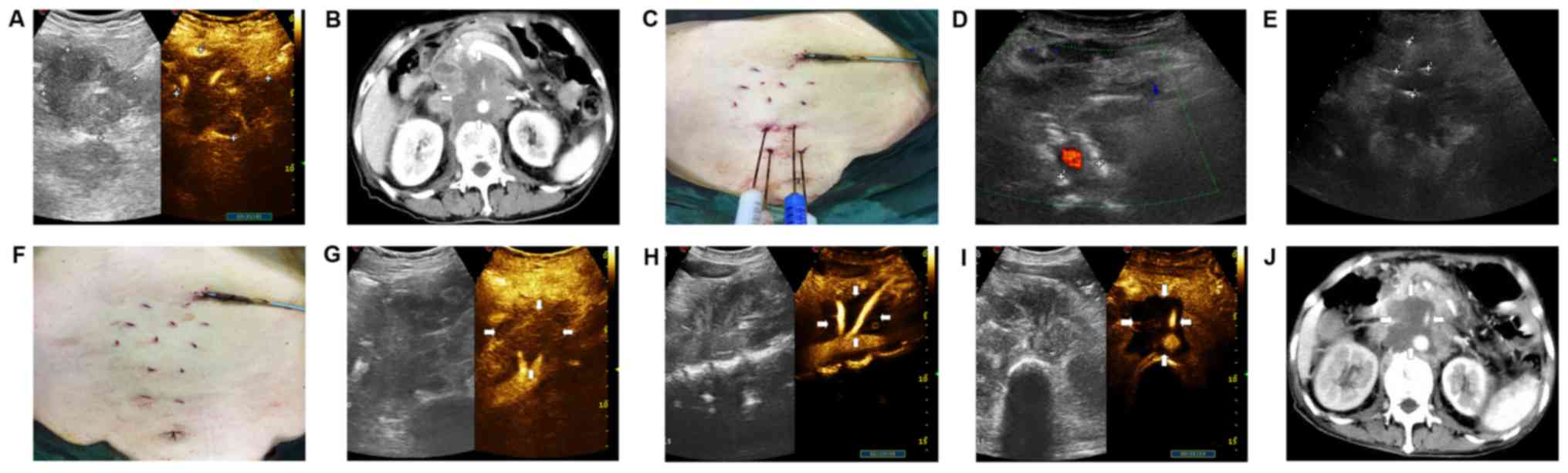
Between April 2016 and September 2017, a total of 3
patients (2 female and 1 male) who had 3 locally advanced
retroperitoneal tumors received percutaneous IRE therapy. The
baseline characteristics of the patients included are provided in
Table I. The patients (case 1,
female; case 2, female; case 3, male) were 60, 43 and 59 years old,
respectively, and all had metastatic retroperitoneal tumors (case
1, ovarian cancer; case 2, gastric cancer; and case 3, pancreatic
cancer), as well as a history of surgical resection or
chemotherapy. On admission, the patients had complaints of waist
pain for several months. The pain intensity was estimated using a
visual analog scale (VAS) from 0 to 10 (where 0 represented no pain
and 10 represented the worst pain imaginable) (14). Pre-operative computed tomography (CT)
or contrast-enhanced ultrasound (CEUS) revealed that the tumors
were between 2.0 and 6.1 cm in size. Pre-operative CEUS was
generated using ultrasound machines with contrast-specific software
(MyLab 70 XVG and MyLab Twice; Esaote) in case 1 revealed the
course of contrast agent wash-in and wash-out as time elapsed
(Fig. 1A), and pre-operative CT
indicated metastatic lymph nodes of 6.1×4.3 cm in size encircling
the abdominal aorta (Fig. 1B). Of
note, all these metastatic tumors were situated deeply and close to
important vessels, posing a risk of massive hemorrhage. The
inclusion criteria for the study were as follows: i) All patients
had their cancer pathologically confirmed; ii) patients were
intolerant to chemotherapy and were reluctant to undergo further
surgery due to the high risk associated with it; iii) measurements
of the following cancer-associated blood parameters were
applicable: Hemoglobin level, ≥8.0 g/dl (male normal range,
12.0–16.5 g/dl; female normal range, 11.0–15.0 g/dl); platelet
count, ≥50×109/l (normal range,
100–300×109/l) and international normalized ratio
>1.5 (normal range, 0.8–1.2); and iv) the patients were void of
severe coronary disease, acute or chronic infection or autoimmune
diseases. This prospective study was approved by the ethics
committee of the First Affiliated Hospital of Zhejiang University
(Zhejiang, China). All of the patients and their relatives were
informed about the procedures and provided their written informed
consent.
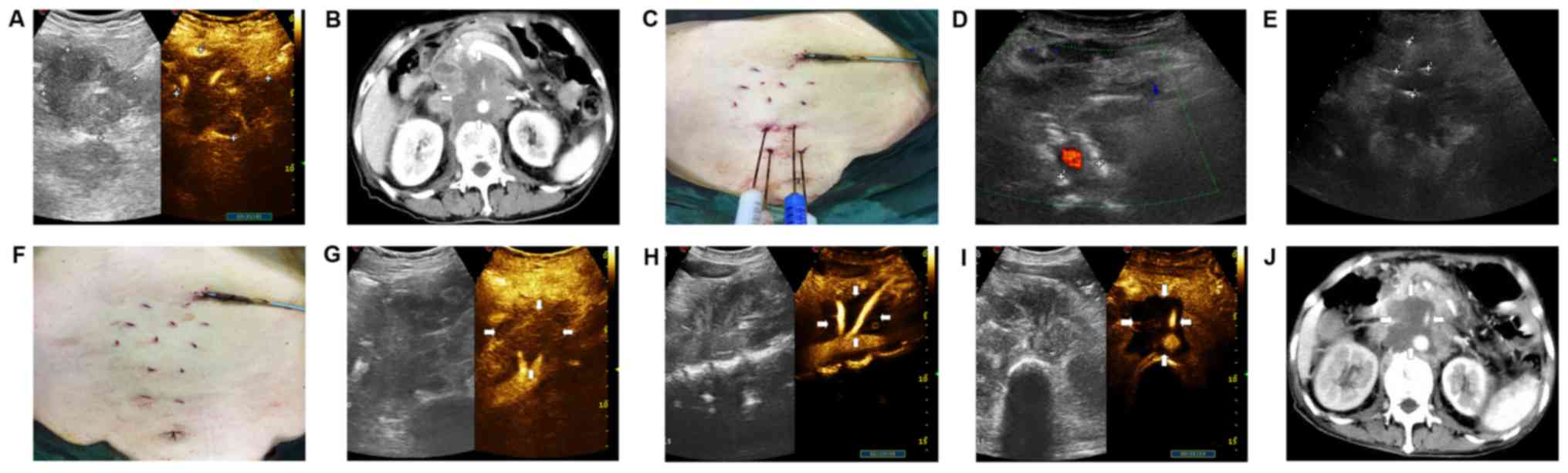 | Figure 1.A 60-year-old female patient with
metastatic retroperitoneal tumors was treated with IRE. (A)
Pre-operative CEUS, revealing irregular arterial hyper
vascularization of 6.36×6.30 cm. (B) Pre-operative CT scan
revealing a tumor of 6.1×4.3 cm in size encircling the abdominal
aorta. (C) The patient was placed in the supine position and
US-guided electrodes were inserted parallel. (D) Grayscale sagittal
US image of the retroperitoneum generated using color-flow Doppler
imaging, demonstrating that the two electrodes parallelly encircled
the tumor mass surrounding the abdominal aorta. (E) US-guided
percutaneous IRE ablation, revealing four needles parallelly
puncturing the targeted tissue. The distance between these needles
was 1.85–2.13 cm. (F) Image of the post-operative abdomen revealing
the needle tract. (G) Immediate post-operative image indicating the
tumors with slight enhancement on CEUS. (H) CEUS 20 days after IRE
revealing regular arterial hyper vascularization adjacent to the
hypoechoic area, corresponding to the immediate post-operative
image. (I) CEUS at 3 weeks following IRE treatment, indicating a
clearly demarcated dark area without perfused tissue. (J) 6 weeks
following IRE, the portal-phase axial CT image revealed tumor
complete necrosis of 5.4×5.2 cm in size (vs. an initial size of
6.1×4.3×4.3 cm3), without contrast enhancement around
the abdominal aorta. CE, contrast-enhanced; US, ultrasound; CT,
computed tomography; IRE, irreversible electroporation. |
 | Table I.Characteristics of patients with
metastatic retroperitoneal tumors. |
Table I.
Characteristics of patients with
metastatic retroperitoneal tumors.
| Case no. | Sex | Age (years) | Primary cancer | History | Location of
tumor |
|---|
| 1 | Female | 60 | Ovarian cancer | Oophorectomy and
chemotherapy | Adjacent to abdominal
aorta |
| 2 | Female | 43 | Gastric cancer | Gastrectomy | Adjacent to abdominal
aorta |
| 3 | Male | 59 | Pancreatic
cancer | Whipple
operation | Adjacent to abdominal
aorta |
IRE procedure
The three cases received percutaneous IRE in the
supine position under general anesthesia to avoid intense muscle
contractions via an electroporation system (NanoKnife®
system; AngioDynamics) using 3–4 19-gauge electrodes depending on
the tumor size. All of the percutaneous procedures were performed
by an interventional radiologist who had at least 10 years'
experience in interventional medicine. Under the guidance of
ultrasonography using MyLab Twice equipment (Esaote), percutaneous
IRE ablation in case 1 was performed using 4 parallel 19-gauge
electrodes, where the length of the tip was 0.5 cm and the
between-electrode distance was fixed at 1.6–2.1 cm (Fig. 1C). Doppler color-flow imaging was
used in real time to guide two needles, parallelly clamping the
target mass surrounding the abdominal aorta (Fig. 1D). All of the mentioned intervals
that are described were confirmed by US (Fig. 1E), and subsequently imported into the
electroporation software in order to select the appropriate voltage
and pulse-length delivery. Preliminary 2,700-V test pulses were
given to check the tissue conductivity. Subsequently, a total of 90
pulses with a length of 70–90 msec were performed in the voltage
range of 2,550–3,000 V under the setting of 1,500 V/cm. The
detailed procedures for treating the target lesions are summarized
in Table II. Cases 1 and 2 only
received one session of IRE therapy, whereas case 3 underwent a
second session of therapy at 5 months after the first IRE
treatment. Inter-electrode distances in the targeting lesions
ranged from 1.5 to 2.0 cm. An electrocardiograph trigger was used
to monitor different types of cardiac arrhythmia. After one session
of electroporation, immediate CEUS images (via the injection of 2.4
ml SonoVue mixed with 10.0 ml 0.9% sodium chloride solution) were
used to examine whether any potential residual lesions existed. In
the procedures for case 1, by parallelly adjusting the puncture
needle to a position ~1.0 cm away from the previous site of
electroporation, the parallel puncture and needle procedures were
repeated three times through a total of 12 rounds in order to
maximize the curative effect (Fig.
1F). Following percutaneous IRE, follow-up by CEUS, CT scan (GE
Healthcare) and measurement of cancer-associated blood parameters
[carcinoembryonic antigen, alpha fetoprotein and carbohydrate
antigen (CA19-9)] was performed at monthly intervals. In addition,
the European Organisation for Research and Treatment of Cancer
(EORTC) quality of life (QoL) questionnaire (QLQ)-C30 (Version 3.0)
is a questionnaire used for health-associated assessment, which
includes 5 functional dimensions (Physical, Role, Cognitive,
Emotional and Social functioning), 3 symptom dimensions (Fatigue,
Pain and Nausea/Vomiting), 1global health status scale and 6 single
items (Constipation, Diarrhea, Insomnia, Dyspnea, Appetite Loss and
Financial Difficulties) (15). The
clinical assessment of QoL in all patients was conducted at the
baseline and at every three months following IRE therapy.
 | Table II.Procedural specifications for each
patient. |
Table II.
Procedural specifications for each
patient.
| Patient | Ablation area
(cm) |
| Number of
needles | Type of needle
(gauge) | Voltage (V) | Number of pulses | Mutual distance of
needles (cm) | Time of survival the
(months) | Complications | Outcome | CEA (ng/ml) (normal
range, 0–5 ng/ml) | AFP (ng/ml) (normal
range, 0–20 ng/ml) | CA19-9 (U/ml) (normal
range, 0–37 ng/ml) |
|---|
|
| Initial | Last follow-up |
|
|
|
|
|
|
|
| Pre-IRE | Post-IRE | Pre-IRE | Post-IRE | Pre-IRE | Post-IRE |
| 1 | CT:6.1×4.3;
CEUS:6.3×4.9 | CT:5.4×5.2 | 4 | 19 | 2,550–3,000 | 80–90 | 1.6; 1.8; 2.0;
2.0 | 5 | Mild pain, minor
bleeding | Alive | 1.0 | 0.9 | 1.4 | 1.3 | 7.1 | 10.8 |
| 2 | CT:2.8×2.0 | CT:2.0×1.5 | 3 | 19 | 2,400–3,000 | 80 | 1.6; 2.0; 1.5 | 2 | Mild pain | Deceased | 64.8 | 2,639.1 | 2.6 | 2.7 | 9.8 | 69.0 |
| 3 | CT:2.8×2.3 | MR:1.8×1.4; | 3 | 19 | 2,800–3,000 | 70–80 | 2.0; 2.0; 2.0 | 11 | Mild pain, minor
bleeding | Deceased | 4.3 | 4.8 | 2.4 | 2.2 | >12,000 | 1,374.1 |
Results
IRE procedure characteristics and
follow up
The three patients enrolled in the present study
underwent palliative IRE therapy for locally advanced
retroperitoneal tumors, with a mean follow-up time of 6 months
post-IRE. For case 1, CEUS imaging immediately after the surgery
revealed regular arterial hyper vascularization adjacent to the
hypoechoic area corresponding to the CEUS images at 3 weeks
post-IRE (Fig. 1G and H).
Furthermore, the 3-week CEUS image exhibited a clear contrast
defect with a sufficient ablation margin (Fig. 1I), which was in accordance with the
contrast-enhanced CT at 1.5 months after IRE, and revealed that the
tumor shrank to 5.4×5.2 cm in size (vs. 6.1×4.3×4.3 cm3
in initial size), without contrast enhancement (Fig. 1J).
At several months following IRE therapy, the cases
exhibited improved clinical symptoms (Table III), and their overall survival
(OS) ranged from 2 to 11 months. Case 1 was alive at the time of
writing. Case 2 and 3 had an OS of 2 and 11 months following IRE,
respectively. Regarding the tumor markers following IRE, these were
all within the normal range for case 1, although case 2 exhibited
an increased carcinoembryonic antigen level, from 64.8 to 2,639.1
ng/ml, and case 3 had CA19-9 levels beyond the upper limit of
normal (Table II). During the
follow-up, minor procedure-associated pain was immediately
detectable for the 3 cases and minor bleeding was instantly
reported in case 1 and 3, which did not receive any treatment.
Compared with the VAS score recorded on admission to the hospital,
the patients exhibited effective pain relief (mean score of 5.8
decreased to 2.2) at the last month of follow-up. Furthermore, when
comparing QoL at the baseline, QoL assessment revealed that global
health status improved and pain score decreased during the last
follow-up (Table III). However,
case 2 died within 2 months and case 3 within 11 months due to
liver metastases of the primary tumor.
 | Table III.Change in quality of life (before
IRE-3 months after IRE). |
Table III.
Change in quality of life (before
IRE-3 months after IRE).
|
| Difference in
quality of life |
|---|
|
|
|
|---|
| EORTC Scale | Before IRE-3 months
after IRE | Before IRE-last
month of follow-up |
|---|
| Global health
status | −12.6a | −15.2a |
| Functional
scales |
|
Physical functioning | −2.8 | −3.2 |
| Role
functioning | −1.3 | 2.6 |
|
Emotional functioning | −1.2 | −7.8 |
|
Cognitive functioning | 3.1 | 5.2 |
| Social
functioning | −7.9 | −6.2 |
| Symptom scales |
|
Fatigue | 1.3 | 5.2 |
|
Nausea/vomiting | 2.3 | 3.8 |
|
Pain |
16.2b | 15.6a |
|
Dyspnea | −0.8 | −2.9 |
|
Insomnia | −4.9 | −3.9 |
|
Appetite loss | 2.5 | 4.3 |
|
Constipation | 7.3 | 6.1 |
|
Diarrhea | 4.9 | 6.8 |
|
Financial problems | −3.6 | −3.1 |
Systematic review
In addition, to substantiate the results of the
present study, a systematic literature search was performed in the
PubMed, Embase, Web of Science, Scoups and Cochrane Library
databases for studied published until September 21st, 2017, using
the following predefined search terms: ‘Irreversible
electroporation’, ‘retroperitoneal’ and ‘cancer’. Of 38 relevant
studies selected based on the title and abstracts screened, the
full-text version of 4 studies was finally reviewed. These studies
comprised 1 study based on a porcine model (16) and 3 studies on human patients
(17–19). Table
IV provides the basic characteristics of the included studies.
A total of 12 patients with 12 tumors underwent IRE treatment using
2–3 electrodes (15–17). The mean age of the patients ranged
from 45.9 to 74 years. During the 1–2-month follow-up period, minor
complications, including anastomotic leak, wound infection and
adverse effects including pain were observed.
 | Table IV.Summary of IRE therapy of end-stage
retroperitoneal tumors reported in the literature. |
Table IV.
Summary of IRE therapy of end-stage
retroperitoneal tumors reported in the literature.
| Author, year | Study period | Design | Country | Subjects | Population
characteristics | Tumor size
(cm) | Treatment
methods | Number of
electrodes | Number of
patients | Males/females | Age (years) | Follow-up interval
(months) | Complications | (Refs.) |
|---|
| Dunki et al
2014 | NA | Retrospective | United States | Porcine | 6 retroperitoneal
tissues | NA | US-guided | 4 | 6 | NA | NA | NA | NA | (16) |
| Underhill et
al 2016 | December 2013 to
April 2015 | Retrospective | United States | Human | 2 sarcoma; 1
carcinoid; 1 giant cell tumor; 1 ovarian; 1 triton tumor; 1
adenocarcinoma | NA | NA | 3 | 7 | 1/6 | 45.9±13.6 | 1 | 1 anastomotic leak;
1 wound infection | (17) |
| Kambakamba et
al, 2016 | September 2012 to
December 2015 | Prospective | Switzerland | Human | 4 retroperitoneal
tumors | NA | US-guided IRE | NA | 4 | NA | NA | NA | NA | (18) |
| Qin et al,
2017 | March 2016 | Retrospective | China | Human | 1 unresectable
retroperitoneal malignant fibroussarcoma | 7.3×7.0×7.5 | CT and US-guided
IRE | 2 | 1 | 0/1 | 74 | 2 | NA | (19) |
Discussion
At present, insufficient evidence is available to
determine the optimal management of patients with retroperitoneal
cancer, and this pathology continues to present a therapeutic
challenge due to medical issues and anatomical challenges. Meng
et al (20) reported a mean
OS of 5.03 months using gemcitabine for the treatment of locally
advanced and metastatic pancreatic adenocarcinoma. Huachansu, an
injectable form of chansu, is a sterilized hot water extract of
dried toad skin and when combined with gemcitabine, may not improve
the prognosis of patients with locally advanced metastatic
pancreatic cancer (20).
IRE was previously performed for PVTT (13). It was determined that end-stage
metastatic retroperitoneal malignant tumors were located at risky
sites (12,13), including vital structures and large
blood vessels. In the present case series, the three patients were
palliatively treated using IRE, with favorable results, including a
mean OS of >6 months. During the follow-up, minor side effects
that did not receive any treatment, including pain and bleeding
from needle wounds, were recorded. The patients exhibited an
improved prognosis compared with that at baseline, and the
post-operative QoL of all three cases was improved in the
functional and symptom dimensions, as well as on the global health
status scale of the EORTC QLQ-C30. However, two cases succumbed to
mortality due to liver metastases from the primary tumor. Over the
course of the last few decades, numerous studies have suggested
that IRE is effective in prolonging the survival of patients with
malignant tumors. In a multicenter prospective trial including 200
patients with locally advanced pancreatic cancer treated with IRE,
the median OS was 24.9 months and only 6 patients (3%) presented
with local recurrence during a median follow-up of 29 months
(21). Narayanan et al
(22) reported a similar median OS
of 27.0 months. This study reported on a case with unresectable
retroperitoneal malignant fibrous sarcoma treated with CT-guided
IRE using 2 electrodes. The CT scan indicated that a lesion
decreased in size from 7.3×7.0×7.5 to 5.1×4.0×5.2 cm, without any
obvious enhancement at 2 months post-operatively (19). In a retrospective study, Underhill
et al (17) identified that
patients undergoing supplemental IRE following surgical resection
for retroperitoneal neoplasms had developed few complications.
Therefore, IRE has emerged as an important supplementary method to
accompany surgical resection for the treatment of retroperitoneal
tumors.
The clinical challenge is enhanced if the
retroperitoneal tumors have a large size and then usually invade
proximal organs. A previous study reported that IRE may induce
cellular apoptosis rather than protein denaturation and necrosis,
and the tumor cells may be removed via cellular phagocytosis;
subsequently, the ablation area was rapidly replaced by normal
cells, which was beneficial in terms of functional recovery
(23). During these procedures,
structures including blood vessels, nervous tissue or bile ducts
remain intact. In terms of safety, selection of appropriate probe
placement, needle exposure length and pulse length is vital. A
preliminary study using a porcine model indicated that probe
exposure of ~2.5 cm in the liver and ~1.5 cm in the pancreas with
an inter-electrode distance of 1.5–2.3 cm were acceptable (16). The accuracy of the IRE procedure is
high due to real-time navigation and monitoring associated with US.
Furthermore, in the present study, ablated residual lesions were
easily located and rapidly identified by using CEUS. The treatment
efficacy of the procedure was not affected by heat-sink effects,
since IRE, as a method, is predominantly based on electrical pulse
breakdown of the cell membrane (24). During the process, irreversible
electroporation does not produce heat, and therefore, it is not
affected by additional external temperature. Compared with thermal
ablation, there are clear boundaries, which do not cause damage to
adjacent normal tissue. In addition, IRE was reported to cause
robust immunogenic effects, which led to increased serum
interleukin-6 levels higher than those achieved through
radiofrequency ablation (25).
Therefore, the results of the present study highlighted that IRE
may be beneficial for cases of locally advanced metastatic tumors
located in proximity to major vessels.
There were certain limitations associated with the
present study. First, the study had a small sample size and two of
the patients were followed up until death. Furthermore, needle
tract seeding is possible, but not controlled, during IRE ablation.
In a previously published study, this was demonstrated to occur in
26% of the treated tumors under CT guidance in 29 patients with
lesions located adjacent to major portal or hepatic veins, bile
duct structures or the intestines (26). Furthermore, in the present study,
confounding factors should be considered, and individual
heterogeneous factors, including individual histories of
therapeutic treatments and lifestyle changes, may have exaggerated
the palliative treatment effects determined. Furthermore, long-term
adjuvant effects may lead to selection bias (27–29).
However, taking all of these limitations into consideration, the
results of the present study still suggest that patients undergoing
IRE therapy were at a lower risk of complications of massive
hemorrhage in at risk regions, compared with those receiving other
treatment options, which may provide a novel line of investigation
in the future.
In conclusion, the present study preliminarily
identified technically effective, percutaneous IRE procedures
utilizing US guidance for unresectable metastatic retroperitoneal
tumors. During short-term follow-up, this may assist in providing
favorable palliative care in terms of improving prognosis. However,
additional large-scale pairwise comparisons with control groups and
long-term studies are required to substantiate these results
regarding IRE therapy.
Acknowledgements
Not applicable.
Funding
The design of the present study, data collection and
analysis were supported by the Natural Science Foundation of
Zhejiang Province (grant no. LY16H180004), the National S&T
Major Project of China (grant nos. SQ2018ZX100301 and
2018ZX10301201), the Key Research Development Program of Zhejiang
province (grant no. 2018C03018), the Key Science and Technology
Program of Zhejiang province (grant no. WKJ-ZJ-1923), the Science
and Technology Project of Zhejiang Province (grant no. 2012C23094)
and the Foundation of Zhejiang Health Committee (grant nos.
2014KYA086 and 2016DTB003).
Availability of data and materials
All data generated during the present study are
included in this published article.
Authors' contributions
Study conception and design: TJ; acquisition of
data: TJ, QZ, XB, GT, XC, LW; analysis and interpretation of data:
QZ, GT; drafting of the manuscript: TJ, QZ; critical revision of
the manuscript for important intellectual content: TJ; statistical
analysis: GT; obtainment of funding: TJ, QZ, XB, XC, LW; technical
or material support: TJ; study supervision: TJ. All authors read
and approved the final manuscript.
Ethics approval and consent to
participate
This prospective study was approved by the ethics
committee of the First Affiliated Hospital of Zhejiang University
(Zhejiang, China). Informed consent for study participation were
obtained.
Consent for publication
Consent for publication of the data and images (CEUS
images, CT or MRI images, laboratory findings, age, sex) was
obtained from all participating patients.
Competing interests
The authors declare that they have no competing
interests.
Glossary
Abbreviations
Abbreviations:
|
IRE
|
irreversible electroporation
|
|
US
|
ultrasonography
|
|
CEUS
|
contrast-enhanced ultrasound
|
|
OS
|
overall survival
|
|
CT
|
computed tomography
|
References
|
1
|
Macneill AJ, Miceli R, Strauss DC,
Bonvalot S, Hohenberger P, Van Coevorden F, Rutkowski P, Callegaro
D, Hayes AJ, Honoré C, et al: Post-relapse outcomes after primary
extended resection of retroperitoneal sarcoma: A report from the
Trans-Atlantic RPS Working Group. Cancer. 123:1971–1978. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Maurice MJ, Yih JM, Ammori JB and
Abouassaly R: Predictors of surgical quality for retroperitoneal
sarcoma: Volume matters. J Surg Oncol. 116:766–774. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Mak KS, Phillips JG, Barysauskas CM, Lee
LK, Mannarino EG, Van Benthuysen L, Raut CP, Mullen JT, Fairweather
M, DeLaney TF and Baldini EH: Acute gastrointestinal toxicity and
bowel bag dose-volume parameters for preoperative radiation therapy
for retroperitoneal sarcoma. Pract Radiat Oncol. 6:360–366. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Lee HS, Yu JI, Lim DH and Kim SJ:
Retroperitoneal liposarcoma: The role of adjuvant radiation therapy
and the prognostic factors. Radiat Oncol J. 34:216–222. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Alqasem K, Abukhiran I, Jasser J, Bisharat
T, Ellati RT, Khzouz J, Al-Saidi I and Al-Daghamin A:
Clinico-pathological outcomes of post-primary and salvage
chemotherapy retroperitoneal lymph node dissection for mixed germ
cell tumors, King Hussein Cancer Center experience. Turk J Urol.
42:256–260. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Mano R, Becerra MF, Carver BS, Bosl GJ,
Motzer RJ, Bajorin DF, Feldman DR and Sheinfeld J: Clinical outcome
of patients with Fibrosis/Necrosis at post-chemotherapy
retroperitoneal lymph node dissection for advanced germ cell
tumors. J Urol. 197:391–397. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Stillström D, Nilsson H, Jesse M,
Peterhans M, Jonas E and Freedman J: A new technique for minimally
invasive irreversible electroporation of tumors in the head and
body of the pancreas. Surgical Endosc. 31:1982–1985. 2017.
View Article : Google Scholar
|
|
8
|
Langan RC, Goldman DA, D'Angelica MI,
Dematteo RP, Allen PJ, Balachandran VP, Jarnagin WR and Kingham TP:
Recurrence patterns following irreversible electroporation for
hepatic malignancies. J Surg Oncol. 115:704–710. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Song ZQ, Xu XH, Pan ZH, Yao CG and Zhou
QH: Mechanisms for steep pulse irreversible electroporation
technology to kill human large cell lung cancer cells L9981. Int J
Clin Exp Med. 7:2386–2394. 2014.PubMed/NCBI
|
|
10
|
Martin RC, Schwartz E, Adams JA, Farah I
and Derhake BM: Intra-operative anesthesia management in patients
undergoing surgical irreversible electroporation of the pancreas,
Liver, Kidney, and retroperitoneal tumors. Anesth Pain Med.
5:e227862015. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Scheltema MJ, Postema AW, de Bruin DM,
Buijs M, Engelbrecht MR, Laguna MP, Wijkstra H, de Reijke TM and de
la Rosette JJMCH: Irreversible electroporation for the treatment of
localized prostate cancer: A summary of imaging findings and
treatment feedback. Diagn Interv Radiol. 23:365–370. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Kos B, Voigt P, Miklavcic D and Moche M:
Careful treatment planning enables safe ablation of liver tumors
adjacent to major blood vessels by percutaneous irreversible
electroporation (IRE). Radiol Oncol. 49:234–241. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Chai W, Tian G and Jiang T: Percutaneous
irreversible electroporation for portal vein tumor thrombus: A case
report. Ultrasound Q. 33:296–299. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Bijur PE, Silver W and Gallagher EJ:
Reliability of the visual analog scale for measurement of acute
pain. Acad Emerg Med. 8:1153–1157. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Giesinger JM, Kuijpers W, Young T,
Tomaszewski KA, Friend E, Zabernigg A, Holzner B and Aaronson NK:
Thresholds for clinical importance for four key domains of the
EORTC QLQ-C30: Physical functioning, emotional functioning, fatigue
and pain. Health Qual Life Outcomes. 14:872016. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Dunki-Jacobs EM, Philips P and Martin RC
II: Evaluation of thermal injury to liver, pancreas and kidney
during irreversible electroporation in an in vivo experimental
model. Br J Surg. 101:1113–1121. 2014. View
Article : Google Scholar : PubMed/NCBI
|
|
17
|
Underhill CE, Walsh NJ, Bateson BP,
Mentzer C and Kruse EJ: Feasibility and safety of irreversible
electroporation in locally advanced pelvic and retroperitoneal
tumors. Am Surg. 82:e263–e265. 2016.PubMed/NCBI
|
|
18
|
Kambakamba P, Bonvini JM, Glenck M,
Castrezana López L, Pfammatter T, Clavien PA and DeOliveira ML:
Intraoperative adverse events during irreversible electroporation-a
call for caution. Am J Surg. 212:715–721. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Qin Z, Zeng J, Liu G, Long X, Fang G, Li
Z, Xu K and Niu L: Irreversible electroporation ablation of an
unresectable fibrous sarcoma with 2 electrodes: A case report.
Technol Cancer Res Treat. Jan 1–2017.doi: 10.1177/1533034617711530
(Epub ahead of print). View Article : Google Scholar
|
|
20
|
Meng Z, Garrett CR, Shen Y, Liu L, Yang P,
Huo Y, Zhao Q, Spelman AR, Ng CS, Chang DZ and Cohen L: Prospective
randomised evaluation of traditional Chinese medicine combined with
chemotherapy: A randomised phase II study of wild toad extract plus
gemcitabine in patients with advanced pancreatic adenocarcinomas.
Br J Cancer. 107:411–416. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Martin RC II, Kwon D, Chalikonda S,
Sellers M, Kotz E, Scoggins CM, McMasters KM and Watkins K:
Treatment of 200 locally advanced (stage III) pancreatic
adenocarcinoma patients with irreversible electroporation: Safety
and efficacy. Ann Surg. 262:486–494. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Narayanan G, Hosein PJ, Beulaygue IC,
Froud T, Scheffer HJ, Venkat SR, Echenique AM, Hevert EC,
Livingstone AS, Rocha-Lima CM, et al: Percutaneous image-guided
irreversible electroporation for the treatment of unresectable,
locally advanced pancreatic adenocarcinoma. J Vasc Interv Radiol.
28:342–348. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Ansari D, Kristoffersson S, Andersson R
and Bergenfeldt M: The role of irreversible electroporation (IRE)
for locally advanced pancreatic cancer: A systematic review of
safety and efficacy. Scand J Gastroenterol. 52:1165–1171. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Lee EW, Thai S and Kee ST: Irreversible
electroporation: A novel image-guided cancer therapy. Gut Liver. 4
(Suppl 1):S99–S104. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Bulvik BE, Rozenblum N, Gourevich S, Ahmed
M, Andriyanov AV, Galun E and Goldberg SN: Irreversible
electroporation versus radiofrequency ablation: A comparison of
local and systemic effects in a Small-animal model. Radiology.
280:413–424. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Distelmaier M, Barabasch A, Heil P,
Kraemer NA, Isfort P, Keil S, Kuhl CK and Bruners P: Midterm safety
and efficacy of irreversible electroporation of malignant liver
tumors located close to major portal or hepatic veins. Radiology.
285:1023–1031. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Schwarze JE, Jeria R, Crosby J, Villa S,
Ortega C and Pommer R: Is there a reason to perform ICSI in the
absence of male factor? Lessons from the latin american registry of
ART. Hum Reprod Open. 2017:hox0132017. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Joong Choi C, Roh YH, Kim MC, Choi HJ, Kim
YH and Jung GJ: Single-port laparoscopic cholecystectomy for gall
bladder polyps. JSLS. 19(pii): e2014.00183. 2015.PubMed/NCBI
|
|
29
|
Pirracchio R, Sprung CL, Payen D and
Chevret S: Utility of time-dependent
inverse-probability-of-treatment weights to analyze observational
cohorts in the intensive care unit. J Clin Epidemiol. 64:1373–1382.
2011. View Article : Google Scholar : PubMed/NCBI
|