Introduction
In the USA, chronic obstructive pulmonary disease
(COPD) affects 7% individuals in the age group of 25–75 years and
is the 4th leading cause of mortality in North America and Europe
(1,2). This chronic progressive disease results
in the gradual loss of lung function, eventually leading to
hypoxemia and dyspnea, with patients complaining of chronic cough,
sputum production and shortness of breath (3). Dyspnea from air-flow limitation usually
restricts patients with COPD from performing strenuous physical
activities with the resultant loss of strength and the endurance of
skeletal muscles (4). Exercise
intolerance is a characteristic of COPD and is observed in the
early stages of the disease. The management of all patients with
COPD, functionally disabled by breathlessness, includes pulmonary
rehabilitation (PR) (5,6). An integral component of PR is physical
training, which can lead to significant improvements in exercise
capacity, breathlessness, fatigue and health-related quality of
life outcomes of patients with COPD (7). PR benefits individuals by decreasing
minute ventilation for any given external work possibly by
improving the metabolic capacity of skeletal muscles (8).
Oxygen supplementation has been an ergogenic aid for
patients with COPD. Long-term oxygen therapy has been shown to be
beneficial for patients with chronic resting hypoxemia (9). Ambulatory oxygen has also been used for
the treatment of patients who experience hypoxemia during routine
daily activities, but are normoxemic at rest (10). Several clinical trials have
investigated the role of supplemental oxygen during exercise
training in PR programs (11–13).
Patients with exercise-induced desaturation may not tolerate
high-intensity exercise and may require reduced intensity training
during PR, thereby limiting its effectiveness (5). It is postulated that oxygen may enhance
the exercise training of patients with COPD (11). The mechanism of supplemental oxygen
in increasing exercise performance has been attributed to decreased
ventilatory response, possibly due to a blunted carotid body drive
or delayed lactic acidosis (14).
The results of randomized controlled trials (RCTs) however, have
been conflicting (13,15). A Cochrane meta-analysis in 2007
reviewing 5 RCTs, reported limited evidence for oxygen
supplementation during exercise training for individuals with COPD
(2). There is thus a need for an
updated systematic review and meta-analysis investigating the role
of oxygen therapy during exercise training for patients with
COPD.
Data and methods
Selection criteria
The primary objective of this systematic review was
to investigate the role of supplemental oxygen in improving
outcomes following exercise training in patients with COPD. This
study was conducted in line with the Preferred Reporting Items for
Systematic Reviews and Meta-analyses (PRISMA) statement (16) and guidelines of the Cochrane Handbook
for Systematic Reviews of Intervention (17). Only RCTs evaluating the efficacy of
supplementary oxygen therapy during the exercise training of
patients with COPD were included. Abstracts, non-English language
studies, uncontrolled studies and retrospective studies were
excluded. The detailed inclusion and exclusion criteria applied for
participants, interventions and outcomes are presented in Table I.
 | Table I.Eligibility criteria for inclusion in
the systematic review. |
Table I.
Eligibility criteria for inclusion in
the systematic review.
|
| Participants | Intervention | Outcomes |
|---|
| Included | Adult patients with
COPD with one of the following: | i) For the study
group: Oxygen therapy provided | Any one of the
following: |
|
| i) Best recorded
EV1/FVC ratio <0.7; ii) best recorded | via wall
units/portable oxygen cylinders/Liquid | i) Maximum exercise
capacity or incremental exercise |
|
| FEV1 <80% | cannisters. For the
control group: Compressed air | capacity or timed
walk tests. |
|
|
| or room air. | ii) Dyspnoea
scores |
|
|
| ii) Intervention
provided during exercise training | iii) Quality of
life outcomes |
| Excluded | Patients with COPD
on long-term oxygen therapy | i) Intervention not
used during exercise therapy. | Not studying any of
the above-mentioned outcomes |
|
|
| ii) Long-term
oxygen therapy like for daily home |
|
|
|
| activities |
Search strategy
PubMed, Scopus, Cochrane Central Register of
Controlled Trials (CENTRAL) and Google scholar databases (first 100
results) were electronically searched for articles published up to
May, 2019. Key words used in various combinations were as follows:
Oxygen therapy [MeSH], oxygen [MeSH], supplemental oxygen [Free
text], chronic obstructive pulmonary disease [MeSH], chronic
obstructive lung disease [MeSH], chronic obstructive airway disease
[MeSH], pulmonary rehabilitation [Free text], exercise [MeSH],
dyspnea [MeSH], quality of life [MeSH] and physical endurance
[MeSH]. References of included studies and review articles were
analyzed for the identification of any additional studies.
Collection of data and analysis
Two independent reviewers examined potentially
eligible studies for inclusion in the review. Following the removal
of duplicates, studies were scrutinized by their title and
abstracts. Full-texts of selected articles were then scanned for
inclusion. Any difference in opinion was resolved by discussion.
The following data from the included trials were extracted:
Authors, publication year, study type, sample size, demographic
data, interventions used, exercise protocol, outcomes assessed and
study conclusions.
Quality assessment
The Cochrane Collaboration risk assessment tool for
RCTs was used for assessing the risk of bias (18). Seven criteria were evaluated for each
study: Random sequence generation, allocation concealment, blinding
of participants and personnel, blinding of outcome assessment,
incomplete outcome data, selective outcome reporting and other
biases. The included studies were judged for each item and rated as
‘high risk’, ‘low risk’ or ‘unclear risk’.
Statistical analysis
Several variable exercise tests have been used for
patients with COPD, such as maximal/incremental/progressive
exercise tests, constant power/sub-maximal/endurance exercise
tests, functional exercise tests and shuttle walk tests. Only
results from the same exercise protocol were combined.
Meta-analysis was conducted only if at least 3 studies reported
data on the same scale. In studies where exercise outcomes were
measured on oxygen and room air, only room air values were
considered. Outcome data extracted were entered into Review Manager
[RevMan, version 5.3; Nordic Cochrane Centre (Cochrane
Collaboration), Copenhagen, Denmark, 2014] for quantitative
analysis. Changes in outcome scores were used for the
meta-analysis. In studies where change scores were missing, the
following equation was used for calculating the change in mean and
standard deviation (SD) scores: i) Mean (change) = mean
(after)-mean (before); ii) SD (change) = square root
{[SD2 (after)-SD2 (before)]/2}.
Considering the heterogeneity amongst studies, a
random-effects model was used to calculate the pooled effect size.
The mean difference (SMD) with 95% confidence interval (CI) was
used for combining the data. Heterogeneity was calculated using the
I2 statistic. I2 values of 25–50% represented
low, values of 50–75% medium and >75% represented substantial
heterogeneity.
Results
A total of 792 studies were screened by their
abstracts (Fig. 1). Out of the 12
studies retrieved for full-text analysis, 5 were excluded. The
reasons for exclusion were as follows: The use of non-invasive
ventilation in the control group (19), the use of supplementary oxygen during
home activities (20), crossover
trial (21), the absence of a
control group (22), and trials on
pre-tested subjects showing improvement with supplemental oxygen
(23). A total of 7 trials were
included in this systematic review and meta-analysis (11–13,15,24–26).
Characteristics of the included
studies
The details of studies included in the review are
presented in Table II. The sample
size was <20 patients per group in all studies, apart from 1
(25). Only 1 trial had a large
sample of 58 patients in the study and 53 patients in the control
group (25). Room air was used in
the control group in 1 trial (11),
while compressed/humidified air was used in the remaining studies.
The exercise protocol included cycle ergometry in 3 studies
(15,24,26) and
treadmill walking in 1 trial (13).
Physical training was carried out in 3 sessions/week in all studies
apart from 1 study (11), which
utilized a 5 session/week protocol. The duration of each session
varied from 30 min to 1 h. In 1 trial, utilizing a 24-week PR
program, outcomes were assessed at 12 and 24 weeks. To maintain
homogeneity with the remaining studies, which conducted a 6–10 week
PR program, outcome data of 12 weeks from this trial were included
(26).
 | Table II.Characteristics of included
studies. |
Table II.
Characteristics of included
studies.
|
|
| Participants | Age in years, mean
(SD) |
|
|
|
|
|
|
|---|
|
|
|
|
|
|
|
|
|
|
|
|---|
| Author, year | Study type | Study | Control | Study | Control | Gases used | Type of
exercise | Sessions per
week | Duration of each
session | Total duration of
training | (Refs.) |
|---|
| Rooyackers et
al, 1997 | RCT | 12 | 12 | 63 (5) | 59 (13) | S: 4 lpm
O2 by nasal cannula | 20 min cycling (2
min exercise then 2 min rest), 5 min rowing, 5 min pulley
(arm, | 5 | 80 min with rest
(51 min exercise) | 10 weeks | (11) |
|
|
|
|
|
|
| C: Room air | shoulder), 5 min
back and abdominals, 3 min isometric strength training of arms and
shoulders and legs, 3 min stair climb, 5 min chair sit/stand and
slalom walk, 5 min arm weights |
|
|
|
|
| Garrod et
al, 2000 | RCT | 11 | 11 | 64.3 (NR) | 71.6 (NR) | S: 4 lpm
O2 by nasal cannula | Upper limb at 1 kg,
lower limb at no resistance, fast walk over 10 m, cycle | 3 | 1 h | 6 weeks | (12) |
|
|
|
|
|
|
| C: 4 lpm compressed
air | ergometer unloaded
until intolerance |
|
|
|
|
| Wadell et
al, 2001 | RCT | 10 | 10 | 64.6 (6.1) | 68.3 (4.1) | S: 5 lpm
O2 by nasal cannula | Treadmill walk | 3 | 30 min | 8 weeks | (13) |
|
|
|
|
|
|
| C: 5 lpm compressed
air |
|
|
|
|
|
| Emtner et
al, 2003 | RCT | 14 | 15 | 66 (7) | 67 (10) | S: 3 lpm
O2 by nasal cannula | Cycle
ergometry | 3 | 45 min | 7 weeks | (15) |
|
|
|
|
|
|
| C: 3 lpm compressed
air |
|
|
|
|
|
| Scorsone et
al, 2010 | RCT | 10 | 10 | 67 (9) | 68 (7) | S: 40% supplemental
O2 | Cycle
ergometry | 3 | 40 min | 8 weeks | (24) |
|
|
|
|
|
|
| C: Humidified
air |
|
|
|
|
|
| Spielmanns et
al, 2014 | RCT | 19 | 17 | 65 (8.7) | 64 (8.4) | S: 4 lpm
O2 by nasal cannula | Cycle
ergometry | 3 | 30 min | 12 weeks | (26) |
|
|
|
|
|
|
| C: 4 lpm compressed
air |
|
|
|
|
|
| Alison et
al, 2019 | RCT | 58 | 53 | 69 (7) | 69 (8) | S: 5 lpm
O2 by nasal cannula | Initially, 20 min
of treadmill walking and 10 min stationary cycling, increased
to | 3 | 40 min | 8 weeks | (25) |
|
|
|
|
|
|
| C: 5 lpm air | 20 min of treadmill
walking and 20 min stationary cycling by week 3 |
|
|
|
|
Outcomes and data analysis
The outcomes assessed varied across studies. Details
of the outcome variables and conclusions of individual studies are
presented in Table III.
 | Table III.Outcomes of included studies. |
Table III.
Outcomes of included studies.
| Author, year | Outcomes
assessed | Conclusions | (Refs.) |
|---|
| Rooyackers | i) Maximal cycle
ergometry-4 lpm O2 and room air | Pulmonary
rehabilitation improved exercise | (11) |
| et al,
1997 | ii) Constant power
cycle ergometry-30% O2 and | performance and
quality of life in both |
|
|
| room air | groups.
O2 supplementation during the |
|
|
| iii) 6MWT-4 lpm
O2 and room air | training did not
add to the effects of training |
|
|
| iv) Stair climb-up
4, plateau, down 3 | on room air. |
|
|
| v) Weight lift-lift
between racks |
|
|
|
| vi) Chronic
respiratory Disease Questionnaire |
|
|
|
| vii) PFT-Spirometry
and transfer coefficient for |
|
|
|
| carbon
monoxide |
|
|
| Garrod | i) Shuttle walk
test | Supplemental
O2 during training does little to | (12) |
| et al,
2000 | ii) Chronic
respiratory Disease Questionnaire | enhance exercise
tolerance although there is a |
|
|
| iii) Hospital
Anxiety and Depression Scale | small benefit in
terms of dyspnea. Patients with |
|
|
| iv) London Chest
Activity of Daily Living Scale | severe disabling
dyspnea may find symptomatic |
|
|
|
| relief with
supplemental oxygen. |
|
| Wadell | i) 6MWT on 5 lpm
O2 and 5 lpm compressed | Supplemental
O2 did not further improve the | (13) |
| et al,
2001 | air (random order)
with a 1 h rest in between | training effect,
compared with training with air, |
|
|
| ii) Arterial blood
gas analysis | in patients with
chronic obstructive pulmonary disease. |
|
| Emtner | i) Maximal cycle
ergometry-30% O2 and | Supplemental
O2 provided during high-intensity | (15) |
| et al,
2003 | compressed air | training yields
higher training intensity and |
|
|
| ii) Constant power
cycle ergometry-30% O2 | evidence of gains
in exercise tolerance in |
|
|
| and compressed
air | laboratory
testing. |
|
|
| iii) Chronic
respiratory disease questionnaire |
|
|
|
| iv) SF-36 |
|
|
|
| v) PFT-spirometry
and lung volume |
|
|
|
| vi) Arterial blood
gas analysis |
|
|
| Scorsone | i) PFT | O2
supplementation does not contribute to | (24) |
| et al,
2010 | ii) Maximal cycle
ergometry | improved exercise
performance in patients with |
|
|
| iii) Constant power
cycle ergometry | moderate to severe
COPD. |
|
|
| iv) Arterial blood
gas analysis |
|
|
| Spielmanns | i) 6MWT-room
air | O2
supplemental oxygen during the training | (26) |
| et al,
2014 | ii) Maximal cycle
ergometry-room air | program had no
additional benefits in improving |
|
|
| iii) SF-36 | quality of life and
exercise capacity in subjects |
|
|
|
| with
moderate-to-severe COPD. |
|
| Alison | i) Endurance
shuttle walk test | Both O2
and Air groups significantly improved | (25) |
| et al,
2019 | ii) Incremental
shuttle walk test | exercise capacity
and health related quality of life |
|
|
| iii) Chronic
Respiratory Disease Questionnaire | with no greater
benefit from training with |
|
|
| iv) Dyspnoea-12
Questionnaire | supplemental
O2 than with medical air. |
|
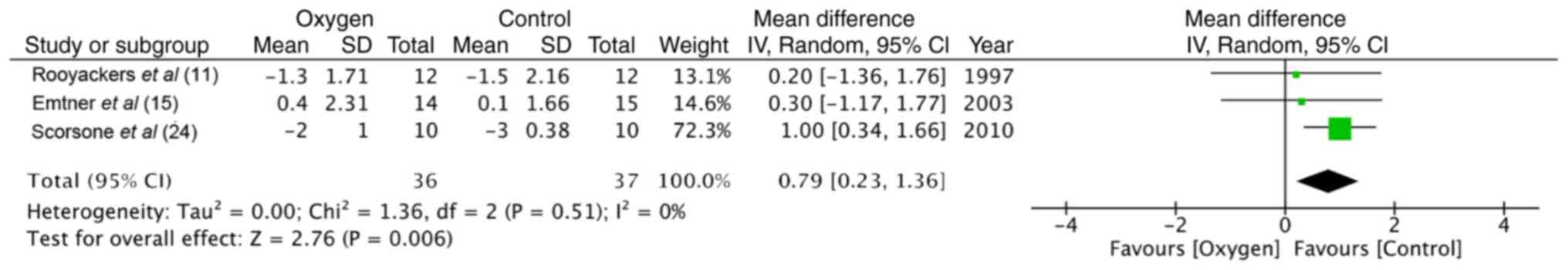
Maximal exercise capacity
Maximal exercise capacity was tested by cycle
ergometry in 4 trials (11,15,24,26). The
data of 55 participants in the study group and 54 in the control
group were pooled for a meta-analysis. No statistically significant
difference was found between the 2 groups in terms of power
(random: MD = −2.38; 95% CI, −5.79 to 1.03; P=0.86, I2 =
0%) (Fig. 2). Similarly, the maximum
energy expenditure (VO2 max) did not differ
significantly between the supplemental oxygen and control groups
(random: MD = −0.01; 95% CI, −0.06 to 0.07; P=0.45, I2 =
0%) (Fig. 3). End-of test dyspnea
scores were pooled from 3 trials (11,15,24). The
results of the meta-analysis indicated no significant advantage of
supplemental oxygen in reducing dyspnea scores (random: MD = 0.79;
95% CI, 0.23 to 1.36; P=0.51, I2 = 0%) (Fig. 4). End-of test oxygen saturation
(SpO2%) was measured by 2 studies (11,15).
Both reported no advantage of supplemental oxygen.
Constant power exercise capacity
Three trials (11,15,24) used
cycle ergometry to measure constant power exercise capacity. Data
were not homogenous to be pooled for a meta-analysis. Endurance
capacity, measured as an increase in exercise time, increased only
in the oxygen group in 1 study (11)
(the change was not significant), while in another trial (15), it improved significantly in both
groups. Isotime VO2 was recorded by 2 trials (15,24).
Both found no significant difference between the 2 groups. One
trial (15) found end-of test
dyspnea scores to be significantly improved in the oxygen group as
compared to the control group. End-of test oxygen saturation
(SpO2%), measured by 2 trials (11,15), did
not differ significantly between the 2 groups.
Functional exercise capacity
Three studies (11,13,26)
measured functional exercise capacity using 6-min walk tests
(6MWT). Pooled data of 41 participants in the study group and 39 in
the control group indicated no significant differences between the
2 groups (random: MD = −14.93; 95% CI, −32.64 to 2.78; P=0.93,
I2 = 0%) (Fig. 5). Two
trials (11,13) recorded end-of test dyspnea scores and
end-of test oxygen saturation and found no significant difference
between the supplemental oxygen and control groups.
Shuttle walk tests
Incremental shuttle walk tests were used as an
outcome measure in 2 trials (12,25).
While 1 study (25) found no
significant difference between groups, the other study recorded a
significant reduction in end-of test dyspnea scores in the oxygen
group (12). Data from the endurance
shuttle walk test from 1 trial (25)
demonstrated significant benefits in both groups with no
significant in-between group difference.
Quality of life
Health-related quality of life was measured using
the Chronic Respiratory Disease Questionnaire (CRQ) in 4 studies
(11,12,15,25).
Data of 95 participants in the study group and 91 participants in
the control group were analyzed. The results of meta-analysis of
total scores indicated no difference between the 2 groups (random:
MD = −0.09; 95% CI, −0.16 to −0.01; P=0.59, I2 = 0%)
(Fig. 6).
Quality of included studies
The authors' judgment of risk of bias of included
trials is presented in Fig. 7. A
total of 6 of the 7 studies described an adequate randomization
method (11–13,15,25,26).
Adequate information on allocation concealment was reported in 3
studies (11,12,25). The
blinding of participants and outcome assessment was clearly
reported in 4 trials (15,24–26). One
trial had a significant number of drop-outs from the study
(26).
Discussion
The primary objective of this systematic review and
meta-analysis was to analyze the beneficial effect of supplemental
oxygen during exercise training in patients with COPD. Overall, the
results of this review can be categorized into 3 sub-headings:
Exercise capacity, dyspnea scores and health-related quality of
life.
Exercise tolerance is an important predictor of
morbidity and mortality in COPD patients. A number of exercise
testing protocols were utilized by the included studies. While
maximal exercise testing measures the participants' response to a
gradually increasing workload, a constant power exercise test
assesses the participants systemic response to a constant metabolic
demand (27). Since maximal exercise
capacity is seldom reached during daily activities, the metabolic
load of day-to-day activities is more suitably assessed using the
constant power exercise test or other functional exercise tests
like 6 or 12 MWT and shuttle walk tests (28). These investigations are also more
sensitive to changes following intervention for exercise training
(2). Another disadvantage of a
maximal exercise test is the high level of motivation required on
behalf of the participant to achieve the actual maximal limit.
Secondly, approximately 6–10% of day-to-day variation in
VO2 max can be observed in patients with COPD (29). Maximal exercise test using cycle
ergometry was utilized by 4 of the 7 included trials. On pooling of
the data, supplemental oxygen during exercise training was not
found to be beneficial in improving VO2 max and power
output.
In the absence of homogenous data, quantitative
analysis was not carried out of the 3 trials reporting constant
power exercise tests. The results of endurance capacity, measured
as an increase in exercise time wer ambiguous. Emtner et al
(15), while reporting a significant
improvement in exercise time in both groups, reported better
outcomes in the supplemental oxygen group. The authors suggested
that the results may have been underestimated as 16 tests in the
oxygen-trained group were terminated at 30 min versus only 7 tests
in the control group. Rooyackers et al (11) found an increase in the cycling time
only in the experimental group with no change in the control group;
however, the change not was statistically significant. Outcome
measurements at specific time-points (isotime responses) during
constant power exercise tests are effort-independent and allow for
a more robust comparison of intervention effects (30). While our review indicates no
significant change in VO2 max and cardiovascular
parameters (heart rate and blood pressure) with supplemental oxygen
therapy, Emtner et al (15)
documented a slower and deeper pattern of breathing in the
oxygen-trained group.
Non-laboratory functional exercise tests, such as
6MWT have been validated to assess the functional status of
patients with COPD (31). Not only
are they easy to perform and inexpensive, but standardization is
also easy for measuring the effect of interventions. The results
from the meta-analysis of 6MWT suggest no benefits with the use of
supplemental oxygen during exercise training of patients with COPD.
Similar results were found by Garrod et al (12) and Alison et al (25) during shuttle walk tests. Although
some authors (13) have reported
better performance of the oxygen group during training sessions,
the outcome assessment on room air failed to demonstrate any
benefit despite prolonged training. One possible explanation
suggested is that control groups train under slight hypoxemia as
compared to the oxygen groups. The ‘slight hypoxemia’ causes
physiological stress, which is required for improving physical
capacity (13).
Dyspnea is an important symptom that limits exercise
tolerance in patients with COPD. The actual role of oxygen in
improving dyspnea is complex and not yet well understood (32). Dyspnea was recorded as an outcome
variable in majority trials of this review. However, meta-analysis
for dyspnea scores measured on the Borg scale was conducted only
for the maximal exercise test, which demonstrated no benefit of
supplemental oxygen therapy. Garrod et al (12) demonstrated a reduction in end-of test
dyspnea scores after shuttle walk tests but without any significant
change of other variables like exercise capacity and health-related
quality of life outcomes. The isolated dyspnea results may be
attributed to the small sample size of the study.
PR has been shown to significantly improve quality
of life outcomes in patients with COPD (7). PR programs include an exercise module
and an education/psychological support module. While the exact
contribution of each module in improving quality of life is
unknown, a recent review suggested that self-management educational
programs can significantly improve the quality of life of COPD
patients (33). Health-related
quality of life outcome was measured via CRQ in 4 studies (11,12,15,25)
included in the review. Our analysis failed to demonstrate any
beneficial effect of supplemental oxygen in improving the quality
of life of patients with COPD.
Some limitations of our study need to be elaborated.
The strength of any systematic review and meta-analysis depends
upon the homogeneity and quality of the included studies. The lack
of homogeneity of the included trials is the largest drawback of
this study. There was a wide variation in the methodology,
intervention, exercise protocol and outcome measurements, which
precluded a quantitative analysis for all variables. The inclusion
criteria also varied between studies. While majority trials were
carried out on participants who desaturate on exercise, studies by
Emtner et al (15) and
Spielmanns et al (26)
focused only on patients with COPD who were normoxemic at rest and
exercise. A sub-group analysis analyzing the effect of oxygen on
each group was not possible considering the heterogeneity.
Secondly, not all studies reported adequate allocation concealment
with blinding of participants and outcome assessment. A lack of
rigorous methodology could have affected results. Thirdly, the
sample size of majority studies was small with less than 20
participants per group.
Nevertheless, this study is an important update over
the previous review on this topic (2). Our results indicate that supplemental
oxygen during the exercise training of patients with COPD does not
improve exercise capacity, dyspnea scores and quality of life.
However, the quality of the evidence is weak. Multi-center RCTs
with homogenous methodology and intervention are required to
provide stronger evidence on this subject.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
All data generated or analyzed during this study are
included in this published article or are available from the
corresponding author on reasonable request.
Authors' contributions
YL and FG designed and searched literature. YL
prepared the manuscript. FG edited the manuscript. Both authors
have read and approved the final manuscript.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Celli BR and MacNee W; ATS/ERS Task Force,
: Standards for the diagnosis and treatment of patients with COPD:
A summary of the ATS/ERS position paper. Eur Respir J. 23:932–946.
2004. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Nonoyama ML, Brooks D, Lacasse Y, Guyatt
GH and Goldstein RS: Oxygen therapy during exercise training in
chronic obstructive pulmonary disease. Cochrane Database Syst Rev.
2:CD0053722007.
|
|
3
|
Ejiofor SI, Bayliss S, Gassamma A and
Turner AM: Ambulatory oxygen for exercise-induced desaturation and
dyspnea in chronic obstructive pulmonary disease (COPD): Systematic
review and meta-analysis. Chronic Obstr Pulm Dis. 3:419–434.
2016.PubMed/NCBI
|
|
4
|
Wagner PD: Skeletal muscles in chronic
obstructive pulmonary disease: Deconditioning, or myopathy?
Respirology. 11:681–686. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Spruit MA, Singh SJ, Garvey C, ZuWallack
R, Nici L, Rochester C, Hill K, Holland AE, Lareau SC, Man WD, et
al: An official American Thoracic Society/European Respiratory
Society statement: Key concepts and advances in pulmonary
rehabilitation. Am J Respir Crit Care Med. 188:e13–e64. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Ries AL, Bauldoff GS, Carlin BW, Casaburi
R, Emery CF, Mahler DA, Make B, Rochester CL, Zuwallack R and
Herrerias C: Pulmonary rehabilitation: Joint ACCP/AACVPR
evidence-based clinical practice guidelines. Chest. 131((5 Suppl)):
4S–42S. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
McCarthy B, Casey D, Devane D, Murphy K,
Murphy E and Lacasse Y: Pulmonary rehabilitation for chronic
obstructive pulmonary disease. Cochrane Database Syst Rev.
2:CD0037932015.
|
|
8
|
Henriksson J and Reitman JS: Quantitative
measures of enzyme activities in type I and type II muscle fibres
of man after training. Acta Physiol Scand. 97:392–397. 1976.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Cranston JM, Crockett A, Moss J and Alpers
JH: Domiciliary oxygen for chronic obstructive pulmonary disease.
Cochrane Database Syst Rev. CD0017442005.PubMed/NCBI
|
|
10
|
Jolly EC, Di Boscio V, Aguirre L, Luna CM,
Berensztein S and Gené RJ: Effects of supplemental oxygen during
activity in patients with advanced COPD without severe resting
hypoxemia. Chest. 120:437–443. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Rooyackers JM, Dekhuijzen PN, Van
Herwaarden CL and Folgering HT: Training with supplemental oxygen
in patients with COPD and hypoxaemia at peak exercise. Eur Respir
J. 10:1278–1284. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Garrod R, Paul EA and Wedzicha JA:
Supplemental oxygen during pulmonary rehabilitation in patients
with COPD with exercise hypoxaemia. Thorax. 55:539–543. 2000.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Wadell K, Henriksson-Larsén K and Lundgren
R: Physical training with and without oxygen in patients with
chronic obstructive pulmonary disease and exercise-induced
hypoxaemia. J Rehabil Med. 33:200–205. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Pépin JL and Lévy P: Principles of
oxygen therapyRespiratory Medicine. Gibson G, Geddes D, Costabel U,
Sterk P and Corrin B: 3rd. Saunders; Edinburgh: pp. 502–521.
2003
|
|
15
|
Emtner M, Porszasz J, Burns M, Somfay A
and Casaburi R: Benefits of supplemental oxygen in exercise
training in nonhypoxemic chronic obstructive pulmonary disease
patients. Am J Respir Crit Care Med. 168:1034–1042. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Moher D, Liberati A, Tetzlaff J and Altman
DG; PRISMA Group, : Preferred reporting items for systematic
reviews and meta-analyses: The PRISMA statement. PLoS Med.
6:e10000972009. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Higgins J and Green S: Cochrane Handbook
for Systemic Reviews of Interventions. Version 5.1.0. The Cochrane
Collaboration2011, http://handbook.cochrane.orgUpdated March
2011.
|
|
18
|
Higgins J, Altman D and Sterne J: Chapter
8: Assessing risk of bias in included studiesCochrane Handbook for
Systemic Reviews of Interventions. Version 5.1.0. The Cochrane
Collaboration. 2011, http://handbook.cochrane.orgUpdated March
2011.
|
|
19
|
Borghi-Silva A, Mendes RG, Toledo AC,
Malosá Sampaio LM, da Silva TP, Kunikushita LN, Dutra de Souza HC,
Salvini TF and Costa D: Adjuncts to physical training of patients
with severe COPD: Oxygen or noninvasive ventilation? Respir Care.
55:885–894. 2010.PubMed/NCBI
|
|
20
|
Ringbaek T, Martinez G and Lange P: The
long-term effect of ambulatory oxygen in normoxaemic COPD patients:
A randomised study. Chron Respir Dis. 10:77–84. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Neunhäuserer D, Steidle-Kloc E, Weiss G,
Kaiser B, Niederseer D, Hartl S, Tschentscher M, Egger A,
Schönfelder M, Lamprecht B, et al: Supplemental oxygen during
high-intensity exercise training in nonhypoxemic chronic
obstructive pulmonary disease. Am J Med. 129:1185–1193. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Helgerud J, Bjørgen S, Karlsen T, Husby
VS, Steinshamn S, Richardson RS and Hoff J: Hyperoxic interval
training in chronic obstructive pulmonary disease patients with
oxygen desaturation at peak exercise. Scand J Med Sci Sports.
20:e170–e176. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Dyer F, Callaghan J, Cheema K and Bott J:
Ambulatory oxygen improves the effectiveness of pulmonary
rehabilitation in selected patients with chronic obstructive
pulmonary disease. Chron Respir Dis. 9:83–91. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Scorsone D, Bartolini S, Saporiti R,
Braido F, Baroffio M, Pellegrino R, Brusasco V and Crimi E: Does a
low-density gas mixture or oxygen supplementation improve exercise
training in COPD? Chest. 138:1133–1139. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Alison JA, McKeough ZJ, Leung RWM, Holland
AE, Hill K, Morris NR, Jenkins S, Spencer LM, Hill CJ, Lee AL, et
al: Oxygen compared to air during exercise training in COPD with
exercise-induced desaturation. Eur Respir J. 53:18024292019.
View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Spielmanns M, Fuchs-Bergsma C, Winkler A,
Fox G, Krüger S and Baum K: Effects of oxygen supply during
training on subjects with COPD who are normoxemic at rest and
during exercise: A blinded randomized controlled trial. Respir
Care. 60:540–548. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Oga T, Nishimura K, Tsukino M, Hajiro T,
Ikeda A and Izumi T: The effects of oxitropium bromide on exercise
performance in patients with stable chronic obstructive pulmonary
disease. Am J Respir Crit Care Med. 161:1897–1901. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Singh SJ, Morgan MD, Hardman AE, Rowe C
and Bardsley PA: Comparison of oxygen uptake during a conventional
treadmill test and the shuttle walking test in chronic airflow
limitation. Eur Respir J. 7:2016–2020. 1994.PubMed/NCBI
|
|
29
|
Noonan V and Dean E: Submaximal exercise
testing: Clinical application and interpretation. Phys Ther.
80:782–807. 2000.PubMed/NCBI
|
|
30
|
Nicolò A, Bazzucchi I, Haxhi J, Felici F
and Sacchetti M: Comparing continuous and intermittent exercise: An
‘isoeffort’ and ‘isotime’ approach. PLoS One. 9:e949902014.
View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Lam HS, Lau FW, Chan GK and Sykes K: The
validity and reliability of a 6-metre timed walk for the functional
assessment of patients with stroke. Physiother Theory Pract.
26:251–255. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Sweer L and Zwillich CW: Dyspnea in the
patient with chronic obstructive pulmonary disease. Etiology and
management. Clin Chest Med. 11:417–445. 1990.PubMed/NCBI
|
|
33
|
Wang T, Tan JY, Xiao LD and Deng R:
Effectiveness of disease-specific self-management education on
health outcomes in patients with chronic obstructive pulmonary
disease: An updated systematic review and meta-analysis. Patient
Educ Couns. 100:1432–1446. 2017. View Article : Google Scholar : PubMed/NCBI
|