Introduction
Patellar fractures comprise 0.5–1.5% of all types of
bone fractures (1). Transverse
fractures are the most common type of patella fracture, which often
cause a functional disability of the knee extensor mechanism
(2). Surgical treatment is
recommended when there is >3 mm of fragment separation or a
step-like discontinuity on the articular surface >2 mm (3). The objectives of surgical treatment
include anatomical reduction of the articular surface, rigid
internal fixation, and the reconstruction of the knee extensor
mechanism, facilitating earlier functional exercises of the knee
joint and avoiding post-traumatic patellofemoral arthritis
(4–6).
Currently, methods combining interfragmentary screw
fixation with the tension band principle have been demonstrated to
provide enhanced fixation strength when compared with the modified
tension band construct alone, and have been more and more widely
used for the treatment of transverse patella fractures (7–10).
However, most of these methods are still performed with an open
technique that requires a long skin incision with a substantial
soft tissues dissection, resulting in a higher probability of
postoperative adhesions, prolonged disability (resulting in time
off work) and cosmetically unsightly scars (11).
In clinical practice, the authors of the current
study developed a new minimally invasive surgical (MIS) technique
to be used instead of the traditional open surgery (OS) technique
when using the Zimmer® Cable-Ready® Cable Pin
System, a combination of the interfragmentary screws (paralleled
pins) and the tension band wire (in a ‘figure eight’ formation) for
fixation of transverse patella fractures. The objective of the
current prospective study was to compare the MIS technique with OS
by analyzing postoperative clinical and radiographic results.
Patients and methods
Patient groups and randomization
Between April 2014 and July 2015, 38 patients with
clinical and X-ray evidence of transverse patella fractures with
displacements >3 mm were recruited at the Department of
Orthopaedics, Changhai Hospital Affiliated to the Second Military
Medical University (Shanghai, China). Age and sex distributions are
presented in Table I. Among them, 21
patients were randomly assigned (by a coin flip) to the MIS group
while 17 patients were assigned to the OS group by a scientist who
was blinded to the present study. Exclusion criteria included an
open fracture, a lower limb fracture on the same side, chronic
degenerative joint disease, previous knee surgical intervention,
peripheral neural damage and osteoporosis defined as bone mineral
density value 2.5 standard deviations or more below peak bone mass
(T-score ≤-2.5) measured by dual-energy X-ray absorptiometry
(12). The current study was
approved by the ethics review committee of the Second Military
Medical University and written informed consent was obtained from
all patients.
 | Table I.Patient characteristics. |
Table I.
Patient characteristics.
| Characteristic | MIS n=21 | OS n=17 | P-value |
|---|
| Sex |
|
|
|
| Male | 14 | 11 | 0.899a |
|
Female | 7 | 6 |
|
| Age (years) | 42.2±12.4 | 40.3±10.5 | 0.587b |
|
19-39 | 8 | 8 | 0.821a |
| 821 | 13 | 9 |
|
| Side of injury |
|
|
|
| Left | 12 | 6 | 0.310a |
|
Right | 9 | 11 |
|
| Mechanism of
injury |
|
|
|
| Fall | 14 | 15 | 0.148c |
| Traffic
accident | 5 | 2 |
|
| SRT | 2 | 0 |
|
| TLIO (hours) | 33.6±18.4 | 38.3±20.2 | 0.418b |
The Cable Pin System
The Zimmer® Cable-Ready® Cable
Pin System (Zimmer Biomet Holdings, Inc., Warsaw, IN, USA) is a new
type of internal fixation system, which consists of a cable and a
pin (Fig. 1). One end of the system
is the pin, a partially threaded 4.0 mm cancellous screw, which can
provide compression between fragments and prevent the cancellous
screw from backing out. The other end of the system is a guide
needle, which can easily be passed through bone tunnels. The
material connecting the two ends is a cable with a special braiding
structure. It is braided from 19 wires with each wire containing 7
monofilament wires with a diameter of 0.005 mm. Therefore, a cable
comprises 133 monofilament wires. This design provides the cable
with great strength and excellent pliability.
Surgical technique
All surgeries were performed by the same surgeon
(QZ). Spinal anesthesia or combined spinal-epidural anesthesia was
adopted for the surgery. The patient was positioned in the supine
position, with a sterile soft cushion used to support the injured
knee, leaving the joint in a 20° flexed position, allowing the knee
to perform flexion-extension movements.
i) MIS surgical technique
If the minor transverse fracture fragment was at the
proximal end and the major fragment was at the distal end of the
patella (Fig. 2), the site of the
proximal fragment would be confirmed and a ~3 cm longitudinal
midline incision would be made from the proximal end of the patella
down to the lower side of the proximal fragment (Fig. 3). The incision was from the skin to
the prepatellar fascia. The soft tissues were pulled downwardto
expose the fracture line. Any hematomas and traumatic bone debris
were removed, and the articular cavity was washed with normal
saline solution. Manipulative reduction was made with the
assistance of two towel clamps applied percutaneously. During the
reduction procedure, the knee joint was flexed and extended several
times, and the fragments were squeezed and pressed against to the
femoral condyle to facilitate the reduction of the articular
surface. A K-wire was then drilled superiorly and percutaneously
into the patella from the lower side of the apex for temporary
fixation following the reduction (Fig.
4A). A C-arm fluoroscopy was used to confirm the anatomical
reduction of the articular surface (Fig.
4B), and then the prepatellar fascia was sutured.
The proximal 3 cm incision was then pulled upward
and the inserting points for the two pins were selected at the
medial and lateral one-third of the superior pole of the patella.
Using a drill guide to protect the quadriceps tendon, the pins of
the Cable Pin System were inserted into the patella in an inferior
direction parallel to the articular surface. The threaded portions
of the pins were drilled across the fracture site, and the two pins
were directed in the patella parallel to each other and
perpendicular to the fracture line, which would provide compression
between the fragments (Fig. 5). Each
pin was drilled until it was slightly countersunk into the bone
cortex to prevent protrusion of the pin into the soft tissues. A 5
mm incision was made at the medial and lateral side of the distal
one-fourth to one-fifth of the patella, respectively. Following
this, two subcutaneous tunnels, starting from the proximal 3 cm
incision and ending at each of the distal 5 mm incision, were
created using a pair of curved forceps to divide the tissues under
the deep fascia covering the distal fracture fragment of the
patella. A horizontally directed bone tunnel was created anterior
to the pins, in the distal fragment, using a drill bit through the
medial and lateral 5 mm incisions (Fig.
6).
The leader of one cable was passed through the
prepatellar subcutaneous tunnel from the proximal 3 cm incision
(assumed as incision X) to the diagonal distal 5 mm incision
(assumed as incision Y; Fig. 7A).
The cable was then inserted into the horizontally directed bone
tunnel from incision Y and out of the tunnel at the other distal 5
mm incision (assumed as incision Z) (Fig. 7B). Finally, the same cable was passed
through the other prepatellar subcutaneous tunnel from incision Z
to X (Fig. 7C). The Cable Pin
Crimper (Zimmer Biomet Holdings, Inc.) was used to pull the two
cables crossed at incision X to remove slack and fasten them in a
crimp, forming a ‘figure eight’ (Fig.
7D). A cable cutter was used to cut the excess cables flush at
the crimp (Fig. 8). Thus, with the
exception of the interfragmentary screw fixation by the two
paralleled pins, the cable was in an incomplete ‘figure eight’,
which reflected the tension band principle (Fig. 9). If the fracture line was in the
distal half of the patella, the midline longitudinal incision would
be made at the distal end of the patella, accordingly, and the two
pins would be reversed and directed superiorly from the lower
side.
ii) Open surgery
The conventional midline longitudinal incision over
the patella, which was ~12 cm in length, was made and the fractures
exposed as described previously (13). Following the preliminary reduction of
the fracture, two pins of the Cable Pin System were inserted in
parallel into the patella through the midline longitudinal incision
to achieve interfragmentary compression. The two cables were
crossed in a ‘figure eight’ over the anterior surface of the
patella, with the leader of one cable passed through the
horizontally directed bone tunnel, and were pulled to remove slack
and fastened in a crimp. The excess cable flush was cut at the
crimp.
Postoperative treatments
For all the 38 patients, an elastic bandage was used
for 2 days after surgery to reduce swelling of the knee and the
likelihood of a hematoma. No immobilization was recommended.
Passive exercise was initiated 1 day after the surgery by a
continuous passive motion machine (Kinetec Optima®;
Kinetec S.A.), for three, 1-h sessions, starting from 0 to 60°,
increasing 15° per day until 90° was achieved. This training lasted
for 3–5 days. Active flexion exercises of the knee joint in prone
position were encouraged. The patients began to get out of bed 3
days after surgery and were encouraged to start bearing weight on
the leg that was operated on during level walking. Active extension
exercises of the knee joint were allowed 3 weeks after surgery, and
full weightbearing was allowed after the fracture was healed
following a radiographic assessment.
Postoperative follow-up and
assessment
Clinical and radiographical follow-up were performed
at 4 and 8 weeks, and at 12 months postoperatively. All the x-ray
films were read independently by two well-trained orthopedic
surgeons (QZ and HN). At 4 and 8 weeks, pain was measured using the
visual analog scale (VAS) (14) with
scores between 0 (no pain) and 10 (the most intense pain), and
active flexion and extension of the knee joint were measured in
degrees by a goniometry. The function of the knee was evaluated by
the clinical grading scale, defined by Bostman et al
(15), at week 8 and month 12. The
total score was stratified as follows: <20, unsatisfactory;
20–27, good; 28–30, excellent.
Statistical analysis
All values are mean ± standard deviation or number
of patients. The Mann-Whitney U test was used to compare
quantitative variables and the chi-square test with continuity
correction or the Fisher exact test was used to compare the
frequency distributions of categorical variables between the two
groups. All statistical analyses were performed using SPSS 15.0
statistical software (SPSS Inc., Chicago, IL, USA). P<0.05
indicated that the difference between groups was statistically
significant.
Results
All patients in the two groups completed ≥1 year of
follow-up time. No statistically significant differences were
identified in sex and age distributions, side distribution of the
fracture, the mechanism of injury or the time lag between injury
and operation between the two groups (Table I).
The average operating time was 49.0 and 52.2 min in
the MIS group and the OS group, respectively, and no significant
difference was observed between the two groups (Table II). The VAS score for pain was
significantly greater in the OS group compared with the MIS group
during the active movement of the injured knee joint at 4 and 8
weeks after surgery. The average angle of active extension of the
injured knee was significantly better in the MIS group at 4 weeks
after surgery, but this difference became non-significant at 8
weeks, when compared with the OS group. The average angle of active
flexion was significantlybetter in the MIS group at 4 and 8 weeks
compared with the OS group. The mean Bostman score reached 28.2
(range, 25–30) in the MIS group 8 weeks after surgery, indicating
asignificantly better function of the injured knee compared with
the OS group, though this difference became non-significant at 12
months. Until the last follow-up visit, no defect of the articular
surface, patellofemoral arthritic changes, breaking or backing out
of pin, or cable rupture was detected through radiological
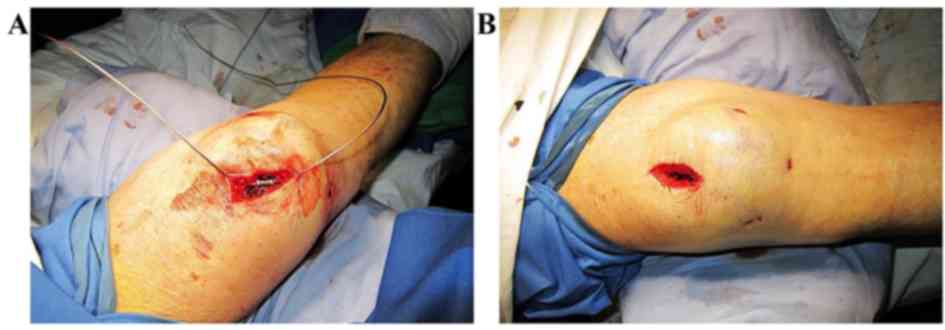
examinations. The longitudinal midline incision was only ≤3 cm in
the MIS group compared with an extensive soft tissue dissections in
the OS group (Fig. 10).
 | Table II.Comparison of postoperative results in
the MIS and OS patient groups. |
Table II.
Comparison of postoperative results in
the MIS and OS patient groups.
| Result | MIS n=21 | OS n=17 | P-value |
|---|
| Operating time
(min) | 49.0±10.2 | 52.2±12.7 | 0.461 |
| VAS score for
pain |
|
|
|
| 4
weeks | 4.0±1.1 | 5.4±1.0 | 0.001 |
| 8
weeks | 1.6±1.3 | 3.5±1.6 | 0.001 |
| Flexion (°) |
|
|
|
| 4
weeks | 52.6±18.3 | 35.5±10.6 | 0.004 |
| 8
weeks | 91.1±14.3 | 75.3±15.2 | 0.005 |
| Extension (°) |
|
|
|
| 4
weeks | −5.0±4.7 | −9.4±6.6 | 0.033 |
| 8
weeks | −1.2±4.4 | −3.5±5.5 | 0.184 |
| Bostman score |
|
|
|
| 8
weeks | 28.2±1.7 | 27.1± 2.2 | 0.038 |
| 12
months | 28.9±1.1 | 28.4±1.1 | 0.162 |
Discussion
MIS is the trend of development in modern surgery
(16). This less painful technique
has been demonstrated to be associated with earlier mobilization
and rehabilitation, a higher functional score of the knee, fewer
joint adhesions or less ankylosis, and lower incidence of wound
complications (16–20). Several studies have investigated MIS
or the percutaneous technique for transverse patella fractures
(17–19). Luna-Pizarro et al (17) performed percutaneous patellar
osteosynthesis using tension band wiring with the aid of a
specifically designed device and revealed that it was superior to
the conventional OS approach. However, it was pointed out that the
intraarticular hematoma and bone marrow particles or small
chondral/osteochondral fragments could not be washed out of the
joint, which may have caused joint adhesions and prolonged
disability during the rehabilitation period (21). Other studies assessed the
arthroscopic-assisted reduction and percutaneous fixation of
displaced patellar fractures (18,19).
However, the technique was technically demanding and not suitable
for the fractures accompanied by the disruption of the extensor
mechanism (18,19).
In the present study, a MIS technique was introduced
and compared with OS when using the Cable Pin System for transverse
patella fractures. The longitudinal midline incision was only ≤3
cm, with two subcutaneous tunnels and a bone tunnel, instead of
extensive soft tissue dissections. In the MIS group, a lower VAS
score for pain was observed at 4 and 8 weeks after surgery, which
could be partially attributed to less destruction of the soft
tissues compared with the OS group. Additionally, the mean angle of
active flexion or extension of the injured knee and the Bostman
functional score, were greater in the MIS group at 4 weeks, and the
mean angle of active flexion was still greater in the MIS group at
8 weeks compared with the OS group, indicating better knee
functions in the early period after surgery. Although those
differences between the two groups could no longer be identified at
the final follow-up, the MIS technique may help patients get back
to the daily work and life earlier with less pain and smaller
scars, improving patient satisfaction.
The authors of the current study elected to not use
a completely percutaneous technique but rather a MIS or
‘semi-percutaneous’ technique as they hypothesized that, unlike
shaft fractures of the limbs, the transverse patella fracture was
more often an intraarticular fracture. Intraarticular hematomas and
traumatic debris, which may cause joint adhesions and prolonged
disability during the rehabilitation period, should be washed out
of the joint. Through the minimally invasive incision, all the
procedures, including removal of intraarticular hematomas and
traumatic debris, dislodgment of the entrapped soft tissue, the
reduction of the fractures and reconstruction of the knee extensor
mechanism, could be carried out. The MIS technique introduced in
the current study had minimal soft tissue disruption, fewer
complications (data not shown) and better outcomes. MIS techniques
may also be applicable to other patterns of internal fixation, such
as interfragmentary screws with tension band wiring or cable.
A limitation of this MIS technique was that the
reduction would be difficult through the minimally invasive
incision when there were multiple fragments at the fracture site
and thus it was not suited to those patella fractures with
comminution of the fragments. Additionally, it is possible that
there were complications, which we had not identified due to the
short follow-up time, and longer follow-ups are required in the
future. Another limitation was the sample size and small
differences of in results between the two groups did not have
clinical relevance.
In conclusion, the MIS technique for transverse
patella fractures was demonstrated to provide better clinical
results and knee functions with less pain when compared to OS in
the early period following surgery. It could be an adequate
alternative in the treatment of transverse patella fractures.
Large-scale studies are necessary to further confirm the
effectiveness of this technique.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
JS, JW, YC and NM performed the experiments. QZ and
HN designed and directed the experiments. JS and JW wrote the
manuscript.
Ethics approval and consent to
participate
The current study was approved by the ethics review
committee of the Second Military Medical University and written
informed consent was obtained from all patients.
Patient consent for publication
All patients consented to the publication of the
current article.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Galla M and Lobenhoffer P: Patella
fractures. Chirurg. 76:987–997. 2005.(In German). View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Boström A: Fracture of the patella. A
study of 422 patellar fractures. Acta Orthop Scand Suppl. 143:1–80.
1972. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Gosal HS, Singh P and Field RE: Clinical
experience of patellar fracture fixation using metal wire or
non-absorbable polyester - a study of 37 cases. Injury. 32:129–135.
2001. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Weber MJ, Janecki CJ, McLeod P, Nelson CL
and Thompson JA: Efficacy of various forms of fixation of
transverse fractures of the patella. J Bone Joint Surg Am.
62:215–220. 1980. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Lotke PA and Ecker ML: Transverse
fractures of the patella. Clin Orthop Relat Res. 180–184.
1981.PubMed/NCBI
|
|
6
|
Catalano JB, Iannacone WM, Marczyk S,
Dalsey RM, Deutsch LS, Born CT and Delong WG: Open fractures of the
patella: Long-term functional outcome. J Trauma. 39:439–444. 1995.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Burvant JG, Thomas KA, Alexander R and
Harris MB: Evaluation of methods of internal fixation of transverse
patella fractures: A biomechanical study. J Orthop Trauma.
8:147–153. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Cekin T, Tükenmez M and Tezeren G:
Comparison of three fixation methods in transverse fractures of the
patella in a calf model. Acta Orthop Traumatol Turc. 40:248–251.
2006.(In Turkish). PubMed/NCBI
|
|
9
|
Curtis MJ: Internal fixation for fractures
of the patella. A comparison of two methods. J Bone Joint Surg Br.
72:280–282. 1990. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Cho JH: Percutaneous cannulated screws
with tension band wiring technique in patella fractures. Knee Surg
Relat Res. 25:215–219. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Gardner MJ, Griffith MH, Lawrence BD and
Lorich DG: Complete exposure of the articular surface for fixation
of patellar fractures. J Orthop Trauma. 19:118–123. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Kanis JA, Melton LJ 3rd, Christiansen C,
Johnston CC and Khaltaev N: The diagnosis of osteoporosis. J Bone
Miner Res. 9:1137–1141. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Sanders R and Gregory PR: Patella
fractures and extensor mechanism injuriesSkeletal trauma basic
science, management, and reconstruction. 4th. Saunders Elsevier
Inc.; Philadelphia, PA: pp. 2013–2015. 2009
|
|
14
|
Butler PV: Linear analogue self-assessment
and procrustean measurement: A critical review of visual analogue
scaling in pain assessment. J Clin Psychol Med Settings. 4:111–129.
1997. View Article : Google Scholar
|
|
15
|
Bostman O, Kiviluoto O and Nirhamo J:
Comminuted displaced fractures of the patella. Injury. 13:196–202.
1981. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Zeng BF: Minimally invasive surgery in
fracture management. Chin Med J (Engl). 121:1349–1351. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Luna-Pizarro D, Amato D, Arellano F,
Hernandez A and Lopez-Rojas P: Comparison of a technique using a
new percutaneous osteosynthesis device with conventional open
surgery for displaced patella fractures in a randomized controlled
trial. J Orthop Trauma. 20:529–535. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
El-Sayed AM and Ragab RK:
Arthroscopic-assisted reduction and stabilization of transverse
fractures of the patella. Knee. 16:54–57. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Turgut A, Günal I, Acar S, Seber S and
Göktürk E: Arthroscopic assisted percutaneous stabilization of
patellar fractures. Clin Orthop Relat Res. 57–61. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Atesok K, Doral MN, Whipple T, Mann G,
Mei-Dan O, Atay OA, Beer Y, Lowe J, Soudry M and Schemitsch:
Arthroscopy-assisted fracture fixation. Knee Surg Sports Traumatol
Arthrosc. 19:320–329. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Kose KC, Kuru I, Maralcan G and Altinel L:
Comparison of a technique using a new percutaneous osteosynthesis
device with conventional open surgery for displaced patella
fractures. J Orthop Trauma. 21:77–78. 2007. View Article : Google Scholar : PubMed/NCBI
|