Introduction
In Mexico City, for each 1,000 live births, 16.5 to
20 are infants born with congenital cardiac disease. Using
birthdate information, we have calculated that 10,000 to 12,000
infants are born with some type of cardiac malformation each year.
Mortality caused by congenital cardiopathy represents the sixth
leading cause of death in the first year of life and has a 3.2%
rate; it represents the ninth leading cause of death in children
aged 1 to 4 years (1.6% rate), and the 14th leading cause of death
in children aged over 5 years (1.1% rate) (1).
Cardiac correction represents the first place in
pediatric surgery. Despite major advances in the past two decades,
sepsis is potential problem after surgery and can lead to death. In
the Pediatric Hospital at the Instituto Mexicano del Seguro Social
(National Medical Center), around 100 children per year are seen
with congenital cardiac malformations. Most of these infants
require cardiac surgery, and more than 60% require cardiopulmonary
bypass (CPB). Sixty percent of those who receive CPB may develop an
infection (2).
Infants undergoing heart surgery are at increased
risk for developing immunosuppression and severe infection
(2). These children may also develop
various complications caused by the physiological response to
ischemia-reperfusion damage (3–4). Many
researchers have considered that this damage may be generated by
CPB, and some have reported lymphopenia after CPB possibly caused
by apoptosis of lymphocytes (5–7).
However, only a few studies have reported lymphopenia in children
(2–8). Patients who develop lymphopenia often
display a characteristic systemic inflammatory response syndrome
(SIRS), which may result from the infection itself or may be a
secondary response of damage-associated molecular patterns to the
original event, such as surgery or hypoxia (9,10).
Bacteremia can cause systemic inflammatory response
and sepsis (11). When bacteria
reach the blood, a set of mechanisms is activated to eliminate the
microorganisms through the release of proinflammatory mediators and
chemical agents. These agents stimulate the immune system to act at
the vascular endothelial level, which can cause damage to blood
vessels and increase permeability. This response activates a plasma
cascade of powerful vasoconstrictors, such as cytokines,
interleukin 1 (IL-1β), IL-6, cyclooxygenase, and lipoxygenase,
which are also involved in the adaptive immune response and send
signals to stimulate apoptosis and produce myocardial
depression.
These changes can cause shock, which activates the
coagulation cascade and the complement cascade, and can
subsequently cause thrombosis in small vessels and hemorrhage at
different levels. This plasma cascade simultaneously stimulates
several chemical agents, which respond to tissue damage, activation
and recruitment of cells such as macrophages, neutrophils, and
lymphocytes, and release of inflammatory mediators (12,13).
Immune cells display membrane receptors called
Toll-like receptors (TLRs). TLRs represent a group of transmembrane
proteins that function as pattern-recognition receptors by
detecting and responding to microbial ligands, which are defined as
pathogen-associated molecular patterns (PAMPs) (14,15).
PAMPs are involved in the processes of bacteremia and endotoxemia,
promote the release of systemic proinflammatory cytokines, and
worsen damage caused by the infection. Bacterial cell wall
products, such as lipopolysaccharide (LPS), lipoteichoic acid, and
peptidoglycans trigger expression of many inflammatory cytokines in
monocytes. LPS, also known as endotoxin, is a major constituent of
the outer membrane of Gram-negative bacteria; LPS elicits an immune
reaction that is responsible for many of the harmful effects in
patients with septic shock (15).
This signal pathway activates a variety of transcription factors,
such as nuclear factor κB (NF-κB), which induces the production of
inflammatory mediators that maintain the inflammatory cycle
(16,17).
It is clear that LPS cannot be responsible for all
clinical features of sepsis and those other factors must also
contribute to sepsis (18). The
major wall components of pathogenic agents and nonpathogenic agents
are considered to contribute to the development of sepsis, septic
shock, and multiple organ dysfunction syndrome (MODS) (19). Similar to LPS, they can interact with
TLR4 and CD14 to initiate signal transduction pathways that lead to
NF-kB activation (20,21). Activation of SIRS, which is generally
chaotic, causes endothelial damage. Damage to the systemic
circulation and microcirculation can cause mitochondrial discharge
and increased extraction and consumption of oxygen. These changes
can cause tissue hypoxia, and hyperlactatemia. Hypoxia and other
types of damage can lead cells to autodestruct through mechanisms
such as apoptosis, which can elicit sequential organ failure and
eventually MODS (22–26).
In the present study, we examined the effects of
cardiac surgery with and without CPB on lymphopenia in children
with congenital cardiac disease. We sought to determine whether
lymphopenia is caused by apoptosis of T and/or B lymphocytes, which
is of relevance since it allows us to know a possible mechanism of
lymphocyte reduction.
Patients and methods
Patients
The study included for 2 years, all children with
congenital heart disease who required cardiac surgery with and
without CPB, who were treated at the Pediatric Hospital of the
Siglo XXI National Medical Center of the Mexican Institute of
Social Security in Mexico City. During this period of time, the
group of children that required CPB was greater than the one that
did not require it. The control group was the children without
bypass. Patients ≥15 years of age, with any autoimmune disease,
diabetes, cancer or who had received previous treatment with
anticoagulants, were excluded from the study. Sixty-eight patients
with congenital cardiopathy needing surgery were studied: 53 who
received the surgery with CPB and 15 without CPB. There were 30
girls and 38 boys (male-to-female ratio 1.2:1) and their average
age was 44.6 months. The present study has been approved by the
Ethics Committee of the Health Research Commission by Dr Zamira
Apis Hernández (approval no. 2005-3603-0022). Written informed
consent was obtained from all parent or legal guardian from
patients prior to enrollment in the study.
Central venous blood was taken from the central
catheter in most patients; for patients without a central catheter,
the samples were obtained using a venipuncture of a peripheral
vein.
Blood was collected using disposable pyrogen-free
syringes (Becton Dickinson, Franklin Lakes, NJ, USA) into two
sterile tubes, one with heparin and the other without heparin.
Methods
The total lymphocyte count and complete blood count
were measured before and after surgery. Lymphopenia was defined as
a lymphocyte count <1,000/mm3.
Peripheral blood mononuclear cells (PBMC) were
isolated for quantification and cell counts using specific membrane
markers to quantify the subpopulations of helper and cytotoxic T
lymphocytes and B lymphocytes before, immediately after, and 24 h
after surgery. Briefly, PBMC were isolated from central blood
samples on a Lymphoprep gradient (Axis Shield, Oslo, Norway), and
the concentration was adjusted to 5×105 cells/ml in RPMI
1640 medium (Life Technologies, Invitrogen, Carlsbad, CA, USA).
The number of apoptotic lymphocytes cells was
assessed using Annexin V-Fluos (BD Biosciences, San Diego, CA, USA)
and flow cytometry (FACS Aria IIu, Becton Dickinson, USA). The
cells were labeled with specific antibodies:
Anti-CD19-allophycocyanin (APC), anti-CD3-phycoerythrin (PE),
anti-CD4-PE, and anti-CD8-PE-Cy5 (BD Biosciences). Isotype controls
were IgG1-PE, IgG2-APC, and IgG1k-PE-Cy5 (BD Biosciences).
The amount of serum IL-2 was measured by
enzyme-linked immunosorbent assay (BD OptEIA™ Set Human IL-2 (BD
Biosciences).
Sepsis was documented based on established criteria
(12) and by the presence and
identification of microorganisms in cultures. Clinical follow-up
was completed until the patients were released from the pediatric
intensive care unit or hospital.
Statistical analysis
The qualitative variables were expressed in absolute
frequencies and percentages, and the quantitative variables in
median and interquartile ranges. Inferential statistics were
performed comparing subjects with and without extracorporeal pump
using χ2 test in qualitative variables and Mann Whitney
U in quantitative variables. To demonstrate the differences between
the pre and post measurements between the groups, Wilcoxon test was
used. P<0.05 was considered to indicate statistically
significant difference. All statistical analyses were performed
using IBM SPSS Statistics software (v. 20; IBM Corp., Armonk, NY,
USA).
Results
Demographic and clinical
characteristics
Sixty-eight pediatric patients with cardiac
congenital alterations needed cardiac surgery; 53 required surgery
with CPB and 15 had surgery without CPB. There were 37 (54.4%) boys
and 31 (45.6%) girls; 28 (52.8%) boys and 25 (47.2%) girls received
CPB, and nine (60%) boys and six (40%) girls did not receive CPB.
The male-to-female ratios were 1.12:1 in patients who received CBP
and 1.5:1 in those who did not receive CBP. The median age was 34
months in the CBP group and 23 months in the non-CBP group
(Table I). The most frequent
cardiopathy was shunt (left-right), 64.2% in the CBP group and
33.3% in the non-CBP group. The most frequent surgical correction
was definitive repair, 96.2% in the CBP group and 66.7% in the
non-CBP group.
 | Table I.Patient information. |
Table I.
Patient information.
|
| Total, n=68 | Without CPB,
n=15 | With CPB, n=53 |
|
|---|
|
|
|
|
|
|
|---|
| Characteristic | Frequency | % | Frequency | % | Frequency | % | P-value |
|---|
| Sex |
|
|
|
|
|
| 0.08 |
|
Male | 37 | 54.4 | 9 | 60.0 | 28 | 52.8 |
|
|
Female | 31 | 45.6 | 6 | 40.0 | 25 | 47.2 |
|
| Age
(months)a | 33 | (10.5–61) | 23 | (12–30) | 34 | (9–62) | 0.05 |
| Weight
(kg)a | 11.1 | (7.6–18) | 11 | (8–19) | 11.2 | (6.8–18) | 0.70 |
| Size
(cm)a | 87 | (65.5–110) | 84 |
(66–110) | 88 | (66–110) | 0.80 |
| Extracorporean
derivation time (min) |
|
|
|
| 105 | (87–125) |
|
| Type of congenital
heart disease |
|
|
|
|
|
| 0.002 |
| Right
ventricle obstruction outflow | 21 | 30.9 | 4 | 26.7 | 17 | 32.1 |
|
| Shunt
(left-right) | 39 | 57.4 | 5 | 33.3 | 34 | 64.2 |
|
| Anomaly
connection pulmonary veins | 4 | 5.9 | 3 | 20.0 | 1 | 1.9 |
|
| Left
outflow obstruction | 4 | 5.9 | 3 | 20.0 | 1 | 1.9 |
|
| Procedure |
|
|
|
|
|
| 0.001 |
|
Palliative | 7 | 10.3 | 5 | 33.3 | 2 | 3.8 |
|
|
Definitive repair | 61 | 89.7 | 10 | 66.7 | 51 | 96.2 |
|
| Complications |
|
|
|
|
|
|
|
| SIRS
(yes) | 35 | 51.5 | 10 | 66.7 | 25 | 47.2 | 0.7 |
| Sepsis
or septic shock (yes) | 7 | 10.3 | 0 | 0.0 | 7 | 13.2 | 0.7 |
|
Cardiogenic shock (yes) | 15 | 22.1 | 2 | 13.3 | 13 | 24.5 | 0.7 |
| MODS
(yes) | 6 | 8.8 | 1 | 6.7 | 5 | 9.4 | 0.8 |
| Mortality | 9 | 13.2 | 2 | 13.3 | 7 | 13.2 | 0.9 |
Blood count
Neutrophil count in patients with CPB increased
significantly (P=0.001), immediately after surgery and counts of
lymphocytes decreased significantly (Table II). In the non-CPB group, neutrophil
counts also increased significantly, and lymphocyte and monocytes
counts decreased significantly after surgery (Table II).
 | Table II.Complete blood count. |
Table II.
Complete blood count.
|
| Without CPB |
| With CPB |
|
|
|---|
|
|
|
|
|
|
|
|---|
|
Cell/mm3 | Median | Percentile 25 | Percentile 75 | P-value
(paired)a | Median | Percentile 25 | Percentile 75 |
P-valueb | P-value
(paired)a |
|---|
| Neutrophils
pre | 4.0 | 3.0 | 5.8 | 0.001 | 3.5 | 2.3 | 5.1 | 0.02 | 0.001 |
| Neutrophils
post | 9.9 | 6.0 | 13.9 |
| 8.3 | 5.0 | 10.5 |
|
|
| Lymphocytes
pre | 3.1 | 1.9 | 4.6 | 0.001 | 3.5 | 2.5 | 4.8 | 0.40 | 0.0001 |
| Lymphocytes
post | 1.5 | 0.9 | 1.9 |
| 1.6 | 1.1 | 2.1 |
|
|
| Monocytes pre | 0.7 | 0.4 | 1.1 | 0.03 | 0.7 | 0.6 | 1.0 | 0.04 | 0.7 |
| Monocytes post | 1.1 | 0.5 | 1.2 |
| 0.6 | 0.3 | 1.0 |
|
|
| Eosinophils
pre | 0.2 | 0.1 | 0.49 | 0.6 | 0.2 | 0.1 | 0.3 | 0.70 | 0.7 |
| Eosinophils
post | 0.0 | 0.0 | 0.01 |
| 0.0 | 0.0 | 0.05 |
|
|
| Basophils pre | 0.0 | 0.0 | 0.10 | 0.7 | 0.1 | 0.0 | 0.1 | 0.90 | 0.8 |
| Basophils post | 0.0 | 0.0 | 0.001 |
| 0.0 | 0.0 | 0.01 |
|
|
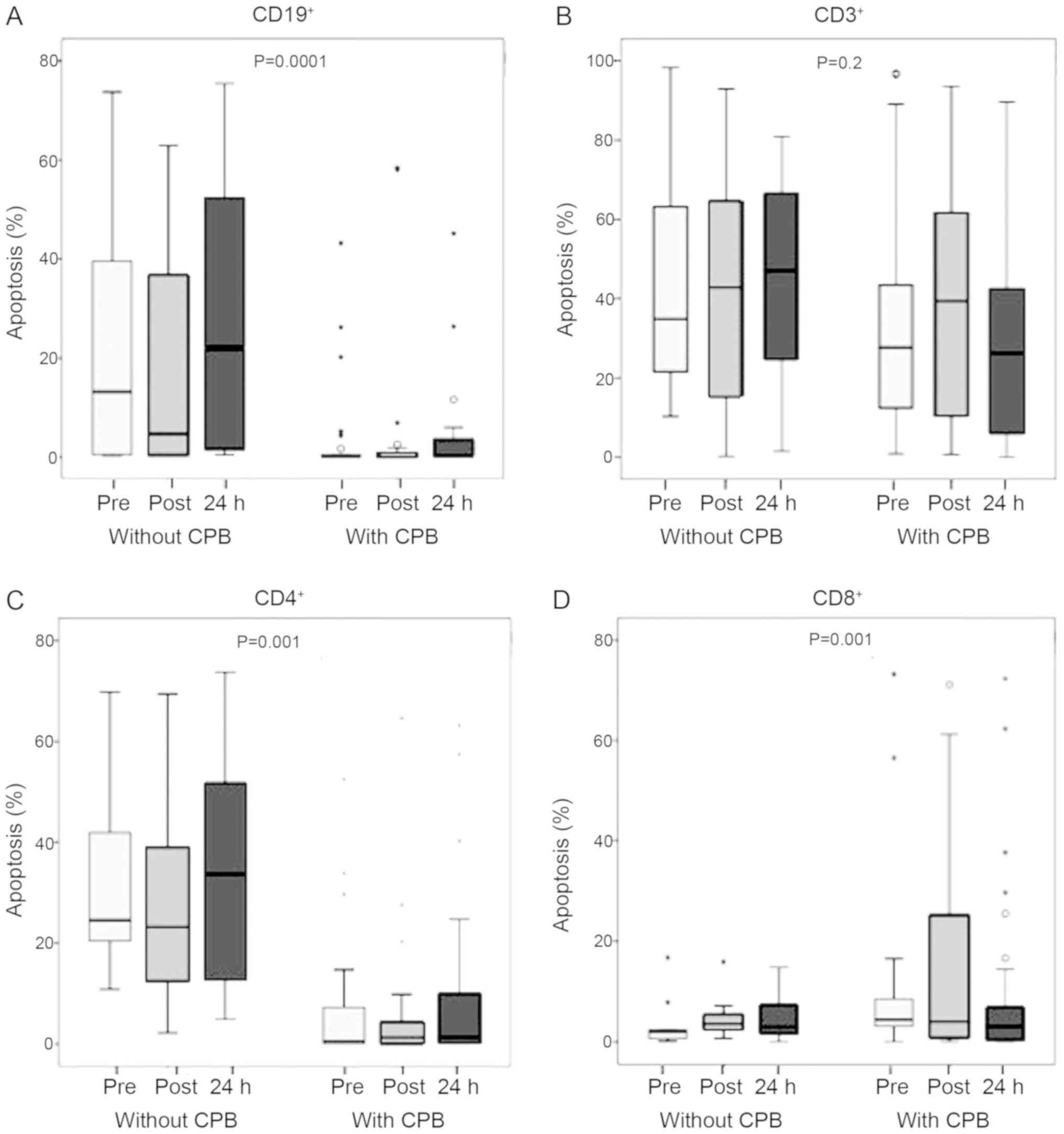
Apoptosis of B and T lymphocytes
We next determined whether the decrease in
lymphocyte count observed in patients undergoing cardiac surgery
with or without CPB was caused by apoptosis of populations of
CD3+ (CD4+, and CD8+) T
lymphocytes, and CD19+ B lymphocytes. The percentage of
apoptotic B (CD19+) lymphocytes was higher in patients
who underwent surgery without CPB than in those who received CPB
(P=0.0001). The percentage of apoptotic cells before surgery was
from 14 to 0% without and with CPB respectively. This percentage
was slightly but not significantly higher 24 h after surgery in
both groups (Fig. 1A).
The percentage of apoptotic CD3+ T
lymphocytes before surgery was similar in both groups (34%). This
percentage increased slightly after surgery but decreased 24 h
later; none of these changes were significant (P=0.2; Fig. 1B). Apoptosis affected 25% of
CD4+ T lymphocytes in without CPB group before surgery,
and this percentage was significantly lower in the CPB group (2%).
The percentage of apoptotic T (CD4+) lymphocytes was
higher in patients who underwent surgery without CPB than in those
who received CPB (P<0.001; Fig.
1C). The percentage of apoptotic CD8+ T lymphocytes
was higher in the CPB group (5%) than in the non-CBP group (2%;
P<0.001). Apoptosis of CD8+ T lymphocytes increased
non significantly immediately and 24 h after surgery in both groups
(Fig. 1D). In Fig. S1 we shown the apoptosis analysis dot
plots of one patient (patient 10), indicating percentages of
apoptosis of B (CD19+) and T (CD3+, CD4+) lymphocytes pre and
post-surgery with CPB.
Clinical complications
Clinical complications developed in a higher
percentage of patients in the CPB group (71.3%) than in the non-CPB
group (60%). A lower percentage of patients in the CPB group
developed SIRS [25 (47.2%) vs. 10 (66.7%)]. Importantly, sepsis
occurred only in the CPB group [7 patients (13.2%)]. Seven patients
(13.2%) died after surgery with CPB, two because of sepsis (28.6%).
Thirteen patients in the CPB group (24.5%) but only two patients in
the non-CPB group (13.3%) exhibited cardiogenic shock (Table I).
Sepsis and mortality
The microorganisms isolated are listed in Table III. Seven patients in the CPB group
(13.2%) died after surgery (Table
I); two (28.6%) died of sepsis and five (20.0%) died of SIRS.
By contrast, in the non-CPB group, only two patients (10%) died of
SIRS (Table I). The mortality rate
was similar in both groups (13.2 and 13.3% in the CPB and non-CPB
groups, respectively). The mortality rate was higher in boys
(85.7%) than in girls (14.3%) in the CPB group.
 | Table III.Sepsis etiology. |
Table III.
Sepsis etiology.
| A, Surgery with
CPB |
|---|
|
|---|
| Isolate
microorganism | Frequency | % |
|---|
| Staphylococcus
sp. | 2 | 3.8 |
| Enterobacter
cloacae | 1 | 1.9 |
| Escherichia
coli | 1 | 1.9 |
| Enterococcus
faecalis | 1 | 1.9 |
| Streptococcus
pneumoniae | 2 | 3.8 |
| Cultivo
negativo | 46 | 86.7 |
| Total | 53 | 100.0 |
|
| B, Surgery
without CPB |
|
| Isolate
microorganism | Frequency | % |
| Cultivo
negativo | 15 | 100.0 |
| Total | 15 | 100.0 |
Interleukin-2
Serum concentration of IL-2 was of 5 to 9 pg/ml, did
not change significantly from before to immediately and 24 h after
surgery and did not differ significantly between groups (data not
shown).
Discussion
Despite advances in technology and the development
of surgery to correct congenital heart defects, cardiopathy still
occurs at a rate of 5.2 to 12.5 per thousand live births in the
pediatric population. Currently in Mexico, six in 1,000 live births
per year present with congenital cardiopathy disease (1). It was previously thought that
lymphopenia in these patients is caused by the exclusive use of CPB
secondary to the effects of ischemia-reperfusion. The devices used
in surgery for these patients have evolved with advances in
technology. However, this situation continues because of factors
occurring during surgery, such as severe hypothermia, aortic
cross-clamping, duration of CPB, metabolic response to trauma,
hypoxia, or sudden changes in temperature. Other factors may also
be involved, such as gene regulatory mechanisms including the
responses of sepsis genes (26),
stress induced by the disease and/or surgery, the patient's
inherent susceptibility, and stress to hematopoietic tissue and
cells, which accelerates the biological cycle and can cause cell
self-destruction. Several studies of adults have reported multiple
complications secondary to the use of CPB. More recent studies of
children have been reported, but only up to 61 months of age. Shi
et al included only pediatric patients and found decreased
lymphocyte counts regardless of the use of CPB (2). Our findings support those of Shi et
al.
The complete blood counts showed similar cell
distributions in both groups of patients. However, despite this
similarity in cell counts, they should not be considered as only
one group before surgery because of differences in their presurgery
physiological condition, which may influence the decision of
cardiologists and surgeons about which patients need or do not need
CPB.
After surgery, patients in both groups showed a
significant increase in neutrophil count, which was probably caused
by an immediate immune response to the damage caused by the surgery
and was independent of the use of CPB. Most studies agree that the
increase in neutrophil count reflects an important change in cells
central to the inflammatory response and the recognition of
pathogens or their ligands. By contrast, lymphocyte count decreased
significantly in both groups, which was unexpected because studies
of adults have reported that lymphopenia occurs only in patients
undergoing surgery with CPB. As in our study, a previous study that
included pediatric patients reported reduced lymphocyte counts in
both patients operated on with and without CPB, although the
decrease was greater in the CPB group (2,27). In
other study that included infants, it was compared the clinical
effectiveness and biocompatibility of poly-2-methoxyethyl acrylate
(PMEA)-coated and heparin-coated CPB circuits in elective cardiac
surgery with CPB for ventricular septum defects, finding that the
leukocyte counts were significantly lower 5 min after CPB in the
PMEA group than the heparin group, showing that PMEA-coated
circuits cause transient leukopenia during pediatric CPB (28). However, this study was different from
ours, because they did not compare cardiac surgery with and without
CPB and did not determine the apoptosis of the lymphocytes. We also
found that the counts of all hematopoietic cell populations
decreased after surgery in the CPB group, which indicated
sensitivity to surgical stress in this group. Eosinophil count
decreased in patients undergoing surgery without CPB. The
differences in hematopoietic cell counts may reflect the
inflammatory response and/or synthesis of cytokines following
surgery (29). Different cytokines
are produced to stimulate the production of specific hematopoietic
lineages after damage to tissues (30).
The decrease in lymphocyte count may increase the
risk of developing an infection, which may lead to severe sepsis,
the precursor of MODS that can lead to death. In tertiary-level
hospitals, sepsis remains an important issue because it is the
leading cause of death in patients surgery to correct congenital
heart defects; it is also the main cause of admission to
postoperative therapy in heart-surgery patients. In this study, we
observed a higher frequency of cardiogenic shock and sepsis in
patients with CPB than in patients without CPB. However, sepsis
developed only in patients who received CPB. These findings suggest
the need for further understanding of the cellular, biochemical,
and molecular mechanisms underlying the responses of pediatric
patients who undergo surgery with CPB.
The decrease in lymphocyte count observed in our
study seemed to be caused by apoptosis of B lymphocytes
(CD19+) in the non-CPB group and of T lymphocytes
(CD8+) in the CPB group, although no significant
differences were found in the rate of apoptosis of B and T
lymphocytes after surgery in both groups. Several studies have
reported that CPB causes cytotoxic effects in several hematopoietic
lineages, such as a decreased mitogenic activity of lymphocytes or
morphological changes in neutrophils (29,31,32).
However, it seems that the effect may be greater in certain cell
lineages, although, to our knowledge, this has not been reported in
any previous work. We observed increased apoptosis of
CD8+ T lymphocytes after surgery with CPB and increased
apoptosis of B lymphocytes after surgery without CPB. The decreased
number of cells may be caused by a cytostatic effect given that
hematopoietic tissue is one of the most sensitive tissues to
environmental changes, such as temperature changes, contact with
foreign surfaces, or cell damage. It is probable that all of these
factors contribute to the decreased number of hematopoietic cells.
This is the first study to show that the decreased in lymphocyte
count in children undergoing corrective heart surgery, with and
without CPB, may result from increased apoptosis of CD8+
T and B lymphocytes. Then, in addition to analyzing the effects of
cardiac surgery with and without CPB in the reduction of
lymphocytes in children with congenital heart disease, we sought to
establish if the reduction of these lymphocytes was caused by the
apoptosis of the T lymphocytes and B lymphocytes, which is of
relevance since it allows us to know a possible mechanism of
lymphocyte reduction.
In addition, sepsis, and cardiogenic shock were also
higher in the CPB group. The rates of sepsis, cardiogenic shock and
MODS were higher in patients who underwent surgery with CPB. These
children also had the highest neutrophil counts and lowest
lymphocyte counts after surgery.
In this study, lymphocyte count decreased after
surgery in both groups, but the reason for this decrease seemed to
differ between the CPB and non-CPB groups. That is, the decrease in
lymphocyte count was probably related to apoptosis of B lymphocytes
(CD19+) in the no-CPB group but to apoptosis of T
lymphocytes (CD8+) in the CPB group. Apoptosis can be
activated by both intrinsic and extrinsic factors and hematopoietic
tissue is one of the most sensitive tissues to extrinsic factors,
such as temperature changes, contact with foreign surfaces, and
cell damage. These factors may be involved in the decreased number
of hematopoietic cells observed after cardiac surgery in infants.
However, it must be considered that the number of patients included
in the groups was different, which may be a limitation of the
study.
In conclusion, this is the first study to determine
the effects of cardiac surgery with and without CPB on leukocyte
subsets in children where it was observed that the decrease of
lymphocytes can be due to the increase in the apoptosis of the T
and B lymphocytes. The decreased lymphocyte count after heart
surgery may be caused by some of the events occurring during
surgery, but not necessarily the effects of CPB. Patients who
received CPB exhibited a large increase in neutrophil counts and a
decrease in lymphocyte, counts. These cells are important mediators
of the inflammatory response and recognition of pathogens and/or
their PAMPs. Leukocytosis seen after cardiac surgery with and
without CPB may have been caused by the increase in neutrophil
count. Lymphocyte count decreased after cardiac surgery in both the
CPB and non-CPB groups, this probably reflects apoptosis of B and T
lymphocytes in response to surgical stress and not to CPB by
itself.
Supplementary Material
Supporting Data
Acknowledgements
The authors would like to thank Dr Horacio Márquez
González (Oficina de Apoyo a la Investigación. Hospital Infantil de
México Federico Gómez) for the statistical reanalysis of the
results, Dr Karla Méndez Maldonado (Instituto de Fisiología
Celular-Neurociencias, Universidad Nacional Autónoma de México,
Ciudad Universitaria) for the reanalysis of the apoptosis results
and editing Fig. S1 and Dr Rocío
Nieto Menéses (Laboratorio de Investigación en Inmunología y
Proteómica. Hospital Infantil de México Federico Gómez) for editing
Fig. 1.
Funding
The present study was supported by Instituto
Mexicano del Seguro Social, Coordinación de Investigación en Salud,
Mexico City, Mexico (grant no. FIS/IMSS/PROT/C2007/053).
Availability of data and materials
The datasets used during the present study are
available from the corresponding author on reasonable request.
Authors' contributions
RJA, ERM and CMB contributed to the conception and
study design. RJA and NSZ contributed to the acquisition of data.
CMB, RJA and NSZ performed the cytometry analysis and
interpretation of data. RTF performed the statistical analyses of
the data. JZ, ASG and CR analyzed and interpreted the patient data
regarding the cardiology diseases. RJA, NSZ and CMB drafted the
manuscript. RJA, NSZ, ERM and CMB revised the manuscript critically
for intellectual content. All authors read and approved the final
manuscript.
Ethics approval and consent to
participate
The present study has been approved by the Ethics
Committee of the Health Research Commission by Dr Zamira Apis
Hernández (approval no. 2005-3603-0022). Written informed consent
was obtained from all parent or legal guardian from patients prior
to enrollment in the study.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Instituto Nacional de Estadística y
Geografía (INEGI). Webpage. http://www.inegi.org.mx/July 12–2018
|
|
2
|
Shi SS, Shi CC, Zhao ZY, Shen HQ, Fang XM,
Tan LH, Zhang XH, Shi Z, Lin R and Shu Q: Effect of open heart
surgery with cardiopulmonary bypass on peripheral blood lymphocyte
apoptosis in children. Pediatr Cardiol. 30:153–159. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Laffey JG, Boylan JF and Cheng DC: The
systemic inflammatory response to cardiac surgery: Implications for
the anesthesiologist. Anesthesiology. 97:215–252. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Stark J, Gallivan S, Lovegrove J, Hamilton
JR, Monro JL, Pollock JC and Watterson KG: Mortality rates after
surgery for congenital heart defects in children and surgeons'
performance. Lancet. 355:1004–1007. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Markewitz A, Faist E, Lang S, Endres S,
Fuchs D and Reichart B: Successful restoration of cell-mediated
immune response after cardiopulmonary bypass by immunomodulation. J
Thorac Cardiovasc Surg. 105:15–24. 1993. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Hisatomi K, Isomura T, Kawara T, Yamashita
M, Hirano A, Yoshida H, Eriguchi N, Kosuga K and Ohishi K: Changes
in lymphocyte subsets, mitogen responsiveness, and interleukin-2
production after cardiac operations. J Thorac Cardiovasc Surg.
98:580–591. 1989. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Chello M, Mastroroberto P, Quirino A, Cuda
G, Perticone F, Cirillo F and Covino E: Inhibition of neutrophil
apoptosis after coronary bypass operation with cardiopulmonary
bypass. Ann Thorac Surg. 73:123–130. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Habermehl P, Knuf M, Kampmann C, Mannhardt
W, Schranz D, Kuroczynski W, Wippermann CF and Zepp F: Changes in
lymphocyte subsets after cardiac surgery in children. Eur J
Pediatr. 162:15–21. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Wesche DE, Lomas-Neira JL, Perl M, Chung
CS and Ayala A: Leukocyte apoptosis and its significance in sepsis
and shock. J Leukoc Biol. 78:325–337. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Hotchkiss RS, Swanson PE, Knudson CM,
Chang KC, Cobb JP, Osborne DF, Zollner KM, Buchman TG, Korsmeyer SJ
and Karl IE: Overexpression of Bcl-2 in transgenic mice decreases
apoptosis and improves survival in sepsis. J Immunol.
162:4148–4156. 1999.PubMed/NCBI
|
|
11
|
Calandra T and Cohen J; International
Sepsis Forum Definition of Infection in the ICU Consensus
Conference, : The international sepsis forum consensus conference
on definitions of infection in the intensive care unit. Crit Care
Med. 33:1538–1548. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Goldstein B, Giroir B and Randolph A;
International Consensus Conference on Pediatric Sepsis, :
International pediatric sepsis consensus conference: Definitions
for sepsis and organ dysfunction in pediatrics. Pediatr Crit Care
Med. 6:2–8. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Szabo G, Romics L Jr and Frendl G: Liver
in sepsis and systemic inflammatory response syndrome. Clin Liver
Dis. 6:1045–1066. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Takeda K and Akira S: Toll-like receptors
in innate immunity. Int Immunol. 17:1–14. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Bianchi ME: DAMPs, PAMPs and alarmins: All
we need to know about danger. J Leukoc Biol. 81:1–5. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Guha M and Mackman N: LPS induction of
gene expression in human monocytes. Cell Signal. 13:85–94. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Lin M and Rikihisa Y: Ehrlichia
chaffeensis downregulates surface Toll-like receptors 2/4, CD14 and
transcription factors PU.1 and inhibits lipopolysaccharide
activation of NF-kappaB, ERK 1/2 and p38 MAPK in host monocytes.
Cell Microbiol. 6:175–186. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Opal SM: The host response to endotoxin,
antilipopolysaccharide strategies, and the management of severe
sepsis. Int J Med Microbiol. 297:365–377. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Lien E and Ingalls RR: Toll-like
receptors. Crit Care Med. 30 (Suppl 1):S1–S11. 2002. View Article : Google Scholar
|
|
20
|
Wang JE, Jørgensen PF, Almlöf M,
Thiemermann C, Foster SJ, Aasen AO and Solberg R: Peptidoglycan and
lipoteichoic acid from Staphylococcus aureus induce tumor necrosis
factor alpha, interleukin 6 (IL-6), and IL-10 production in both T
cells and monocytes in a human whole blood model. Infect Immun.
68:3965–3970. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Pålsson-McDermott EM and O'Neill LA:
Signal transduction by the lipopolysaccharide receptor, Toll-like
receptor-4. Immunology. 113:153–162. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Shimaoka M and Park EJ: Advances in
understanding sepsis. Eur J Anaesthesiol Suppl. 42:146–153. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Weigand MA, Hörner C, Bardenheuer HJ and
Bouchon A: The systemic inflammatory response syndrome. Best Pract
Res Clin Anaesthesiol. 18:455–475. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Li S, Price R, Phiroz D, Swan K and Crane
TA: Systemic inflammatory response during cardiopulmonary bypass
and strategies. J Extra Corpor Technol. 37:180–188. 2005.PubMed/NCBI
|
|
25
|
Day JR and Taylor KM: The systemic
inflammatory response syndrome and cardiopulmonary bypass. Int J
Surg. 3:129–140. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Castellheim A, Brekke OL, Espevik T,
Harboe M and Mollnes TE: Innate immune responses to danger signals
in systemic inflammatory response syndrome and sepsis. Scand J
Immunol. 69:479–491. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Aldemir M, Baki ED, Adali F, Çarşanba G,
Tecer E and Taş HU: Comparison of neutrophil:lymphocyte ratios
following coronary artery bypass surgery with or without
cardiopulmonary bypass. Cardiovasc J Afr. 26:159–164. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Itoh H, Ichiba S, Ujike Y, Douguchi T,
Kasahara S, Arai S and Sano S: A prospective randomized trial
comparing the clinical effectiveness and biocompatibility of
heparin-coated circuits and PMEA-coated circuits in pediatric
cardiopulmonary bypass. Perfusion. 31:247–254. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Khabar KS, elBarbary MA, Khouqeer F, Devol
E, al-Gain S and al-Halees Z: Circulating endotoxin and cytokines
after cardiopulmonary bypass: Differential correlation with
duration of bypass and systemic inflammatory response/multiple
organ dysfunction syndromes. Clin Immunol Immunopathol. 85:97–103.
1997. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Miller BE and Levy JH: The inflammatory
response to cardiopulmonary bypass. J Cardiothorac Vasc Anesth.
11:355–366. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Meldrum DR: Tumor necrosis factor in the
heart. Am J Physiol. 274:R577–R595. 1998.PubMed/NCBI
|
|
32
|
Hill GE: Cardiopulmonary bypass-induced
inflammation: Is it important? J Cardiothorac Vasc Anesth. 12 (2
Suppl 1):S21–S25. 1998.
|