Introduction
Lupus nephritis (LN) is one of the most common
clinical manifestations and serious complications in patients with
systemic lupus erythematosus (SLE). Almost all patients with SLE
have renal damage in the course of their disease and 25–50% of
patients have clinical manifestations of nephropathy at the time of
diagnosis (1). In recent years, due
to early diagnosis and comprehensive treatment, the survival rate
of patients with LN has significantly improved, but in certain
patients, traditional immunosuppressive agents are still
ineffective. Indeed, ~30% of treated patients fail to improve and
certain patients develop refractory LN (RLN) after one year of
traditional treatment (2).
Patients with RLN have been indicated to display no
serum creatinine improvement after 2–3 months under the traditional
treatment regimen [cyclophosphamide (CTX) + glucocorticoids (GC)]
or no proteinuria or albumin improvement after 6 months (3,4).
According to the World Health Organization, LN may be classified
into 6 categories based on renal biopsy, ranging from type I to
type VI and the respective prognosis is in the order from good to
bad. In general, patients with class III, IV, V, III+V and IV+V LN
are prone to develop RLN. A cohort study in Egypt indicated that
patients with class II LN had a complete response to treatment and
~27.3% of patients with class III, IV and V LN did not respond to
treatment (5). Patients with LN who
do not respond to treatment tend to have more irreversible injuries
and the condition is more likely to deteriorate in such patients. A
cohort study from a Chinese population suggested that the treatment
was ineffective in ~26.5% of the population and they eventually
developed end-stage renal failure (6). Another study suggested that failure to
respond after treatment for one year was an independent predictor
of mortality in patients with LN (7).
If the traditional treatment regimen fails, such as
if there is no response after 6 months of treatment, the patient
has refractory LN (8). In this case,
a large number of novel pharmaceutical preparations, including
mycophenolate mofetil (MMF), tacrolimus (TAC) and rituximab (RTX),
have been developed in China and elsewhere, and these drugs were
reported to have a certain therapeutic effect in RLN. However,
there are no studies that evaluate the best treatment for RLN.
Therefore, the present meta-analysis study aimed to systematically
evaluate the effectiveness and safety of common therapeutic drugs
for the treatment of RLN and screen the optimal therapeutic drugs
or regimens to provide a basis for the clinical treatment of
RLN.
Materials and methods
Search strategy
The PubMed, Embase, Cochrane Library, China
Knowledge Network Infrastructure, VIP and Wanfang databases were
searched from inception to April 30, 2018. The search terms include
‘refractory’, ‘lupus nephritis’ and ‘treatment’. The search
strategy was adjusted according to the different databases. The
title and abstract of the citations were screened first, and then
the full text was screened. In addition, the references were
manually checked in published reviews to thoroughly search the
literature.
Inclusion and exclusion criteria
The following publication references were included
in the present study: i) Subjects, patients with refractory lupus
nephritis; ii) randomized controlled trials (RCTs); iii)
observation group or control group containing ≥1 of the following
drugs: Glucocorticoids, cyclophosphamide, mycophenolate mofetil,
tacrolimus, leflunomide, cyclosporine A and/or rituximab; and iv)
available data, effectiveness or adverse reactions. However,
studies on animal models, crossover studies, case reports and
studies without sufficient data were excluded.
Data extraction and quality
assessment
Then, two reviewers independently screened and
crosschecked the literature. In case of disagreement, the
discussion was resolved or submitted to a third researcher.
Duplicates were removed, and unrelated literature was excluded by
reading the title and abstract. Then, the citations were determined
by reading the full text. The collected data mainly included
indicators of effectiveness i.e. complete remission (CR) and
partial remission (PR); evaluation criteria for effectiveness, i.e.
24-h urine protein <0.3 g/l for CR, and 24-h urine protein
<1.0 g/l, serum albumin >30 g/l and serum creatinine <25%
for PR; the total number of cases with effective treatment was
determined as the number of cases with CR + number of cases with PR
(9). The safety indicators were
infection and other adverse reactions including gastrointestinal
reactions, leukopenia, liver damage and bone marrow suppression.
The Jadad scoring standard was used to quantitatively evaluate the
quality of the included studies. The score ranged from 0 to 5; a
total score of ≥4 indicated high quality (10).
Statistical analysis
Stata 14.0 software (Stata Corp.) was used in the
present Network Meta Analysis (NMA). The odds ratio and 95% CI were
determined to compare the efficacy and adverse reactions of the
nine treatment regimens for RLN. The degree of heterogeneity was
quantified using I2 calculations. Values of
I2<50% were considered to indicate no heterogeneity.
The analysis was performed using the fixed-effects model or
random-effects model as appropriate. Furthermore, a sensitivity
analysis was performed by omitting studies one by one to determine
the source of heterogeneity. The P-value of the Z test was used to
assess the direct and indirect comparison results in NMA (11). If P>0.05, the direct comparison
result is consistent with the indirect comparison result; otherwise
it is inconsistent. The efficacy and adverse reaction risks of each
treatment regimen were sequenced using the surface under the
cumulative ranking curve (SUCRA) and the optimal treatment protocol
was determined.
Results
Selection of studies for
inclusion
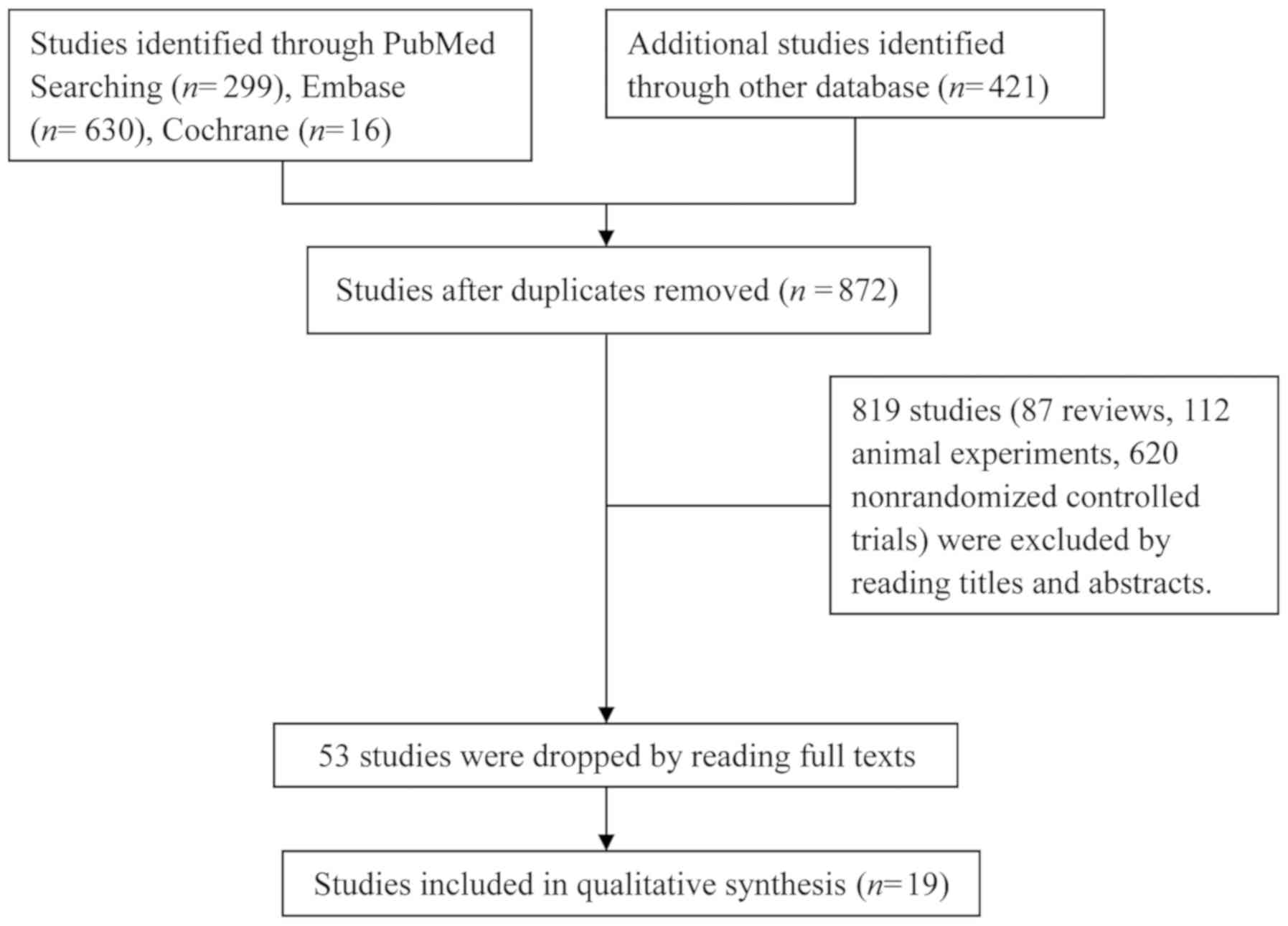
A total of 1,366 relevant articles were initially
retrieved, of which 494 duplicated articles and 819 studies (87
reviews, 112 animal experiments and 620 non-randomized controlled
trials) were excluded after reading their titles and abstracts. In
addition, 34 articles did not meet the inclusion criteria and were
also excluded. Finally, 19 articles comprising a total of 1,127
patients were included (Fig. 1).
Studies included in the
meta-analysis
Among the 19 articles, 17 were in Chinese (9,12–27) and
2 were in English (28,29). Except for one study that was a
three-arm study (26), the remaining
18 were two-arm studies. Only three studies (7,21,25) were
identified as high-quality studies (Jadad score=4). A total of
seven therapeutic drugs were used in nine different treatment
regimes. The basic characteristics of the studies included and the
treatment regimens are specified in Table I. Fig.
2 shows the sample size for each treatment regimen and the
number of studies compared between the two regimens, such as the
largest number of studies comparing CTX + GC and MMF + GC.
 | Table I.Basic characteristics of the studies
included. |
Table I.
Basic characteristics of the studies
included.
| First author
(year) | Sample size (n) | M/F | Treatment
regimen | Biopsy class | Duration
(months) | Jadad score | (Refs.) |
|---|
| Ma (2016) | 64 | 40/24 | GC, MMF (25
mg/day)+GC | Unclear | 3 | 3 | (9) |
| Li (2012) | 86 | 49/37 | GC, MMF (25
mg/day)+GC | Unclear | 3 | 3 | (10) |
| Wang (2015) | 156 | 20/136 | CTX (100
mg/m2)+GC, MMF (1.5 g/day)+GC | Unclear | 6 | 3 | (11) |
| Zheng (2015) | 31 | 18/13 | CTX+GC, MMF(0.1
g/day)+GC | Unclear | 3 | 2 | (12) |
| Dong (2014) | 78 | 9/69 | CTX (1,000
mg/m2)+GC, MMF (1.5 g/day)+GC | Unclear | 24 | 3 | (13) |
| Liu (2013) | 79 | 9/70 | CTX (100
mg/m2)+GC, MMF (1.5 g/day)+GC | III, IV,V | 24 | 3 | (14) |
| Liu (2009) | 39 | 7/32 | CTX (100
mg/m2)+GC, MMF (1.5 g/day)+GC | IV | 24 | 3 | (15) |
| Yang (2008) | 60 | 22/38 | CTX (200
mg/m2)+GC, MMF (0.75 mg/day)+GC | Unclear | 6 | 3 | (16) |
| Zhen (2006) | 40 | 26/14 | CTX (1,000
mg/m2)+GC, MMF (1.5 g/day)+GC | Unclear | 6 | 3 | (17) |
| Shi (2006) | 53 | 5/48 | CTX (400
mg/m2)+GC, MM F(1.5 g/day)+GC | IV | 6 | 3 | (18) |
| Li (2002) | 40 | 1/39 | CTX (400
mg/m2)+GC, MMF (1.5 g/day)+GC | Unclear | 3 | 3 | (19) |
| Mostafi (2010) | 31 | 4/27 | CsA (4
mg/kg/day)+GC, MMF (1.5 g/day)+GC | IV | 108 | 3 | (20) |
| Lu (2017) | 74 | 25/49 | CTX (1,000
mg/m2)+GC, TAC (2 mg/day)+GC | Unclear | 12 | 4 | (21) |
| Liu (2016) | 30 | 3/27 | LE F(30 mg/day)+GC,
TAC (2 mg/day)+GC | III, IV, V, III+V,
IV+V | 6 | 3 | (22) |
| Xiang (2017) | 60 | 7/53 | CTX (400
mg/m2)+GC, CTX (400 mg/m2)+ LEF (20
mg/day)+GC | IV | 6 | 4 | (7) |
| Liang (2014) | 50 | 13/37 | CTX (400
mg/m2)+GC, CTX (400 mg/m2)+ TAC (3.5
mg/day)+GC | Unclear | 6 | 3 | (23) |
| Yi (2014) | 27 | 5/22 | CTX (800
mg/m2)+GC, CTX(800 mg/m2)+ RTX (375
mg/m2)+GC | III+V, IV+V | 6 | 3 | (24) |
| Zhang (2015) | 84 | – | CTX (800
mg/m2)+GC, CTX (800 mg/m2)+ RTX (375
mg/m2)+GC | III+V, IV+V | 12 | 4 | (25) |
| Mo (2009) | 45 | 4/41 | CTX (400
mg/m2)+GC MMF (1.5 g/day)+GC CTX (400
mg/m2)+TAC (3.5 mg/day)+GC | IV, V, III+V,
IV+V | 6 | 2 | (26) |
Analysis of inconsistency
In the evidence network diagram, CTX+GC, MMF+GC and
CTX+TAC+GC formed a closed loop; thus, the direct evidence and
indirect evidence of the three treatment regimens were consistently
tested. The Z test result was indicated no inconsistency
(P=0.931, P>0.05).
Detection of publication bias
A funnel plot was used to evaluate publication bias.
The funnel plot was symmetrical in this analysis, and it can be
considered that there was no publication bias in the direct
comparison meta-analysis (Fig.
3).
 | Figure 3.Funnel plot for assessment of
publication bias or small sample effect. A, GC; B, CTX+GC; C,
MMF+GC; D, LEF+GC; E, FK506+GC; F, CsA+GC; G, CTX+RTX+GC; H,
CTX+LEF+GC; I, CTX+FK506+GC. GC, glucocorticoid; CTX,
cyclophosphamide; MMF, mycophenolate; TAC, tacrolimus; LEF,
leflunomide; RTX, rituximab; CsA, cyclosporine A. |
NMA results
Comparison of treatment effect
The present results suggested that MMF+GC produced
significantly higher overall responses (CR+PR), and MMF+GC
(OR=2.58; 95% CI, 1.67–3.97), TAC+GC (OR=3.14; 95% CI, 1.05–9.43),
CTX+LEF+GC (OR=3.05; 95% CI, 1.05–8.84), CTX+RTX+GC (OR=3.89; 95%
CI, 1.60–9.45) and CTX+TAC+GC (OR=6.22; 95% CI, 1.93–20.05) had
significantly higher overall responses than CTX+GC. In addition,
the present results suggested that MMF+GC produced significantly
higher overall responses, and MMF+GC (OR=4.13; 95% CI, 1.72–9.96),
TAC+GC (OR=5.04; 95% CI, 1.16–21.97), CTX+LEF+GC (OR=4.89; 95% CI,
1.15–20.78), CTX+RTX+GC (OR=6.24; 95% CI, 1.66–23.39) and
CTX+TAC+GC (OR=9.98; 95% CI, 2.23–44.56) had significantly higher
overall responses than GC. There were no statistically significant
differences in the effectiveness of any of the other regimens in
the treatment of RLN (Fig. 4).
Comparison of safety
Comparison of infection suggested that the
difference between MMF+GC and CTX+GC was statistically significant.
Comparison of gastrointestinal reactions and leukopenia indicated
no statistically significant differences between any of the groups
(Figs. 5 and 6).
Results sorting
In terms of efficiency, the maximum SUCRA value of
CTX+TAC+GC was 80.6%, indicating that TAC+CTX+GC was likely to be
the best currently used treatment. The maximum SUCRA values of
CTX+GC were 67.8%, 80.1% and 65.4% for infection, gastrointestinal
reaction and leukopenia, indicating that CTX+GC had the highest
risk of adverse reaction (Table
II).
 | Table II.SUCRA values (%) for treatment
efficacy and safety of each regimen. |
Table II.
SUCRA values (%) for treatment
efficacy and safety of each regimen.
| Treatment
regimen | Efficacy | Infection | Gastrointestinal
reaction | Leukocyte
decline |
|---|
| TAC+CTX+GC | 80.6 | 15.8 | 24.1 | N.A. |
| LEF+GC | 68.9 | N.A. | 23.3 | N.A. |
| CsA+GC | 65.9 | N.A. | N.A. | N.A. |
| RTX+CTX+GC | 64.3 | 55.0 | 59.5 | N.A. |
| TAC+GC | 54.8 | N.A. | 36.3 | 42.4 |
| LEF+CTX+GC | 54.1 | 69.1 | 79.1 | 59.0 |
| MMF+GC | 45.1 | 42.3 | 47.6 | 20.2 |
| CTX+GC | 12.7 | 67.8 | 80.1 | 65.4 |
| GC | 3.6 | N.A. | N.A. | 63.0 |
Discussion
At present, the cause of RLN remains elusive, but
studies have indicated that non-compliance with treatment and lack
of efficacy of the induction therapy regimens for LN may promote
the development of RLN (7). However,
there is no uniform guideline for the treatment of RLN patients;
therapeutic drugs and treatment regimens depend largely on the
patients' condition and the clinician's experience. Therefore, the
present study compared the effectiveness and safety of common
therapeutic drugs for the treatment of RLN to provide a reference
for the clinical prescription of drugs.
The traditional induction therapy used for LN is a
combination of GC and intravenous CTX. The basic drug used in the
induction phase is CTX at a sufficient dose, with a subsequent
gradual dose reduction according to the patient's condition. In
order to avoid the toxic effects of CTX, it recently was replaced
with MMF (30,31). Studies have indicated that, although
the effectiveness of MMF in the treatment of LN is not different
from that of CTX, it reduces the risk of ovarian failure associated
with CTX (32). However, the present
study indicated that MMF was more effective and was associated with
less gastrointestinal adverse reactions than CTX in the treatment
of RLN. In addition, MMF had a greater likelihood of reducing the
risk of adverse effects, including infection and leukopenia, when
compared with CTX.
The present study also indicated that TAC combined
with CTX in the treatment of RLN was superior to the traditional
regimen, but did not perform differently from MMF. This is
consistent with previous results from an NMA of three drugs for LN
(33). However, these three
treatment regimens exhibited no difference in adverse reactions,
including infection, leukopenia and gastrointestinal reactions. The
mechanisms of action of MMF and tacrolimus are different; MMF
reduces B-cell and T-cell proliferation, leads to antibody
production, and recruitment of lymphocytes and monocytes, while
tacrolimus reduces cytokine production and T-cell activation, and
stabilizes the actin cytoskeleton of podocytes (34). Although the two drugs produce similar
effects, tacrolimus is more expensive. RLN patients require
long-term medication, and thus, the patients' financial situation
should also be considered when selecting an effective
treatment.
In a prospective cohort study (35), a multi-target regimen (MMF+TAC+GC)
was first proposed for the treatment of LN, and the incidence of
complete remission were significantly higher than those with
intravenous CTX, with fewer adverse events. The multi-target
treatment also exhibited certain advantages in the treatment of RLN
with not only a better treatment effect but also reduced hormone
dosage and less resistance compared to traditional treatment
regimen (36,37). The present study compared three
multi-target treatment regimens, namely the traditional regimen
combined with RTX, the traditional regimen combined with LEF and
the traditional regimen combined with TAC. The results suggest that
the three multi-target treatment regimens are superior to the
traditional treatment regimen and the ranking results suggested
that the traditional regimen combined with TAC was the best of the
nine regimens. It was also likely to have the lowest risk of
infection in the treatment of RLN. Compared to traditional
treatment regimen, multi-target therapy was not associated with any
corresponding increase in adverse reactions. Furthermore, it not
only produces an improved therapeutic effect but may also reduce
the economic burden on patients to a certain extent (38). Thus, the clinical use of multi-target
therapy should be promoted. However, with regard to the adverse
reactions, including gastrointestinal reactions, infections and
leukopenia, the multi-target therapy did not exhibit any difference
from other regimens. However, this may be due to the small number
of studies included.
In conclusion, the present study compared the
effectiveness and safety of common therapeutic drugs and medication
regimens in the treatment of RLN. The results indicated the
superiority of the regimen of TAC+CTX+GC regarding its clinical
efficacy in patients with RLN. Furthermore, the traditional
treatment regimen (CTX+GC) had the highest probability of causing
adverse effects among the nine interventions compared. However, the
present study had certain limitations. First of all, for most of
the regimens, the data for direct comparison were limited,
resulting in insufficient evidence for indirect comparisons.
Furthermore, previous studies have suggested that positive personal
factors, including low-calorie diets and physical exercise,
contribute to improved renal function (39,40), but
these factors were not considered in the present study and may have
a potential impact on the results. Finally, in terms of adverse
reactions, only infections, gastrointestinal reactions and
leukopenia were analyzed, while other adverse reactions, including
leukopenia, myelosuppression, alopecia, liver damage and menstrual
disorders, were not analyzed due to incomplete data. Therefore,
subsequent studies on RLN should focus on its adverse reactions
when studying the curative effects.
Acknowledgements
The authors would like to thank Professor Dongqing
Ye (Department of Epidemiology and Biostatistics, Anhui Medical
University) for his encouragement and support.
Funding
This study was supported by the Natural Science
Foundation of Anhui Province, China (grant nos. 1608085MH219 and
1808085QH251).
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
HY and HP conceived the study. MJT, LX and LRJ
selected the studies. ZL and JS extracted the data. JZ analyzed the
data and wrote the manuscript. All of the above authors contributed
to the discussion of the results and revision of the
manuscript.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
Glossary
Abbreviations
Abbreviations:
|
SLE
|
systemic lupus erythematosus
|
|
RLN
|
refractory lupus nephritis
|
|
NMA
|
network meta-analysis
|
|
GC
|
glucocorticoids
|
|
CTX
|
cyclophosphamide
|
|
MMF
|
mycophenolate mofetil
|
|
TAC
|
tacrolimus
|
|
LEF
|
leflunomide
|
|
CsA
|
cyclosporine A
|
|
RTX
|
rituximab
|
|
SUCRA
|
surface under the cumulative ranking
curve
|
|
CR
|
complete remission
|
|
PR
|
partial remission
|
References
|
1
|
Maroz N and Segal MS: Lupus nephritis and
end-stage kidney disease. Am J Med Sci. 346:319–323. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Contis A, Vanquaethem H, Truchetet ME,
Couzi L, Rigothier C, Richez C, Lazaro E and Duffau P: Analysis of
the effectiveness and safety of rituximab in patients with
refractory lupus nephritis: A chart review. Clin Rheumatol.
35:517–522. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Moroni G and Ponticelli C: The
multifaceted aspects of refractory lupus nephritis. Expert Rev Clin
Immunol. 11:281–288. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Kronbichler A, Brezina B, Gauckler P,
Quintana LF and Jayne DRW: Refractory lupus nephritis: When, why
and how to treat. Autoimmun Rev. 18:510–518. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Momtaz M, Fayed A, Wadie M, Gamal SM,
Ghoniem SA, Sobhy N, Kamal Elden NM and Hamza WM: Retrospective
analysis of nephritis response and renal outcome in a cohort of 928
Egyptian lupus nephritis patients: A university hospital
experience. Lupus. 26:1564–1570. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Tang Y, Qin W, Peng W and Tao Y:
Development and validation of a prediction score system in lupus
nephritis. Medicine (Baltimore). 96:e80242017. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
The CL, Phui VE, Ling GR, Ngu LS, Wan SA
and Tan CH: Causes and predictors of mortality in biopsy-proven
lupus nephritis: The Sarawak experience. Clin Kidney J. 11:56–61.
2018. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Pons-Estel GJ, Serrano R, Plasín MA,
Espinosa G and Cervera R: Epidemiology and management of refractory
lupus nephritis. Autoimmun Rev. 10:655–663. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Xiang H: Clinical efficacy of leflunomide
and cyclophosphamide in the treatment of patients with severe
refractory lupus nephritis. Hebei Med J. 39:919–920. 2017.(In
Chinese).
|
|
10
|
Jadad AR, Moore RA, Carroll D, Jenkinson
C, Reynolds DJ, Gavaghan DJ and McQuay HJ: Assessing the quality of
reports of randomized clinical trials: Is blinding necessary?
Control Clin Trials. 17:1–12. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Zhang C, Yan JZ, Sun F, Liu Q, Guo Y and
Zeng XT: Differentiation and handling of homogeneity in network
meta-analysis. Chin J Evidence Based Med. 14:884–888. 2014.
|
|
12
|
Ma Y, Song Y, Tong SS, Wang X, Wang GZ and
Dai H: Analysis of the therapeutic effect of mycophenolate mofetil
on refractory lupus nephritis. World Latest Med Information.
16:832016.(In Chinese).
|
|
13
|
Li L: Analysis of the efficacy of
mycophenolate mofetil in the treatment of refractory lupus
nephritis and its effect on clinical symptoms. China Med Herald.
9:75–76. 2012.(In Chinese).
|
|
14
|
Wang Z, Zheng DW and Liu GH: The curative
effect and safety of refractory lupus nephristis treated by
mycophenolate mofetil combined with prednisone. J North Pharm.
12:127–128. 2015.(In Chinese).
|
|
15
|
Zheng S, Zheng JG, Han L and Wang DH: 31
cases of clinical curative effect analysis of mycophenolate mofetil
treat refractory lupus nephritis. World Latest Med Information.
15:20–67. 2015.(In Chinese).
|
|
16
|
Dong YM, Zhou LZ, Li J, Li QH and Liu Z:
Therapeutic effect of mycophenolate mofetil combined with
prednisone in the treatment of refractory lupus nephritis. Chin J
Clin Rational Drug Use. 7:44–45. 2014.(In Chinese).
|
|
17
|
Liu CY, Jiang Y and Wang L: Comparison of
curative effect of mycophenolate mofetil and cyclophosphamide for
the treatment of refractory lupus nephritis. China Modern Doctor.
51:48–50. 2013.(In Chinese).
|
|
18
|
Liu CY: Application of mycophenolate
mofetil and cyclophosphamide in refractory lupus nephritis. Strait
Pharmaceutical J. 21:137–138. 2009.(In Chinese).
|
|
19
|
Yang FF, Lin B, Wang J and You YW:
Efficacy evaluation of combined immunosuppressive agents in the
treatment of refractory lupus nephritis. Chin Youjiang Med J.
36:134–135. 2008.(In Chinese).
|
|
20
|
Zhen HM, Zhang HY, Huo G, Zhao SJ and Li
JS: Clinical observation of steroid combined with mycophenolate
mofetil in the treatment of refractory lupus nephritis. Inner
Mongolia Med J. 38:1023–1025. 2006.(In Chinese).
|
|
21
|
Shi J, Chen BP and He XZ: Clinical
efficacy of mycophenolate mofetil in the treatment of 26 cases of
refractory type IV lupus nephritis. Negative. 27:19202006.(In
Chinese).
|
|
22
|
Li L, Li WQ and Qi WC: Clinical
observation of mycophenolate mofetil in the treatment of refractory
lupus nephritis. Chin J Postgraduates Med. 25:42–43. 2002.(In
Chinese).
|
|
23
|
Lu Y: One-year follow-up observation of
tacrolimus in the treatment of refractory lupus nephritis. J Med
Forum. 38:167–169. 2017.(In Chinese).
|
|
24
|
Liu H, Huang DQ and Liang Y: Comparative
study of tacrolimus and leflunomide in the treatment of refractory
lupus nephritis. J Qiqihar Med University. 37:3419–3420. 2016.(In
Chinese).
|
|
25
|
Liang B, Zhang JH, Wang CA and Han JL:
Comparison of traditional treatment and multi-target treatment for
refractory lupus nephritis. Chin J Control Endemic Diseases.
29:34–35. 2014.(In Chinese).
|
|
26
|
YI L, Luo FZ, Deng CP and Wu CY:
Application of rituximab monoclonal antibody in the treatment of
refractory lupus nephritis. J Nanjing Med University (Natural
Sciences). 34:1102–1104. 2014.(In Chinese).
|
|
27
|
Mostafi M, Rabbani MG, Hossain MR,
Siddiqui AR and Rabbani SB: Cyclosporine & mycophenolate
mofetil in the treatment of cyclophosphamide refractory Class-IV
lupus nephritis. JAFMC Bangladesh. 5:8–13. 2009.
|
|
28
|
Zhang J, Zhao Z and Hu X: Effect of
rituximab on serum levels of anti-C1q and antineutrophil
cytoplasmic autoantibodies in refractory severe lupus nephritis.
Cell Biochem Biophys. 72:197–201. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Mo YM and Li Long: Comparison of multiple
target regimens and traditional classic regimens in the treatment
of refractory lupus nephritis. Clin Misdiagnosis Mistherapy.
22:53–54. 2009.(In Chinese).
|
|
30
|
Kasitanon N, Boripatkosol P and Louthrenoo
W: Response to combination of mycophenolate mofetil, cyclosporin A
and corticosteroid treatment in lupus nephritis patients with
persistent proteinuria. Int J Rheum Dis. 21:200–207. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Sedhain A, Hada R, Agrawal RK, Bhattarai
GR and Baral A: Low dose mycophenolate mofetil versus
cyclophosphamide in the induction therapy of lupus nephritis in
Nepalese population: A randomized control trial. BMC Nephrol.
19:1752018. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Joo YB, Kang YM, Kim HA, Suh CH, Kim TJ,
Park YW, Lee J, Lee JH, Yoo DH, Bae SC, et al: Outcome and
predictors of renal survival in patients with lupus nephritis:
Comparison between cyclophosphamide and mycophenolate mofetil. Int
J Rheum Dis. 21:1031–1039. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Hannah J, Casian A and D'Cruz D:
Tacrolimus use in lupus nephritis: A systematic review and
meta-analysis. Autoimmun Rev. 15:93–101. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Mok CC: Calcineurin inhibitors in systemic
lupus erythematosus. Best Pract Res Clin Rheumatol. 31:429–438.
2017. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Bao H, Liu ZH, Xie HL, Hu WX, Zhang HT and
Li LS: Successful treatment of class V+IV lupus nephritis with
multitarget therapy. J Am Soc Nephrol. 19:2001–2010. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Jesus D, Rodrigues M, da Silva JAP and
Inês L: Multitarget therapy of mycophenolate mofetil and
cyclosporine A for induction treatment of refractory lupus
nephritis. Lupus. 27:1358–1362. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Choi CB, Won S and Bae SC: Outcomes of
multitarget therapy using mycophenolate mofetil and tacrolimus for
refractory or relapsing lupus nephritis. Lupus. 27:1007–1011. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Xiao CJ, Rao H, Xu XY and Zeng QH:
Clinical analysis of 23 cases of V+IV lupus nephritis treated with
multiple targets. Chin J Clin (Electronic Edition). 7:6733–6734.
2013.
|
|
39
|
Morales E, Valero MA, León M, Hernández E
and Praga M: Beneficial effects of weight loss in overweight
patients with chronic proteinuric nephropaties. Am J Kidney Dis.
41:319–327. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Szulińska M, Skrypnik D, Ratajczak M,
Karolkiewicz J, Madry E, Musialik K, Walkowiak J, Jakubowski H and
Bogdański P: Effects of endurance and endurance-strength exercise
on renal function in abdominally obese women with renal
hyperfiltration: A prospective randomized trial. Biomed Environ
Sci. 29:706–771. 2016.PubMed/NCBI
|