Introduction
Lesions of the long head of the biceps tendon (LHBT)
are among the most common causes of shoulder disorders and pain
(1,2). LHBT lesions alone are relatively rare;
they are mostly associated with other lesions of the shoulder
joint, particularly rotator cuff (RC) injury (1,3–8). The normal physiological function of the
LHBT depends on the role of the block system, which is mainly
composed of supraspinatus (SSP), coracohumeral ligament, superior
glenohumeral ligament and subscapularis (SSC) (9). These ligaments are reinforced by the
check-points of the SSP and SSC tendons, which maintain LHBT
stability in the intertubercular sulcus (Fig. 1). SSP and SSC injuries are more
common among RC injuries (10–12),
since the tendons in them are used as reinforcement of the block
system. SSP and SSC damage leads to instability of the LHBT, easily
causing LHBT lesions following RC injury. Studies have indicated
that the proportion of LHBT lesions combined with RC injury
accounts for 30–69% (6,13); this was not well known in the past,
when only RC injury was treated and the pain caused by LHBT lesions
was frequently ignored (14). In
recent years, increasing attention has been paid to persistent pain
caused by LHBT lesions (15–19). With the development of imaging and
arthroscopic technology, it has been recognized that LHBT lesions
are caused by repeated friction with the intertubercular sulcus and
the surgical method of choice has changed from large-incision to
small-incision or minimally invasive treatment under
arthroscopy.
In recent years, a large number of comparative
studies on the clinical efficacy of LHBT tenotomy and LHBT
tenodesis have been performed (20–31), but
the results remain controversial. It has been reported that LHBT
tenotomy and LHBT tenodesis achieve satisfactory efficacy. As
compared with LHBT tenodesis, pure LHBT tenotomy has the advantages
of simplicity, short surgery time and rapid post-operative recovery
(21,32,33), but
it may cause complications including Popeye sign deformity
(21,24,25,28),
upper arm spastic pain, loss of stability of the humeral head
(34–36) and reduced forearm supination strength
(20,22,23).
LHBT tenodesis is a more invasive surgical procedure, but it
maintains the length and tension of the original tendon and the
strength of the elbow muscle, effectively prevents muscle atrophy
and minimizes spastic and Popeye sign deformity in the upper arm
(37,38).
Although the clinical manifestations and advantages
of LHBT tenodesis in biomechanics have been confirmed, the choice
between proximal and distal tenodesis remains controversial. Recent
studies have reported frequent residual pain in the intertubercular
sulcus following arthroscopic proximal LHBT tenodesis (39,40). In
addition, LHBT lesions are frequently combined with other injuries
and there are few comparative studies on the clinical treatment of
LHBT lesions accompanied by RC repair (RCR). In the present study,
the efficacy between small-incision open distal subpectoral
tenodesis and arthroscopic proximal tenodesis was analyzed in
patients with LHBT lesions accompanied by RCR, with the aim of
providing evidence and support for their use in the clinic.
Materials and methods
Patients and ethics
All clinical procedures were approved by the Ethical
Committee of the Affiliated Traditional Chinese Medicine Hospital
of Southwest Medical University (Luzhou, China; approval no.
KY20180603), performed in accordance with the 1964 Declaration of
Helsinki and its later amendments and the study was registered as a
clinical trial in the Chinese Trial Registry (no.
ChiCTR1800015643). All patients understood the intervention
procedure and signed the relevant informed consent form. From June
2014 to June 2016, 71 patients with LHBT lesions with RCR who
underwent shoulder arthroscopy met the inclusion criteria for the
study. All RC injuries were repaired by arthroscopy and tenodesis
was performed after LHBT lesions were cut off under arthroscopy
(Fig. 2). Of the 71 patients, 35
were treated with small-incision open distal subpectoral biceps
tenodesis (subpectoral group; 17 males and 18 females aged 46–69
years). Arthroscopic proximal biceps tenodesis was performed in 36
patients (arthroscopic group; 16 males and 20 females aged 42–71
years). All patients were further diagnosed with LHBT lesions
combined with RCR by pre-operative medical history, clinical
examination, MRI examination and intra-operative microscopy. No
statistically significant differences were observed in terms of
sex, diabetes, age, smoking, time of onset, type of LHBT lesions
(41) or size of RC tear between the
two groups (P>0.05; Table I).
 | Table I.Comparison of demographic
characteristics of patients in the subpectoral tenodesis group and
the arthroscopic tenodesis group. |
Table I.
Comparison of demographic
characteristics of patients in the subpectoral tenodesis group and
the arthroscopic tenodesis group.
| Characteristic | Subpectoral group
(n=35) | Arthroscopic group
(n=36) | P-value |
|---|
| Age (years) | 53.46±8.45 | 54.32±10.73 | 0.709 |
| Sex |
|
| 0.727 |
|
Male | 17 | 16 |
|
|
Female | 18 | 20 |
|
| Dominant
shoulder | 29 (82.9) | 31 (86.1) | 0.705 |
| BMI
(kg/m2) | 24.65±3.78 | 23.79±4.36 | 0.378 |
| Pain duration
(days) | 129.76±18.36 | 137.53±17.78 | 0.119 |
| Rotator cuff tear
size |
|
| 0.832 |
|
Small | 18 | 20 |
|
|
Medium | 13 | 11 |
|
|
Large | 4 | 5 |
|
| Type of LHBT
lesion |
|
| 0.755 |
|
Tendinitis | 24 | 27 |
|
|
Subluxation | 2 | 1 |
|
| Total
dislocation | – | – |
|
| Partial
tear | 9 | 8 |
|
|
Complete rupture | – | – |
|
| Diabetes
mellitus | 5 (14.3) | 3 (8.3) | 0.676 |
| Smoking | 10 (28.6) | 12 (33.3) | 0.664 |
Pre-operative physical examination of the patients
clearly indicated that the diseased shoulder was accompanied by
limited movement, RC injury and positive signs of LHBT lesions, as
determined by tests including the pain arc test (+), Hawkins sign
(+), Yergason test (+) and Speed test (+). Imaging examination
confirmed that the patients had typical RC injury and LHBT
lesions.
Inclusion criteria
The inclusion criteria were as follows: i) Shoulder
pain accompanied by limited movement, particularly in terms of
functions such as outspreading and anteflexion; ii) shoulder MRI
revealed RC injury and abnormal LHBT signal; iii) further
arthroscopic confirmation of patients with LHBT lesions accompanied
by RC; iv) patients fully understood the surgical method and signed
the relevant doctor-patient communication and informed consent
forms; v) follow-up time was >1 year.
Exclusion criteria
The exclusion criteria were as follows: i) No RC
injury or irreparable RC injury; ii) open injury or other serious
shoulder joint disease; iii) revision surgery; iv) patients
unsuitable for surgery due to chronic wasting disease or infectious
diseases; v) patients refused to sign relevant doctor-patient
communication or informed consent form; vi) the follow-up time was
<1 year.
Surgical procedure
The patient was maintained in a recumbent position
on the healthy side, with a fixed head and neck and suspended upper
limb of the affected side using SPIDER MAN (MAQUET GmbH; able to
rotate multi-directionally, effect of free fixation), instead of
human traction fixation. The limb was outspread 40° and anteflexed
15°, the arthroscopic equipment was connected, the skin was
disinfected using iodine and alcohol and the sterile towels and
waterproof sheet spread were applied (Fig. 3). A 30° arthroscopy lens was placed
in the acromion posterolateral edge, and a planning and a radio
frequency instrument was placed in the acromion-anterolateral
border. First, the glenohumeral joint was explored and other
lesions were detected. The synovial tissue around the tendon in the
articular cavity was cleaned by the electric knife using the
anterior approach and the hyperplasia osteophytes were properly
removed using a drill. A radio frequency ion knife was used to
repair the tear edge of the RC in different ways, depending on the
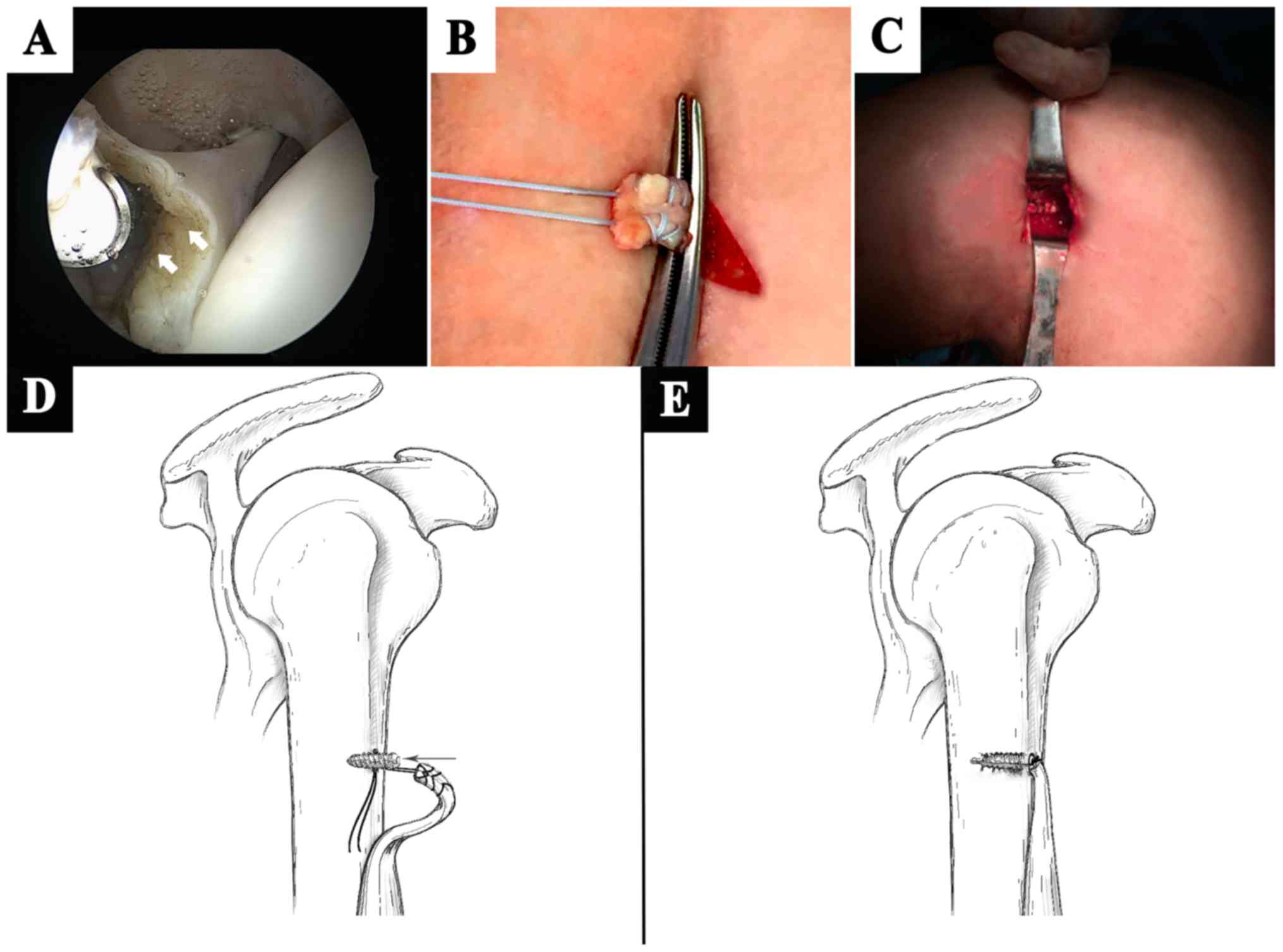
type of RC injury. Following the surgery, the LHBT lesions were cut
off under arthroscopy, after checking that the fixation was firm
(Fig. 4A).
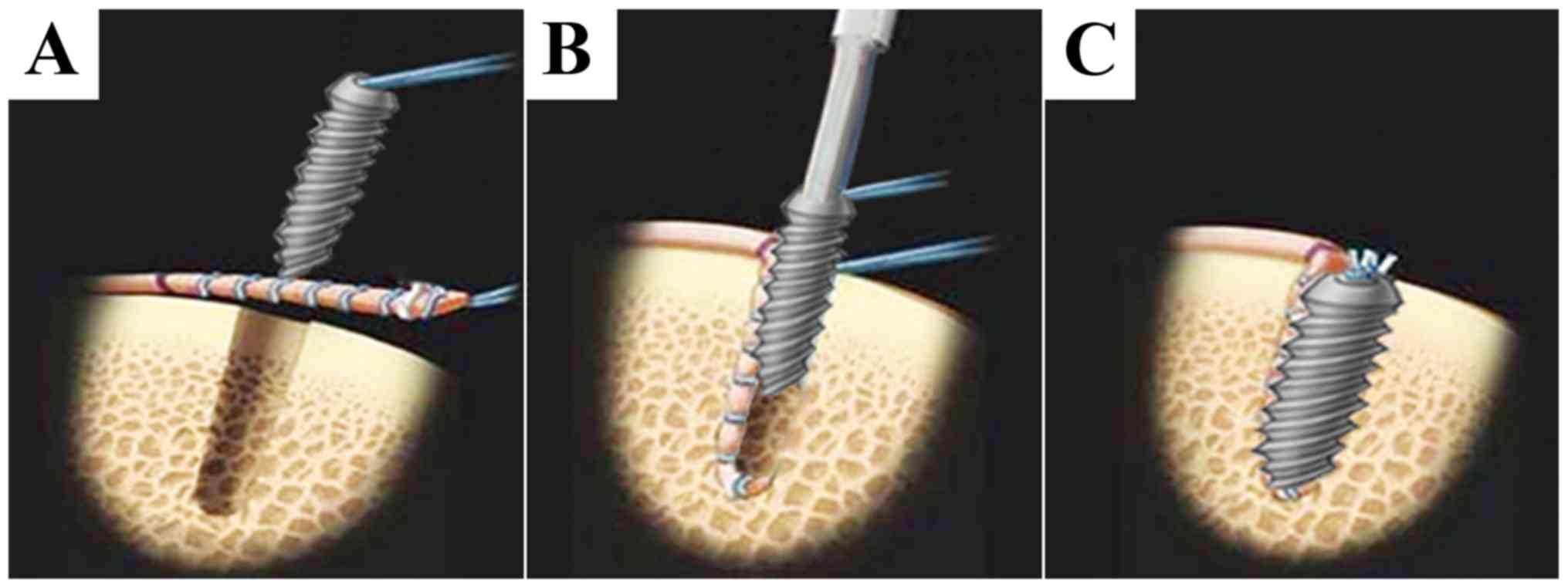
In the subpectoral group, an incision was made ~3 cm
along the inferior margin of the medial ectopectoralis. The skin
was incised, the superficial fascia was separated until reaching
the LHBT, the LHBT was removed under the ectopectoralis, the bony
cortex of the ectopectoralis was slightly polished with a grinding
drill, a bone drill was used to drill to a proper depth and
fixation was performed using a tendon suture (Johnson & Johnson
Medical Equipment Co., Ltd.) and interference screw
(MILAGRO®; Johnson & Johnson; Fig. 4B and C). A schematic illustration of
small-incision open distal subpectoral tenodesis is provided in
Fig. 4D and E. Following
re-examination of the supraspinatus, deltoid, LHBT, infraspinatus
and teres minor muscles, it was confirmed that there was no obvious
active bleeding and a plasma drainage tube was inserted. The
incision was stitched layer by layer and compressed using sterile
dressing, and the affected limb was bandaged. Following the
surgery, the affected limb was suspended or fixed with external
braces immediately.
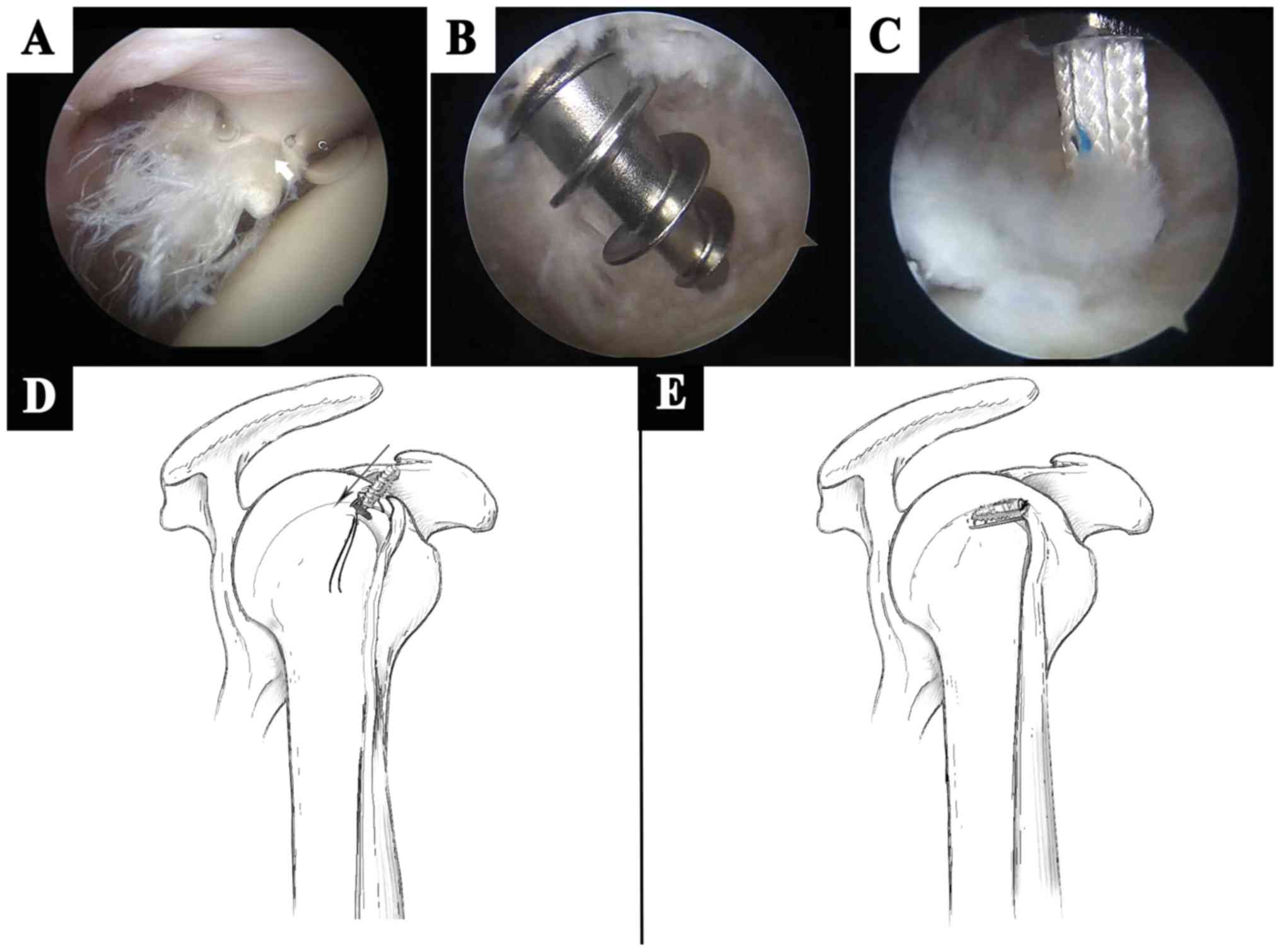
In the arthroscopic tenodesis group, following the
confirmation of intra-articular LHBT injury (Fig. 5A), the arthroscope was repositioned
to the subacromial space and the tendon sheath of the LHBT was
cleared with an electric knife to fully expose the LHBT. The inner
part of the sheath was explored. The bony cortex was slightly
polished with a polishing head on the intertubercular sulcus, fixed
with sutures anchors after stabilizing the proximal LHBT (ThRevo,
CF6160H; 5.0 mm, outside diameter × 18.0 mm length, w/Three#2 Hi-Fi
Suture; Smith & Nephew plc) (Fig. 5B
and C). A schematic illustration of arthroscopic proximal
tenodesis is provided in Fig. 5D and
E. No obvious active bleeding was observed and a plasma
drainage tube was inserted. The incision was stitched layer by
layer, compressed using sterile dressing and the affected limb was
bandaged. Following the surgery, the affected limb was suspended or
fixed with external braces immediately.
Post-operative treatment
The affected shoulder was fixed with external braces
immediately after surgery. Routine anti-infection, detumescence,
pain relief and intermittent ice compresses were administered and
the plasma drainage tube was removed 24 h post-operatively. At 2
weeks post-operatively, active or passive fist clenching and
bending of the elbow, as well as assisted forward bending, back
stretching and abduction (Abd) of the affected shoulder flexion
were performed. At 3 weeks post-operatively, active forward
bending, back stretching and Abd of the affected shoulder were
gradually performed. At 6 weeks post-operatively, full-range
exercises of the affected shoulder were initiated. Muscle strength
training began 3 months later and the patient gradually returned to
their original activity level at ~6 months post-operatively.
Clinical evaluation indicators
The surgery time and intra-operative bleeding volume
were recorded. Furthermore, muscle strength, Shoulder joint
function, pain and range of motion (ROM) of the shoulder joint were
recorded in detail pre-operatively and post-operatively at 2 weeks,
3 months and a final follow-up (the mean follow-up duration was 21
months). Patient satisfaction (16)
at ~one year post-surgery was also evaluated. The shoulder joint
function was assessed using the University of California at Los
Angeles (UCLA), Constant and American Shoulder and Elbow Surgeons
(ASES) scores. The visual analog scale (VAS) score (15,16) was
used to evaluate post-operative pain. At the time of the last
follow-up, complications were evaluated using ultrasound and biceps
apex distance (BAD).
Statistical analysis
Pearson's χ2 test was used to analyze the
categorical outcomes. One-way analysis of variance and the paired
t-test were used to compare potential differences in the surgery
time, intra-operative blood loss and ROM, as well as the UCLA,
Constant, ASES and VAS scores between the two groups. Values are
expressed as the mean ± standard deviation. All data were processed
using SPSS statistical software (version 20; IBM Corp.). P<0.05
was considered to indicate a statistically significant
difference.
Results
Post-operative conditions
All 71 patients successfully completed the surgery
without any serious complications, e.g. vascular or nerve injury.
The intra-operative data of the two groups are provided in Table II. The surgery time in the
subpectoral group was significantly shorter than that in the
arthroscopic group (P<0.05). Intra-operative blood loss in the
subpectoral group was significantly less than that in the
arthroscopic group (P<0.05). The plasma drainage tube was
removed 24 h post-operatively and all incisions achieved grade A
healing. The patients were discharged smoothly and no
post-operative infection occurred.
 | Table II.Peri-operative data and comparison
between two groups of patients. |
Table II.
Peri-operative data and comparison
between two groups of patients.
| Item | Subpectoral group
(n=35) | Arthroscopic group
(n=36) | P-value |
|---|
| Operative time
(min) | 105.90±15.75 | 124.38±18.84 | <0.001 |
| Intra-operative
blood loss (ml) | 40.28±4.92 | 64.46±8.77 | <0.001 |
Clinical outcomes
The patients were followed up for a minimum of 1.5
years. The mean follow-up duration in the subpectoral group was
21.03±2.42 months and that in the arthroscopic group was 21.45±1.24
months. The follow-up data of the two groups are provided in
Table III. With the prolongation
of the follow-up time, the UCLA, Constant and ASES scores increased
significantly in each group, while the VAS score decreased
significantly; significant differences were observed within the
same group at different time-points (P<0.05). No significant
difference was observed in the UCLA, Constant, ASES and VAS scores
at the pre-operative stage between the two groups (P>0.05).
Furthermore, no significant difference was observed in the Constant
and UCLA scores at 2 weeks post-operatively between the two groups
(P>0.05); however, the ASES score of the subpectoral group at
this time-point was significantly higher than that of the
arthroscopic group and the VAS score of the subpectoral group was
significantly lower than that of the arthroscopic group
(P<0.05). At 3 months post-operatively, there was no significant
difference in the UCLA, Constant and ASES scores between the two
groups (P>0.05); however, the VAS score of the subpectoral group
at this time-point was still significantly better than that of the
arthroscopic group (P<0.05). No significant difference was
observed in the UCLA, Constant, VAS and ASES scores between the two
groups at the time-point of final follow-up (P>0.05).
 | Table III.Comparison of clinical results
between the two groups. |
Table III.
Comparison of clinical results
between the two groups.
| Characteristic | Subpectoral group
(n=35) | Arthroscopic group
(n=36) | P-value |
|---|
| UCLA score |
| BL | 18.45±3.22 | 18.62±2.76 | 0.812 |
|
Post-operative week 2 |
|
Score | 25.78±2.44 | 24.38±4.03 | 0.082 |
|
P-value | <0.001 | <0.001 |
|
|
Post-operative month 3 |
|
Score | 29.46±3.71 | 29.07±3.15 | 0.634 |
|
P-value | <0.001 | <0.001 |
|
| Last
follow-up |
|
Score | 33.54±1.07 | 33.41±1.24 | 0.638 |
|
P-value | <0.001 | <0.001 |
|
|
Constant score |
| BL | 51.58±9.72 | 49.12±7.53 | 0.237 |
|
Post-operative week 2 |
|
Score | 59.47±7.38 | 58.66±8.49 | 0.670 |
|
P-value | <0.001 | <0.001 |
|
|
Post-operative month 3 |
|
Score | 72.32±10.71 | 74.71±8.04 | 0.290 |
|
P-value | <0.001 | <0.001 |
|
| Last
follow-up |
|
Score | 88.49±4.55 | 89.14±5.37 | 0.584 |
|
P-value | <0.001 | <0.001 |
|
| ASES score |
| BL | 42.81±4.68 | 41.74±5.27 | 0.369 |
|
Post-operative week 2 |
|
Score | 58.42±4.33 | 53.02±6.82 | <0.001 |
|
P-value | <0.001 | <0.001 |
|
|
Post-operative month 3 |
|
Score | 69.83±6.84 | 68.43±6.49 | 0.379 |
|
P-value | <0.001 | <0.001 |
|
| Last
follow-up |
|
Score | 86.13±7.58 | 87.69±5.27 | 0.316 |
|
P-value | <0.001 | <0.001 |
|
| VAS score |
| BL | 7.62±0.72 | 7.54±0.95 | 0.691 |
|
Post-operative week 2 |
|
Score | 4.37±1.47 | 5.92±1.99 | <0.001 |
|
P-value | <0.001 | <0.001 |
|
|
Post-operative month 3 |
|
Score | 3.25±0.52 | 3.68±0.78 | 0.008 |
|
P-value | <0.001 | <0.001 |
|
| Last
follow-up |
|
Score | 2.04±0.83 | 2.13±0.91 | 0.665 |
|
P-value | <0.001 | <0.001 |
|
ROM
The pre-operative ROM of the shoulder joint are
described in Table IV and mainly
include Abd, internal rotation (IR), external rotation to the side
(ERs) and forward flexion (FF). In the subpectoral group, the
active FF changed from 138.25±24.18 pre-operatively to 160.24±13.94
at the time of the final follow-up; furthermore, ERs changed from
45.96±11.32 to 59.96±10.85, IR from 38.42±9.18 to 56.71±8.73 and
Abd from 145.80±21.42 to 170.17±8.32. In the arthroscopic tenodesis
group, the active FF changed from 136.82±25.77 pre-operatively to
157.63±15.81 at the final follow-up; furthermore, ERs changed from
46.83±14.74 to 58.32±11.41, IR from 38.93±8.35 to 54.26±9.45 and
Abd from 148.48±23.04 to 168.53±7.98 (Table IV). All values had improved
significantly at the time of the final follow-up (P<0.05).
However, no significant difference was observed between the two
groups with regard to improvement in Abd, IR, ERs and FF of the
shoulder joint.
 | Table IV.Comparison of range of motion between
the two groups. |
Table IV.
Comparison of range of motion between
the two groups.
| Item | Subpectoral group
(n=35) | Arthroscopic group
(n=36) | P-value |
|---|
| BL |
| FF | 138.25±24.18 | 136.82±25.77 | 0.810 |
|
ERS | 45.96±11.32 | 46.83±14.74 | 0.782 |
| IR | 38.42±9.18 | 38.93±8.35 | 0.807 |
|
Abd | 145.80±21.42 | 148.48±23.04 | 0.614 |
| Last follow-up |
|
|
|
| FF | 160.24±13.94 | 157.63±15.81 | 0.464 |
|
P-value | <0.001 | <0.001 |
|
|
ERS | 59.96±10.85 | 58.32±11.41 | 0.537 |
|
P-value | <0.001 | <0.001 |
|
| IR | 56.71±8.73 | 54.26±9.45 | 0.261 |
|
P-value | <0.001 | <0.001 |
|
|
Abd | 170.17±8.32 | 168.53±7.98 | 0.397 |
|
P-value | <0.001 | <0.001 |
|
Evaluation of complications using BAD
and ultrasound
Between the two groups, a significant difference was
observed in the synovitis around the bicipital groove at 3 months
(P<0.05), although no significant differences were observed
between the two groups at the time of the final follow-up. At 3
months post-operatively, synovitis around the bicipital groove was
detected in 2 cases (5.7%) of the subpectoral group, which
disappeared at the time of the final follow-up. In the arthroscopic
tenodesis group, 12 cases (33.3%) of synovitis around the bicipital
groove and 3 cases (8.3%) of residual synovitis were detected at
the time of the final follow-up. At 3 months post-operation,
synovitis was significantly higher in the arthroscopic tenodesis
group (P<0.05). Until the last follow-up RC re-tear occurred in
one case (2.9%) of the subpectoral group and 3 cases (8.3%) of the
arthroscopic tenodesis group (Table
V). There was no significant difference in the prevalence of
re-tear between the two groups. There was no case of fixation
failure in the biceps in the two groups. No significant difference
in the BAD was observed between the two groups at the time of the
last follow-up.
 | Table V.Evaluations of the biceps tendon. |
Table V.
Evaluations of the biceps tendon.
| Item | Subpectoral group
(n=35) | Arthroscopic group
(n=36) | P-value |
|---|
| Synovitis around
the bicipital groove using U/S |
|
Post-operative month 3 | 2 (5.71%) | 12 (33.33%) | 0.003 |
| Last
follow-up | 0 (0%) | 3 (8.33%) | 0.248 |
| BAD (cm) | 0.26±0.12 | 0.29±0.09 | 0.237 |
| Retear of rotator
cuff | 1 (2.86%) | 3 (8.33%) | 0.627 |
Discussion
Proximal LHBT lesions are a common cause of shoulder
pain and dysfunction. Pure LHBT lesions are relatively rare; they
are frequently accompanied by RC injury (3–6,20–23). At
present, the clinical diagnosis of LHBT lesions is challenging and
the condition is easily neglected (42). Another challenge for surgeons is the
selection of the appropriate treatment following diagnosis
(21,43). For cases of mild LHBT lesion, oral
non-steroidal anti-inflammatory drugs, immobilization,
physiotherapy and other treatments are usually administered at
first, but even in slightly serious cases, surgical intervention is
required (37,44). Barber et al (45) have reported that a local tear of the
tendon of <25% is reversible and conservative treatment may be
applied. However, when the tear area exceeds 30% or the lesions are
subluxation or degeneration of the LHBT or above type II superior
labrum anterior and posterior lesion, local debridement alone may
not achieve satisfactory results. This is due to the fact that pain
in the shoulder may persist even following RCR (46–48).
LHBT tenotomy or tenodesis is commonly performed at the same time
as RCR.
In recent years, most researchers have focused on
the comparison between the curative effects of LHBT tenotomy and
tenodesis. A large number of clinical comparative studies and
meta-analyses have assessed the treatment of LHBT lesions combined
with RCR with tenotomy and tenodesis (20–23,49–53).
These studies indicated that the pain and function of the shoulder
joint may be significantly improved by the two methods. Zhang et
al (21) observed no significant
differences in the curative effect, patient satisfaction and rate
of complications between the two groups. However, Oh et al
(22) and Lee et al (51) suggested that LHBT tenodesis may
maintain the supination function of the forearm and significantly
reduce the incidence of Popeye sign deformity, as compared with
simple LHBT tenotomy. Oh et al (22) also observed that residual pain in the
pectoral muscles following LHBT tenotomy is likely to occur. A
meta-analysis by Ge et al (49), including 7 studies, suggested that
LHBT tenodesis had a higher Constant score and lower incidence of
upper arm spastic pain and Popeye sign deformity than simple
tenotomy. Shang et al (50)
included 10 high-quality studies in their meta-analysis. No
significant differences were identified in the function and
incidence of upper arm spastic pain between LHBT tenodesis and
tenotomy; however, LHBT tenodesis still had a lower incidence of
Popeye sign deformity and a higher Constant score. In general,
simple LHBT tenotomy should be avoided in physically active young
patients with cosmetic requirements.
Although the advantages of LHBT tenodesis regarding
biomechanics and clinical efficacy have been confirmed, there is
still considerable controversy regarding the choice of fixing
position. Arthroscopic proximal fixation and small
incision-assisted distal fixation are common. In recent years,
there have also been clinical studies on the comparison of the
efficacy between distal and proximal fixation of the LHBT (15,16,54–58), all
of which suggested that the two methods have a good clinical
efficacy, high patient satisfaction and few complications; no
significant differences were observed in functional recovery, pain
improvement and complications between the two methods. However, in
the study by Duchman et al (15), a significant difference was observed
in the shoulder flexion function between the two groups. Few
studies compared and analyzed the efficacy of the preliminary phase
following surgery, and it was therefore not possible to
comprehensively evaluate the efficacy. In addition, LHBT lesions
alone are rare; they are frequently combined with other complex
shoulder diseases, such as subacromial impingement, synovitis of
shoulder joint, which was a limitation of the present study. To
date, only a small number of studies have compared the clinical
efficacy between distal and proximal fixation of the LHBT in the
treatment of patients with LHBT lesions accompanied by RCR.
According to the results of the present study,
small-incision open distal subpectoral and arthroscopic proximal
tenodesis may effectively improve the function of the shoulder
joint and relieve pain. Up to the last follow-up, no significant
difference in the shoulder activity degree was observed between the
two groups. Small-incision open tenodesis had further advantages
pertaining to surgery time and amount of inter-operative blood
loss. At 2 weeks following surgery, the VAS and ASES scores of the
subpectoral group were higher than those of the arthroscopic group.
In the treatment of LHBT lesions combined with RCR, the negative
responses observed in the arthroscopic group during the early
follow-up, as compared with the effect in the subpectoral group,
may be due to early intrapectoral inflammation in the arthroscopic
group. On the other hand, LHBT tendonitis may have pre-existed.
Arthroscopy is the gold standard for diagnosing LHBT lesions
(59); even under maximum
visualization during shoulder arthroscopy (60), the average moving length of the LHBT
in the cadaver model is 15–19 mm (61,62),
which is ~14 mm in the human body (63). Only 78% of the length from the
beginning of LHBT to the lower edge of the tendon of the
subscapularis muscle and 55% of the proximal edge of the pectoralis
major muscle may be observed, which means that nearly 1/3 of the
tendinous parts of the LHBT cannot be observed in the joint
(62). Moon et al (64) reported that ~80% of intra-articular
tendon tears had hidden lesions extending to the outer part of the
distal joint. Therefore, distal tenodesis is considered to be a
better option for removing all hidden LHBT lesions, as it is
challenging to control the length and tension of the LHBT via
arthroscopic proximal tenodesis. On the other hand, the early
intrapectoral inflammation in the arthroscopic group may be due to
tension-length mismatch or LHBT tenosynovitis caused by the
insertion of a fixation screw under the acromion; small-incision
open distal subpectoral tenodesis is able to remove all hidden LHBT
lesions and avoid pain caused by inflammation of remaining LHBT
lesions. In the present study, the identification of synovitis
around the bicipital groove was an important result. Therefore, as
compared with arthroscopic proximal tenodesis, small-incision open
distal subpectoral distal tenodesis is a more effective way to
relieve pain and avoid post-operative LHBT tenosynovitis. However,
regardless of the surgical method, the present study suggested that
the synovitis around the bicipital groove did not completely
disappear at 3 months post-operatively. Therefore, in order to
obtain better results as rapidly as possible, the inflammatory
tissue must be carefully cleaned during surgery.
The present study had certain limitations. First, it
was not a randomized controlled trial or a prospective trial.
Furthermore, the average follow-up time of ~21 months employed in
the study is insufficient to assess long-term outcomes. In
addition, the strength of the elbow joint was not assessed and not
all types of RC injury (such as rupture of at least two of the four
RC tendons) were covered. Due to the lack of continuous MRI and
LHBT biopsy, it was not possible to confirm whether the advantages
of small-incision open distal subpectoral biceps tenodesis in early
functional therapy and remaining biceps tendinitis were directly
correlated, which may be the focus of future research.
In conclusion, small-incision open distal
subpectoral and arthroscopic proximal biceps tenodesis may
effectively improve the function of the shoulder joint and relieve
pain in the treatment of LHBT lesions accompanied by RC tears. By
contrast, small-incision open distal subpectoral tenodesis has the
advantages of shorter surgery time, less intra-operative bleeding
and encouraging early results over arthroscopic proximal tenodesis.
However, regardless of the surgical method, special attention
should be paid to the careful removal of the inflammatory
tissue.
Acknowledgements
Not applicable.
Funding
This work was supported by the Academician
Workstation Construction Project of Luzhou, Sichuan Province, China
(grant no. 20180101).
Availability of data and materials
The datasets generated and/or analyzed during the
current study are not publicly available due to being restricted by
the medical ethics committee of the Affiliated Traditional Chinese
Medicine Hospital of Southwest Medical University but are available
from the correspoinding author on reasonable request for
researchers who meet the criteria to access confidential
information.
Authors' contributions
GY and SF designed the research and wrote the first
draft of the manuscript. GY, JY and LZ performed the data
acquisition and follow ups of patients. YL and JY analyzed and
interpreted the data as well as finalized the manuscript. XG and SF
Processed pictures and proofread the manuscript. All authors read
and approved the final version of the manuscript.
Ethics approval and consent to
participate
All clinical procedures were approved by the Ethics
Committee of the Affiliated Traditional Chinese Medicine Hospital
of Southwest Medical University (Luzhou, China; approval no.
KY20180603), performed in accordance with the 1964 Declaration of
Helsinki and its later amendments and the study was registered as a
clinical trial in the Chinese Trial Registry (no.
ChiCTR1800015643). All patients understood the intervention
procedure and signed the relevant informed consent form.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Boileau P, Baqué F, Valerio L, Ahrens P,
Chuinard C and Trojani C: Isolated arthroscopic biceps tenotomy or
tenodesis improves symptoms in patients with massive irreparable
rotator cuff tears. J Bone Joint Surg Am. 89:747–757. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Landreau P, Catteeuw A, Hamie F, Saithna
A, Sonnery-Cottet B and Smigielski R: Anatomic study and reanalysis
of the nomenclature of the anterolateral complex of the knee
focusing on the distal iliotibial band: Identification and
description of the condylar strap. Orthop J Sports Med.
7:23259671188180642019. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Ataoglu MB, Cetinkaya M, Ozer M, Ayanoglu
T and Kanatli U: The high frequency of superior labrum, biceps
tendon, and superior rotator cuff pathologies in patients with
subscapularis tears: A cohort study. J Orthop Sci. 23:304–309.
2018. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Kennedy NI, Sanchez G, Mannava S, Ferrari
MB, Frangiamore SJ and Provencher MT: Arthroscopic rotator cuff
repair with mini-open subpectoral biceps tenodesis. Arthrosc Tech.
6:e1667–e1674. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Su WR, Budoff JE and Lou JP: The effect of
posterosuperior rotator cuff tears and biceps loading on
glenohumeral translation. Arthroscopy. 26:578–586. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Desai SS and Mata HK: Long head of biceps
tendon pathology and results of tenotomy in full-thickness
reparable rotator cuff tear. Arthroscopy. 33:1971–1976.
2017.PubMed/NCBI
|
|
7
|
Hassan S and Patel V: Biceps tenodesis
versus biceps tenotomy for biceps tendinitis without rotator cuff
tears. J Clin Orthop Trauma. 10:248–256. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Forsythe B, Agarwalla A, Puzzitiello RN,
Mascarenhas R and Werner BC: Rates and risk factors for revision
open and arthroscopic proximal biceps tenodesis. Orthop J Sports
Med. 7:23259671188254732019. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Godenèche A, Nové-Josserand L, Audebert S,
Toussaint B, Denard PJ; French Society for Arthroscopy (SFA), ;
Lädermann A: Relationship between subscapularis tears and injuries
to the biceps pulley. Knee Surg Sports Traumatol Arthrosc.
25:2114–2120. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Lee SH, Nam DJ, Kim SJ and Kim JW:
Comparison of clinical and structural outcomes by subscapularis
tendon status in massive rotator cuff tear. Am J Sports Med.
45:2555–2562. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Motley GS, Guengerich B, Schuller T and
Turbyfill A: The ramp test: An arthroscopic technique for
confirming intra-articular subluxation and instability of the long
head of the biceps tendon within the shoulder. Arthrosc Tech.
7:e327–e330. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Osti L, Buda M, Buono AD, Osti R and
Massari L: Clinical evidence in the treatment of rotator cuff tears
with hyaluronic acid. Muscles Ligaments Tendons J. 5:270–275. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Shi LL, Mullen MG, Freehill MT, Lin A,
Warner JJ and Higgins LD: Accuracy of long head of the biceps
subluxation as a predictor for subscapularis tears. Arthroscopy.
31:615–619. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Watson ST, Robbins CB, Bedi A, Carpenter
JE, Gagnier JJ and Miller BS: Comparison of outcomes 1 year after
rotator cuff repair with and without concomitant biceps surgery.
Arthroscopy. 33:1928–1936. 2017.PubMed/NCBI
|
|
15
|
Duchman KR, DeMik DE, Uribe B, Wolf BR and
Bollier M: Open versus arthroscopic biceps tenodesis: A comparison
of functional outcomes. Iowa Orthop J. 36:79–87. 2016.PubMed/NCBI
|
|
16
|
Green JM, Getelman MH, Snyder SJ and Burns
JP: All-Arthroscopic suprapectoral versus open subpectoral
tenodesis of the long head of the biceps brachii without the use of
interference screws. Arthroscopy. 33:19–25. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Xu GJ and Dai XS: Tenotomy fixed on distal
trochlea under arthroscopy for long head of biceps tendon and
rotator cuff tear. Zhongguo Gu Shang. 31:612–616. 2018.(In
Chinese). PubMed/NCBI
|
|
18
|
Veen EJD, Koorevaar CT and Diercks RL:
Using the long head of biceps tendon autograft as an anatomical
reconstruction of the rotator cable: An arthroscopic technique for
patients with massive rotator cuff tears. Arthrosc Tech.
7:e699–e703. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Saithna A, Longo A, Leiter J, Old J and
MacDonald PM: Shoulder arthroscopy does not adequately visualize
pathology of the long head of biceps tendon. Orthop J Sports Med.
4:23259671156239442016. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Meraner D, Sternberg C, Vega J, Hahne J,
Kleine M and Leuzinger J: Arthroscopic tenodesis versus tenotomy of
the long head of biceps tendon in simultaneous rotator cuff repair.
Arch Orthop Trauma Surg. 136:101–106. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Zhang Q, Zhou J, Ge H and Cheng B:
Tenotomy or tenodesis for long head biceps lesions in shoulders
with reparable rotator cuff tears: A prospective randomised trial.
Knee Surg Sports Traumatol Arthrosc. 23:464–469. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Oh JH, Lee YH, Kim SH, Park JS, Seo HJ,
Kim W and Park HB: Comparison of treatments for superior
labrum-biceps complex lesions with concomitant rotator cuff repair:
A prospective, randomized, comparative analysis of debridement,
biceps tenotomy, and biceps tenodesis. Arthroscopy. 32:958–967.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Franceschi F, Longo UG, Ruzzini L,
Rizzello G, Maffulli N and Denaro V: No advantages in repairing a
type II superior labrum anterior and posterior (SLAP) lesion when
associated with rotator cuff repair in patients over age 50: A
randomized controlled trial. Am J Sports Med. 36:247–253. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
24
|
De Carli A, Vadalà A, Zanzotto E, Zampar
G, Vetrano M, Iorio R and Ferretti A: Reparable rotator cuff tears
with concomitant long-head biceps lesions: Tenotomy or
tenotomy/tenodesis? Knee Surg Sports Traumatol Arthrosc.
20:2553–2558. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Koh KH, Ahn JH, Kim SM and Yoo JC:
Treatment of biceps tendon lesions in the setting of rotator cuff
tears: Prospective cohort study of tenotomy versus tenodesis. The
Am J Sports Med. 38:1584–1590. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Cho NS, Cha SW and Rhee YJ: Funnel
tenotomy versus intracuff tenodesis for lesions of the long head of
the biceps tendon associated with rotator cuff tears. Am J Sports
Med. 42:1161–1168. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Karlsson J: In reparable rotator cuff
tears with lesions of the long head of the biceps brachii tendon,
tenotomy did not differ from tenodesis in terms of function or
pain. J Bone Joint Surg Am. 99:3512017. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Ikemoto RY, Pileggi PE, Murachovsky J,
Nascimento LG, Serpone RB, Strose E and Oliveira LH: Tenotomy with
or without tenodesis of the long head of the biceps using repair of
the rotator cuff. Rev Bras Ortop. 47:736–740. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Kukkonen J, Rantakokko J, Virolainen P and
Aärimaa V: The effect of biceps procedure on the outcome of rotator
cuff reconstruction. ISRN Orthop. 2013:8409652013. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Sentürk I, Ozalay M, Akpınar S, Leblebici
B, Cınar BM and Tuncay C: Clinical and isokinetic comparison
between tenotomy and tenodesis in biceps pathologies. Acta Orthop
Traumatol Turc. 45:41–46. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Delle Rose G, Borroni M, Silvestro A,
Garofalo R, Conti M, De Nittis P and Castagna A: The long head of
biceps as a source of pain in active population: Tenotomy or
tenodesis? A comparison of 2 case series with isolated lesions.
Musculoskelet Surg. 96 (Suppl 1):S47–S52. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Ahmad CS, DiSipio C, Lester J, Gardner TR,
Levine WN and Bigliani LU: Factors affecting dropped biceps
deformity after tenotomy of the long head of the biceps tendon.
Arthroscopy. 23:537–541. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Klinger HM, Spahn G, Baums MH and Steckel
H: Arthroscopic debridement of irreparable massive rotator cuff
tears-a comparison of debridement alone and combined procedure with
biceps tenotomy. Acta Chir Belg. 105:297–301. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Friedman JL, FitzPatrick JL, Rylander LS,
Bennett C, Vidal AF and McCarty EC: Biceps tenotomy versus
tenodesis in active patients younger than 55 years: Is there a
difference in strength and outcomes? Orthop J Sports Med.
3:23259671155708482015. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Gervasi E, Sebastiani E and Cautero E:
No-holes transpectoral tenodesis technique tenotomy of the long
head of the biceps brachii. Muscles Ligaments Tendons J. 6:427–432.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Park JY, Lee JH, Oh KS, Chung SW, Bang JY
and Noh YM: Bridge Tenodesis: A Secure fixation technique for
biceps long head tendinopathy during arthroscopic rotator cuff
repair using a suture-bridge technique. Arthrosc Tech.
5:e1077–e1081. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Nassos JT and Chudik SC: Arthroscopic
rotator cuff repair with biceps tendon augmentation. Am J Orthop
(Belle Mead NJ). 38:279–281. 2009.PubMed/NCBI
|
|
38
|
Elser F, Braun S, Dewing CB, Giphart JE
and Millett PJ: Anatomy, function, injuries, and treatment of the
long head of the biceps brachii tendon. Arthroscopy. 27:581–592.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Hufeland M, Kolem C, Ziskoven C, Kircher
J, Krauspe R and Patzer T: The influence of suprapectoral
arthroscopic biceps tenodesis for isolated biceps lesions on elbow
flexion force and clinical outcomes. Knee Surg Sports Traumatol
Arthrosc. 25:3220–3228. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Faruqui S, Kotob MA, Hanna CC and Foad A:
The modified Norwegian method of biceps tenodesis: How well does it
work? Knee Surg Sports Traumatol Arthrosc. 25:3264–3269. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Chen CH, Hsu KY, Chen WJ and Shih CH:
Incidence and severity of biceps long head tendon lesion in
patients with complete rotator cuff tears. J Trauma. 58:1189–1193.
2005. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Jeong JY, Park SM, Park YE and Yoo JC:
Morphological classification of anatomical variants of the
intra-articular portion of the long head of the biceps brachii
tendon and analysis of the incidence and the relationship with
shoulder disease for each subtype. J Orthop Surg (Hong Kong).
25:23094990177422072017. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Ciccotti MG: Editorial commentary: The
long head of the biceps brachii tendon-the shoulder surgeon's
conundrum. Arthroscopy. 33:1937–1939. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Frost A, Zafar MS and Maffulli N: Tenotomy
versus tenodesis in the management of pathologic lesions of the
tendon of the long head of the biceps brachii. Am J Sports Med.
37:828–833. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Barber FA, Byrd JW, Wolf EM and Burkhart
SS: How would you treat the partially torn biceps tendon.
Arthroscopy. 17:636–639. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Kelly AM, Drakos MC, Fealy S, Taylor SA
and O'Brien SJ: Arthroscopic release of the long head of the biceps
tendon: Functional outcome and clinical results. Am J Sports Med.
33:208–213. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Maynou C, Mehdi N, Cassagnaud X, Audebert
S and Mestdagh H: Clinical results of arthroscopic tenotomy of the
long head of the biceps brachii in full thickness tears of the
rotator cuff without repair: 40 cases. Rev Chir Orthop Réparatrice
Appar Mot. 91:300–306. 2005.(In French). View Article : Google Scholar
|
|
48
|
Kim YS, Jeong JY and Lee HJ: Arthroscopic
tenodesis of the long head of the biceps tendon. JBJS Essent Surg
Tech. 7:e192017. View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Ge H, Zhang Q, Sun Y, Li J, Sun L and
Cheng B: Tenotomy or tenodesis for the long head of biceps lesions
in shoulders: A systematic review and meta-analysis. PLoS One.
10:e01212862015. View Article : Google Scholar : PubMed/NCBI
|
|
50
|
Shang X, Chen J and Chen S: A
meta-analysis comparing tenotomy and tenodesis for treating rotator
cuff tears combined with long head of the biceps tendon lesions.
PLoS One. 12:e01857882017. View Article : Google Scholar : PubMed/NCBI
|
|
51
|
Lee HJ, Jeong JY, Kim CK and Kim YS:
Surgical treatment of lesions of the long head of the biceps
brachii tendon with rotator cuff tear: A prospective randomized
clinical trial comparing the clinical results of tenotomy and
tenodesis. J Shoulder Elbow Surg. 25:1107–1114. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
52
|
Leroux T, Chahal J, Wasserstein D, Verma
NN and Romeo AA: A systematic review and meta-analysis comparing
clinical outcomes after concurrent rotator cuff repair and long
head biceps tenodesis or tenotomy. Sports Health. 7:303–307. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
53
|
Hsu AR, Ghodadra NS, Provencher MT, Lewis
PB and Bach BR: Biceps tenotomy versus tenodesis: A review of
clinical outcomes and biomechanical results. J Shoulder Elbow Surg.
20:326–332. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
54
|
Yi Y, Lee JM, Kwon SH and Kim JW:
Arthroscopic proximal versus open subpectoral biceps tenodesis with
arthroscopic repair of small or medium-sized rotator cuff tears.
Knee Surg Sports Traumatol Arthrosc. 24:3772–3778. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
55
|
Gombera MM, Kahlenberg CA, Nair R,
Saltzman MD and Terry MA: All-arthroscopic suprapectoral versus
open subpectoral tenodesis of the long head of the biceps brachii.
Am J Sports Med. 43:1077–1083. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
56
|
Biz C, Vinanti GB, Rossato A, Arnaldi E
and Aldegheri R: Prospective study of three surgical procedures for
long head biceps tendinopathy associated with rotator cuff tears.
Muscles Ligaments Tendons J. 2:133–136. 2012.PubMed/NCBI
|
|
57
|
Werner BC, Lyons ML, Evans CL, Griffin JW,
Hart JM, Miller MD and Brockmeier SF: Arthroscopic suprapectoral
and open subpectoral biceps tenodesis: A comparison of restoration
of length-tension and mechanical strength between techniques.
Arthroscopy. 31:620–627. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
58
|
Lutton DM, Gruson KI, Harrison AK,
Gladstone JN and Flatow EL: Where to tenodese the biceps: Proximal
or distal? Clin Orthop Relat Res. 469:1050–1055. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
59
|
Bennett WF: Visualization of the anatomy
of the rotator interval and bicipital sheath. Arthroscopy.
17:107–111. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
60
|
Hart ND, Golish SR and Dragoo JL: Effects
of arm position on maximizing intraarticular visualization of the
biceps tendon: A cadaveric study. Arthroscopy. 28:481–485. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
61
|
Taylor SA, Khair MM, Gulotta LV, Pearle
AD, Baret NJ, Newman AM, Dy CJ and O'Brien SJ: Diagnostic
glenohumeral arthroscopy fails to fully evaluate the biceps-labral
complex. Arthroscopy. 31:215–224. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
62
|
Festa A, Allert J, Issa K, Tasto JP and
Myer JJ: Visualization of the extra-articular portion of the long
head of the biceps tendon during intra-articular shoulder
arthroscopy. Arthroscopy. 30:1413–1417. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
63
|
Gilmer BB, DeMers AM, Guerrero D, Reid JB
III, Lubowitz JH and Guttmann D: Arthroscopic versus open
comparison of long head of biceps tendon visualization and
pathology in patients requiring tenodesis. Arthroscopy. 31:29–34.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
64
|
Moon SC, Cho NS and Rhee YG: Analysis of
‘hidden lesions’ of the extra-articular biceps after subpectoral
biceps tenodesis: The subpectoral portion as the optimal tenodesis
site. Am J Sports Med. 43:63–68. 2015. View Article : Google Scholar : PubMed/NCBI
|