Introduction
Congenital heart disease (CHD) is one of the most
common birth defects and is a major cause of childhood morbidity
and mortality (1). Most patients
with CHD require surgery to correct these heart defects (2). Some complex CHDs require multiple
open-heart surgeries; consequently, numerous heart patches for the
repair of cardiac defects are needed (2). Despite significant progress in the
development of various materials to make cardiac patches, including
Dacron (3), Gore-Tex (4) and autologous (5) or bovine pericardium (6), significant drawbacks exist, including
increased risk of immune response (7), calcification (6), thrombosis (8,9) and the
lack of growth potential (10).
Moreover, these materials may become fibrous calcified tissues that
cannot degrade, thereby preventing simultaneous growth within the
heart and loss of function over time (11). Hence, patients typically require
reoperation, which may cause delayed recovery and could result in
an increased economic burden to both the family and society
(11). Therefore, optimal materials
for heart patches should be able to inhibit the immune response,
calcification and thrombosis, and support growth of native tissue
(10).
With the advantages of non-toxicity,
biocompatibility and degradability, natural materials such as
chitosan, collagen and gelatin have been used in various tissue
engineering applications (12–14).
These materials have shown good scaffold properties that allow for
better mechanics and a significant influence on cellular behavior
(12–14). However, the compositions of these
materials are relatively simple and cannot provide a complete
extracellular matrix (ECM) environment (15). On the other hand, ECM harvested from
decellularized tissue lacks most of the immunogenicity but retains
the majority of the ECM components (16). Previous studies showed that ECM,
which is biocompatible, provides physical structural support and
plays an essential role in providing signaling for cell attachment,
proliferation and differentiation (17–19).
Thus, the ideal biological scaffold would be made by a mixture of
these two types of materials, and would be able to retain
mechanical properties while also providing an extracellular matrix
environment (20).
Previous studies found that ECM can be harvested
from tissues such as cartilage, skeletal muscle, tendons, adipose
tissue, vessels, lung, liver, intestine (17,21,22) and
bovine ureter (23), and may be
applied as biological scaffolds with beneficial results. Previous
studies in which porcine heart matrix was used for construction of
tissue engineered heart patches demonstrated that porcine ECM could
support cardiomyocytes, improved heart function and was capable of
heart defect repair (24,25). However, ECM is frequently derived
from non-cardiac or heart tissue of other species. The present
study hypothesized that ECM from human heart tissue may have a
higher biocompatibility. Therefore, the present study combined
human cardiac (cECM) with biodegradable natural chitosan-gelatin
(CG) for the construction of cardiac extracellular
matrix-chitosan-gelatin (cECM-CG) composite scaffold and studied
its characteristics.
Thrombosis is a significant limitation of current
grafts (8). Accumulating evidence
showed that the endothelium, which maintains vessel integrity,
plays an essential role in preventing thrombosis (26). Previous studies suggested that
endothelial progenitor cells (EPCs), characterized by the ability
to differentiate into endothelial cells, are a potential source of
endothelial repair by participating in the process of
endothelialization (27–29). Moreover, CD34+ cells are
considered to be EPCs (30). A
previous study showed that stent surfaces coated with antibodies
against CD34, exhibited high affinity for EPC and could promote
rapid endothelialization, prevent stent thrombosis and reduce
restenosis (31). The present study
hypothesized that CD34+ EPCs seeded on the scaffold of
tissue-engineered heart patches could promote the scaffold
endothelialization.
The present study created a cECM-CG composite
scaffold seeded with CD34+ EPCs intended for
tissue-engineered heart patch. The present study investigated the
characteristics of this scaffold, including its
endothelialization.
Materials and methods
Cardiac tissue and bone marrow
samples
Human right atrial appendage and bone marrow samples
were collected after written informed consent from parents of
pediatric patients was obtained. All experiments were approved by
the Ethics Committee at Shanghai Children's Medical Center
(approval no. SCMCIRB-K2016025). All investigations were conducted
according to the principles expressed in the Declaration of
Helsinki. Specimens of right atrial appendage and bone marrow of
sternum were collected from the patients (including 22 females and
28 males; age, 1 month-3 years old) diagnosed as ventricular septal
defect (VSD) or atrial septal defect (ASD) during open-heart
surgery from May 2016 to May 2018 in our hospital. Right atrial
appendages were processed for cECM preparation. Bone marrow was
used to isolate CD34+ EPCs.
Preparation of cECM and scaffolds
Collected right atrial appendages were frozen in
optimal cutting temperature compound, sectioned at 50 µm, and
decellularized in 0.2% SDS solution for 12 h with constant shaking
at 37°C. Subsequently, the tissues were stirred in 200 mg/l DNase I
solution for 30 min at 37°C. Finally, the decellularized cardiac
tissue was rinsed with deionized water until complete removal of
detergents. The ECM was lyophilized, quantified and milled into
fine powder (32). Then, 2% chitosan
and 2% gelatin were prepared. Chitosan (cat. no. 1105508;
Sigma-Aldrich; Merck) was added to 1% glacial acetic acid. The
solution was shaken at 37°C for 12 h to ensure complete
solubilization. Gelatin (cat. no. 1288485, Sigma-Aldrich; Merck)
was dissolved in deionized water and incubated in a water bath at
50°C for 15 min. Subsequently, chitosan and gelatin were mixed at a
ratio of 2:1. The cECM powder was added to the chitosan and gelatin
mixture solution, and was subsequently grounded using an
ultrasonicator. The concentration of the cECM was 1.6 mg/ml.
The CG mixture and the cECM-CG mixture were poured
into a 96-well plate (50 µl/well). Subsequently, both mixtures were
frozen at −80°C overnight, lyophilized for 24 h in a vacuum
freeze-drier (VirtisBenchtop 6.6, SP Industries) to form porous
scaffolds. The scaffolds were washed with ethanol to remove
residual glacial acetic acid. Subsequently, the scaffolds were
washed gently with PBS for five times (10 min each), and were
sterilized by overnight incubation at room temperature using
ultraviolet light in a cell culture hood.
Analysis of cECM components
Cardiac tissues before and after decellularization
were fixed in 4% paraformaldehyde at 4°C for 24 h, embedded in
paraffin, and cut into 5-µm thick sections. Sections were rinsed
twice with xylene for 15 min and dehydrated with a descending
alcohol series (100% alcohol for 5 min; 95% alcohol for 5 min; 75%
alcohol for 5 min). Tissue was then stained with hematoxylin for 10
min and eosin for 5 min at room temperature.
The sections were dewaxed, rehydrated, stained in
Weigert's iron hematoxylin solution for 5 min at room temperature,
washed. Sections were then treated with Van Gieson's solution for
3–5 min at room temperature. Finally, the tissue was dehydrated,
cleared and sealed.
The sections were dewaxed, rehydrated, stained in
Weigert's iron hematoxylin solution at room temperature for 10 min,
rinsed and washed. Sections were then stained in Biebrich
scarlet-acid fuchsin solution at room temperature for 10–15 min,
washed and then differentiated in phosphomolybdic-phosphotungstic
acid solution for 10–15 min. The sections were transferred directly
to aniline blue solution and stained for 5–10 min at room
temperature, rinsed and differentiated in 1% acetic acid solution
for 2–5 min at room temperature. Finally, the sections were
dehydrated, cleared and sealed. The presence of the adhesive
proteins fibronectin and laminin in cECM was assessed by
immunohistochemical staining. Briefly, the slides were placed in
citrate antigen retrieval buffer and heated to 95°C for 20 min.
After cooling to room temperature, the sections were treated with
3% hydrogen peroxide solution for 20 min at room temperature and
then incubated in a humidity chamber for 30 min with 10% (w/v)
normal goat serum (cat. no. 016201; Invitrogen; Thermo Fisher
Scientific, Inc.). Hereafter, sections were incubated with rabbit
anti-fibronectin antibody (1:250; cat. no. ab32419; Abcam) at 4°C
overnight. After sections were washed with PBS, goat anti-rabbit
IgG H&L (HRP) (1:1,000; cat. no. ab6721; Abcam) was added for
30 min. Sections were then rinsed in PBS, and diaminobenzidine
solution (DAB) was applied. After staining, slides were dehydrated,
cover-slipped. All sections were imaged under a light Olympus CX31
microscope (magnification ×20; Olympus Corporation).
cECM quantification
Glycosaminoglycans (GAG) present in the cECM was
measured using Glycosaminoglycans Assay kit (Chondrex, Inc).
Briefly, samples before and after decellularization were weighed
after lyophilization. Subsequently, lyophilized samples were
digested and stained with 1, 9-dimethylmethylene blue (DMB) for 4
min at room temperature. A dilution series of chondroitin sulfate
was used as standard. Absorbance was measured at 525 nm with a
Synergy HT Microplate Absorbance Reader (BioTek Instruments, Inc.).
The GAG content was normalized to the dry weight of the
samples.
DNA content was assayed using the tissue gDNA
Miniprep kit (Biomiga, Inc.), and DNA concentration was determined
by spectrophotometry (NanoDrop 2000c; Thermo Fisher Scientific,
Inc.).
Determination of scaffold
characteristics
Scanning electron microscope (SEM) was used to
visualize the structure of the CG and cECM-CG scaffolds. Scaffolds
were prepared by fixation with 2.5% glutaraldehyde for 2 h at room
temperature, followed by dehydration with a series of ethanol
rinses (30-100%). The samples were critical point dried and coated
with iridium. Electron microscopy images were obtained using SEM
(magnification, ×800; Quanta 2000; FEI; Thermo Fisher Scientific,
Inc.).
CG and cECM-CG scaffolds were created in a 96-well
plate in triplicates. The dry weight (Wd) of both scaffolds was
measured before they were transferred to a 24-well plate and
allowed to swell in PBS. The swelled weight (Ws) was measured every
10 min for 1 h. Swelling ratios were calculated as follows:
Swelling ratio = (Ws - Wd) / Wd.
Isolation and culture of
CD34+ EPCs
Human bone marrow samples were collected from
pediatric patients undergoing VSD or ASD surgery. Bone marrow
mononuclear cells were collected using gradient centrifugation.
Bone marrow was resuspended in Hank's balanced salt solution (GE
Healthcare Life Sciences) and 20 µ/ml heparin (Sigma-Aldrich;
Merck) and then centrifuged for 30 min at 400 g at room
temperature. CD34+ EPCs were isolated from the
mononuclear cells using magnetic cell sorting. Then the cells were
seeded on the pre-prepared scaffolds at 37°C in CO2
incubator.
Flow cytometry analysis
To study the purity of sorted cells, freshly
isolated CD34+ EPCs were collected for flow cytometry
analysis. Briefly, cell suspensions were centrifuged at 300 × g for
5 min at 4°C, and cell pellets resuspended in PBS containing 1%
BSA. Mouse Anti-Human CD34 antibody (cat. no. 560710; BD
Biosciences) was diluted to 1:100 in PBS. Samples were incubated
for 30 min in the dark on ice, followed by two washing steps with
PBS (centrifugation for 5 min at 300 × g after each washing step at
4°C). Finally, samples were subjected to flow cytometry analysis
using Accuri C6 flow cytometer (BD Biosciences). Fluorescence was
analyzed with CFlow Plus software (BD Biosciences).
Cell viability analysis
To investigate the viability of CD34+
EPCs cultured on the scaffolds, cell viability was analyzed 5 days
after seeding using a viability assay. Cells were collected, washed
with PBS, and incubated in 5 µmol/l calcein AM (labeling living
cells; Thermo Fisher Scientific, Inc.) and 9 µmol/l propidium
iodide (labeling dead cells; Thermo Fisher Scientific, Inc.) for 30
min at 37°C. Images of the stained samples were obtained using an
optical microscope (Nikon Corporation). The number of living and
dead cells was calculated based on three different fields of view
(magnification, ×20).
Cell proliferation analysis
To identify the proliferative activity of
CD34+ EPCs, Cells cultured on CG and cECM-CG scaffolds
were stained with primary antibody Mouse anti-Ki67 IgG (1:200; cat.
no. 561165; BD Biosciences, CA, USA) by overnight incubation at
4°C. Donkey anti-mouse IgG conjugated to Alexa 488 (1:500; cat. no.
R37114; Invitrogen; Thermo Fisher Scientific, Inc.) was added as
the secondary antibody and incubated for 1 h at room temperature.
Cells were counterstained with DAPI for 15 min at room temperature.
For the negative controls, cells were incubated in 5% donkey serum
at room temperature (cat. no. 017-000-121; Jackson ImmunoResearch
Laboratories, Inc.) instead of the primary antibody at 4°C
overnight. Fluorescent images were acquired using a Nikon
fluorescence microscope (magnification, ×20; Nikon
Corporation).
MTT assay
Cells were incubated with CellTiter96®
AQueous One Solution Reagent (Promega Corporation) at 37°C for 4 h
after being cultured on CG and cECM-CG scaffolds for 1, 3, 5, 7, 10
and 14 days. The absorbance at 490 nm was measured using the Biotek
Synergy HT Multi-Mode Microplate Reader (BioTek Instruments,
Inc.).
Cell differentiation analysis and
reverse transcription-quantitative PCR (RT-qPCR)
A comparative RT-qPCR analysis was performed for the
endothelial cell-associated genes CD31, von Willebrand factor (vWF)
and CD144. Primer sequences are presented in Table I. Cells seeded on the CG and cECM-CG
scaffolds were collected at day 21 and RNA was isolated using
Quick-RNA MicroPrep (Zymo Research Corp.). Extracted RNA
concentration was measured by spectrophotometry (NanoDrop 2000;
Thermo Fisher Scientific, Inc.), and 400 ng RNA was used for
first-strand cDNA synthesis (First-Strand cDNA Synthesis Kit;
Yeasen Technologies). Subsequently, RT-qPCR was performed using
SYBR (Hieff qPCR SYBR Green Master Mix, High Rox Plus; Yeasen
Technologies). The amplification reactions were performed with
initial denaturation at 95°C for 5 min, followed by 40 cycles of
two-step PCR at 95°C for 10 sec and 60°C for 30 sec. Primer
specificity was determined based on the melt curve analysis. The
housekeeping gene GAPDH was chosen for normalization. Fold change
expression was calculated using 2−ΔΔCq (33). n=3 for each condition.
 | Table I.Primers for reverse
transcription-quantitative PCR. |
Table I.
Primers for reverse
transcription-quantitative PCR.
| Gene | Primer sequence
(5′→3′) |
|---|
| GAPDH | F:
CTCATTTCCTGGTATGACAACGA |
|
| R:
CTTCCTCTTGTGCTCTTGCT |
| CD31 | F:
AACAGTGTTGACATGAAGAGCC |
|
| R:
TGTAAAACAGCACGTCATCCTT |
| vWF | F:
CCGATGCAGCCTTTTCGGA |
|
| R:
TCCCCAAGATACACGGAGAGG |
| CD144 | F:
AAGCGTGAGTCGCAAGAATG |
|
| R:
TCTCCAGGTTTTCGCCAGTG |
Immunofluorescence staining
To further identify the differentiation of the
CD34+ EPCs into endothelial cells, at day 21 cultured
cells were fixed in 4% paraformaldehyde for 15 min at room
temperature, permeabilized in 0.5% Triton X-100, followed by
blocking with 5% donkey serum (cat. no. 017-000-121; Jackson
ImmunoResearch Laboratories, Inc.) for 1 h at room temperature and
overnight incubation at 4°C with the following primary antibodies:
Mouse anti-CD31 (1:200; cat. no. ab24590; Abcam), rabbit anti-vWF
(1:200; cat. no. ab6994; Abcam). Then, secondary antibodies of
donkey anti-mouse Alexa594 (1:500; cat. no. A32744; Invitrogen;
Thermo Fisher Scientific, Inc.) and donkey anti-rabbit Alexa488
(1:500; cat. no. A-21206; Invitrogen; Thermo Fisher Scientific,
Inc.) were added to the samples and incubated for 1 h at room
temperature. Cell nucleus was counterstained using DAPI for 15 min
at room temperature. Fluorescence was observed using a fluorescence
microscope (magnification, ×40; Nikon Corporation).
In vitro tube formation assay
Tube formation assay was performed as described
previously (34). Human umbilical
vein endothelial cells (HUVECs; ScienCell Research Laboratories,
Inc.) were serum starved overnight at 37°C in 1640 medium (cat. no.
72400120; Thermo Fisher Scientific, Inc.) without FBS. Matrigel (BD
BioSciences) was thawed at 4°C overnight and added into the
pre-chilled 96-well plate using cooled pipette tips. Each well was
coated homogeneously with 50 µl Matrigel and incubated at 37°C with
5% CO2 for 1 h. Starved HUVECs were seeded at a density
of 2×104/well and cultured with a different conditioned
medium for 8 h at 37°C with 5% CO2. The conditioned
medium was collected from the CD34+ EPCs cultured on the
CG or cECM-CG scaffolds for 24 h in 1640 medium (cat. no. 72400120;
Gibco; Thermo Fisher Scientific, Inc.) without FBS. Images were
obtained using a phase-contrast light microscope (magnification,
×20; Olympus Corporation). Tube-forming capacity was quantified
based on the total length of capillary-like structures and the
total number of branch points. The experiment was repeated three
times, with duplicate measurements of each condition in each
experiment.
Statistical analysis
Statistical analyses were performed using SPSS 13.0
(SPSS Inc.) and GraphPad Prism 5.0 software (GraphPad Prism
Software, Inc.). Each experiment was repeated ≥3 times. Data are
presented as mean ± SEM. Student's t-test was used to analyze the
data. P<0.05 was considered to indicate a statistically
significant difference.
Results
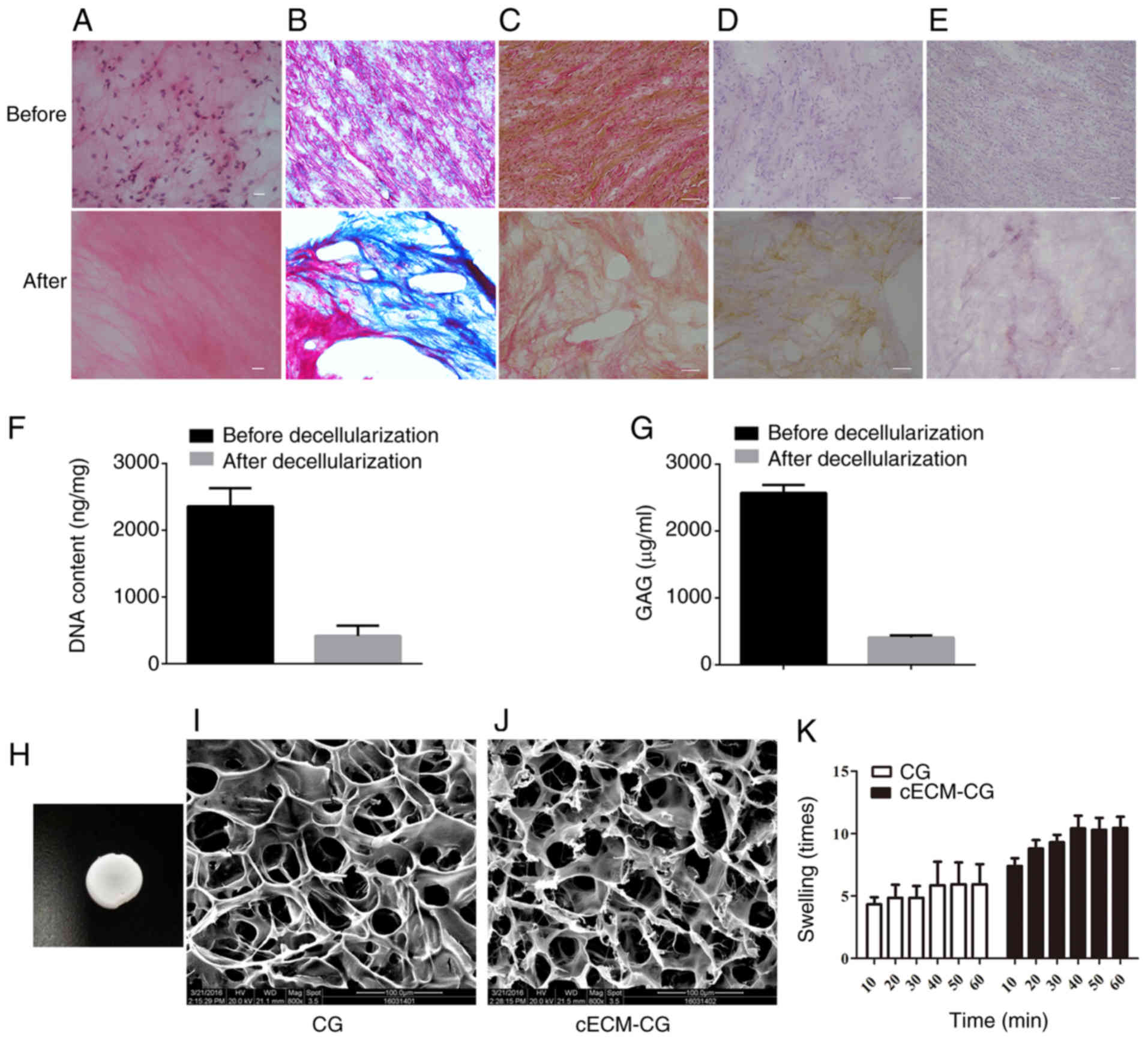
Preparation and characterization of
cECM and CG/cECM-CG scaffolds
To detect whether the decellularization process was
complete and the main ECM components were retained, histologic and
immunohistochemical analyses were performed. Histologic analysis
showed that most of the cells were removed and the main cECM
components were well preserved (Fig.
1A). Histology and immunohistochemistry analyses were used to
evaluate the constructs of the cECM before and after
decellularization (Fig. 1B-E). The
components of the structural protein collagen (Fig. 1B) and elastic fiber (Fig. 1C) and the adhesive protein
fibronectin (Fig. 1D) and laminin
(Fig. 1E) present in the cECM were
retained. DNA content analysis identified the complete
decellularization process and removal of cell immunogenicity
(Fig. 1F). Although the level of GAG
was significantly decreased after decellularization, ~18% of the
GAG could be preserved after decellularization (2.57±0.12 µg/mg
before decellularization vs. 0.41±0.03 µg/mg after
decellularization; Fig. 1G).
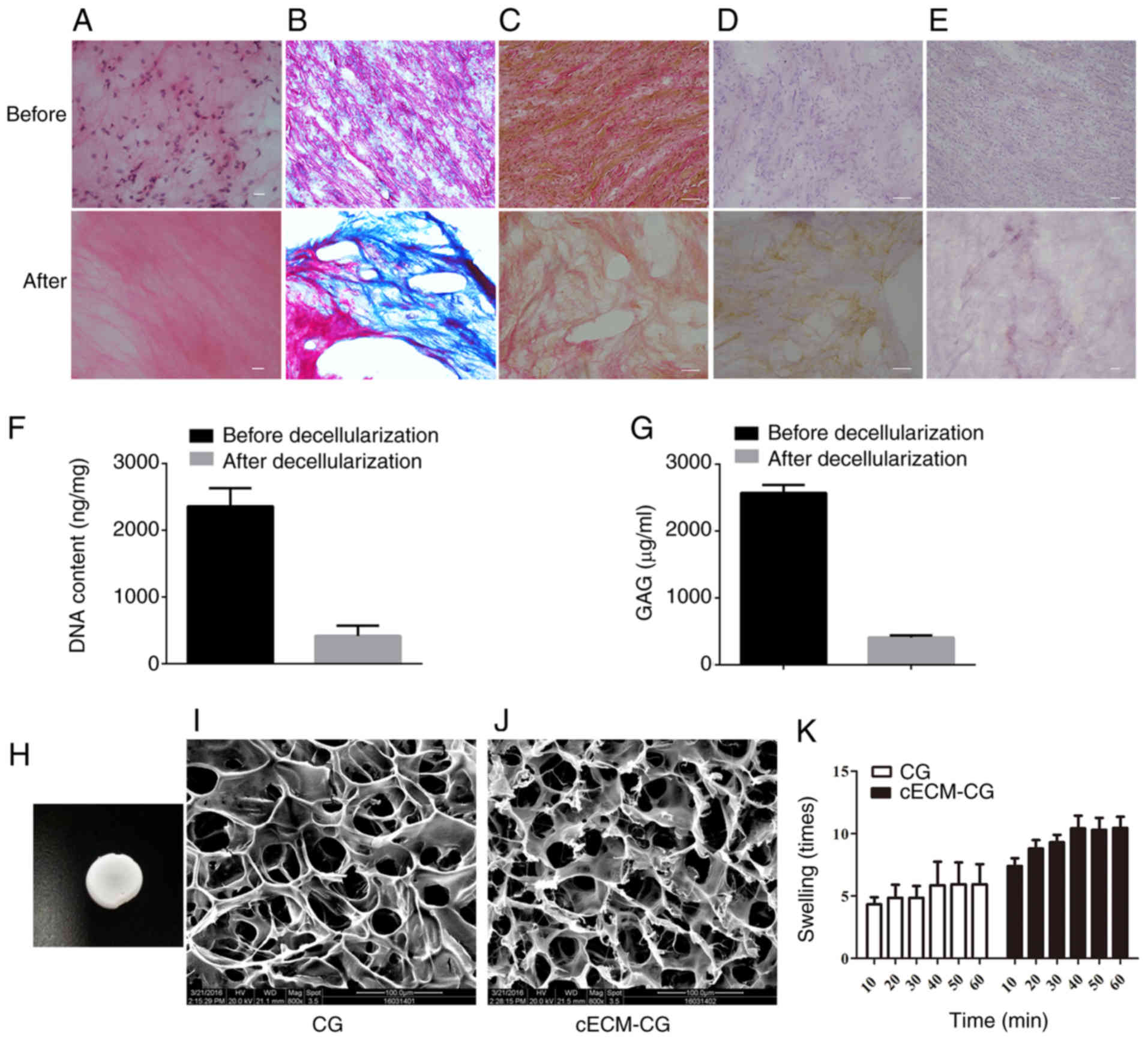 | Figure 1.Preparation and characterization of
cECM and CG/cECM-CG scaffolds. Comparison of cECM composition of
heart tissue before and after decellularization. (A) Hematoxylin
and eosin staining was performed to confirm complete
decellularization. Scale bar, 10 µm. (B) Masson staining was
performed for collagen fiber evaluation, collagen fibers were
stained blue. Scale bar, 50 µm. (C) Van Gieson staining was
performed for elastic fiber evaluation, elastic fibers were stained
yellow. Scale bar, 50 µm. Immunohistochemical staining of (D)
fibronectin and (E) laminin, fibronectin and laminin were stained
brown. Scale bar, 50 µm. (F) Statistical analysis of DNA content.
n=3 in each group. (G) Statistical analysis of GAG content of heart
tissue before and after decellularization. (H) Macrostructure of
the scaffold. SEM analysis of (I) CG and (J) cECM-CG composite
scaffolds. (K) Evaluation of the water absorption capacity of the
scaffolds. GAG, glycosaminoglycans; cECM, cardiac extracellular
matrix; CG, chitosan-gelatin; cECM-CG, cardiac extracellular
matrix-chitosan-gelatin. |
The gross appearance of the newly lyophilized
scaffolds was white and uniform (Fig.
1H). Microstructures of the scaffolds were assessed using
scanning electron microscopy; representative images are presented
in (Fig. 1I and J). Both scaffolds
presented uniform three-dimensional structures and similar pore
sizes of 40–100 µm, which is sufficient for cell ingrowth and
distribution on multiple layers (35).
Water absorption ability, defined by the swelling
ratio, was evaluated by comparing the dry and hydrated mass of CG
and cECM-CG composite scaffolds. Both scaffolds presented a similar
water uptake trend as both started swelling rapidly in the first 10
min, indicating good water absorption and retention capacity
(Fig. 1K). However, the cECM-CG
composite scaffold absorbed water 10 times its dry weight, whereas
the CG scaffold absorbed only about 5 times its dry weight. The
present results suggested that the addition of cECM may lead to
increased water absorption capacity.
cECM-CG composite scaffolds promote
survival and proliferation of CD34+ EPCs
Average purity of CD34+ EPCs isolated by
MACS was 98% (and <99.2%) based on flow cytometry (Fig. 2A and B). Moreover, cell viability
assay demonstrated the viability of CD34+ EPCs cultured
on the scaffolds at day 5. Cells growing on both CG and cECM-CG
composite scaffolds showed no dead cells, indicating that the
scaffolds were non-toxic (Fig.
2C).
 | Figure 2.Scaffold composited with cECM
improves cell survival and promotes proliferation of
CD34+ EPCs. (A) The population of the sorted cells. (B)
The purity of CD34+ EPCs after magnetic cell sorting
isolation. (C) Cell viability assay analyzed the viability of
CD34+ EPCs seeded on the scaffolds at day 5 by
fluorescence microscopy. Living cells were stained green by
calcein-AM. Dead cells were stained red by propidium iodide. Scale
bar, 20 µm. (D) Representative images of cell proliferation
assessed by Ki67 immunofluorescence staining at day 10. Positive
cells were stained green. Scale bar, 100 µm. (E) Proliferation was
analyzed by MTT assay on days 1, 3, 5, 7, 10 and 14. n=3 in each
group. (F) Percentage of Ki67 positive cells using
immunofluorescence staining was calculated by counting the positive
cells in three different and randomly chosen view fields.
**P<0.01 vs. CG. cECM, cardiac extracellular matrix; CG,
chitosan-gelatin; cECM-CG, cardiac extracellular
matrix-chitosan-gelatin; EPC, endothelial progenitor cells. |
Cells growing on the cECM-CG composite scaffold
showed a significant increase in Ki67 expression level compared
with those growing on the CG scaffold (Fig. 2D and F), which suggested that the
cECM-CG composite scaffold could promote proliferation of
CD34+ EPCs and had a better biocompatibility. Cell
proliferation was also investigated by MTT assay on days 1, 3, 5,
7, 10 and 14. The proliferation of the CD34+ EPCs
growing on the cECM-CG composite scaffold increased from day 1–14,
reaching the maximal level on day 10. At all the time points,
cECM-CG group exhibited a higher proliferation rate compared with
the CG group (Fig. 2E). Therefore,
the present results indicated that the cECM-CG scaffold promoted
proliferation of bone marrow-derived CD34+ EPCs.
cECM-CG composite scaffolds promote
differentiation of CD34+ EPCs
To investigate the differentiation capacity of
CD34+ EPCs seeded on the scaffolds, cells were cultured
on CG and cECM-CG composite scaffolds. After culturing for 21 days,
RT-qPCR was performed. The present results indicated that the mRNA
expression levels of CD31 (1.9±0.2-fold; P<0.05), vWF
(3.0±0.3-fold; P<0.01) and CD144 (9.8±0.1-fold; P<0.001) of
the CD34+ EPCs cultured on cECM-CG composite scaffold
was significantly higher compared with cells cultured on CG
scaffold (Fig. 3A). The
differentiation of CD34+ EPCs cultured on the scaffolds
was further investigated by immunofluorescence staining (Fig. 3D and E). At day 21, CD34+
EPCs cultured on cECM-CG scaffold showed a strong positive staining
for endothelial marker CD31 and vWF compared with cells on CG
scaffold. Differentiation rate of CD34+ EPCs cultured on
the cECM-CG scaffold was significantly higher compared with the CG
scaffold (Fig. 3B and C). The
present results suggested that CD34+ EPCs can
differentiate into endothelial cells and that the scaffold
composited with cECM could promote this differentiation
process.
 | Figure 3.In vitro differentiation of
CD34+ EPCs into endothelial cells cultured on CG and
cECM-CG composite scaffolds. (A) Reverse transcription-quantitative
PCR results showed that the CD34+ EPCs seeded on cECM-CG
scaffold upregulated the gene expression levels of EC markers
including CD31, vWF and CD144 on day 21, compared with cells seeded
on CG scaffold. Percentages of (B) CD31-positive and (C)
vWF-positive cells were calculated at day 21 in three different and
randomly chosen view fields. CD34+ EPCs on cECM-CG
scaffold showed a higher differentiation rate compared with CG. The
experiment was repeated three times. Representative images of
immunofluorescence staining of the expression levels of (D) CD31
and (E) vWF. Scale bar, 50 µm. *P<0.05, **P<0.01,
***P<0.001 vs. CG. cECM, cardiac extracellular matrix; CG,
chitosan-gelatin; cECM-CG, cardiac extracellular
matrix-chitosan-gelatin; EPC, endothelial progenitor cells; vWF,
von Willebrand factor. |
cECM-CG composite scaffold-based
conditioned medium increases tube formation of HUVECs
In addition to the direct differentiation of
CD34+ EPCs into endothelial cells, the present study
investigated whether the cECM-CG composite scaffold-based
conditioned medium could enhance endothelialization. The present
results indicated that cECM-CG composite scaffold-based conditioned
medium caused an increase in tube formation of HUVECs (Fig. 4A and B). Cells treated with a
conditioned medium harvested from CD34+ cells cultured
on cECM-CG composite scaffold showed an increasing number of branch
points (Fig. 4C). Furthermore, the
tube length of the cECM-CG composite scaffold group showed a
significant increase compared with the CG scaffold group (Fig. 4D). The present results indicated that
the cECM-CG composite scaffold seeded with CD34+ EPCs
could promote tube formation of the HUVECs.
Discussion
The present study constructed a three-dimensional
scaffold for tissue-engineered heart patch using human cECM,
chitosan and gelatin. In addition, the present study investigated
the characteristics and the endothelialization potential of the
scaffold seeded with CD34+ EPCs.
ECM, previously described as containing various
groups of molecules forming a microenvironment and providing
structural and biological support for cells, has been reported to
be associated with tissue remodeling and mechanical function
(3). The composition of the ECM
consists of a mixture of various molecules which form a
three-dimensional matrix (16). In
previous studies, some ECM components such as collagen and elastin,
were used for the construction of cardiac grafts to repair heart
defects (36,37). Other studies used natural materials,
such as chitosan and gelatin, for cardiac tissue engineering
(14,38). However, due to their relatively
simple composition, natural materials cannot fully mimic the
composition and complex structure of the ECM (15). Previous studies have attempted to use
decellularized ECM from different tissues, such as porcine-derived
cECM and intestinal submucosal or adipose-derived ECM, as a
scaffold for tissue engineering (18,24,39,40).
Removal of cells expressing surface antigens leads to a significant
reduction of immunogenicity (41).
However, most of the ECM materials are derived from non-cardiac
tissues or other species. Although ECM components are similar in
many tissues, each tissue has its own distinct combination of
molecules and has tissue-specific ECM architecture (42). Therefore, to the best of our
knowledge, the most suitable tissue is human-derived heart tissue
to develop a tissue-engineered heart patch for clinical use.
In the present study, specimens of discarded human
right atrial appendage were collected during heart surgery of
pediatric patients with CHD. These tissue samples can be obtained
regularly in hospitals and conveniently cryopreserved. Following
mixing the human cardiac-derived ECM with chitosan and gelatin, the
mixture was lyophilized and was used to develop a cECM-CG composite
scaffold for use as a tissue-engineered heart patch. The present
results indicated that the scaffold was a three-dimensional porous
scaffold that could promote cell survival and proliferation of
CD34+ EPCs. More importantly, the present results
suggested that the cECM-CG composite scaffold could promote the
differentiation of CD34+ EPCs, thus inducing the
endothelialization of the scaffold. Decellularization of tissues
involves a combination of physical, ionic, chemical and enzymatic
processes (43). Importantly the
decellularization agents should be tailored to different tissues. A
previous study showed that the use of 1% SDS, an ionic agent,
damaged the ECM components and negatively influenced their
mechanical property (44). The
present study decreased the concentration of SDS to 0.2%. The
present results indicated that the main components of the ECM, such
as the structural proteins collagen and elastic fiber and the
adhesive proteins fibronectin and laminin, were well maintained,
while most of the cells and DNA were removed after
decellularization. The present results suggested that the proteins
in the cECM, which mimicked the natural ECM structure and
environment, were well preserved and the potential immunogenicity
was mostly removed. Moreover, a scaffold should have a large
surface area and be highly porous to ensure cell adhesion and
transport of nutrients and metabolic wastes (45). The present cECM-CG composite scaffold
was porous with a uniform pore size of 40–100 µm. The present
scaffold had a strong water absorption capacity which may indicate
high cell adhesion and proliferation, as well as exchange of
substances between cells and the extracellular environment.
Therefore, the present results suggested the cECM-CG composite
scaffold could not only mimic the ECM environment but also
indicated advantageous physical properties of porosity and
efficient water absorption. Although human derived heart tissues
may be the most suitable tissue for the engineering of a heart
patch for clinical use, the heart tissues derived from humans were
not sufficient to be used for the construction of the scaffold
after decellularization. Therefore, the present study could not
achieve scaffold for patient-specific use.
Thrombosis is a significant limitation of current
grafts, and accumulating evidence shows that endothelial cells play
an essential role in preventing thrombosis by maintaining
endothelium integrity (46).
CD34+ cells were shown to be endothelial progenitor
cells with the capability to differentiate into endothelial cells,
thus participating in endothelialization (30). Previous studies have shown that
seeding of CD34+ cells on grafts enhances
endothelialization of the grafts (47). A previous study using a EPC
CD34+ capture stent coated with CD34 antibodies used for
congenital heart disease surgery demonstrated that the stent could
capture EPCs, thereby inhibiting thrombosis by promoting
endothelial formation (48). In the
present study, human bone marrow-derived CD34+ EPCs were
selected and seeded on CG and cECM-CG scaffolds. The present
results suggested that CD34+ EPCs cultured on cECM-CG
composite scaffold showed increased mRNA expression levels of
endothelial cell markers CD31, vWF and CD144 at day 21. CD144 is
often used as a marker to identify endothelial cells (49). Although freshly isolated bone
marrow-derived CD34+ endothelial progenitor cells can
also express a small amount of CD144, CD34+ endothelial
progenitor cells acquire higher expression of CD144 when
differentiating into endothelial cells. As shown in our previous
study, the expression ratio of CD144 in freshly isolated bone
marrow-derived CD34+ endothelial progenitor cells was
only 1% (49). In present
immunofluorescence staining and tube formation assay suggested that
the cECM-CG composite scaffold promoted the differentiation of
CD34+ EPCs and enhanced tube formation. The present
results indicated that the combination of CD34+ EPCs and
cECM-CG composite scaffold could facilitate endothelialization of
the scaffold. The achievement of endothelialization of grafts is
thought to be critically important for the prevention of graft
thrombosis (50). Future studies
should include testing of the characteristics of the present
scaffold in vivo, which could lead to further improvements
of the material.
In conclusion, the present results suggested that
the constructed cECM-CG composite scaffold provided advantageous
properties and promoted cell survival and proliferation.
Furthermore, seeding of CD34+ EPCs enhanced
endothelialization of the scaffold. The present results indicated
that the cECM-CG composite scaffold may potentially be used in
heart tissue engineering research.
Acknowledgements
Not applicable.
Funding
The present study was supported by Shanghai Hygiene
Science Research (grant no. 20134026), Shanghai Science and
Technology Commission (grant nos. 14411964900 and 16411962700) and
National Natural Science Foundation of China (grant no.
81670464).
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
HC and ZZ designed and supervised the experiments.
JL and WL performed the experiments. JL, GS, FZ, and XH analyzed
the data. JL wrote the article. All authors read and approved the
final manuscript.
Ethics approval and consent to
participate
All experiments were approved by the Ethics
Committee at Shanghai Children's Medical Center (approval no.
SCMCIRB-K2016025). Written informed consent from parents of
pediatric patients was obtained.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Benjamin EJ, Muntner P, Alonso A,
Bittencourt MS, Callaway CW, Carson AP, Chamberlain AM, Chang AR,
Cheng S, Das SR, et al: Heart disease and stroke statistics-2019
update: A report from the American heart association. Circulation.
139:e56–e528. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Tsilimigras DI, Oikonomou EK, Moris D,
Schizas D, Economopoulos KP and Mylonas KS: Stem cell therapy for
congenital heart disease: A systematic review. Circulation.
136:2373–2385. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Kochupura PV, Azeloglu EU, Kelly DJ,
Doronin SV, Badylak SF, Krukenkamp IB, Cohen IS and Gaudette GR:
Tissue-engineered myocardial patch derived from extracellular
matrix provides regional mechanical function. Circulation. 112
(Suppl 9):I144–I149. 2005.PubMed/NCBI
|
|
4
|
Mosala Nezhad Z, Poncelet A, Fervaille C
and Gianello P: Comparing the host reaction to CorMatrix and
different cardiac patch materials implanted subcutaneously in
Growing Pigs. Thoracic Cardiovasc Surg. 67:44–49. 2019. View Article : Google Scholar
|
|
5
|
Nishida H, Nakatsuka D, Kawano Y, Hiraiwa
N, Takanashi S and Tabata M: Outcomes of totally endoscopic atrial
septal defect closure using a glutaraldehyde-treated autologous
pericardial patch. Circ J. 81:689–693. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Lee C, Lim HG, Lee CH and Kim YJ: Effects
of glutaraldehyde concentration and fixation time on material
characteristics and calcification of bovine pericardium:
Implications for the optimal method of fixation of autologous
pericardium used for cardiovascular surgery. Interact Cardiovasc
Thorac Surg. 24:402–406. 2017.PubMed/NCBI
|
|
7
|
Rieder E, Steinacher-Nigisch A and Weigel
G: Human immune-cell response towards diverse xenogeneic and
allogeneic decellularized biomaterials. Int J Surg. 36:347–351.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Spadaccio C, Chello M, Trombetta M, Rainer
A, Toyoda Y and Genovese JA: Drug releasing systems in
cardiovascular tissue engineering. J Cell Mol Med. 13:422–439.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Anderson DEJ, Truong KP, Hagen MW, Yim EKF
and Hinds MT: Biomimetic modification of poly(vinyl alcohol):
Encouraging endothelialization and preventing thrombosis with
antiplatelet monotherapy. Acta Biomater. 86:291–299. 2019.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Shoji T and Shinoka T: Tissue engineered
vascular grafts for pediatric cardiac surgery. Transl Pediatr.
7:188–195. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Mantakaki A, Fakoya AOJ and Sharifpanah F:
Recent advances and challenges on application of tissue engineering
for treatment of congenital heart disease. PeerJ. 6:e58052018.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Afewerki S, Sheikhi A, Kannan S, Ahadian S
and Khademhosseini A: Gelatin-polysaccharide composite scaffolds
for 3D cell culture and tissue engineering: Towards natural
therapeutics. Bioeng Transl Med. 4:96–115. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Thein-Han WW, Saikhun J, Pholpramoo C,
Misra RD and Kitiyanant Y: Chitosan-gelatin scaffolds for tissue
engineering: Physico-chemical properties and biological response of
buffalo embryonic stem cells and transfectant of GFP-buffalo
embryonic stem cells. Acta Biomater. 5:3453–3466. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Pok S, Myers JD, Madihally SV and Jacot
JG: A multilayered scaffold of a chitosan and gelatin hydrogel
supported by a PCL core for cardiac tissue engineering. Acta
Biomater. 9:5630–5642. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Silva AC, Rodrigues SC, Caldeira J, Nunes
AM, Sampaio-Pinto V, Resende TP, Oliveira MJ, Barbosa MA,
Thorsteinsdóttir S, Nascimento DS and Pinto-do-Ó P:
Three-dimensional scaffolds of fetal decellularized hearts exhibit
enhanced potential to support cardiac cells in comparison to the
adult. Biomaterials. 104:52–64. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Yi S, Ding F, Gong L and Gu X:
Extracellular matrix scaffolds for tissue engineering and
regenerative medicine. Curr Stem Cell Res Ther. 12:233–246. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Scholl FG, Boucek MM, Chan KC, Valdes-Cruz
L and Perryman R: Preliminary experience with cardiac
reconstruction using decellularized porcine extracellular matrix
scaffold: Human applications in congenital heart disease. World J
Pediatr Congenit Heart Surg. 1:132–136. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Wang X, Yu T, Chen G, Zou J, Li J and Yan
J: Preparation and characterization of a
Chitosan/Gelatin/Extracellular Matrix Scaffold and its application
in tissue engineering. Tissue Eng Part C Methods. 23:169–179. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Tian Y and Liu Y: Preparation and
evaluation of extracellular matrix scaffold of human adipose
tissue. Zhonghua Zheng Xing Wai Ke Za Zhi. 33:129–135. 2017.(In
Chinese). PubMed/NCBI
|
|
20
|
Stoppel WL, Hu D, Domian IJ, Kaplan DL and
Black LD III: Anisotropic silk biomaterials containing cardiac
extracellular matrix for cardiac tissue engineering. Biomed Mater.
10:0341052015. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Shell DH IV, Croce MA, Cagiannos C,
Jernigan TW, Edwards N and Fabian TC: Comparison of
small-intestinal submucosa and expanded polytetrafluoroethylene as
a vascular conduit in the presence of gram-positive contamination.
Ann Surg. 241:995–1004. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Porzionato A, Stocco E, Barbon S, Grandi
F, Macchi V and De Caro R: Tissue-engineered grafts from human
decellularized extracellular matrices: A systematic review and
future perspectives. Int J Mol Sci. 19(pii): E41172018. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Chemla ES and Morsy M: Randomized clinical
trial comparing decellularized bovine ureter with expanded
polytetrafluoroethylene for vascular access. Br J Surg. 96:34–39.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Pok S, Benavides OM, Hallal P and Jacot
JG: Use of myocardial matrix in a chitosan-based full-thickness
heart patch. Tissue Eng Part A. 20:1877–1887. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Pok S, Stupin IV, Tsao C, Pautler RG, Gao
Y, Nieto RM, Tao ZW, Fraser CD Jr, Annapragada AV and Jacot JG:
Full-thickness heart repair with an engineered multilayered
myocardial patch in rat model. Adv Healthc Mater. 6:2017.doi:
10.1002/adhm.201600549. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Bunting S, Moncada S and Vane JR:
Antithrombotic properties of vascular endothelium. Lancet.
2:1075–1076. 1977. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Walter DH, Rittig K, Bahlmann FH,
Kirchmair R, Silver M, Murayama T, Nishimura H, Losordo DW, Asahara
T and Isner JM: Statin therapy accelerates reendothelialization: A
novel effect involving mobilization and incorporation of bone
marrow-derived endothelial progenitor cells. Circulation.
105:3017–3024. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Urbich C and Dimmeler S: Endothelial
progenitor cells: Characterization and role in vascular biology.
Circ Res. 95:343–353. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Werner N, Priller J, Laufs U, Endres M,
Böhm M, Dirnagl U and Nickenig G: Bone marrow-derived progenitor
cells modulate vascular reendothelialization and neointimal
formation: Effect of 3-hydroxy-3-methylglutaryl coenzyme a
reductase inhibition. Arterioscler Thromb Vasc Biol. 22:1567–1572.
2002. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Hirashima M, Kataoka H and Nishikawa S,
Matsuyoshi N and Nishikawa S: Maturation of embryonic stem cells
into endothelial cells in an in vitro model of vasculogenesis.
Blood. 93:1253–1263. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Aoki J, Serruys PW, van Beusekom H, Ong
AT, McFadden EP, Sianos G, van der Giessen WJ, Regar E, de Feyter
PJ, Davis HR, et al: Endothelial progenitor cell capture by stents
coated with antibody against CD34: The HEALING-FIM (healthy
endothelial accelerated lining inhibits neointimal growth-first in
man) registry. J Am Coll Cardiol. 45:1574–1579. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
French KM, Boopathy AV, DeQuach JA,
Chingozha L, Lu H, Christman KL and Davis ME: A naturally derived
cardiac extracellular matrix enhances cardiac progenitor cell
behavior in vitro. Acta Biomater. 8:4357–4364. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Livak KJ and Schmittgen TD: Analysis of
relative gene expression data using real-time quantitative PCR and
the 2(-Delta Delta C(T)) method. Methods. 25:402–408. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Olmer R, Engels L, Usman A, Menke S, Malik
MNH, Pessler F, Göhring G, Bornhorst D, Bolten S,
Abdelilah-Seyfried S, et al: Differentiation of human pluripotent
stem cells into functional endothelial cells in scalable suspension
culture. Stem Cell Reports. 10:1657–1672. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Zhang Y, Fan W, Ma Z, Wu C, Fang W, Liu G
and Xiao Y: The effects of pore architecture in silk fibroin
scaffolds on the growth and differentiation of mesenchymal stem
cells expressing BMP7. Acta Biomater. 6:3021–3028. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Miyagi Y, Chiu LL, Cimini M, Weisel RD,
Radisic M and Li RK: Biodegradable collagen patch with covalently
immobilized VEGF for myocardial repair. Biomaterials. 32:1280–1290.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Shi C, Li Q, Zhao Y, Chen W, Chen B, Xiao
Z, Lin H, Nie L, Wang D and Dai J: Stem-cell-capturing collagen
scaffold promotes cardiac tissue regeneration. Biomaterials.
32:2508–2515. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Fu JH, Zhao M, Lin YR, Tian XD, Wang YD,
Wang ZX and Wang LX: Degradable chitosan-collagen composites seeded
with cells as tissue engineered heart valves. Heart Lung Circ.
26:94–100. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Ropcke DM, Ilkjaer C, Tjornild MJ, Skov
SN, Ringgaard S, Hjortdal VE and Nielsen SL: Small intestinal
submucosa tricuspid valve tube graft shows growth potential,
remodelling and physiological valve function in a porcine model†.
Interact Cardiovasc Thorac Surg. 24:918–924. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Efraim Y, Sarig H, Cohen Anavy N, Sarig U,
de Berardinis E, Chaw SY, Krishnamoorthi M, Kalifa J, Bogireddi H,
Duc TV, et al: Biohybrid cardiac ECM-based hydrogels improve long
term cardiac function post myocardial infarction. Acta Biomater.
50:220–233. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Meyer SR, Nagendran J, Desai LS, Rayat GR,
Churchill TA, Anderson CC, Rajotte RV, Lakey JR and Ross DB:
Decellularization reduces the immune response to aortic valve
allografts in the rat. J Thorac Cardiovasc Surg. 130:469–476. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Padhi A and Nain AS: ECM in
differentiation: A review of matrix structure, composition and
mechanical properties. Ann Biomed Eng. Sep 4–2019.doi:
10.1007/s10439-019-02337-7 (Epub ahead of print). View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Brown BN and Badylak SF: Extracellular
matrix as an inductive scaffold for functional tissue
reconstruction. Transl Res. 163:268–285. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Mancuso L, Gualerzi A, Boschetti F, Loy F
and Cao G: Decellularized ovine arteries as small-diameter vascular
grafts. Biomed Mater. 9:0450112014. View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Hutmacher DW: Scaffolds in tissue
engineering bone and cartilage. Biomaterials. 21:2529–2543. 2000.
View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Vane JR and Botting RM:
Endothelium-thromboresistance. Wien Klin Wochenschr. 103:403–404.
1991.PubMed/NCBI
|
|
47
|
Bhattacharya V, McSweeney PA, Shi Q, Bruno
B, Ishida A, Nash R, Storb RF, Sauvage LR, Hammond WP and Wu MH:
Enhanced endothelialization and microvessel formation in polyester
grafts seeded with CD34(+) bone marrow cells. Blood. 95:581–585.
2000. View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Cabanelas N, Martins JD and Pinto F:
Initial use of endothelial progenitor cells capturing stents in
paediatric congenital heart disease. Cardiol Young. 24:900–904.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Gao LP, Du MJ, Lv JJ, Schmull S, Huang RT
and Li J: Use of human aortic extracellular matrix as a scaffold
for construction of a patient-specific tissue engineered vascular
patch. Biomed Mater. 12:0650062017. View Article : Google Scholar : PubMed/NCBI
|
|
50
|
Melchiorri AJ, Hibino N and Fisher JP:
Strategies and techniques to enhance the in situ endothelialization
of small-diameter biodegradable polymeric vascular grafts. Tissue
Eng Part B Rev. 19:292–307. 2013. View Article : Google Scholar : PubMed/NCBI
|