Introduction
Hip replacement is a large-scale complex orthopedic
operation requiring long operation time. It is mainly applicable to
some fractures (such as femoral neck fracture), osteoarthritis,
bone neoplasms, ankylosis or hip dysplasia, and others. As one of
the most effective methods for joint correction, hip replacement is
mainly to relieve hip joint pain, correct deformity, restore and to
improve hip joint movement function (1–3). It uses
prostheses similar to human bone joints made of metal materials
with good biocompatibility and mechanical properties to replace
joint surfaces damaged by diseases or injuries through surgical
methods (4–6). However, hip replacement brings a high
risk of lower limb deep venous thrombosis, and lower limb deep
venous thrombosis is a common complication, which not only affects
the efficacy of hip replacement, but also greatly affects the
recovery of patients, and even leads to death under serious
situations (7,8).
CXC ligand 13 (CXCL13) is a main factor for
recruiting B cells in neuro-inflammatory reaction. In various
inflammatory diseases, a large number of monocytes aggregate, and
chemokine CXCL13 is expressed in a large amount locally, further
leading to inflammatory cascade reaction and local tissue or organ
damage (9–11). IL-6, as a very important part of
interleukins, and participates in many inflammatory reactions and
diseases in human body (12,13). CXCL13 and IL-6 are both important
pro-inflammatory factors (10,13).
Research shows that the coagulation promoting effect of
inflammation and vicious circle caused by the interaction of
coagulation-inflammation network have become important pathogenesis
of thrombosis (14,15).
Therefore, this study compared the patients
suffering from lower limb vein thrombus after hip replacement to
those not suffering from it after hip replacement in terms of serum
CXCL13 and IL-6 levels, and the serum CXCL13 and IL-6 levels were
considered as biological indexes for early prediction of lower limb
vein thrombus, so as to provide reference in clinical practice.
This study also analyzed independent risk factors affecting hip
replacement, so as to provide reference for protection to patients
undergoing hip replacement.
Patients and methods
Clinical data of patients
A total of 128 patients undergoing hip replacement
in The First Affiliated Hospital of Guizhou University of
Traditional Chinese Medicine (Guiyang, China) from May 2016 to May
2018, were divided into group A (n=68) and group B (n=60). Group A
consisted of 35 males and 33 females, with an average age of
50.7±7.5 years, and group B consisted of 35 males and 25 females,
with an average age of 50.1±6.8 years. There were no statistical
differences in sex and age between the two groups (both
P>0.05).
The study was approved by the Medical Ethics
Committee of the Hospital and each patient signed an informed
consent form after understanding the requirements of the study.
Inclusion and exclusion criteria
The inclusion criteria were as follows: Patients
confirmed with osteoarthritis based on imaging who received hip
replacement, patients meeting the diagnostic criteria of Guidance
for the Diagnosis and Treatment of Osteoarthritis (2018) (16), patients with all the required
clinical data, and patients willing to cooperate with the treatment
and follow-up.
Exclusion criteria were as follows: Patients with
congenital immunodeficiency, patients with severe infectious
diseases or inflammatory disease, patients with other malignant
tumors, patients with hepatic or kidney function obstacle, patients
with expected survival time less than 3 months, and pregnant or
lactating women.
Instruments and reagents
Human IL-6 ELISA kit and human CXCL13 ELISA kit
(Shanghai Enzyme-linked Biotechnology Co., Ltd., PI330 and
ml057504); blood analyzer (Japan SYSMEX, XS-800i), and supporting
reagents for testing blood routine indexes; enzyme-linked
immuno-sorbent assay (ELISA) test kit (Wuhan Elabscience
Biotechnology Co., Ltd., E-EL-H0102c).
Sample collection and ELISA detection
methods
Venous blood (5 ml) was sampled from patients in
group A and B, allowed to stand for 30 min, and centrifuged at
1,000–2,000 × g and 4°C for 10 min after the whole blood was
naturally coagulated and serum was separated to obtain the
supernatant. ELISA was used to detect the expression of serum
chemokine CXCL13 and IL-6. A blank well, a standard well and a
sample well were set, respectively. Standards with a concentration
of 0 were added into the blank well, and 50 µl of standards with
different concentrations were added into the standard well. The
well for samples to be determined was added with 10 µl of the
samples, and 40 µl of sample diluent. The blank well was not added
with sample diluent. Each well was added with 100 µl of horseradish
peroxidase (HRP)-labeled detection antibody except the blank well.
The reaction wells were blocked with a microplate sealer, and
incubated in a water bath at 37°C for 65 min. The liquid in each
well was discarded, and each well was patted to dry with absorbent
paper, filled with washing solution, and allowed to stand for 2
min. After 2 min, the washing solution was shaken off, and each
well was patted dry with absorbent paper. After 6 repeats of the
above steps, each well was added with 50 µl of substrate A and 50
µl of substrate B, and incubated at 37°C in the dark for 10 min.
Each well was added with 50 µl of stop solution, and within 15 min
after the addition, the optical density (OD) of each well was
measured at 450 nm wavelength and the concentration was
calculated.
Observation indexes
Primary observation indexes: The serum chemokine
CXCL13 and IL-6 in group A were compared with those in group B, and
receiver operating characteristic (ROC) curves of serum chemokine
CXCL13 and IL-6 in predicting lower limb vein thrombus after hip
replacement were drawn.
Secondary observation indexes: The Pearson's
correlation coefficient was used to analyze the correlation between
serum chemokine CXCL13 and serum IL-6, and logistic regression
analysis was employed to analyze risk factors affecting hip
replacement.
Statistical analysis
In the present study, the collected data were
analyzed statistically using SPSS20.0 software package, and
visualized into required figures using GraphPad 7 software package.
General data of the patients were analyzed using the chi-square
test, and biological indexes were analyzed using the t-test. The
data in normal distribution were expressed by the mean ± standard
deviation (SD), and comparison between groups was carried out by
the independent-samples t-test. Data not in normal distribution
were expressed by the quartile [Mean (P25-P75)], and ROC curves of
serum chemokine CXCL13 and IL-6 for predicting lower limb vein
thrombus after hip replacement were drawn. P<0.05 indicates a
statistically significant difference. Pearson's correlation
coefficient was used to analyze the correlation between serum
chemokine CXCL13 and IL-6, and logistic regression analysis to
analyze the risk factors affecting the efficacy of hip
replacement.
Results
General data of patients
There were significant differences between the two
groups in age, body mass index (BMI), diabetes history,
hypertension history, and hyperlipidemia history (all P<0.05),
but there were no significant differences between them in sex,
smoking history, drinking history, and place of residence (all
P>0.05) (Table I).
 | Table I.General data of the patients. |
Table I.
General data of the patients.
| Variables | Group A (n=68) | Group B (n=60) | χ2 | P-value |
|---|
| Sex |
| Male | 35 (51.47) | 35 (58.33) | 0.606 | 0.436 |
|
Female | 33 (48.53) | 25 (41.67) |
|
|
| Age (years) |
|
|
|
|
|
<30 | 28 (47.18) | 36 (60.00) | 4.518 | 0.034 |
| ≥30 | 40 (58.82) | 24 (40.00) |
|
|
| BMI
(kg/m2) |
|
|
|
|
| ≥22 | 41 (60.29) | 21 (35.00) | 8.165 | 0.004 |
|
<22 | 27 (39.71) | 39 (65.00) |
|
|
| Smoking |
|
|
|
|
| Yes | 33 (48.53) | 26 (43.33) | 2.170 | 0.141 |
| No | 35 (51.47) | 34 (56.67) |
|
|
| Drinking |
|
|
|
|
| Yes | 38 (55.88) | 34 (56.67) | 0.008 | 0.929 |
| No | 30 (44.12) | 26 (43.33) |
|
|
| Diabetes |
|
|
|
|
| Yes | 40 (58.82) | 24 (40.00) | 4.518 | 0.034 |
| No | 28 (47.18) | 36 (60.00) |
|
|
| Hypertension |
|
|
|
|
| Yes | 41 (60.29) | 22 (36.67) | 7.120 | 0.008 |
| No | 27 (39.71) | 38 (63.33) |
|
|
| Hyperlipidemia |
|
|
|
|
| Yes | 38 (55.88) | 19 (31.67) | 7.567 | 0.006 |
| No | 30 (41.12) | 41 (61.33) |
|
|
| Place of
residence |
|
|
|
|
| Urban
area | 29 (42.65) | 23 (38.33) | 0.246 | 0.621 |
| Rural
area | 39 (57.35) | 37 (61.67) |
|
|
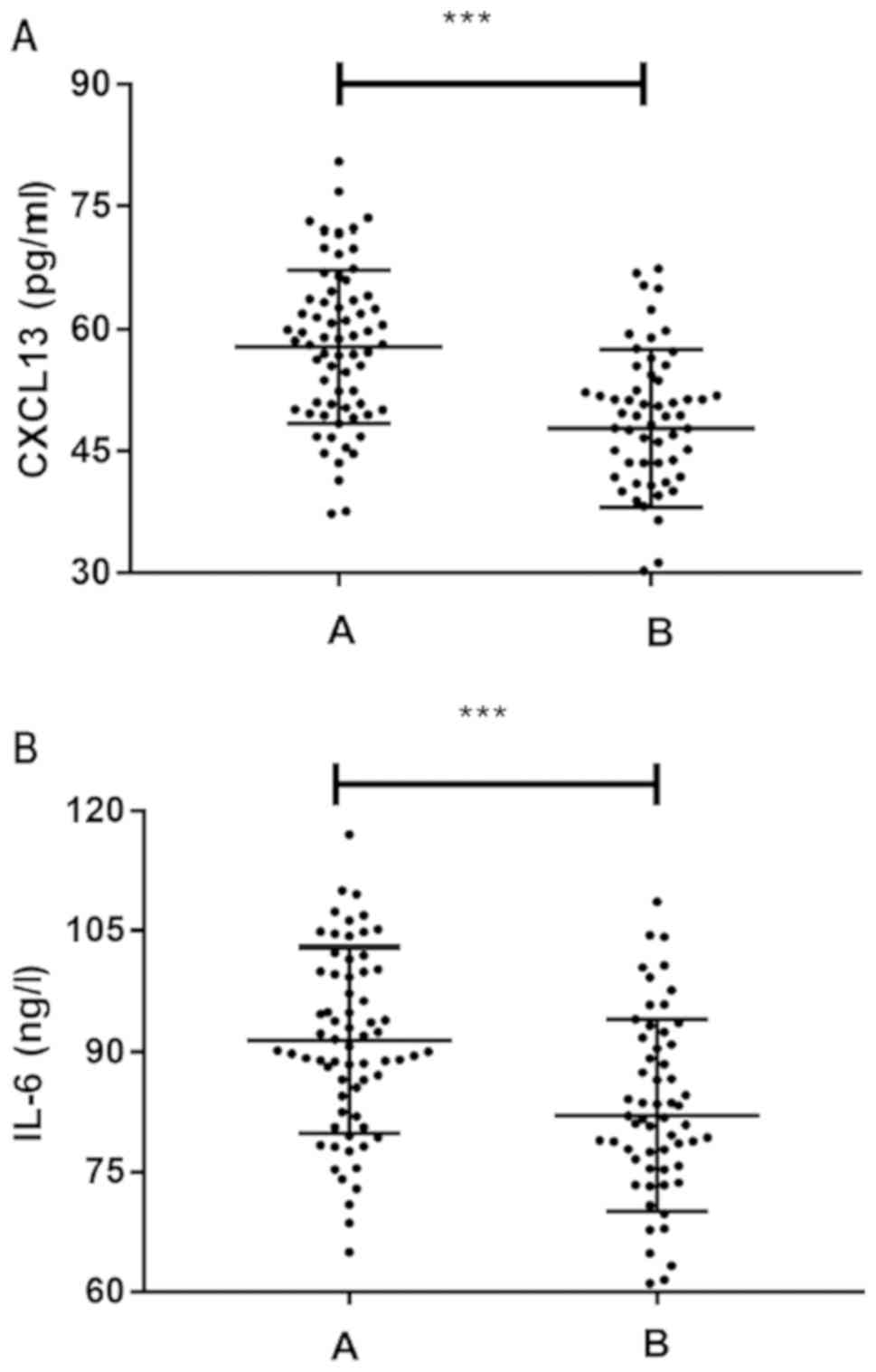
Expression of CXCL13 and IL-6 in group
A and B
Comparison between group A and B in CXCL13 and IL-6
levels revealed that group A showed significantly higher CXCL13 and
IL-6 levels than B (both P<0.05) (Fig. 1).
ROC curves of CXCL13 and IL-6 levels
in predicting lower limb vein thrombus after surgery
The levels of CXCL13 and IL-6 in group A were
compared with those in group B, and ROC curves of CXCL13 and IL-6
levels in predicting lower limb vein thrombus after hip replacement
were drawn (Fig. 2 and Table II).
 | Table II.Predictive value of CXCL13 and IL-6
levels in lower limb vein thrombus after hip replacement. |
Table II.
Predictive value of CXCL13 and IL-6
levels in lower limb vein thrombus after hip replacement.
| Index | AUC | 95% CI | Specificity % | Sensitivity % | Youden index % | Cut-off |
|---|
| CXCL13 | 0.763 | 67.67~89.22 | 61.76 | 80.00 | 43.24 | 55.491 |
| IL-6 | 0.710 | 53.31~78.31 | 70.59 | 66.67 | 38.73 | 86.557 |
Analysis on the correlation between
serum CXCL13 and serum IL-6 in the patients
Based on the comparison between the two groups in
CXCL13 and IL-6 levels, the Pearson's correlation coefficient was
employed to analyze the correlation between the two factors, and it
was found that they were positively correlated (Fig. 3).
Risk factors affecting efficacy
The results in Table
I show that the age of the patients, BMI, diabetes history,
hyperlipidemia history, and hypertension history were independent
factors affecting hip replacement, and our study results revealed
that the CXCL13 and IL-6 levels in the patients were also
independent factors affecting hip replacement. Therefore, we
adopted the logistic regression analysis to analyze the risk
factors for hip replacement by taking age, BMI, diabetes history,
hyperlipidemia history, hypertension history, CXCL13 level and IL-6
level as covariates. Assignment was carried out on independent
factors based on the original data (Table III). The final results showed that
age, BMI, diabetes history, hyperlipidemia history, hypertension
history, CXCL13 level, and IL-6 level were independent risk factors
affecting the efficacy of hip replacement (all P<0.05) (Table IV).
 | Table III.Assignments. |
Table III.
Assignments.
| Factors | Assignment |
|---|
| Age (years) | <30=0,
≥30=1 |
| BMI
(kg/m2) | <22=0,
≥22=1 |
| CXC13 (pg/ml) | <50.92=0,
≥50.92=1 |
| IL-6 (ng/l) | <88.15=0,
≥88.15=1 |
| Diabetes
history | Yes=0, No=1 |
| Hyperlipidemia
history | Yes=0, No=1 |
| Hypertension
history | Yes=0, No=1 |
| Lower limb vein
thrombus | Yes=0, No=1 |
 | Table IV.Risk factors for efficacy of hip
replacement. |
Table IV.
Risk factors for efficacy of hip
replacement.
|
|
|
|
|
|
| 95% CI of EXP
(B) |
|---|
|
|
|
|
|
|
|
|
|---|
| Factors | B | SD | Wals | Sig. | Exp (B) | Lower limit | Upper limit |
|---|
| Age | 2.122 | 0.515 | 16.961 | 0.009 | 8.345 | 3.04 | 22.904 |
| BMI | 1.65 | 0.503 | 10.765 | 0.015 | 5.207 | 1.943 | 13.951 |
| CXC13 | 1.353 | 0.485 | 7.785 | 0.005 | 3.867 | 1.496 | 10.001 |
| IL-6 | 0.848 | 0.471 | 3.245 | 0.008 | 2.335 | 0.928 | 5.873 |
| Diabetes
history | 0.201 | 0.478 | 0.177 | 0.032 | 1.223 | 0.479 | 3.121 |
| Hypertension
history | 0.804 | 0.498 | 2.605 | 0.034 | 2.233 | 0.842 | 5.926 |
| Hyperlipidemia
history | 0.56 | 0.489 | 1.313 | 0.025 | 1.751 | 0.672 | 4.562 |
Discussion
With the development of global aging, joint diseases
such as various osteoarthritis, bone fractures, and femoral head
necrosis become an important health problem (17,18), and
with the improvement of medical level, hip replacement has become a
reliable treatment (19). Hip
replacement is a mature and reliable treatment method, which fixes
artificial prosthesis, including femoral and acetabular parts, on
normal bones with bone cement and screws to replace diseased joints
and rebuild the normal function of hip joint of patients. It has
the following advantages: Contributing to good joint motion and
early off-bed activity, and reducing long-term bedridden
complications of elderly patients (20,21).
However, it has the characteristics of high difficulty and high
risk. Lower limb vein thrombus after hip replacement is the most
common complication affecting its efficacy and prognosis, and is a
crucial factor. It may cause partial or complete loss of limb
function and disability, and may even cause pulmonary embolism and
endanger life under serious situations (22). Predicting the risk of lower limb vein
thrombus after hip replacement in advance and taking appropriate
protective measures in time are the main methods to reduce lower
limb vein thrombus. Finding sensitive biological indexes is also
the focus of clinical research (23,24).
In this study, comparison between group A and B in
serum CXCL13 and IL-6 levels revealed that group A showed
significantly higher CXCL13 and IL-6 levels than group B (both
P<0.001). Some studies have concluded that serum CXCL13 and IL-6
are important pro-inflammatory factors, and involved in occurrence
and development of inflammatory reactions (10,13) and
the development of inflammation often induces thrombus, which is
one of the mechanisms of thrombosis (14). Wang et al (25) compared the levels of inflammation
markers and coagulation factors in 59 patients with lower limb vein
thrombus and those in 26 patients without it, finding that
inflammatory reaction and coagulation factors interact with each
other to promote coagulation. The development of inflammatory
activities often leads to the increase of coagulation factors.
Therefore, inflammatory reaction is closely related to lower limb
venous thrombosis and is one of its mechanisms. Based on the
present study, we deduced that inflammatory response was one of the
mechanisms involved in lower limb vein thrombus after hip
replacement, so patients with lower limb vein thrombus after hip
replacement would show significantly higher serum CXCL13 and IL-6
levels than those without lower limb vein thrombus after
surgery.
The sensitivity and specificity were also compared
of separate serum CXCL13 level or serum IL-6 level and those of
combined serum CXCL13 level and serum IL-6 level in diagnosing
lower limb vein thrombus after hip replacement, finding that serum
CXCL13 and IL-6 levels have certain value in diagnosis after hip
replacement. Serum CXCL13 and IL-6 are important pro-inflammatory
factors (10,13) and inflammatory activity is one of the
important mechanisms of thrombosis (14). Based on this study, it was concluded
that serum CXCL13 and IL-6 can be used as biological indicators to
diagnose lower limb vein thrombus after hip replacement. Logistic
regression analysis revealed that patients' age, BMI, diabetes
history, hyperlipidemia history, hypertension history, CXCL13
level, and IL-6 level were independent risk factors affecting the
efficacy of hip replacement. Therefore, for patients who are older
or have a relatively high BMI index, diabetes history,
hyperlipidemia history or hypertension history, more protective
measures should be given to prevent lower limb vein thrombus after
surgery. For example, asking the patients turn over regularly and
take appropriate activities, observing their lower limb status, and
strengthening nursing work. Moreover, corresponding protective
measures could be taken in advance to prevent lower limb vein
thrombus based on detected serum CXCL13 and IL-6 levels in patients
after surgery.
In conclusion, the levels of CXCL13 and IL-6 in the
serum of patients with lower limb venous thrombosis after hip
replacement significantly increased, which can be used as
biological indicators for early prediction of lower limb venous
thrombosis after hip replacement.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
ZG wrote the manuscript and designed the study. ZG
approved the final manuscript.
Ethics approval and consent to
participate
The study was approved by the Ethics Committee of
The First Affiliated Hospital of Guizhou University of Traditional
Chinese Medicine (Guiyang, China). Patients who participated in
this study, signed the informed consent and had complete clinical
data.
Patient consent for publication
Not applicable.
Conflict of interest
The author declares that there are no competing
interests.
References
|
1
|
Learmonth ID, Young C and Rorabeck C: The
operation of the century: Total hip replacement. Lancet.
370:1508–1519. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Galia CR, Diesel CV, Guimarães MR and
Ribeiro TA: Total hip arthroplasty: A still evolving technique. Rev
Bras Ortop. 52:521–527. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Zagra L: Advances in hip arthroplasty
surgery: What is justified? EFORT Open Rev. 2:171–178. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Pivec R, Johnson AJ, Mears SC and Mont MA:
Hip arthroplasty. Lancet. 380:1768–1777. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Knight SR, Aujla R and Biswas SP: Total
Hip Arthroplasty - over 100 years of operative history. Orthop Rev
(Pavia). 3:e162011.doi: 10.4081/or.2011.e16. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Rogers BA, Garbedian S, Kuchinad RA,
Backstein D, Safir O and Gross AE: Total hip arthroplasty for adult
hip dysplasia. J Bone Joint Surg Am. 94:1809–1821. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Nam D, Nunley RM, Johnson SR, Keeney JA,
Clohisy JC and Barrack RL: The effectiveness of a risk
stratification protocol for thromboembolism prophylaxis after hip
and knee arthroplasty. J Arthroplasty. 31:1299–1306. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Fukushima K, Takahira N, Uchiyama K,
Moriya M, Minato T and Takaso M: The incidence of deep vein
thrombosis (DVT) during hip arthroscopic surgery. Arch Orthop
Trauma Surg. 136:1431–1435. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Han BK, Kuzin I, Gaughan JP, Olsen NJ and
Bottaro A: Baseline CXCL10 and CXCL13 levels are predictive
biomarkers for tumor necrosis factor inhibitor therapy in patients
with moderate to severe rheumatoid arthritis: A pilot, prospective
study. Arthritis Res Ther. 18:932016. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Allam SI, Sallam RA, Elghannam DM and
El-Ghaweet AI: Clinical significance of serum B cell chemokine
(CXCL13) in early rheumatoid arthritis patients. Egypt Rheumatol.
41:11–14. 2019. View Article : Google Scholar
|
|
11
|
Irani DN: Regulated production of CXCL13
within the central nervous system. J Clin Cell Immunol. 7:72016.
View Article : Google Scholar
|
|
12
|
Sapan HB, Paturusi I, Jusuf I, Patellongi
I, Massi MN, Pusponegoro AD, Arief SK, Labeda I, Islam AA, Rendy L,
et al: Pattern of cytokine (IL-6 and IL-10) level as inflammation
and anti-inflammation mediator of multiple organ dysfunction
syndrome (MODS) in polytrauma. Int J Burns Trauma. 6:37–43.
2016.PubMed/NCBI
|
|
13
|
Rose-John S: The soluble interleukin 6
receptor: Advanced therapeutic options in inflammation. Clin
Pharmacol Ther. 102:591–598. 2017. View
Article : Google Scholar : PubMed/NCBI
|
|
14
|
Iba T and Levy JH: Inflammation and
thrombosis: Roles of neutrophils, platelets and endothelial cells
and their interactions in thrombus formation during sepsis. J
Thromb Haemost. 16:231–241. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Lankeit M and Held M: Incidence of venous
thromboembolism in COPD: Linking inflammation and thrombosis? Eur
Respir J. 47:369–373. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Wang J, Yang L, Li Q, Wu Z, Sun Y, Zou Q,
Li X, Xu Z and Ye C: Construction of an adherence rating scale for
exercise therapy for patients with knee osteoarthritis. BMC
Musculoskelet Disord. 19:2632018. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Rahmati M, Nalesso G, Mobasheri A and
Mozafari M: Aging and osteoarthritis: Central role of the
extracellular matrix. Ageing Res Rev. 40:20–30. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Li YS, Xiao WF and Luo W: Cellular aging
towards osteoarthritis. Mech Ageing Dev. 162:80–84. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Gademan MG, Hofstede SN, Vliet Vlieland
TP, Nelissen RG and Marang-van de Mheen PJ: Indication criteria for
total hip or knee arthroplasty in osteoarthritis: A
state-of-the-science overview. BMC Musculoskelet Disord.
17:4632016. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Liu XW, Zi Y, Xiang LB and Wang Y: Total
hip arthroplasty: A review of advances, advantages and limitations.
Int J Clin Exp Med. 8:27–36. 2015.PubMed/NCBI
|
|
21
|
Burnett RSJ and Abos D: Total hip
arthroplasty: Techniques and results. BC Med J. 52:455–464.
2010.
|
|
22
|
Jameson SS, Bottle A, Malviya A, Muller SD
and Reed MR: The impact of national guidelines for the prophylaxis
of venous thromboembolism on the complications of arthroplasty of
the lower limb. J Bone Joint Surg Br. 92:123–129. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Shimoyama Y, Sawai T, Tatsumi S, Nakahira
J, Oka M, Nakajima M, Jotoku T and Minami T: Perioperative risk
factors for deep vein thrombosis after total hip arthroplasty or
total knee arthroplasty. J Clin Anesth. 24:531–536. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Fisher WD: Impact of venous
thromboembolism on clinical management and therapy after hip and
knee arthroplasty. Can J Surg. 54:344–351. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Wang MF, Yang LH, Yang XL, Zhang RJ, Hou
LH and Liu XE: Correlation of inflammatory marker and coagulation
factors with deep vein thrombosis. Zhongguo Shi Yan Xue Ye Xue Za
Zhi. 18:753–756. 2010.(In Chinese). PubMed/NCBI
|