Introduction
Pulmonary hypertension (PH) is defined as a disease
or pathophysiological syndrome featured by increased pulmonary
pressure: Mean pulmonary artery pressure ≥25 mmHg measured by right
heart catheterization (RHC) at rest (1). Usually, PH is insidiously progressive
and clinically manifests as dyspnea, fatigue, chest pain, loss of
weight, edema, weakness, palpitation and syncope, having a strong
impact on patients' activities of daily life. The complex
pathogenesis, limited treatment and no cure impose a psychological
as well as economic burden on the patients.
According to pathology, hemodynamics, clinical
diagnosis and treatment, PH is classified into five groups
(1): Group I, pulmonary arterial
hypertension (PAH); group II, PH due to left heart disease; group
III, PH due to lung diseases and/or hypoxia; group IV, CTEPH and
group V, PH with unclear multifactorial mechanisms. Evidence
suggested that quality of life (QoL) is closely associated with
age, gender, level of education, economic situation and supportive
system (health care system and social society) (2,3).
Symptoms, inflammatory cytokines, limitation of function, exercise
capacity [6-minute walking distance (6MWD)], side effects of
treatment, other chronic underlying diseases, the classification of
PH and functional class of the patients were closely correlated
with their health-associated QoL (2,4-7).
In addition, as with other chronic diseases, the
uncertainty of treatment and limitation of activity in patients
with PH frequently lead to anxiety and depression. One
cross-sectional study indicated that 50.6% of the patients had
depression, among which 19.2% of patients presented with severe
depression, 14.8% had panic disorders and 7.1% had phobias. In
patients with severe psychological problems, the QoL was obviously
impaired (8). The reported mental
disorders in patients with PH increased from 17.7% in New York
Health Association (NYHA) class I to 61.9% in NYHA class IV
(9). A study by Harzheim et
al (10) revealed that scores in
all aspects of SF-36 in patients with PH with severe mental
disorders decreased and the severity of depression and anxiety had
an apparent negative correlation with scores of QoL (P<0.05); in
all dimensions of QoL, anxiety and depression appeared to be
independent influencing factors (11).
With the improvement of modern medicine, the
evaluation of prognosis should not only include objective
parameters of disease but also include the comprehensive assessment
of patients regarding their social status and psychological state.
A previous study on PAH focused on survival and several biological
parameters (12). To date, studies
on the QoL, anxiety and depression in patients with PAH have been
mostly cross-sectional; however, only few studies evaluated
interventions regarding influencing factors and further observed
the changes of symptoms, objective parameters, QoL and the mental
condition after the intervention (5-7,10,13).
Domestic baseline data on depression, anxiety and QoL in patients
with PH and further intervention are currently limited. Research on
the QoL of patients with PAH and the relevant risk factors and the
implementation of appropriate interventions are of vital clinical
significance to improve patient prognosis.
While several studies demonstrated that medication
improved the hemodynamics and exercise capacity of patients with
PH, their functional status and QoL was not improved accordingly
(4,13). QoL has been frequently ignored in
clinical practice (12,14,15), and
to date, few studies (2,5,9) have
focused on mental symptoms (anxiety and depression) and their
impact on QoL. Thus, the present study based on a Chinese
population investigated anxiety and depression as well as QoL in
patients with PH and discussed the following aspects: i) The
association between mental symptoms (anxiety and depression) and
QoL and the influencing factors; ii) the link between the presence
of anxiety and/or depression and the outcome for patients with PH,
which provided a theoretical basis for preventing deterioration and
improving survival.
Patients and methods
Study population
The present study was approved by the Ethics
Committee of Beijing Chao-yang hospital (Beijing, China). Patients
diagnosed with PH by RHC between March 2015 and February 2016 at
Beijing Chao-yang Hospital (Beijing, China) were enrolled. All
patients consented to study participation and provided written
informed consent for the use and publication of their data in the
present study. The inclusion criteria were as follows: i) Age
>18 years and ii) the diagnosis was confirmed by RHC. The
exclusion criteria were as follows: i) Patients had known mental
diseases and intellectual disability recorded in their medical
history; ii) cerebrovascular disease and senile dementia; iii)
systematic hormonotherapy; iv) if patients had one of the
following: Severe heart disease, dysfunction of kidney or liver or
other organ dysfunction.
Collection of clinical baseline
data
Patients meeting the inclusion criteria signed the
informed consent form and their baseline data (age, sex, duration
of symptoms, occupation, education, financial status) were
collected, as well as their clinical data including N-terminal
pro-brain natriuretic peptide, blood gas analysis, pulmonary
function test, cardiac color ultrasound, RHC and treatment.
Questionnaires, including Generalized Anxiety Disorder-7 (GAD-7;
none, score 0-4; mild, score 5-9; moderate, score 10-14; severe,
15-21), the Patient Health Questionnaire depression scale-9 (PHQ-9;
none, score 0-4; mild, score 5-9; moderate, score 10-14; severe,
score 15-19; very severe, score 20-27) and the short form 36 Health
Survey Questionnaire (SF-36) (16)
were applied to the patients.
Follow-up
Patients enrolled were followed up by telephone or
at the outpatient department every 3 months to record whether an
end-point event occurred. The total follow-up time was 1 year and
the average follow-up time for the cohort was 6 months. The
end-point event was defined as death or re-admission due to
exacerbation. The definition of exacerbation included exacerbation
of symptoms including cough, dyspnea, palpitation or syncope
leading to admission or other conditions, including pneumonia
requiring clinical treatment.
Statistical analysis
SPSS 18.0 software (SPSS, Inc.) was used to analyze
the data. Descriptive statistics were used to indicate the
characteristics of the participants. Continuous variables were
expressed as the mean ± standard deviation or median with range
when appropriate. Enumeration data were expressed using the
constituent ratio or rate. Continuous variables of the baseline
characteristics were compared using analysis of variance. A linear
correlation was assumed to assess the correlation between two
variables. A Spearman's logistic regression analysis (univariate
logistic regression analysis and multivariate logistic regression
analysis) was performed to calculate odds ratios and 95% confidence
intervals for different baseline characteristics regarding the
impact on anxiety and/or depression was assessed. Variables with
P<0.05 in the univariate logistic regression analysis were
subjected to multivariate logistic regression analysis. Follow-up
results of patients were presented by Kaplan-Meier curves in a
time-to-event model and compared between groups by using the
log-rank test. All analyses were performed as two-sided
significance tests and statistical significance was set at
P<0.05.
The SF-36 includes 36 items in 8 dimensions:
Physical functioning, role limitations due to physical health (RP),
body pain (BP), general health perceptions, vitality, social
functioning, role limitation due to emotional problems and mental
health. The GAD-7 and PHQ-9 include 7 and 9 questions and aim to
screen anxiety and depression, respectively (17,18).
Results
Basic information of the
participants
A total of 156 patients with PH were recruited for
the present study. Of these, 40 cases were excluded, as RHC was not
performed or the RHC data were not available. Furthermore, 1
patient was excluded for refusing to complete the SF-36, and 2
patients were excluded due to lack of the PHQ-9 and GAD-7 results.
In addition, 15 patients were excluded due to undesired
classifications of PH after further examination. Finally, 98
patients were enrolled.
The cohort of the present study included 36 patients
with PAH and 62 patients with CTEPH. The number of patients with
anxiety was 51 (52%) and the number of patients with depression was
56 (57.1%). Based on the results of the PHQ-9 and GAD-7
questionnaires, the patients were divided into two groups: Group 1
included patients with PH with anxiety and/or depression, while
group 2 included patients with PH with no anxiety/depression. Group
1 comprised 65 patients (20 males and 45 females; average age,
47.94±12.84 years). Group 2 consisted of 33 patients with PH (18
males, 15 females; average age, 49.53±16.91 years), thus, 66.33% of
the participants with PH had anxiety and/or depression, while less
than half classified as ‘no anxiety or depression’ based on GAD-7
and PHQ-9. The two groups were mostly made up of patients with
CTEPH: There were 44 (67.7%) patients with CTEPH in group 1 and 18
(54.5%) patients with CTEPH in group 2. In group 1, 16 patients
(24.6%) received basic treatment (Warfarin or conservative
treatment), 14 patients (21.5%) received pulmonary
thrombendarterectomy during the follow-up period and 35 (53.8%)
received oral targeted drugs (endothelin receptor antagonist,
phosphodiesterase inhibitors-V, prostacyclin analogues). In group
1, 6 patients (18.2%) received basic treatment (Warfarin or
etiological treatment), 7 patients (21.2%) received pulmonary
thrombendarterectomy during the follow-up period and 20 (60.6%)
received oral targeted drugs (endothelin receptor antagonist,
phosphodiesterase inhibitors-V, prostacyclin analogues). A summary
and comparison of demographics, functional classification,
hemodynamics and major treatments is provided in Table I.
 | Table IComparison of baseline
information. |
Table I
Comparison of baseline
information.
| Parameter | Anxiety and/or
depression (n=65) | No anxiety or
depression (n=33) | P-value |
|---|
| Age (years) | 47.94±12.84 | 49.53±16.91 | 0.606 |
| Sex (male vs.
female) | 20 (30.8) | 18 (54.5) | 0.023 |
| BMI
(kg/m2) | 23.52±3.625 | 23.55±3.183 | 0.962 |
| Course of disease
(months) | 24 (10-48) | 18 (7-54) | 0.916 |
| Classification of
PH | | | 0.205 |
|
PAH (I) | 21 (32.3) | 15 (45.5) | |
|
CTEPH
(IV) | 44 (67.7) | 18 (54.5) | |
|
Other
underlying diseases | 28 (43.1) | 9 (27.1) | 0.122 |
| CVP | 5 (2.5-10) | 3 (2-9) | 0.212 |
| mPAP | 50.45±10.48 | 55.33±16.22 | 0.074 |
| Cardiac index | 2.03 (1.60-2.54) | 2.07 (1.72-2.60) | 0.287 |
| PVR | 1,097.15±543.49 | 1,013.05±491.57 | 0.472 |
| 6MWD | 364.89±109.24 | 403.91±87.41 | 0.080 |
| Score of Borg ≥4 | 24 (40) | 5 (15.1) | 0.021 |
| Cardiac function WHO
III/IV |
34
(52.3) | 10 (30.3) | 0.036 |
| FEV1/pre | 86.25±13.40 | 75.04±14.77 | 0.001 |
| DLCO/VA | 75.93±19.56 | 80.86±17.70 | 0.287 |
| NT-proBNP | 962.7
(211.5-1,946.0) | 414.65
(79.97-2,469.8) | 0.339 |
| Major
treatment | | | 0.743 |
|
Basic
treatment | 16 (24.6) | 6 (18.2) | |
|
Surgery | 14 (21.5) | 7 (21.2) | |
|
Targeted
medicine | 35 (53.8) | 20 (60.6) | |
| Adverse event
during follow-up | 15 (23.1) | 2 (6) | 0.022 |
There was no significant difference between groups 1
and 2 for all patients with PH, in the classification of PH, 6MWD
and major treatment. However, the gender distribution, Borg scores
and cardiac function classification were significantly different
(P<0.05): In the anxiety and/or depression group, the proportion
of females and the Borg scores were higher than those group 2 (sex,
P=0.023; Borg score, P=0.021); in addition, cardiac insufficiency
was more severe in the anxiety and/or depression group
(P=0.044).
In the study population, according to the GAD-7 and
PHQ-9 score, respectively, 51 patients (52%) had anxiety symptoms
and the proportion of mild, moderate and severe anxiety was 30, 14
and 8%, and 56 patients (57%) had symptoms of depression.
Depression was divided into four degrees: Mild depression (29%),
moderate depression (12%), severe depression (10%) and very severe
depression (6%; Fig. 1).
Correlation analysis between
anxiety/depression and QoL
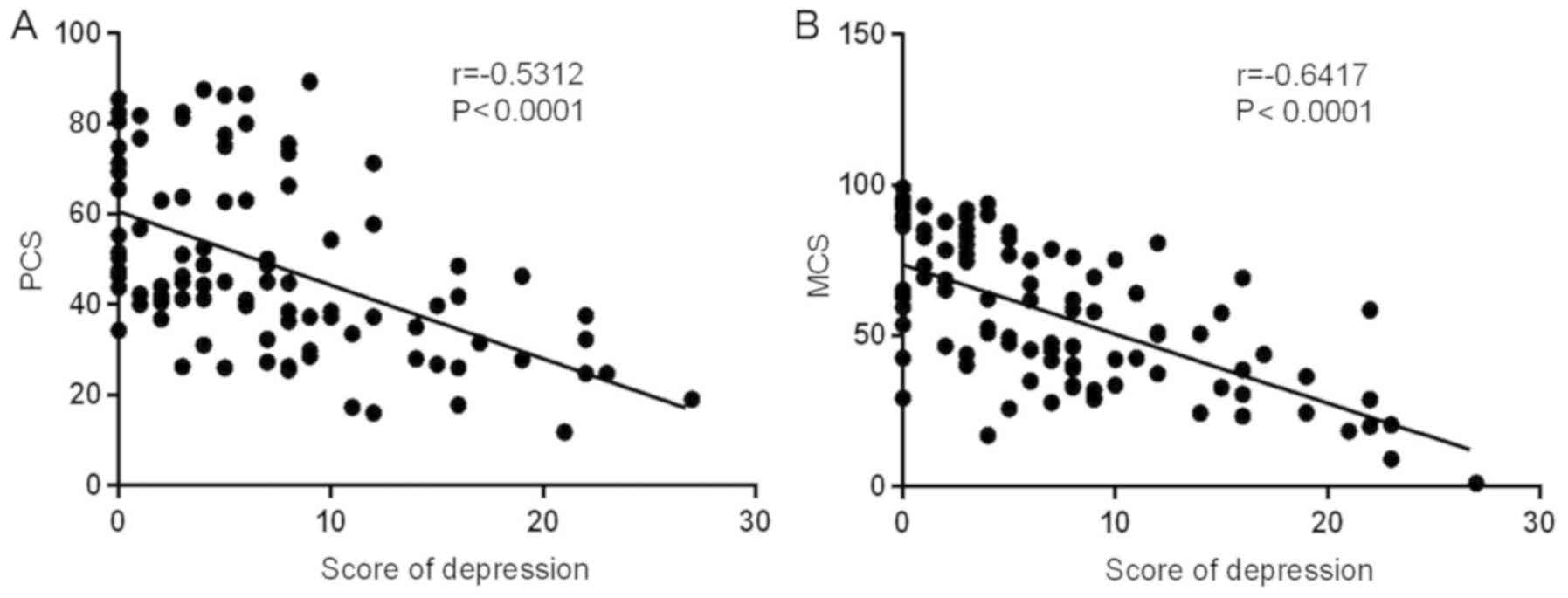
In SF-36, physical component summary (PCS) and
mental component summary (MCS) were summarized. It was revealed
that anxiety was negatively correlated with the Physical Component
Summary (PCS) and was also negatively correlated with the Mental
Component Summary (MCS; Fig. 2). The
correlation analysis between depression and QoL indicated that
depression was negatively correlated with PCS and MCS (Fig. 3).
Comparison of QoL
In the anxiety and/or depression group, all
dimensions of QoL were obviously more impaired than in the group
without anxiety and/or depression and the difference was
statistically significant (RP, P=0.033; BP, P=0.016; all other
dimensions, P<0.01; Fig. 4).
 | Figure 4.Comparison of quality of life between
two groups in eight dimensions: PF, RP, BP, GH, VT, SF, RE, MH, PCS
and MCS. PF, physical functioning; RP, role limitations due to
physical health; BP, bodily pain; GH, general health perceptions;
VT, vitality; SF, social functioning; RE, role limitation due to
emotional problems; MH, mental health; PCS, Physical Component
Summary; MCS, Mental Component Summary. |
Logistic regression analysis of
influencing factors of anxiety and/or depression
Based on the results of the univariate
logistic-regression analysis (Table
II), the multivariate logistic regression analysis was
performed to identify influencing factors of anxiety and/or
depression in patients with PH (Table
III). The significant influencing factors were financial
situation (OR, 4.616; 95%CI, 1.498-14.227; P=0.008) and right
ventricular enlargement (OR, 6.639; 95%CI, 1.047-42.107;
P=0.045).
 | Table IIUnivariate logistic regression
analysis of influencing factors of anxiety and/or depression. |
Table II
Univariate logistic regression
analysis of influencing factors of anxiety and/or depression.
| | | | 95% CI |
|---|
| Variable | P-value | OR | Lower | Upper |
|---|
| Sex (male vs.
female) | 0.746 | 1.111 | 0.588 | 2.100 |
| Marital status
(married vs. unmarried) | 0.002 | 1.406 | 1.132 | 1.747 |
| University degree
or higher | 0.001 | 1.481 | 1.171 | 1.874 |
| Financial situation
(monthly income <2000RMB) | 0.024 | 1.383 | 1.043 | 1.835 |
| Targeted
medicine | 0.002 | 1.577 | 1.189 | 2.091 |
| Other underlying
diseases | 0.003 | 3.111 | 1.468 | 6.593 |
| Decreasing
TAPSE | 0.007 | 2.048 | 1.215 | 3.450 |
| Right ventricular
enlargement | 0.005 | 1.929 | 1.222 | 3.044 |
| Decreased LVEF
(<50%) | 0.341 | 3.000 | 0.312 | 28.841 |
| Right atrial
enlargement | 0.002 | 2.174 | 1.327 | 3.562 |
| Pericardial
effusion | 0.069 | 2.600 | 0.927 | 7.293 |
| Cardiac function
WHO III/IV | 0.000 | 1.686 | 1.265 | 2.248 |
| 6MWD <350
meters | 0.003 | 3.571 | 1.545 | 8.257 |
| Obstructive
ventilation function disturbance | 0.732 | 0.889 | 0.453 | 1.743 |
| Score of Borg
≥4 | 0.001 | 4.800 | 1.831 | 12.58 |
| Increased
NT-proBNP | <0.001 | 2.765 | 1.588 | 4.815 |
 | Table IIIMultivariate logistic regression
analysis of influencing factors of anxiety and/or depression. |
Table III
Multivariate logistic regression
analysis of influencing factors of anxiety and/or depression.
| | | | 95% CI |
|---|
| Variable | P-value | OR | Lower | Upper |
|---|
| Marital status
(married vs. unmarried) | 0.841 | 1.142 | 0.314 | 4.158 |
| University degree
or higher | 0.722 | 1.246 | 0.372 | 4.170 |
| Financial situation
(monthly income <2000RMB) | 0.008 | 4.616 | 1.498 | 14.227 |
| Targeted
medicine | 0.614 | 0.769 | 0.278 | 2.132 |
| Other underlying
diseases | 0.214 | 0.476 | 0.148 | 1.534 |
| Decreasing
TAPSE | 0.218 | 2.500 | 0.582 | 10.737 |
| Right ventricular
enlargement | 0.045 | 6.639 | 1.047 | 42.107 |
| Right atrial
enlargement | 0.143 | 0.253 | 0.04 | 1.594 |
| Cardiac function
WHO III/IV | 0.506 | 0.643 | 0.175 | 2.364 |
| 6MWD <350
meters | 0.301 | 0.493 | 0.129 | 1.884 |
| Score of Borg
≥4 | 0.432 | 0.587 | 0.155 | 2.220 |
| Increased
NT-proBNP | 0.567 | 0.655 | 0.154 | 2.789 |
Results of end-point events and
anxiety and/or depression
During the follow-up period, end-point events (death
or admission due to deterioration) occurred in two cases (6%) in
group 2; by contrast, the number of cases with end-point events in
group 1 was significantly higher (n=15, 23.1%, P=0.022; Table I). Kaplan-Meier analysis indicated
that survival without adverse events in group 2 was higher than
that in group 1 (P=0.0730; Fig. 5A).
In the analysis for anxiety and depression individually, survival
without adverse events in the patients with anxiety was lower than
that in the patients without anxiety, but the difference was not
significant (P=0.3477; Fig. 5B);
however, survival without adverse event in patients with depression
was significantly lower than that of the patients without
depression (P=0.008; Fig. 5C).
Discussion
In the present study, 98 patients diagnosed with PAH
or CTEPH by RHC were enrolled. The results of the questionnaires
suggested that the incidence of anxiety and/or depression in
patients with PH was considerable in the study population. In the
present study, 51 patients (52%) had anxiety, among which 22% had
moderate and severe anxiety; furthermore, 56 patients (57%) had
depression, with 28% of patients having moderate or severe
depression. There was an obvious correlation between the state of
anxiety, depression and the impairment of QoL. Furthermore, the
presence of depression was correlated with poor prognosis of the
patients. The result of the high incidence of mental symptoms in
patients with PAH and CTEPH was in accordance with previous studies
in other countries (5,8,14). By
analyzing the association between anxiety, depression, QoL and
prognosis, the present study emphasized the importance of
incorporating mental health into the management of patients with
PH.
The association between mental health and QoL has
been studied in multiple diseases, including cystic fibrosis,
diabetes mellitus and heart diseases (10). The occurrence of mental disorders has
been linked to difficulties in daily activities; however, whether
difficulty in daily activities was the result of mental diseases or
the cause of mental diseases remains elusive. Due to the type and
severity of PH, affected patients are vulnerable to emotional
problems, including anxiety, depression and panic attacks (19). In patients with PAH, the estimated
incidence of moderate to severe depression is 20-50% (5,20,21). One
cross-sectional study revealed that 19.2% of patients with PH
developed severe depression and may develop other types of mental
disorders, yet only 23.4% of patients from outpatient department
and 8.6% patients from the inpatient department were receiving
psychotherapy, while more than half wished for a relevant therapy
(8). Furthermore, >90% of
patients at the inpatient department with moderate to severe mental
problems had not been treated with psychoactive medication
(8). The present result that the
incidence of anxiety and/or depression in patients with PAH and
CTEPH was high was in accordance with those of previous studies
(8-10).
The present study revealed that anxiety and
depression were negatively correlated with PCS and MCS of QoL. The
QoL score in all dimensions was decreased in patients with PAH and
CTEPH with anxiety and/or depression status compared with those
without anxiety or depression.
In the present study, anxiety and/or depression
occurred more frequently in females (75 vs. 53% in males), which
was in accordance with previous results indicating that females
were vulnerable to mental diseases (22). It has been demonstrated that anxiety
and depression are common complications of chronic obstructive
disease (23). The present study
indicated that the significant influencing factors of
anxiety/depression were the financial situation and right
ventricular enlargement. The conclusion that the financial
situation as a significant influencing factor of anxiety/depression
was in accordance with a previous descriptive study by our group,
according to which patients with PH reported that the financial
burden due to their diseases was heavy and they had emotional
problems (24). It appears that the
self-assessment of the mental condition and QoL by patients,
together with clinical parameters determined by clinicians, may be
part of a comprehensive assessment.
Harzheim et al (10) indicated that although most patients
did not receive psychological treatment, there was no difference in
long-term survival between patients with moderate, severe, mild or
no anxiety and depression. The rate of end-point events (death or
hospitalization due to exacerbation) in the group with anxiety
and/or depression was much higher than that in the
non-anxiety/depression group during the follow-up period. The
prognosis of patients with anxiety was inferior to that of the
patients without anxiety, but the difference was not statistically
significant. However, adverse events more frequently occurred in
patients with depression than in patients without depression and
the difference was statistically significant. Compared with
patients with anxiety, patients with depression tend to develop
adverse outcomes, suggesting that depression may be associated with
constant reflection of the physical condition on the mental state
and was more associated with prognosis.
Of note, the present study had certain limitations.
It was difficult to perform a subgroup analysis for anxiety and/or
depression and QoL in different types of patients with PH due to
the small sample and relatively short follow-up period in the
present study; thus, it is required to widen the sample size and
prolong the follow-up period in a further study. As another
limitation, screening tools for anxiety and depression were used,
which identified symptoms but were not able to make a definite
diagnosis for mental disease. The use of those tools may be
associated with considerable bias. The patients were screened with
self-assessment questionnaires. In the medical procedure, the
patients' mental symptoms were frequently ignored. The present
initial survey was made to call for more attention with this regard
and more studies in China. A psychiatrist is required to make a
definite diagnosis using more professional tools (Chinese version
of the Structured Clinical Interview for Diagnostic and Statistical
Manual of Mental Disorders, Fourth Edition (25,26) and
this may be performed in further studies by our group. Thus,
cooperation with the psychological department is required for
screening and further diagnosis in order to guide clinical
management and specific treatment if required. Finally, the present
study did not investigate whether the patients received
psychological intervention and the outcome of anxiety and
depression was not determined; therefore, the relevance between the
outcome of anxiety and depression and the clinical outcome was not
discussed in the present study. Future studies are required to
answer those questions.
Regarding prospects for future research, previous
studies to evaluate the impact of PH therapy on anxiety and
depression were limited. One study concluded that the rate of
anxiety and/or depression in patients with PH using Epoprostenol
was lower than in those who did not (4). It was also reported that outcomes in
patients with PAH using selective serotonin reuptake inhibitors
(SSRIs) to treat depression may be better; however, due to multiple
effects of SSRIs, this conclusion requires to be further confirmed
(27). A later study indicated that
SSRIs were associated with an increased death rate and clinical
deterioration risk in PAH (28).
Exercise training as an adjuvant therapy may improve exercise
capacity, QoL and relative parameters of long-term outcome in
patients with inoperable or residual CTEPH and may improve the 1, 2
and 3-year survival rate (15). It
may be proposed that a similar adjuvant therapy may improve anxiety
and depression in patients similar to those of the present cohort
and further studies are required to provide evidence.
In conclusion, even though optimized treatments for
PH are now available, anxiety and/or depression were frequently
identified in such patients and were significantly correlated with
impaired QoL. The present study based on a Chinese population calls
for the necessity of including the screening for and diagnosis of
anxiety and depression by professional questionnaires into routine
clinical examination. In addition, there should be more randomized
controlled trials to address the role of interventions including
psychological consultation, psychological-social support and
medication in patients with PH with anxiety and depression.
Acknowledgements
Not applicable.
Funding
The present study was supported by the fund of the
National Natural Science Foundation of China (grant no. 81570049),
the Beijing Natural Science Foundation (grant no. 7152062) and the
National Key Research and Development Program of China (grant no.
2016YFC0905600).
Availability of data and materials
The datasets used and/or analyzed during the present
study are available from the corresponding author on reasonable
request.
Authors' contributions
XZ, HS and ZhZ were responsible for patient data
collection, analysis and interpretation, and were major
contributors in writing the manuscript. CW, YY and ZuZ made
substantial contributions to the conception and design of the study
and were involved in drafting the manuscript. All authors agreed to
be accountable for all aspects of the work in ensuring that
questions associated with the accuracy or integrity of any part of
the work are appropriately investigated and resolved. All authors
read and approved the final manuscript.
Ethics approval and consent to
participate
This study was approved by the Ethics Committee of
Beijing Chao-yang Hospital (Beijing, China). Written informed
consent to participate was obtained from all patients and was in
written form.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Galiè N, Humbert M, Vachiery JL, Gibbs S,
Lang I, Torbicki A, Simonneau G, Peacock A, Vonk Noordegraaf A,
Beghetti M, et al: 2015 ESC/ERS guidelines for the diagnosis and
treatment of pulmonary hypertension: The joint task force for the
diagnosis and treatment of pulmonary hypertension of the European
society of cardiology (ESC) and the European respiratory society
(ERS): Endorsed by: Association for European paediatric and
congenital cardiology (AEPC), international society for heart and
lung transplantation (ISHLT). Eur Heart J. 37:67–119.
2016.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Matura LA, McDonough A and Carroll DL:
Symptom prevalence, symptom severity, and health-related quality of
life among young, middle, and older adults with pulmonary arterial
hypertension. Am J Hosp Palliat Care. 33:214–221. 2016.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Heyworth IT, Hazell ML, Linehan MF and
Frank TL: How do common chronic conditions affect health-related
quality of life. Br J Gen Pract. 59:e353–e358. 2009.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Shafazand S, Goldstein MK, Doyle RL,
Hlatky MA and Gould MK: Health-related quality of life in patients
with pulmonary arterial hypertension. Chest. 126:1452–1459.
2004.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Batal O, Khatib OF, Bair N, Aboussouan LS
and Minai OA: Sleep quality, depression, and quality of life in
patients with pulmonary hypertension. Lung. 189:141–149.
2011.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Rubenfire M, Lippo G, Bodini BD, Blasi F,
Allegra L and Bossone E: Evaluating health-related quality of life,
work ability, and disability in pulmonary arterial hypertension: An
unmet need. Chest. 136:597–603. 2009.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Chua R, Keogh AM, Byth K and O'Loughlin A:
Comparison and validation of three measures of quality of life in
patients with pulmonary hypertension. Intern Med J. 36:705–710.
2006.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Larisch A, Neeb C, de Zwaan M, Pabst C,
Tiede H, Ghofrani A, Olsson K, Hoeper M and Kruse J: Mental
distress and wish for psychosomatic treatment of patients with
pulmonary hypertension. Psychother Psychosom Med Psychol.
64:384–389. 2014.(In German). PubMed/NCBI View Article : Google Scholar
|
|
9
|
Löwe B, Gräfe K, Ufer C, Kroenke K, Grünig
E, Herzog W and Borst MM: Anxiety and depression in patients with
pulmonary hypertension. Psychosom Med. 66:831–836. 2004.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Harzheim D, Klose H, Pinado FP, Ehlken N,
Nagel C, Fischer C, Ghofrani A, Rosenkranz S, Seyfarth HJ, Halank
M, et al: Anxiety and depression disorders in patients with
pulmonary arterial hypertension and chronic thromboembolic
pulmonary hypertension. Respir Res. 14(104)2013.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Halank M, Einsle F, Lehman S, Bremer H,
Ewert R, Wilkens H, Meyer FJ, Grünig E, Seyfarth HJ, Kolditz M, et
al: Exercise capacity affects quality of life in patients with
pulmonary hypertension. Lung. 191:337–343. 2013.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Flattery MP, Pinson JM, Savage L and
Salyer J: Living with pulmonary artery hypertension: Patients'
experiences. Heart Lung. 34:99–107. 2005.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Cicero C, Franchi SM, Barreto AC and Lopes
AA: Lack of tight association between quality of life and exercise
capacity in pulmonary arterial hypertension. Arq Bras Cardiol.
99:876–885. 2012.(In English, Portuguese). PubMed/NCBI View Article : Google Scholar
|
|
14
|
McCabe C, Bennett M, Doughty N, MacKenzie
Ross R, Sharples L and Pepke-Zaba J: Patient-reported outcomes
assessed by the CAMPHOR questionnaire predict clinical
deterioration in idiopathic pulmonary arterial hypertension and
chronic thromboembolic pulmonary hypertension. Chest. 144:522–530.
2013.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Nagel C, Prange F, Guth S, Herb J, Ehlken
N, Fischer C, Reichenberger F, Rosenkranz S, Seyfarth HJ, Mayer E,
et al: Exercise training improves exercise capacity and quality of
life in patients with inoperable or residual chronic thromboembolic
pulmonary hypertension. PLoS One. 7(e41603)2012.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Li L, Wang HM and Shen Y: Chinese SF-36
health survey: Translation, cultural adaptation, validation, and
normalisation. J Epidemiol Community Health. 57:259–263.
2003.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Spitzer RL, Kroenke K, Williams JB and
Löwe B: A brief measure for assessing generalized anxiety disorder:
The GAD-7. Arch Intern Med. 166:1092–1097. 2006.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Kroenke K, Spitzer RL and Williams JB: The
PHQ-9: Validity of a brief depression severity measure. J Gen
Intern Med. 16:606–613. 2001.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Matura LA, McDonough A and Carroll DL:
Health-related quality of life and psychological states in patients
with pulmonary arterial hypertension. J Cardiovasc Nurs.
29:178–184. 2014.PubMed/NCBI View Article : Google Scholar
|
|
20
|
McCollister DH, Beutz M, McLaughlin V,
Rumsfeld J, Masoudi FA, Tripputi M, Yaeger T, Weintraub P and
Badesch DB: Depressive symptoms in pulmonary arterial hypertension:
Prevalence and association with functional status. Psychosomatics.
51:339–339.e8. 2010.PubMed/NCBI View Article : Google Scholar
|
|
21
|
White J, Hopkins RO, Glissmeyer EW,
Kitterman N and Elliott CG: Cognitive, emotional, and quality of
life outcomes in patients with pulmonary arterial hypertension.
Respir Res. 7(55)2006.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Buoli M, Caldiroli A, Serati M, Grassi S
and Altamura AC: Sex steroids and major psychoses: Which role for
DHEA-S and progesterone. Neuropsychobiology. 73:178–183.
2016.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Maurer J, Rebbapragada V, Borson S,
Goldstein R, Kunik ME, Yohannes AM and Hanania NA: ACCP Workshop
Panel on Anxiety and Depression in COPD: Anxiety and depression in
COPD: Current understanding, unanswered questions, and research
needs. Chest. 134 (4 Suppl):43S–56S. 2008.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Zhai Z, Zhou X, Zhang S, Xie W, Wan J,
Kuang T, Yang Y, Huang H and Wang C: The impact and financial
burden of pulmonary arterial hypertension on patients and
caregivers: Results from a national survey. Medicine (Baltimore).
96(e6783)2017.PubMed/NCBI View Article : Google Scholar
|
|
25
|
First MB, Spitzer RL, Gibbon M and
Williams JBW: Structured clinical interview for DSM.IV.TR axis I
disorders, research version, patient edition (SCID.I/P). New York:
Biometrics Research, New York State Psychiatric Institute,
2002.
|
|
26
|
Kam IW: Development of the bilingual
(Chinese/English) SCID-I (Structured Clinical Interview for DSM-IV
axis I disorder): A study of its reliability and validity in an
in-patient population (Dissertation for Part III Examination of
FHKCPsych) Hong Kong College of Psychiatrist, Hong Kong, 2000.
|
|
27
|
Kawut SM, Horn EM, Berekashvili KK,
Lederer DJ, Widlitz AC, Rosenzweig EB and Barst RJ: Selective
serotonin reuptake inhibitor use and outcomes in pulmonary arterial
hypertension. Pulm Pharmacol Ther. 19:370–374. 2006.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Sadoughi A, Roberts KE, Preston IR, Lai
GP, McCollister DH, Farber HW and Hill NS: Use of selective
serotonin reuptake inhibitors and outcomes in pulmonary arterial
hypertension. Chest. 144:531–541. 2013.PubMed/NCBI View Article : Google Scholar
|