Introduction
The thumb plays a critical role in hand performance
and grip. If the thumb is injured overall hand function can be
severely affected. Proper repair of thumb soft tissue defects is
therefore of significant importance in maintaining hand function
(1-3).
Soft tissue defects of the thumb are usually accompanied by
exposure of the distal phalanx or flexor tendons. Flap surgery is a
subspecialty of plastic and reconstructive surgery. In this
procedure a piece of tissue is transferred from the donor site to
the recipient site while maintaining its own blood supply. These
donor tissues may form local flaps (adjacent to the defect site),
regional flaps or distant flaps (located at a significant distance
from the donor site) (4). Multiple
techniques and methods have been employed to repair soft tissue
defects of the thumb tip (5).
Mitsunaga et al (6)
demonstrated that a modified digital artery perforator flap allowed
for preservation of digital length, volume and finger function.
These flaps can be raised as adiposal-only flaps or extended flaps
and supercharged through perforator-to-perforator anastomoses. For
traumatic fingertip and finger stump reconstructions, digital
artery perforator flaps deliver consistent aesthetic and functional
results (7-9).
Subsequently, numerous clinical trials have demonstrated that the
thumb dorsoulnar artery pedicle flap is an effective technique to
repair soft tissue defects (7-14).
Ramirez and Gonzalez (15) described
the local patterns of the thumb vascular anatomy of 30 fresh right
hands from male and female cadavers using a vascular injection
technique with methyl methacrylate, providing anatomical evidence
for the pedicle flap design. However, conventional flap design has
certain limitations, which reduce the clinical efficacy of soft
tissue repair, due to the tension in the subcutaneous tunnel, and
lower the survival rate of the flap. In the present case report,
thumb dorsoulnar artery pedicle flaps tunneled during flap
transposition were designed to repair thumb tip defects and their
success was evaluated through tests of hand grip and pinch
strength.
Patients and methods
Patient information and study
design
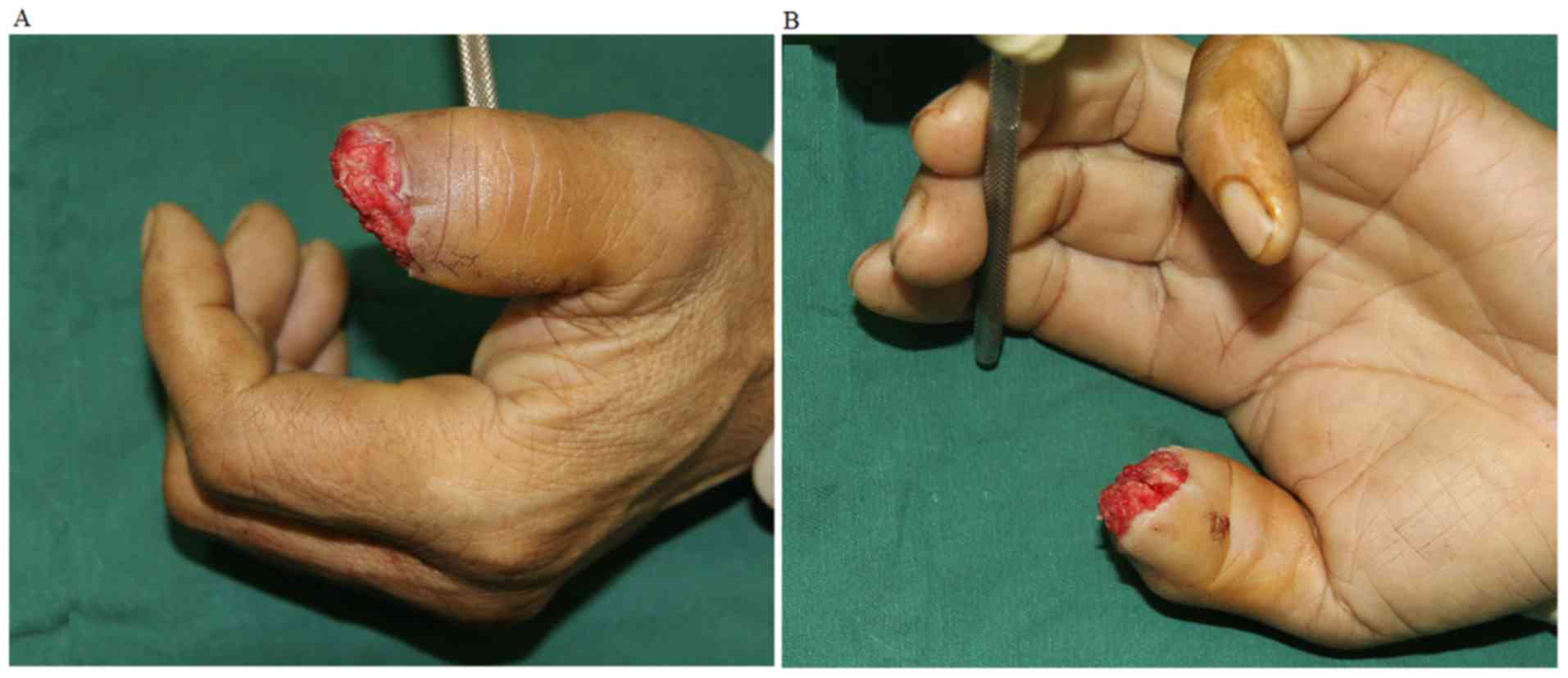
Between February 2012 and March 2014, 10 modified
dorsoulnar artery pedicle flaps were utilized in 10 patients (9
males and 1 female). The area of the thumb tip defects ranged from
2 to 9 cm2 in size (Fig.
1). These tip defects were caused by crush, cutting, avulsion
or wringer injuries. The mean patient age was 47 years, with a
range from 24 to 60 years. Seven cases involved left thumb injury
and three involved right thumb injury. The phalanx or tendon was
exposed in all cases.
The study inclusion criteria were as follows: i) The
soft tissue defect was on the palm side of the hand; ii) the end
point of the flexor pollicis longus tendon was not damaged; and
iii) there was no obvious damage to the nail bed. The study
exclusion criteria were: i) The patient had defects in the flexor
pollicis longus tendon; ii) the patient had suffered damage to more
than 1/4 of the nail bed; iii) the proximal end of the wound was
beyond the interphalangeal joint; and iv) surgery could not be
tolerated due to systemic disease.
Emergency debridement was delivered before surgical
procedures were performed using thumb dorsoulnar artery pedicle
flaps. All patients underwent surgery between 1 and 4 days after
injury. All cases were surgically treated with modified dorsoulnar
artery pedicle flaps (Table I).
 | Table IBaseline data of 10 patients included
in the current study. |
Table I
Baseline data of 10 patients included
in the current study.
| Sex | Age | Injury side | Cause of injury | Postoperative
necrosis | Flap size (cm) | Survival
condition |
|---|
| Male | 43 | Right | Machine | No | 3x2.5 | Healed |
| Female | 57 | Left | Machine | No | 4x3 | Healed |
| Male | 40 | Left | Machine | Partial | 3.5x2 | Healed |
| Male | 24 | Left | Machine | No | 4x2.5 | Healed |
| Male | 59 | Left | Machine | No | 3x2 | Healed |
| Male | 40 | Right | Machine | No | 3x2 | Healed |
| Male | 60 | Left | Machine | No | 2x1 | Healed |
| Male | 56 | Left | Crush injury | Partial | 2x1 | Healed |
| Male | 48 | Right | Machine | No | 2x1.6 | Healed |
| Male | 43 | Left | Crush injury | No | 2.3x1.4 | Healed |
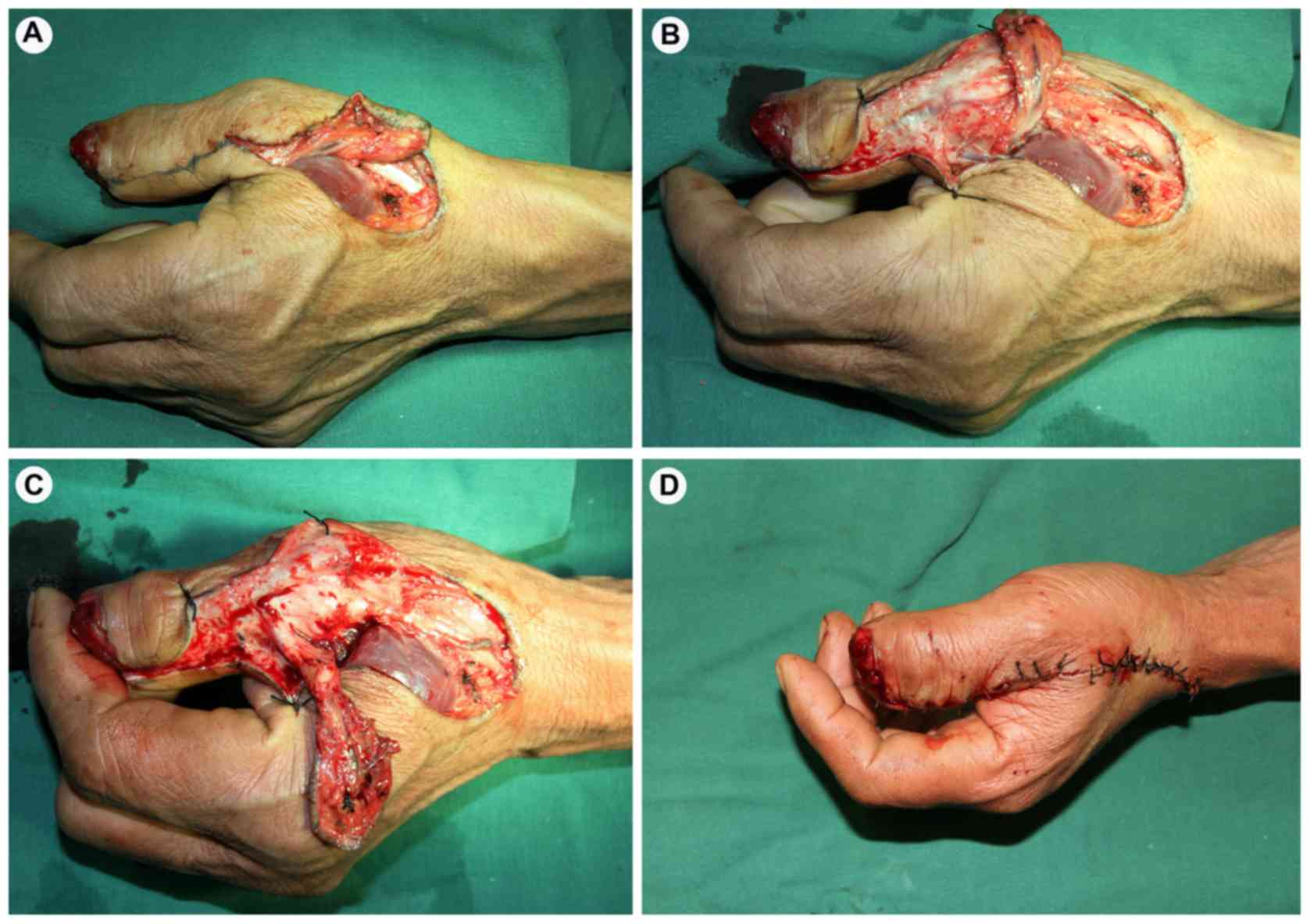
Triangular flap design
All cases were subject to brachial plexus
anesthesia. All necrotic and poorly vascularized tissues were
thoroughly debrided and utilized as the recipient site of modified
flaps. The size of the tip defects was measured and then the donor
site of the modified flaps was marked as follows: i) The connection
between the snuffbox proximal and the metacarpophalangeal joints of
the first dorsal ulnar side was marked as the central line of the
flap. To ensure adequate vascularity, the donor site flap was at
least 0.5 cm away from the proximal interphalangeal joint of the
thumb; ii) the flap tail was modified to an equilateral triangle
(Fig. 2); iii) the coverage of the
donor flap was slightly greater than that of the defect, or more
specifically the external portion of the turnover flap was slightly
oversized; and iv) the distal pivot point was >0.7-1 cm from the
tips of the defects (the distal end of flap was configured as an
equilateral triangle to fully cover the pedicle when rotating the
flap).
Written informed consent was obtained from all
patients. The study procedures were approved by the Ethics
committee of the Affiliated Hospital of Nantong University.
Flap transfer
All flap transfers were performed by an experienced
hand surgeon (Dr Renguo Xie) accredited with expertise level 4 for
flap surgery (16-18).
The skin at the distal end was excised and the thumb dorsal artery
was exposed. An incision was made from the edge to the proximal end
of the flap and the thumb dorsal ulnar artery was ligated. From the
thumb extensor aponeurosis and superficial adductor muscle
membrane, the flap containing a portion of the sarcolemma was
turned over in the opposite direction. The flap, 1.0 cm in length
and 0.8 cm in width, containing the thumb dorsal ulnar artery and 1
to 2 dorsal veins was designed along the dorsal ulnar artery. The
flap pedicle was located at either ulnar side. The proximal part of
the flap was used as the pedicle. The point of rotation did not
exceed one half of the plane of the middle phalanx (Fig. 2). After turning over the flap, to
cover the wound area, the flap was sutured without any tension. The
superficial branch of the radial nerve was fixed to coaptate to the
digital nerve, to recover the nerve sensation. It could be directly
sutured due to the small donor site (Fig. 3). If turning over the flap led to
tension, then a full-thickness skin graft from the inner aspect of
the forearm could be used. The blood vessel distribution,
color/temperature change and flap survival rate of the flap were
closely observed within 24 h after surgery. The suture was removed
14 days after surgery.
Strength measurements
Measuring grip and pinch strength is an important
part of hand injury evaluation. Grip strength was measured with a
Jamar hand dynamometer and the pinch strengths were measured with a
Jamar hydraulic pinch gauge (Patterson Medical Products, Inc.), the
non-injured hand was used as the control. The elbow was bent at
90˚, the forearm was in a neutral position, the wrist was flexed
from 0˚ to 30˚, and the scale deviation was 0˚ to 15˚. Each test
was repeated 3 times at 2 min intervals and all evaluations were
performed by a single investigator.
Statistical analysis
Grip and pinch strength were analyzed with a paired
t-test using the SPSS version 18.0 (SPSS, Inc.). Data were analyzed
in triplicate and were presented as the mean and standard
deviation. P<0.05 was considered to indicate a statistically
significant difference.
Results
Postoperative flap survival
All the modified flaps in the 10 patients survived.
The flaps survived at the skin graft donor sites in four patients
and after direct suture in the remaining 6 cases. Eight patients
obtained complete survival of the modified flaps, whereas two
patients suffered from distal flap necrosis. Subsequently, the
necrotic tissues were removed and replaced with healthy tissue at
~5 weeks after the first procedure. One patient presented with
postoperative venous insufficiency, which was effectively managed
by the treatment described below.
Postoperative thumb motion and
function
Postoperatively, 10 patients underwent follow-up for
6 to 12 months. The modified flaps were observed to be in good
condition (Fig. 4). Two measurements
were taken at 6 and 12 months after surgery. The range of motion of
the thumb interphalangeal joint ranged from 5˚ to 75˚, and for the
metacarpopalangeal joint 5˚ to 65˚, suggesting that partial
recovery of static two-point discrimination had been achieved in
the thumb flaps (Fig. 5). For
postoperative coverage of the donor sites, skin grafts were
utilized in 4 cases, and the donor sites were directly sutured in
the remaining 6 patients. One case exhibited venous insufficiency,
which was resolved by therapy and one case lost the distal flexor
pollicis longus tendon. First, the pedicle suture of the flap was
removed so that the pedicle was relaxed and did not squeeze the
vein. One or two veins were identified at the distal edge of the
flap. The dark venous blood at the edge of the flap was released by
the surgeon until bright red arterial blood appeared and these
procedures were repeated every 30 min by family members. The venous
insufficiency was monitored hourly by surgeons and had disappeared
within 12 h.
Grip and pinch strength were measured twice, 6 and
12 months after using a modified dorsoulnar artery pedicle flap in
the repair of the thumb tip defects. None of the patients started
new medication. Grip measurement was related to the second position
of the dynamometer and was performed with the elbow at ~90˚
according to the American Society of Hand Therapists
recommendations (19). Pinch
strength was measured between the tip of the thumb and index
finger. Three consecutive measurements were performed with a 2 min
inter-measurement interval. At 6 and 12 months after surgery, the
grip and pinch strength of the affected hands were restored to 85%
of the normal side (P>0.05; Table
II).
 | Table IIGrip and pinch strengths at 6 and 12
months after surgery. |
Table II
Grip and pinch strengths at 6 and 12
months after surgery.
| | 6 months | | 12 months | |
|---|
| | Affected hand | Normal hand | P-value | Affected hand | Normal hand | P-value |
|---|
| Pinch Strength
(kg) | 3.62±1.77 | 3.82±1.80 | 0.175 | 3.73±1.85 | 3.82±1.80 | 0.137 |
| Grip strength
(kg) | 27.3±8.3 | 32.0±11.4 | 0.186 | 28.4±7.12 | 32.0±11.4 | 0.143 |
The flap sutures and the flap pedicle were released,
the hematocele inside the tunnel removed, the flap pedicle covered
with vaseline gauze, and the tunnel skin sutured at postoperative
day 7. Mild adverse events occurred throughout the surgical
procedures, which were handled in a timely manner.
Discussion
Overall, the modified dorsoulnar artery pedicle flap
is an efficacious and safe technique for the repairment of the
thumb tip defects in clinical settings. In this case report, the
range of motion of interphalangeal joint activity was 5-75˚ and
5-45˚ for the metacarpophalangeal joint activity. Though the range
of motion improved, it did not recover completely. This may be due
to several potential factors. It is possible that scar tissue
extended into the metacarpophalangeal joints when the incision was
healed, as the incision was created from the snuffbox to the thumb
wound through the ulnar metacarpophalangeal joint. Another
possibility is that a majority of patients resisted performing
joint movement during the early stages of recovery, due to poor
tolerance of the severe pain. It is also possible that the, partial
tumescent flaps impacted interphalangeal joint flexion. In one
case, the distal flexor pollicis longus tendon was lost.
The present case study reports the design of a
distal flap through the creation of a dorsoulnar flap with an
equilateral triangle tail. Concurrently, the thumb wound was
directly coapted with the pedicle and the flap embedded in the tip
of the shuttle-type tunnel, which could avoid the incidence of
pedicle entrapment and reduce the risk of flap necrosis. Both the
donor and recipient sites functioned properly and the donor site
could be directly sutured. No apparent difference was identified in
the grafted skin color between the donor and recipient sites. The
risk of severe damage to the major vascular supply of the thumb
could be averted. The modified thumb flaps were suitable for large
degrees of rotation in a large area. A long vascular pedicle with a
flexible transfer could be created, which could conveniently reach
the tip of the wound site. The follow-up data at 6 and 12 months
post-surgery showed that grip and pinch strength of the affected
hands was restored to 85% of the normal side.
Bertehlli and Koury (5) improved the configuration of thumb
dorsal ulnar artery pedicle flaps and prolonged flap survival in 30
patients, using a technique termed the Brunelli flap. Yu et
al (9) evaluated the functional
sensory recovery of random-pattern abdominal skin flaps in the
repair of fingertip cutaneous deficiency and found that all flaps
obtained satisfactory flexibility and texture and that sensory
recovery was achieved. Hrabowski et al (20) reported that the maximum area of the
harvested thumb radial dorsal artery island flap was 5x4
cm2, slightly larger than 4x3 cm2 in the
present case study. Moschella and Cordova (21) demonstrated that the large area of
radial flap, which could be harvested, might readily lead to venous
congestion, even necrosis. In a previous study, it was determined
that the skin of the donor site lacks flexibility after direct
suture and this affected the perception of patients' towards the
results. Traditionally, the thumb dorsal ulnar artery flap was a
round or oval shape. The pedicle could reach the thumb defects
through a closed tunnel.
Wang et al (22) reported that the furthest
communicating branch between the thumb palmar artery and thumb
dorsal artery was located approximately 0.5 cm from the proximal
interphalangeal joint. The thumb dorsal artery island flap, which
contained superficial radial nerve branches, was harvested from the
first metacarpal dorsal site. It would be prudent to restore
sensory function when suturing the superficial radial nerve and the
digital nerve (22). In previous
studies, the flap nerve was directly sutured with the digital nerve
stump, whereas the result was not satisfactory, especially for
two-point discrimination test (9-14).
Similar findings were obtained in the present case report, though
the thumb flap two-point discrimination was partially restored.
Local flaps can be further divided according to
their blood supply. Random pattern flaps have no known feeding
blood vessel, while axial pattern flaps are based on a known artery
that directly supplies a specific skin territory. Interconnections
between branches of adjacent axial vessels exist that connect
neighboring skin territories. The V-Y advancement flap is suitable
for the coverage of transverse or dorsal oblique fingertip
amputations with exposed bone and sufficient nail bed support and
length (23). The thenar flap is
indicated for volar skin avulsions over the pulp of the finger
(24). The cross-finger flap is more
suited to treat distal defects, in which more tissue is required
for coverage than can be obtained from a local advancement flap
such as V-Y flap (25). The
homodigital island flap that is based on the volar blood supply of
the fingers, either the radial or ulnar digital artery and its
venae comitantes (26). The dorsal
metacarpal artery flap is based on a constant palmar-dorsal
perforator present in the digital web-space and it increases the
span of the flap to reach more distal defects (27).
In the present case report, the two-point
discrimination of the thumb flaps was slightly different than that
of the healthy side. Grip and pinch strength of the affected hands
could be restored to 85% of the normal side. The only partial
recovery of two-point discrimination was likely associated with the
adverse events induced by soft tissue injury. For the eight
patients undergoing postoperative follow-up, two-point
discrimination of the flaps was inferior to that of the healthy
side, but it did not affect the motion of the hands. Hand motion
was fully restored at postoperative 12 months, whereas nerve
sensation was not fully recovered, probably because the modified
thumb flaps do not carry complete innervation. The length of the
thumb was almost retained, the wound was fully healed and the
function of the thumb was slightly impaired. Taken together, the
grip and pinch strength of the affected hands were slightly less
than that of the contralateral side. During postoperative
follow-up, partial flap necrosis occurred in 2 patients. The dorsal
ulnar artery was injured during surgical exploration, which led to
constrained flap vascularization and subsequent flap necrosis. In
one case, the venous return of the flap became unobstructed after
treatment
Triangular flaps were used for the repair of 10
thumbs, showing that this technique not only resolved the tension
of the subcutaneous tunnel and, but also improved the survival rate
of the flap when compared to previous experience. The advantage of
this method is that the flap blood vessels are stable; the
amputation surface can be completely covered. However, this method
cannot be used for skin defects of a finger supplied by a
dorsoulnar artery, which limits its application in hand
surgery.
In conclusion, application of triangular dorsoulnar
artery pedicle flap in repair of thumb tip defects improved the
tension of the subcutaneous tunnel and the flap survival rate and
restored the grip and the pinch strength for the repaired hand. At
6 and 12 months after the modified dorsoulnar artery pedicle flap
had been used to repair the thumb tip defects, the grip and pinch
strength of the affected hands had been restored to 85% of that in
the normal side. The modified dorsoulnar artery pedicle flap is an
efficient and safe technique to repair thumb tip defects.
Acknowledgements
The authors would like to thank Ms. Lihua Chen
(Operating Room Nursing Department of the Affiliated Hospital of
Nantong University) for her surgical assistance.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the present
study are available from the corresponding author on reasonable
request.
Authors' contribution
TM proposed and designed this modified skin flap,
performed all surgeries, performed research and completed the
manuscript. RX participated in the design of the skin flap and part
of the surgery. GW and SX participated in part of the surgery and
collected and analyzed the data. All authors read and approved the
final manuscript.
Ethics approval and consent to
participate
Written informed consent was obtained from all
patients. The study procedures were approved by the Ethics
committee of the Affiliated Hospital of Nantong University.
Patient consent for publication
Patients provided written consent for the
publication of their data.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Muzaffar AR, Chao JJ and Erdidrich JB:
Posttraumatic thumb reconstruction. Plast Rdconstr Surg.
116:103e–122e. 2005.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Vdder NB and Hanel DP: The mangled upper
exteremity. In: Green's Operative Hand Surgery. Green D (ed). 5th
edition. Elsevier/Churchill Livingstone, New York, NY, pp1587-1628,
2005.
|
|
3
|
Tang JB, Elliot D, Adani R, Saint-Cyr M
and Stang F: Repair and reconstruction of thumb and finger tip
injures: A global view. Clin Plast Surg. 41:325–359.
2014.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Foucher G, Boulas HJ and Braga Da Silva J:
The use of flaps in the treatment of fingertip injuries. World J
Surg. 15:458–462. 1991.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Bertehlli JA and Koury Z: Neurocutaneous
island flap in the hand: Anatomical basis and preliminary results.
Br J Plast Surg. 45:586–590. 1992.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Mitsunaga N, Mihara M, Koshima I, Gonda K,
Takuya I, Kato H, Araki J, Yamamoto Y, Yuhei O, Todokoro T, et al:
Digital artery perforator (DAP) flaps: Modifications for fingertip
and finger stump reconstruction. J Plast Reconstr Aesthet Surg.
63:1312–1317. 2010.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Zhu L, Xu Q, Kou W, Ning B and Jia T:
Outcome of free digital artery perforator flap transfer for
reconstruction of fingertip defects. Indian J Orthop. 48:594–598.
2014.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Usami S, Kawahara S, Yamaguchi Y and
Hirase T: Homodigital artery flap reconstruction for fingertip
amputation: A comparative study of the oblique triangular
neurovascular advancement flap and the reverse digital artery
island flap. J Hand Surg Eur Vol. 40:291–297. 2015.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Yu YD, Zhang YZ, Bi WD and Wu T:
Functional sensory function recovery of random-pattern abdominal
skin flap in the repair of fingertip skin defects. Exp Ther Med.
5:830–834. 2013.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Panse N and Sahasrabudhe P: The ulnar
digital artery perforator flap: A new flap for little finger
reconstruction-a preliminary report. Indian J Plast Surg.
43:190–194. 2010.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Horta R, Barbosa R, Oliveira L, Amarante
JM, Marques M, Cruz Reis J and Rebelo M: Neurosensible
reconstruction of the thumb in an emergency situation: Review of
107 case. Tech Hang Up Extrem Surg. 13:85–89. 2009.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Teran P, Carnero S, Miranda R, Trillo E
and Estefanía M: Refinements in dorsoulnar flap of the thumb: 15
cases. J Hand Surg Am. 35:1356–1359. 2010.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Cheah AE and Chong AK: Soft-tissue
coverage of the hand. Curr Orth Practice. 23:336–345. 2012.
|
|
14
|
Han D, Sun H, Jin Y, Wei J and Li Q: A
technique for the non-microsurgical reconstruction of thumb tip
amputations. J Plast Reconstr Aesthet Surg. 66:973–977.
2013.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Ramirez AR and Gonzalez SM: Arteries of
the thumb: Description of anatomical variations and review of the
literature. Plast Reconstr Surg. 129:468e–476e. 2012.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Tang JB: Uncommon methods of flexor tendon
and tendon-bone repairs and grafting. Hand Clin. 29:215–221.
2013.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Tang JB: Re: Levels of experience of
surgeons in clinical studies. J Hand Surg Eur Vol. 34:137–138.
2009.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Tang JB and Avanessian B: Clinical
reports: The importance of reporting a surgeon's level of
expertise. J Hand Surg Am. 40:416–417. 2015.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Fess EE and Moran C: Clinical Assessment
Recommendations. American Society of Hand Therapists, Indianapolis,
1981.
|
|
20
|
Hrabowski M, Kloeters O and Germann G:
Reverse homodigital dorsoradial flap for thumb soft tissue
reconstruction: Surgical technique. J Hand Surg Am. 35:659–662.
2010.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Moschella F and Cordova A: Reverse
homodigital dorsal radial flap of the thumb. Plast Reconstr Surg.
117:920–926. 2006.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Wang C, Xu J and Zhang L: Applied anatomy
of the island flap pediceled with dorsal digital vessels. Chin J
Clin Anat. 24:514–517. 2006.
|
|
23
|
Ramirez MA and Means KR Jr: Digital soft
tissue trauma: A concise primer of soft tissue reconstruction of
traumatic hand injuries. Iowa Orthop J. 31:110–20. 2011.PubMed/NCBI
|
|
24
|
Gatewood A: A plastic repair of finger
defects without hospitalization. JAMA. 87(1479)1926.
|
|
25
|
Cronin TD: The cross finger flap: A new
method of repair. Am Surg. 17:419–425. 1951.PubMed/NCBI
|
|
26
|
Weeks PM and Wray RC (eds): Management of
Acute Hand Injury: A Biological Approach. Mosby, St. Louis, MI,
1973.
|
|
27
|
Maruyama Y: The reverse dorsal metacarpal
flap. Br J Plast Surg. 43:24–27. 1990.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Dellon AL: Management of peripheral nerve
problems in the upper and lower extremity using quantitative
sensory testing. Hand Clin. 15:697–715. 1999.PubMed/NCBI
|
|
29
|
Nizamis K, Rijken NH, Mendes A, Janssen
MM, Bergsma A and Koopman BF: A novel setup and protocol to measure
the range of motion of the wrist and the hand. Sensors (Basel).
18(E1881)2018.PubMed/NCBI View Article : Google Scholar
|
|
30
|
MacDermid JC: Measurement of health
outcomes following tendon and nerve repair. J Hand Ther.
18:297–312. 2005.PubMed/NCBI View Article : Google Scholar
|