Introduction
Coronary artery calcium score (CACS), as an
indicator of severity of coronary artery calcification (1), is an important preoperative parameter
for coronary atherosclerosis (2) and
an important basis for diagnosis of coronary heart disease. The
score can be used to assess the overall condition of patients with
coronary heart disease. Studies found that related inflammatory
factors and oxidative stress markers are associated with onset and
progression of coronary heart disease. Abnormal expression of these
indicators plays an important role in aggravating myocardial injury
(3). Inflammatory factors such as
interleukin-23 (IL-23) has pro-inflammatory effects. It is a
related mediator of oxidative stress response and may be involved
in inflammatory response, macrophage response, and immune disease
progression. IL-35 is thought to be an inducing factor that
activates the anti-inflammatory M2-like macrophage phenotype.
Recent studies showed that both cytokines are abnormal in plaque
formation (4). It was reported that
both IL-23 can promote inflammatory response and regulate
malondialdehyde (MDA) and superoxide dismutase (SOD) to promote
tissue damage (5). Expression of
IL-35 and SOD in peripheral blood of patients with coronary heart
disease often decreased, while expression of MDA increased. IL-35
may have a synergistic effect with oxidative stress indicators
during inflammatory activation, and MDA and SOD are inversely
correlated (6). In MDA-mediated
oxidative stress and inflammation, it was noted that the expression
of microRNA (miRNA) in serum may also be abnormal (7). According to the literature reports on
coronary heart disease, two factors were selected from the gene
bank in association with inflammatory injury and oxidative stress,
i.e. microRNA-126 (miR-126) and microRNA-146a (miR-146a) (8,9). In this
study, expression levels of related factors in serum of patients
with coronary heart disease were measured, and their correlation
with CACS was analyzed for potential clinical application.
Patients and methods
Clinical information
A total of 192 patients diagnosed with coronary
heart disease who were admitted to The Third Affiliated Hospital of
Qiqihar Medical University (Qiqihar, China) from January 2018 to
December 2018 were recruited into observation group. Patients who
met following criteria were eligible for the study: Patients who
experienced precordial pain during physical exertion and rest, and
were diagnosed with coronary heart disease by coronary CT
angiography; and new patients who were not treated before. Patients
who met following criteria were excluded from this study: Patients
who had other heart conditions such as myocarditis and valvular
heart disease; patients who had rheumatic autoimmune diseases;
patients who had malignant tumors; and patients who dropped out of
the study halfway. In the observation group, there were 100 males
and 92 females aged 46-88 years with an average age of 60.1±7.2
years. A total of 69 volunteers were selected as the control group.
These volunteers underwent physical examination in the same period,
they were adults with no obvious organic disease after
cardiovascular system testing, and provided their blood samples. In
the control group, there were 39 males and 30 females aged 40-62
years with an average age of 56.2±6.9 years. This study met the
relevant requirements and was approved by the hospital ethics
committee. Patients and their families signed an informed consent
form.
Measurement of levels of IL-23, IL-35,
MDA and SOD
Approximately 3 ml of fasting venous blood were
taken from the subjects in the observation group in the morning
after diagnosis, whereas fasting venous blood samples were taken
from the control group in the morning, and were centrifuged at 300
x g at room temperature for 20 min. The supernatant was collected
and stored for analysis. ELISA was performed to measure serum
levels of IL-23 (ELISA kit #RLN2207 from Suzhou Ruiying
Biotechnology Co., Ltd.), SOD (ELISA kit #RLT4364 from Suzhou
Ruiying Biotechnology Co., Ltd.), IL-35 (ELISA kit #70-EK135-24
from Hangzhou Lianke Biotechnology Co., Ltd.) and MDA (ELISA kit
#70-ab30841-050 from Hangzhou Lianke Biotechnology Co., Ltd.),
respectively. The user manuals of these ELISA kits were strictly
followed for reliable measurements.
Measurement of levels of miR-126 and
miR-146a
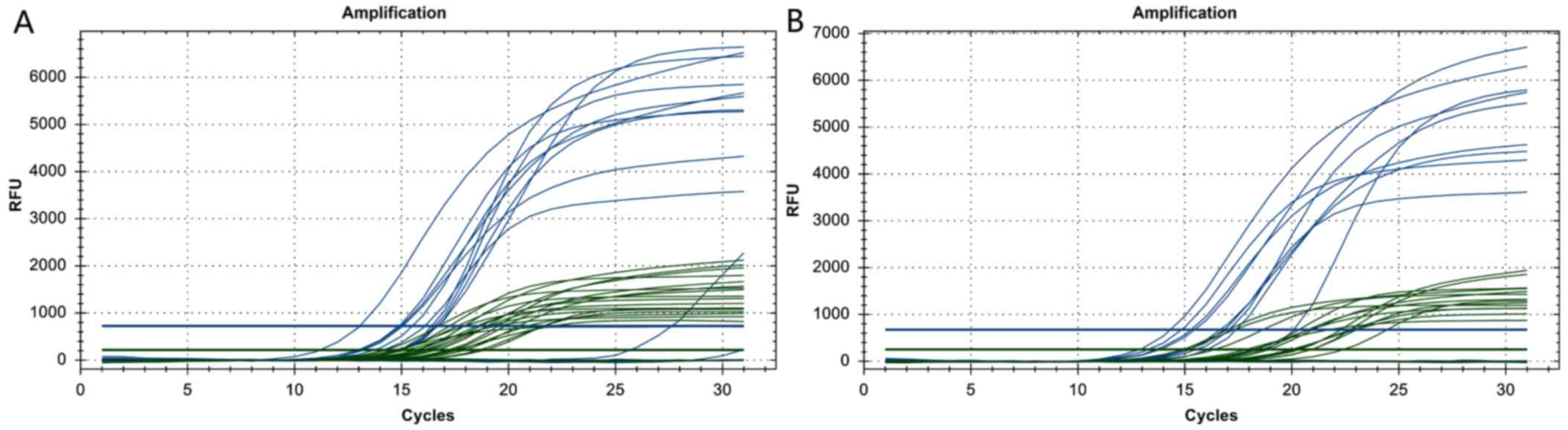
Total RNA was extracted, and cDNA was synthesized
via reverse transcription. Real-time fluorescence-based
quantitative PCR was performed using cDNA as a template to measure
levels of miR-126 and miR-146a. Mature sequences of miR-126 and
miR-146a were obtained from the miRNA database (www.mirbase.org), and primers were designed
accordingly. U6 was used as a reference gene. The primer sequences
were as follows: for miR-126 primer (60 bp long) the forward
sequence was 5'-GGG TGA GAA CTG AAT TCCA-3', and the reverse
sequence was 5'-CAG GTG GCG TCG TGG ATG-3'; for miR-146a primer (79
bp long) the forward sequence was 5'-GCA TAA CAC TAG AGG GTC CA-3',
and the reverse sequence was 5'-CAG GTG AAT TTC CCA GGT CGG-3'; and
for U6 primer (75 bp long), the forward sequence was 5'-GCT TCG GCA
CAT ATA CTA AAAA-3', and the reverse sequence was 5'-CGC TTC ACG
AAT TTG CGT GTCA-3'. The primers were synthesized by Suzhou Ruiying
Biotechnology Co., Ltd. The PCR kit was from Invitrogen; Thermo
Fisher Scientific, Inc. and Suzhou Ruiying Biotechnology Co., Ltd.
IQ5 PCR Instrument (Bio-Rad) was used. The PCR amplification
reaction was performed as follows: Pre-denaturation at 95˚C for 10
min, 10 cycles of 95˚C for 15 sec and 60˚C for 20 sec, followed by
another 35 cycles of 95˚C for 25 sec and 60˚C for 35 sec. The Ct
value was calculated for each sample, and the relative expression
level of the target gene was calculated using the 2-ΔΔCt
method.
CACS assessment method
Coronary CT angiography (CTA) was performed in all
patients using a Siemens SOMATOM Definition AS+ 64 Rows/128 Slices
CT scanner. The phase of cardiac cycle with the best vessel
visibility was chosen for image reconstruction. The image had a
slice thickness of 0.625 mm. The coronary arteries comprise the
left main trunk, the anterior descending branch, the circumflex
branch, and the right coronary artery. The scan covered the area
from the base to the apex of the heart. After data processing,
images were reconstructed at 55% of the R-R interval using B35f
convolution kernel, and the reconstructed slice thickness was 3 mm
with an increment of 3 mm. Detection and quantitative analysis of
coronary calcification plaques were performed using CaScoring
software. There are three methods: Agatston integral method (AS),
volume integral method (VS), and mass integration method (MS). The
areas of calcified plaques were marked in each branch of the
coronary arteries. AS, VS, MS of the left main trunk, the anterior
descending branch, the circumflex branch, and the right coronary
artery, as well as the total score, were obtained automatically.
The calcification of the diagonal branch belongs to the left
anterior descending branch, and the calcification of the obtuse
round branch belongs to the left circumflex. The sum of the above
four coronary artery calcification scores was calculated.
Statistical analysis
Statistical analysis was performed using the SPSS
17.0 software. The Chi-square test was used for comparison of
rates, and the odds ratio (OR) for the evaluation. OR=1 showed that
the factor had no effect, OR >1 indicated a risk factor, and OR
<1 indicated a protective factor. Mean ± standard deviation was
used for quantitative data (including ratio), Kolmogorov-Smirnov
was used to detect the normal distribution of data, and t-test for
comparison of normal distribution between two groups, analysis of
variance was used among multiple groups (SNK method for pairwise
comparison), and Mann-Whitney U test was to compare the non-normal
distribution between groups. Spearman correlation test were
conducted. A difference was statistically significant at
P<0.05.
Results
Comparison of IL-23 and IL-35
expression levels
As shown in Fig. 1,
IL-23 data in the two groups were normally distributed. The
differences in IL-23 (65.32±6.39 vs. 35.26±6.28 mg/l, t=8.31,
P=0.001) were statistically significant. The IL-35 data in the two
groups were not normally distributed, and the Mann-Whitney U test
was applied. The differences in IL-35 (75.26±6.84 vs. 99.36±9.21
mg/l, Z=12.298, P<0.001) were statistically significant.
Expression levels of both IL-23 and IL-35 in the observation group
were higher than those in the control group.
Comparison of MDA and SOD expression
levels
As shown in Fig. 2,
the data of MDA and SOD in the two groups were not normally
distributed, and Mann-Whitney U test was applied. The differences
in MDA (8.39±2.34 vs. 5.27±0.88 mg/l, Z=9.40, P<0.001) and SOD
(95.24±13.94 vs. 106.33±14.29 IU/l, Z=7.689, P<0.001) were
statistically significant. In the observation group, the MDA level
was higher while the SOD level was lower than the corresponding
level in the control group.
Comparison of expression levels of
miR-126 and miR-146a
As shown in Table I,
Figs. 3 and 4, the expression levels of miR-126 and
miR-146a in the observation group were significantly higher than
those in the control group. The difference in expression level of
miR-126 and miR-146a between the two groups were statistically
significant.
 | Table IComparison of expression levels of
miR-126 and miR-146a. |
Table I
Comparison of expression levels of
miR-126 and miR-146a.
| Items | Observation
group | Control group |
|---|
| Patient no. | 192 | 69 |
| miR-126 | 3.19±0.25 | 1.17±0.20 |
| t value | 4.11 | |
| P-value | 0.024 | |
| OR value | 3.87 | |
| 95% CI | 1.002-5.654 | |
| miR-146a | 4.28±0.54 | 1.38±0.49 |
| t value | 5.15 | |
| P-value | 0.011 | |
| OR value | 2.65 | |
| 95% CI | 1.452-3.062 | |
Comparison of levels of IL-23, IL-35,
MDA, SOD, miR-126 and miR-146a at different stages of disease
severity in the observation group
As shown in Table
II, the difference in levels of IL-23, IL-35, MDA, SOD, miR-126
and miR-146a in serum of patients with coronary heart disease at
different stages of severity was statistically significant.
 | Table IIComparison of levels of IL-23, IL-35,
MDA, SOD, miR-126 and miR-146a at different stages of disease
severity in the observation group. |
Table II
Comparison of levels of IL-23, IL-35,
MDA, SOD, miR-126 and miR-146a at different stages of disease
severity in the observation group.
| | Disease severity | | |
|---|
| Item | Single-vessel
disease | Two-vessel
disease | Three-vessel disease
and above | F-value | P-value |
|---|
| Case no. | 50 | 11230 | | | |
| IL-23 | 60.59±6.31 | 66.23±9.26 | 72.35±9.84 | 5.39 | 0.005 |
| IL-35 | 85.02±10.31 | 75.98±12.30 | 65.31±11.97 | 6.23 | <0.001 |
| MDA | 7.45±2.37 | 8.30±1.30 | 9.31±1.29 | 4.30 | 0.012 |
| SOD | 104.31±25.37 | 95.01±20.17 | 80.13±16.39 | 5.31 | 0.006 |
| miR-126 | 2.54±0.37 | 3.27±0.64 | 4.12±0.54 | 2.95 | 0.025 |
| miR-146a | 3.51±0.64 | 4.20±0.71 | 5.34±0.81 | 3.02 | 0.021 |
Correlation analysis between CACS and
level of IL-23, IL-35, MDA, SOD, miR-126 and miR-146a in the
observation group
As shown in Table
III, a Spearman correlation test was conducted and showed
positive correlation between CACS and IL-23, MDA, miR-126 and
miR-146a, respectively (P<0.05); while a negative correlation
existed between CACS and IL-35, SOD (P<0.05) in the observation
group.
 | Table IIICorrelation between CACS and related
biomarkers in serum of patients with coronary heart disease. |
Table III
Correlation between CACS and related
biomarkers in serum of patients with coronary heart disease.
| Biomarker | Correlation
coefficient (r) | P-value |
|---|
| IL-23 | 0.46 | 0.025 |
| IL-35 | -0.49 | 0.020 |
| MDA | 0.51 | 0.016 |
| SOD | -0.48 | 0.022 |
| miR-126 | 0.53 | 0.013 |
| miR-146a | 0.54 | 0.012 |
Discussion
Coronary atherosclerosis with calcification is the
result of disease progression of atherosclerotic plaques. In
clinic, the severity of atherosclerotic plaques is often used as an
important indicator of disease progression. Symptoms of coronary
heart disease are often not evident in its early development. When
the disease progresses to a more serious stage, it often leads to
myocardial infarction and arrhythmia in clinic. Therefore, an early
screening of the disease using objective indicators is important.
Detection and quantitative analysis of coronary calcification are
of great value in early diagnosis of the lesion and early
preventive intervention. Interleukins are a group of cytokines that
are involved in the formation of macrophages, and have obvious
effects on formation of cholesterol crystals. In addition, some
members of the interleukin family are involved in the body's
oxidative stress response, such as IL-17, IL-23 and IL-35, of which
IL-17 and IL-35 have the strongest effects. Jing et al
(10) reported that IL-23 was
upregulated in a mouse model of kidney injury and was associated
with the body's inflammatory response and oxidative stress
response. MDA and SOD are classic oxidative stress indicators. When
the body is in an oxidative stress state, there is an increase in
oxidation products such as MDA (11), which aggravate the damage to cells
and tissues. Moreover, oxidative stress also render the
deformability of neutrophils and weaken macrophages, induce
activation of nuclear factor and activated protein-1, and modulate
the release of inflammatory mediators. As a result, macrophages and
damaged cells are induced to release a large number of oxygen free
radicals and a variety of mediators, aggravating the imbalance of
local protease/anti-protease and oxidation/anti-oxidation, which
causes a vicious circle. In recent years, association of miRNA with
coronary heart disease and coronary atherosclerosis has drawn
considerable attentions from researchers. miRNAs are non-coding
small RNA molecules that regulate lipoprotein metabolism and are
associated with plaque formation (12). Both miR-126 and miR-146a are not only
involved in inflammatory response and oxidative stress response,
but also modulate macrophage functions (13).
The present study is CACS-related experimental
research, in which correlations between CACS and inflammatory
factors and related oxidative stress indicators were explored. The
results showed that expression levels of IL-23, MDA, miR-126 and
miR-146a were significantly higher, while the IL-35, SOD levels
were significantly lower in serum of patients with coronary heart
disease than those in the control group. Above findings suggested
that abnormal expression of IL-23, IL-35, MDA, SOD, miR-126 and
miR-146a is an important factor in promoting lesion formation.
IL-23 is an important pro-inflammatory cytokine involved in immune
response. IL-35 inhibits inflammatory response. Both are associated
with the modulating effects of IL-1 (14,15).
Studies have shown that overexpression of IL-1 can induce the
release of higher levels of IL-23 by hepatocytes and macrophages,
and cause disorders of lipid metabolism, triggering formation of an
inflammatory microenvironment (16,17). It
was also reported that IL-23 is overexpressed in local tissues of
atherosclerotic plaques, while IL-35 expression is low, suggesting
that IL-23 and IL-35 are associated with the formation of
atherosclerotic plaques (18,19). In
this study, the results showed that high expression of MDA and low
expression of SOD were not only associated with the formation of
atherosclerotic plaques, but also associated with the severity of
the lesions, suggesting that abnormal expression of both markers
may have some auxiliary significance for judging the extent of
lesions, and can promote onset and progression of coronary heart
disease. MDA and SOD are important indicators of oxidative stress
in the body. Abnormal expression of both indicators suggested that
the formation of atherosclerotic plaques may be associated with
oxidative stress. Abnormal expression of MDA and SOD can lead to
increased production of oxygen free radicals, aggravating local
damage of vascular endothelial cells. Under this condition,
platelets, granulation tissue and macrophages start to aggregate,
causing local abnormal lipid metabolism and accelerated formation
of plaques (20,21). Patients with coronary heart disease
may experience high oxidative stress locally or systemically,
leading to aggravated damage to local tissue of the arterial wall
and increased release of mediators after activation of nuclear
factors, including inflammatory mediators and oxygen free radicals.
This condition may render imbalanced local redox reaction and
promote disease progression. Treatments of coronary heart disease
targeting oxidative stress and inflammation may have some effects.
Although there are many factors that can modulate the release of
cytokines, miRNAs have drawn attention that it may be associated
with coronary heart disease. In this study, it was found that
miR-126 and miR-146a were associated with the formation and
severity of coronary heart disease. Our results were consistent
with the findings in literature, in which Wang et al
(22) found abnormal expression of
miR-126 in patient serum. In this study, a clear positive
correlation was found between CACS and miR-126 and miR-146a,
respectively, suggesting that miR-126 and miR-146a played important
roles in disease progression. Both miR-126 and miR-146a may be
promoting factors in disease formation (23,24),
exhibiting a modulating effect on local inflammatory
microenvironment and oxidative stress (25,26). In
particular, IL-35, as a pro-inflammatory factor, forms a ‘waterfall
effect’ to initiate the modulation of related cytokines (27-29).
Detection of expression of IL-23, IL-35, MDA, SOD, miR-126 and
miR-146a may offer a theoretical insight to diagnosis, prevention
and severity assessment of coronary heart disease.
In conclusion, biomarkers IL-23, IL-35, MDA, SOD,
miR-126 and miR-146a were abnormally expressed in serum of patients
with coronary heart disease, and were found to be correlated with
CACS. Detection of changes of related biomarkers in serum may have
certain values in diagnosis of disease formation, as well as
assessment of disease severity.
Acknowledgements
Not applicable.
Funding
The study was funded by a basic Scientific research
project from Heilongjiang Department of Education (no.
2018-KYYWF-0084).
Availability of data and materials
The datasets used and/or analyzed during the present
study are available from the corresponding author on reasonable
request.
Authors' contributions
DC, ML and YL conceived and designed the study. DC,
CJ, YS and DX were responsible for the collection and analysis of
the experimental data. DC and ML interpreted the data and drafted
the manuscript. CJ and YL revised the manuscript critically for
important intellectual content. All authors read and approved the
final manuscript.
Ethics approval and consent to
participate
The study was approved by the Ethics Committee of
The Third Affiliated Hospital of Qiqihar Medical University
(Qiqihar, China). Signed informed consents were obtained from the
patients.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Cameron SA, White SM, Arrollo D, Shulman
ST and Rowley AH: Arterial immune protein expression demonstrates
the complexity of immune responses in Kawasaki disease arteritis.
Clin Exp Immunol. 190:244–250. 2017.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Lo-Kioeng-Shioe M, Rijlaarsdam-Hermsen D,
van Domburg R, Hadamitzky M, Lima JAC, Hoeks SE, et al: Prognostic
value of coronary artery calcium score in symptomatic individuals:
A meta-analysis of 34,000 subjects. Int J Cardiol. 4:167–180.
2019.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Mitrokhin V, Nikitin A, Brovkina O,
Khodyrev D, Zotov A, Vachrushev N, Dragunov D, Shim A, Mladenov M
and Kamkin A: Association between IL-18/18R gene polymorphisms and
coronary artery disease: Influence of IL-18/18R genetic variants on
cytokine expression. J Inflamm Res. 11:1–9. 2018.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Liu X, Zhang R, Hou J, Wu J, Zhang M, Fang
S, Wang X, Huang X, Tian J, Li H, et al: Interleukin-35 promotes
early endothelialization after stent implantation by regulating
macrophage activation. Clin Sci (Lond). 133:869–884.
2019.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Hu X, Ma R, Lu J, Zhang K, Xu W, Jiang H
and Da Y: IL-23 promotes myocardial I/R injury by increasing the
inflammatory responses and oxidative atress eeactions. Cell Physiol
Biochem. 38:2163–2172. 2016.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Wei LF, Zhang HM, Wang SS, Jing JJ, Zheng
ZC, Gao JX, Liu Z and Tian J: Changes of MDA and SOD in brain
tissue after secondary brain injury with seawater immersion in
rats. Turk Neurosurg. 26:384–288. 2016.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Zhou Y, Wang ZF, Li W, Hong H, Chen J,
Tian Y and Liu ZY: Protective effects of microRNA-330 on amyloid
β-protein production, oxidative stress, and mitochondrial
dysfunction in Alzheimer's disease by targeting VAV1 via the MAPK
signaling pathway. J Cell Biochem. 119:5437–5448. 2018.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Cheleschi S, De Palma A, Pascarelli NA,
Giordano N, Galeazzi M, Tenti S and Fioravanti A: Could oxidative
stress regulate the expression of microRNA-146a and microRNA-34a in
human osteoarthritic chondrocyte cultures? Int J Mol Sci.
18(2660)2017.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Fang Y, Chen S, Liu Z, Ai W, He X, Wang L,
Xie P, Jiang B and Fang H: Endothelial stem cells attenuate cardiac
apoptosis via downregulating cardiac microRNA-146a in a rat model
of coronary heart disease. Exp Ther Med. 16:4246–4252.
2018.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Jing T, Liao J, Shen K, Chen X, Xu Z, Tian
W, Wang Y, Jin B and Pan H: Protective effect of urolithin a on
cisplatin-induced nephrotoxicity in mice via modulation of
inflammation and oxidative stress. Food Chem Toxicol. 129:108–114.
2019.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Baggott MJ, Garrison KJ, Coyle JR,
Galloway GP, Barnes AJ, Huestis MA and Mendelson JE: Effects of the
psychedelic amphetamine MDA (3,4-methylenedioxyamphetamine) in
healthy volunteers. J Psychoactive Drugs. 51:108–117.
2019.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Amr KS, Abdelmawgoud H, Ali ZY, Shehata S
and Raslan HM: Potential value of circulating microRNA-126 and
microRNA-210 as biomarkers for type 2 diabetes with coronary artery
disease. Br J Biomed Sci. 75:82–87. 2018.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Zha L, Li S, Liu X, Li Z, Jiang J, Huang L
and Yang Z: Association of miR-146a gene polymorphism at loci
rs2910164 G/C, rs57095329 A/G, and rs6864584 T/C with
susceptibility to Kawasaki disease in Chinese children. Pediatr
Cardiol. 40:504–512. 2019.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Staciwa M and Broncel M: The biological
function and significance of IL-35 in the pathogenesis of
atherosclerosis. Pol Merkur Lekarski. 44:161–164. 2018.PubMed/NCBI(In Polish).
|
|
15
|
Gorzelak-Pabiś P, Chalubinski M, Wojdan K,
Luczak E, Duraj I, Mozdzan M and Broncel M: Increased plasma
concentrations of interleukin 35 in patients with coronary artery
disease. Arch Med Sci. 13:778–784. 2017.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Zhu Z, Zhang Y, Ye J, Wang X, Fu X, Yin Y,
Wen J, Wu X and Xia Z: IL-35 promoted STAT3 phosphorylation and
IL-10 production in B cells, but its production was reduced in
patients with coronary artery diseases. Hum Immunol. 79:869–875.
2018.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Su Y, Feng S, Luo L, Liu R and Yi Q:
Association between IL-35 and coronary arterial lesions in children
with Kawasaki disease. Clin Exp Med. 19:87–92. 2019.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Shateri H, Fadaei R, Najafi M, Vatannejad
A, Teimouri M, Zali F, Emamgholipour S, Parvaz E, Asadnia M and
Doosti M: Circulating levels of IL-35 and gene expression of FoxP3
in coronary artery disease: Is there any interplay between them and
25-hydroxyvitamin D3? Clin Lab. 64:483–490. 2018.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Lin Y, Xue Y, Huang X, Lu J, Yang Z, Ye J,
Zhang S, Liu L, Liu Y and Shi Y: Association between interleukin-35
polymorphisms and coronary heart disease in the Chinese Zhuang
population: A case-control study. Coron Artery Dis. 29:423–428.
2018.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Musthafa QA, Abdul Shukor MF, Ismail NAS,
Mohd Ghazi A, Mohd Ali R, M Nor IF, Dimon MZ and Wan Ngah WZ:
Oxidative status and reduced glutathione levels in premature
coronary artery disease and coronary artery disease. Free Radic
Res. 51:787–798. 2017.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Spasojevic-Kalimanovska V,
Bogavac-Stanojevic N, Kalimanovska-Ostric D, Memon L, Spasic S,
Kotur-Stevuljevic J and Jelic-Ivanovic Z: Factor analysis of risk
variables associated with iron status in patients with coronary
artery disease. Clin Biochem. 47:564–569. 2014.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Wang X, Lian Y, Wen X, Guo J, Wang Z,
Jiang S and Hu Y: Expression of miR-126 and its potential function
in coronary artery disease. Afr Health Sci. 17:474–480.
2017.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Bastami M, Ghaderian SM, Omrani MD,
Mirfakhraie R, Vakili H, Parsa SA, Nariman-Saleh-Fam Z and Masotti
A: miRNA-related polymorphisms in miR-146a and TCF21 are associated
with increased susceptibility to coronary artery disease in an
Iranian population. Genet Test Mol Biomarkers. 20:241–248.
2016.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Khanaghaei M, Tourkianvalashani F,
Hekmatimoghaddam S, Ghasemi N, Rahaie M, Khorramshahi V, Sheikhpour
A, Heydari Z and Pourrajab F: Circulating miR-126 and miR-499
reflect progression of cardiovascular disease; correlations with
uric acid and ejection fraction. Heart Int. 11:e1–e9.
2016.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Zhou HY, Wei Q, Shi XD, Cao HY and Qin L:
miR-146a rs2910164 polymorphism might be associated with coronary
artery disease risk in Asians. Cell Mol Biol. 63:27–29.
2017.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Suchanek H, Myśliwska J, Siebert J,
Wieckiewicz J, Hak Ł, Szyndler K and Kartanowicz D: High serum
interleukin-18 concentrations in patients with coronary artery
disease and type 2 diabetes mellitus. Eur Cytokine Netw.
16:177–185. 2005.PubMed/NCBI
|
|
27
|
Lin Y, Huang Y, Lu Z, Luo C, Shi Y, Zeng
Q, Cao Y, Liu L, Wang X and Ji Q: Decreased plasma IL-35 levels are
related to the left ventricular ejection fraction in coronary
artery diseases. PLoS One. 7(e52490)2012.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Suh I, Oh KW, Lee KH, Psaty BM, Nam CM,
Kim SI, Kang HG, Cho SY and Shim WH: Moderate dietary fat
consumption as a risk factor for ischemic heart disease in a
population with a low fat intake: A case-control study in Korean
men. Am J Clin Nutr. 73:722–727. 2001.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Shateri H, Fadaei R, Najafi M, Vatannejad
A, Teimouri M, Zali F, Emamgholipour S, Parvaz E, Asadnia M and
Doosti M: Circulating levels of IL-35 and gene expression of FoxP3
in coronary artery disease: Is there any interplay between them and
25-Hydroxyvitamin D3. Clin Lab. 64:483–490. 2018.PubMed/NCBI View Article : Google Scholar
|