Introduction
Urinary calculus is one of the most common urinary
system diseases worldwide (1). A
previous study indicated an association between chronic kidney
disease and urinary calculus, regardless of stone location, and
demonstrated that urinary calculus leads to inflammation during
urinary tract infection (2).
Currently, extracorporeal shock wave lithotripsy is used as an
efficient technique for the treatment of urinary calculus (3-5). A
clinical investigation indicated that young patients with urinary
calculi were treated successfully, in a single procedure, using
pneumatic lithotripsy under ureteroscopy (6). A previous study evaluated the efficacy
of ureteroscopy and pneumatic lithotripsy in pregnant women with
urethral calculi, and this study also identified that lithotripsy
can be regarded as a safe and effective treatment for the mother
and the fetus (7).
Metallic ureteral stents (MUS) have been widely used
in the surgical treatment of ureteral obstruction and upper urinary
tract calculi (8). Chow et al
(9) demonstrated that MUS are
effective and safe to use in the treatment of non-urological
malignancies, abdominal ureteral obstruction and lymphatic
metastasis. Additionally, ureteral stent exchange is usually
performed under fluoroscopic and cystoscopic guidance, which is a
good option to use as an alternative to the cystoscopic procedure
or percutaneous procedure through percutaneous nephrostomy tract
for its plasticity and probability (9). Furthermore, MUS combined with
endoureterotomy has also been used as a therapeutic approach for
experimental ureteral stricture; however, this technique is not a
reliable therapeutic option for ureteral disorders due to failure
of these devices (10). Further
research is required to establish the application of MUS as a
treatment for urinary calculus.
In the present study, the efficacy of flexible
ureteroscopy lithotripsy combined (FURS) with MUS was assessed for
the treatment of upper urinary tract calculi. The present study
also analyzed the benefits between FURS-MUS and FURS in a total of
38 patients with upper urinary tract calculi.
Materials and methods
Patients
The present study was performed in The Fifth
Affiliated Hospital of Guangzhou Medical University (Guangzhou,
China) between August 2013 and December 2016. The mean age of
patients included in the current study was 42.4 years old (range,
28.6-56.4). A total of 38 patients with upper urinary tract calculi
were recruited and 24 male patients and 14 female patients were
included. All patients were not receiving any previous/ongoing
treatment at the time of enrollment. A total of 18 patients
received FURS and 20 patients received FURS-MUS. All patient
characteristics are summarized in Table
I. Patients with chronic renal failure and diabetes mellitus
were excluded from the current study. All patients were required to
exhibit calculi with diameters of <2 cm. The inclusion criteria
were as follows: i) Age >18 years old; ii) diagnosed upper
urinary tract calculi. The exclusion criteria were as follows: i)
Glomerular filtration rate <45; ii) a diagnosis of bladder or
prostate cancer; iii) claustrophobia; and iv) contraindications to
urological imaging. The clinical design of the present study was
approved by the ethics committee of the First Branch of the Fifth
Affiliated Hospital of Guangzhou Medical University (approval no.
20120418R). All patients provided informed consent.
 | Table ICharacteristics of patients with upper
urinary tract calculi. |
Table I
Characteristics of patients with upper
urinary tract calculi.
| Characteristics | FURS | FURS-MUS | P-value |
|---|
| Sex | | | |
|
Male | 10 | 13 | 0.035 |
|
Female | 8 | 7 | |
| Mean patient age,
years | 40.5 | 41.2 | 0.78 |
| Body mass index,
kg/m2 | 20.6±3.2 | 19.8±3.5 | 0.064 |
| Mean ureteral stone
diameter, mm | 0.153 | 0.162 | 0.65 |
| Stone opacity | | | |
|
Radio-opaque | 12 (66.67%) | 14 (70%) | 0.58 |
|
Radiolucent | 6 (33.33%) | 6 (30%) | 0.76 |
Surgical procedure
The methods of FURS and FURS-MUS were performed
under local anesthesia by urologists. The FURS protocol was
standardized to a previous study (11). The stone was positioned in the
excretory phase. The FURS procedures were performed using a 7.5-F
flexible ureterorenoscope (Karl Storz SE & Co.) through the
cystoscope under fluoroscopy. A Flexi-Tip Dual Lumen Ureteral
Access Catheter (Cook Medical) was used for insertion of a second
0.038-inch guidewire. A ureteral access sheath (9/11F or 12/14F;
Rapidia Tech Inc.) was subsequently used to insert the ureteroscope
into the ureter and disintegration was performed using a 200-micron
holmium laser fiber at an energy level of 0.5-0.8 J and at a rate
of 10-20 Hz. Stones located in the ureteropelvic junction were
pushed into the renal pelvis softly for disintegration. The
perfusion pressure of the irrigating fluid was <40 cm
H2O, and the irrigating fluid volume was <2,000 ml
for all patients during surgery. For FURS-MUS, MUS of 7.5 mm in
diameter, and 10.0-15.0 cm in length, were used to advance the
stent proximally in the bladder prior to FURS, as described
previously (12). A representative
FURS-MUS computed tomography (CT) scan image of one patient is
presented in Fig. 1(13).
Cytokine analysis
Blood samples (10 ml) were collected from each
patient, and serum was isolated via centrifugation at 8,000 x g for
10 min at 4˚C. Serum levels of interleukin (IL)-1β (cat. no.
RLB00), tumor necrosis factor-α (TNF-α; cat. no. RTA00), IL-6 (cat.
no. R6000B), IL-8 (cat. no. D8000C) and interferon-γ (IFN-γ; cat.
no. DIF50) were evaluated using commercial ELISA kits (all, R&D
Systems China Co., Ltd.), according to the manufacturer's
protocols.
Inflammation scoring system
Criteria for the evaluation of inflammation were
determined using an inflammation scoring system (14). Mean inflammation severity scores were
evaluated using the percentage of white blood cells, according to a
previous report (15). Inflammation
severity scores were evaluated as follows: Mild, 0-3; moderate,
4-7; severe, 8-10.
Measurement of parameters
The stone clearance rate was determined using the
number of residual stones/total number in each patients with upper
urinary tract calculi, as described previously (16). The occurrence of sepsis was
determined as organ dysfunction in the presence of proven or
suspected infection based on the Sepsis-3 guidelines (17). Blood loss was calculated during the
intraoperative period for patients who received FURS or FURS-MUS.
Readmission rate indicated by the amount of patients in need of
further treatment.
Complication rate analysis
A CT scan was performed for every patient prior to
surgery, and 24-48 h following surgery, to assess stone free
status. Stone opacity was classified based on preoperative plain
Kidney-Ureter-Bladder CT scan (18).
Stone recurrence was also assessed using a CT scan. The nephrostomy
tube was removed on postoperative day 3-4 when the drainage was
clear. The Double-J stent was extracted 1-2 weeks following
surgery.
Operative time and blood volume
The operative time was calculated from the time of
first incision to the placement of the nephrostomy tube. The blood
volume was calculated in a blood collection tube (TYK09; Chongqing
New World Trading Co., Ltd.).
Statistical analysis
All data are presented as the mean ± SEM. All
experiments were conducted in triplicate. Statistical analysis was
performed using Stata/SE software version 12.1 (StataCorp LP). A
Student's t-test was used to evaluate the differences between two
groups. Progression-free survival was analyzed using the
Kaplan-Meier method and the log-rank test. P<0.05 was considered
to indicate a statistically significant difference.
Results
Efficacy of FURS-MUS for operative
time in upper urinary tract calculi patients
The operative time between FURS-MUS and FURS in
patients with upper urinary tract calculi was assessed. The results
demonstrated that FURS-MUS shorted the mean operative time compared
with FURS in all 38 patients (35.2±1.2 vs. 57.4±1.7 min,
respectively; P<0.01: Table II).
This observation indicated that FURS-MUS is an efficient method for
the treatment of patients with upper urinary tract calculi.
 | Table IIEfficacy of FURS and FURS-MUS for the
treatment of patients with upper urinary tract calculi. |
Table II
Efficacy of FURS and FURS-MUS for the
treatment of patients with upper urinary tract calculi.
| Parameters | FURS | FURS-MUS | P-value |
|---|
| Operative time,
min | 57.4±1.7 | 35.2±1.2 | 0.0047 |
| Clearance rate,
% | 87.8 | 94.5 | 0.0360 |
| Postoperative
inflammation | 4.2±1.0 | 6.2±0.8 | 0.0326 |
| Blood loss, ml | 4.6±1.2 | 4.2±1.8 | 0.762 |
| Hospital stay,
days | 7.5±1.5 | 4.5±0.5 | 0.0378 |
| Complication rate,
% | 6.5 | 5.9 | 0.0826 |
Efficacy of FURS-MUS for clearance
rate in patients with upper urinary tract calculi
Clearance rate is an important indicator that is
used to evaluate the efficacy of lithotripsy treatment in patients
with urinary tract calculi (19). In
the current study, the clearance rate of FURS-MUS and FURS
treatment was analyzed in patients with upper urinary tract
calculi. An increased clearance rate was observed in the FURS-MUS
group compared with FURS (94.5 and 87.8%, respectively; P<0.05;
Table II). This result indicated
that FURS-MUS is more efficient in treating upper urinary tract
calculi.
Efficacy of FURS-MUS for postoperative
inflammation in patients with upper urinary tract calculi
Inflammation was analyzed in patients with upper
urinary tract calculi following FURS-MUS or FURS treatment. The
results indicated that FURS-MUS significantly increased
postoperative inflammation compared with FURS (Table II; 6.2±0.8 vs. 4.2±1.0 min,
respectively; P<0.05). However, blood loss exhibited no
significant difference between FURS-MUS and FURS (4.2±1.8 ml vs.
4.6±1.2 ml) in patients with upper urinary tract calculi (Table II). These results indicated that
FURS-MUS increased inflammation and decreased blood loss in
patients with upper urinary tract calculi.
Efficacy of FURS-MUS for hospital
stays in patients with upper urinary tract calculi
In the present study, the duration of hospital stay
and complication rate were investigated in patients with upper
urinary tract calculi. Data indicated that FURS-MUS treatment
decreased postoperative hospital stay duration compared with FURS
(4.5±0.5 vs. 7.5±1.5 day, respectively; P<0.05) for patients
with upper urinary tract calculi (Table
II). No significant difference was observed between the
complication rates of FURS-MUS and FURS (6.5% vs. 5.9%,
respectively) for patients with upper urinary tract calculi. These
data indicated that FURS-MUS decreased hospital stay duration, and
did increase complication rates in patients with upper urinary
tract calculi.
Efficacy of FURS-MUS for inflammatory
cytokines in patients with upper urinary tract calculi
Changes in inflammatory cytokines were recorded in
patients with upper urinary tract calculi. The results demonstrated
that FURS-MUS significantly decreased inflammatory cytokine
expression, including IL-1β, IL-6, IL-8 and IFN-γ expression,
compared with FURS in patients with upper urinary tract calculi
(Table III; IL-1β, IL-6, IL-8 and
IFN-γ, P<0.01). FURS-MUS also decreased TNF-α expression
(P<0.0203). These data suggested that FURS-MUS could decrease
inflammatory cytokine expression in patients with upper urinary
tract calculi.
 | Table IIIEfficacy of FURS-MUS in inflammatory
cytokine expression in patients with upper urinary tract
calculi. |
Table III
Efficacy of FURS-MUS in inflammatory
cytokine expression in patients with upper urinary tract
calculi.
| Cytokine | FURS | FURS-MUS | P-value |
|---|
| TNF-α, ng/l | 17.43±5.56 | 11.52±3.42 | 0.0203 |
| IL-1β, mg/l | 15.62±4.25 | 10.28±2.17 | 0.0048 |
| IL-6, mg/l | 18.42±5.46 | 11.30±2.75 | 0.0037 |
| IL-8, mg/l | 32.28±8.56 | 15.20±3.60 | 0.0010 |
| IFN-γ, mg/l | 42.36±8.82 | 26.17±5.07 | 0.0008 |
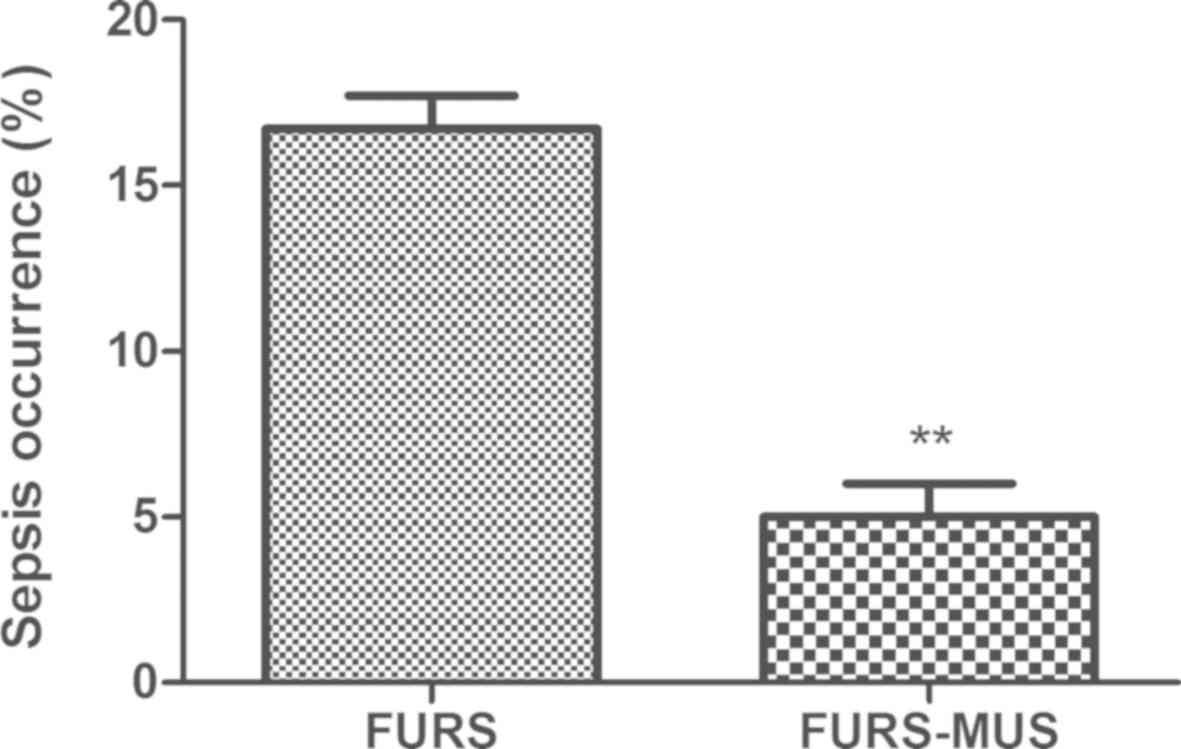
Readmission rate between FURS-MUS and
FURS groups
The differences in readmission rate were
investigated between the FURS-MUS and FURS-treated patient groups.
The unplanned readmission rate in FURS-MUS and FURS groups during a
period of 420 days are presented in Fig.
2. The readmission rate was 22.2% (n=4) and 10% (n=2) in the
FURS and FURS-MUS groups, respectively (P<0.01). The mean
interval between discharge from hospital and readmission was 15 and
24 days in the FURS and FURS-MUS group, respectively (Fig. 3; P<0.01). A total of three (16.7%)
patients exhibited sepsis in the FURS group, while only one patient
(5%) exhibited sepsis in the FURS-MUS group (Fig. 4; P<0.01). These data suggested
that FURS-MUS decreased readmission rate and the risk of sepsis in
patients with upper urinary tract calculi.
Stone recurrence between the FURS-MUS
and FURS groups
The stone recurrence was analyzed between the
FURS-MUS and FURS groups. The results demonstrated that stone
recurrence was 16.7% (n=3) and 5% (n=1) after 420 days in the FURS
and FURS-MUS groups, respectively (Fig.
5; P<0.01). The results also demonstrated that FURS-MUS
exhibited significantly higher progression-free survival rates than
patients who underwent FURS (66.67% vs. 85%, respectively;
P<0.05; Fig. 6). These data
indicated that FURS-MUS improved stone recurrence and
progression-free survival in patients with upper urinary tract
calculi.
Discussion
Currently, FURS is most commonly used in the
treatment of patients with proximal ureteral and renal calculi
(20). A previous study indicated
that ureteroscopic laser lithotripsy can be used as an effective
treatment modality for patients with spinal cord injury and with
upper urinary tract calculi (21).
Additionally, MUS can be used in the treatment of malignant
ureteral obstruction (22). In the
current study, the therapeutic effects of FURS-MUS in patients with
upper urinary tract calculi were investigated. The results
indicated that FURS-MUS is an efficient method for the treatment of
patients with upper urinary tract calculi.
FURS is a safe, highly efficient, minimally invasive
and reproducible operation for the removal of upper urinary tract
calculi in infants (23). The
current study indicated that auxiliary MUS contributed to the
treatment with FURS for patients with upper urinary tract calculi.
Data in the current study indicated that the FURS-MUS technique can
be used as a novel method for the treatment of upper urinary tract
calculi, and to aid in the rapid recovery of patients with upper
urinary tract calculi. The results demonstrated that FURS-MUS
decreased hospital stay duration and operative time, and increased
stone clearance rate. The current study also demonstrated that
FURS-MUS increased the stone clearance rate in patients with upper
urinary tract calculi compared with patients treated using FURS.
The FURS-MUS technique can be performed easily in all patient
cases. As compared with the FURS technique, FURS-MUS presents the
advantages of low postoperative inflammation and readmission
rates.
Postoperative inflammation is the most common
characteristic in patients with upper urinary tract calculi
(24). In the present study, it was
indicated that FURS-MUS increased postoperative inflammation
compared with FURS. This discrepancy in postoperative inflammation
rates between FURS and FURS-MUS was caused by MUS. A previous study
demonstrated that chronic inflammation is associated with the
volume of the prostate and storage symptoms, which may also be one
of the causes of lower urinary tract symptoms (25). The results of the current study
reported that FURS-MUS did not increase the complication rate for
patients with upper urinary tract calculi. The use of FURS-MUS
decreased complications and drawbacks compared with single FURS due
to the shortened operative time. Additionally, the blood loss was
not significantly different between the FURS-MUS and FURS
techniques. The results of the current study indicated that
FURS-MUS significantly decreased the inflammatory cytokines TNF-α,
IL-1β, IL-6, IL-8 and IFN-γ in patients with upper urinary tract
calculi, which may contribute to a shorter hospital stay duration
when compared with FURS. In all cases, FURS-MUS allowed for easy
access to the stone through a ureteral access sheath with minimal
tract dilation. Fewer perioperative complications were observed in
cases receiving FURS-MUS than in those receiving only FURS, and
this result provided new evidence of the efficacy of FURS-MUS use
in the treatment of upper urinary tract calculi.
A previous study revealed that patients with upper
urinary tract calculi are associated with an increased risk of
sepsis and mortality (26).
Therefore, decreasing the occurrence of postoperative sepsis is
beneficial for patients with urinary tract calculi. The results of
the current study indicated that FURS-MUS decreased the occurrence
of sepsis, which further led to the lower readmission rate than
that for FURS alone in patients with urinary tract calculi.
Additionally, FURS-MUS increased the mean interval between
discharge from hospital and readmission. A previous report
indicated that stone recurrence is a risk factor for patients with
urinary tract calculi and new stones can occur following surgery
(27). In the present study, the
results demonstrated that FURS-MUS significantly decreased stone
recurrence compared with FURS during a 420-day period, which
resulted in a higher progression-free survival rate compared with
patients who underwent FURS. However, other risk factors in
patients between the FURS-MUS and FURS groups need to be assessed
in future studies. Additionally, the present study used a small
number of cases. Therefore, in future studies, the efficacy of the
FURS-MUS technique should be identified in additional populations
of patients with upper urinary tract calculi.
In conclusion, the data in the current study
indicated that FURS-MUS represents a notable improvement for the
treatment of upper urinary tract calculi. FURS-MUS technique
increased postoperative inflammation and improved the operative
time, hospital stay duration, readmission rate, stone recurrence
and clearance rate for patients with upper urinary tract calculi.
These data provided evidence that FURS-MUS may have a specific role
in the range of urological treatments for patients with upper
urinary tract calculi, suggesting that FURS-MUS is reliable method
for the treatment of upper urinary tract calculi.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
TL designed experiments and wrote manuscript. XZS,
XL and YZH performed the experiments.
Ethics approval and consent to
participate
The Ethical Committee of the he Fifth Affiliated
Hospital of Guangzhou Medical University approved this study.
Written informed consent was provided by all patients.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Jia B, Wu Z and Gu C: Fragment of pubis
through the urinary bladder wall causing urinary bladder calculus.
Urol Res. 40:181–183. 2012.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Keller JJ, Chen YK and Lin HC: Association
between chronic kidney disease and urinary calculus by stone
location: A population-based study. BJU Int. 110:E1074–E1078.
2012.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Celik S, Bozkurt O, Kaya FG, Egriboyun S,
Demir O, Secil M and Celebi I: Evaluation of computed tomography
findings for success prediction after extracorporeal shock wave
lithotripsy for urinary tract stone disease. Int Urol Nephrol.
47:69–73. 2015.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Nakasato T, Morita J and Ogawa Y:
Evaluation of Hounsfield Units as a predictive factor for the
outcome of extracorporeal shock wave lithotripsy and stone
composition. Urolithiasis. 43:69–75. 2015.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Pereira-Arias JG, Gamarra-Quintanilla M,
Urdaneta-Salegui LF, Mora-Christian JA, Sánchez-Vazquez A,
Astobieta-Odriozola A and Ibarluzea-González G: Current status of
extracorporeal shock wave lithotripsy in urinary lithiasis. Arch
Esp Urol. 70:263–287. 2017.PubMed/NCBI(In Spanish).
|
|
6
|
Guo HQ, Li XG, Gan WD, Zeng LQ, Zhang ZW,
Sun XZ and Sun ZY: Clinical investigation of the treatment of
children urethral calculi with pneumatic lithotripsy under
ureteroscopy. Zhonghua Nan Ke Xue. 9:578–579. 2003.PubMed/NCBI(In Chinese).
|
|
7
|
Keshvari Shirvan M, Darabi Mahboub MR,
Rahimi HR and Seyedi A: The evaluation of ureteroscopy and
pneumatic lithotripsy results in pregnant women with urethral
calculi. Nephrourol Mon. 5:874–878. 2013.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Morcillo E, Fernández I, Pamplona M,
Sánchez-Margallo FM and Soria F: Metallic ureteral stents. Present
and future. Arch Esp Urol. 69:583–594. 2016.PubMed/NCBI(In Spanish).
|
|
9
|
Chow PM, Hsu JS, Wang SM, Yu HJ, Pu YS and
Liu KL: Metallic ureteral stents in malignant ureteral obstruction:
short-term results and radiological features predicting stent
failure in patients with non-urological malignancies. World J Urol.
32(3):729–736. 2014.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Soria F, Sun F, Duran E, Sánchez FM and
Usón J: Metallic ureteral stents versus endoureterotomy as a
therapeutic approach for experimental ureteral stricture. J Vasc
Interv Radiol. 16:521–529. 2005.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Aboutaleb H: Fluoroscopy free flexible
ureteroscopy with holmium: Yttrium-aluminium-garnet laser
lithotripsy for removal of renal calculi. Arab J Urol. 14:123–130.
2016.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Chow PM, Chiang IN, Chen CY, Huang KH, Hsu
JS, Wang SM, Lee YJ, Yu HJ, Pu YS and Huang CY: Malignant ureteral
obstruction: Functional duration of metallic versus polymeric
ureteral stents. PLoS One. 10(e0135566)2015.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Abdelhamid M, Mosharafa AA, Ibrahim H,
Selim HM, Hamed M, Elghoneimy MN, Salem HK, Abdelazim MS and Badawy
H: A prospective evaluation of high-resolution CT parameters in
predicting extracorporeal shockwave lithotripsy success for upper
urinary tract calculi. J Endourol. 30:1227–1232. 2016.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Davis WR, Halls JE, Offiah AC, Pilkington
C, Owens CM and Rosendahl K: Assessment of active inflammation in
juvenile dermatomyositis: A novel magnetic resonance imaging-based
scoring system. Rheumatology (Oxford). 50:2237–2244.
2011.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Pounis G, Bonaccio M, Di Castelnuovo A,
Costanzo S, de Curtis A, Persichillo M, Sieri S, Donati MB,
Cerletti C, de Gaetano G and Iacoviello L: Polyphenol intake is
associated with low-grade inflammation, using a novel data analysis
from the Moli-sani study. Thromb Haemost. 115:344–352.
2016.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Karakose A, Atesci YZ and Aydogdu O: The
stone formation in the Memotherm urethral stent implantation area:
Is it a rare complication? Can Urol Assoc J. 8:E213–E214.
2014.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Howitt SH, Herring M, Malagon I, McCollum
CN and Grant SW: Incidence and outcomes of sepsis after cardiac
surgery as defined by the Sepsis-3 guidelines. Br J Anaesth.
120:509–516. 2018.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Maghsoudi R, Etemadian M, Kashi AH and
Ranjbaran A: The association of stone opacity in plain radiography
with percutaneous nephrolithotomy outcomes and complications. Urol
J. 13:2899–2902. 2016.PubMed/NCBI
|
|
19
|
Jiang JT, Li WG, Zhu YP, Sun WL, Zhao W,
Ruan Y, Zhong C, Wood K, Wei HB, Xia SJ and Sun XW: Comparison of
the clinical efficacy and safety of retroperitoneal laparoscopic
ureterolithotomy and ureteroscopic holmium laser lithotripsy in the
treatment of obstructive upper ureteral calculi with concurrent
urinary tract infections. Lasers Med Sci. 31:915–920.
2016.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Andreoni C, Afane J, Olweny E and Clayman
RV: Flexible ureteroscopic lithotripsy: First-line therapy for
proximal ureteral and renal calculi in the morbidly obese and
superobese patient. J Endourol. 15:493–498. 2001.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Tepeler A, Sninsky BC and Nakada SY:
Flexible ureteroscopic laser lithotripsy for upper urinary tract
stone disease in patients with spinal cord injury. Urolithiasis.
43:501–505. 2015.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Goldsmith ZG, Wang AJ, Bañez LL, Lipkin
ME, Ferrandino MN, Preminger GM and Inman BA: Outcomes of metallic
stents for malignant ureteral obstruction. J Urol. 188:851–855.
2012.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Li J, Xiao J, Han T, Tian Y, Wang W and Du
Y: Flexible ureteroscopic lithotripsy for the treatment of upper
urinary tract calculi in infants. Exp Biol Med (Maywood).
242:153–159. 2017.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Prstojevic JK, Junuzovic D, Hasanbegovic
M, Lepara Z and Selimovic M: Characteristics of calculi in the
urinary tract. Materia Sociomed. 26:297–302. 2014.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Kim SH, Jung KI, Koh JS, Min KO, Cho SY
and Kim HW: Lower urinary tract symptoms in benign prostatic
hyperplasia patients: Orchestrated by chronic prostatic
inflammation and prostatic calculi? Urol Int. 90:144–149.
2013.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Badia M, Iglesias S, Serviá L, Domingo J,
Gormaz P, Vilanova J, Gavilan R and Trujillano J: Mortality
predictive factors in patients with urinary sepsis associated to
upper urinary tract calculi. Med Intensiva. 39:290–297.
2015.PubMed/NCBI View Article : Google Scholar : (In Spanish).
|
|
27
|
Noe HN: Hypercalciuria and pediatric stone
recurrences with and without structural abnormalities. J Urol.
164:1094–1096. 2000.PubMed/NCBI View Article : Google Scholar
|