Introduction
The current study outlines an outbreak of severe
acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection
caused the coronavirus disease 2019 (COVID-19) that was firstly
reported in Wuhan, Hubei Province, China. COVID-19 rapidly spread
to other cities in China and across the world subsequent to the
initial outbreak (1,2). On January 30, 2020, the International
Health Regulations Emergency Committee of World Health Organization
(WHO) declared that the epidemic caused by the new coronavirus had
become a ‘public health emergency of international concern’
(3). WHO subsequently declared a
pandemic as the number of infections increased exponentially around
the world.
As of April 3, 2020, the number of confirmed
COVID-19 infections worldwide was 972,303 and number of deaths was
50,322, with a total of 213,600 confirmed cases and 4,793 deaths
being reported in the United States of America (4). Currently, with the rapid spread of
COVID-19 around the world, researchers are rapidly increasing the
development of vaccines and screening of effective therapeutic
drugs (5,6). Despite this, the number of new cases
and deaths is still increasing with the evolution of the outbreak.
The cytokine storm, which can lead to acute respiratory distress
syndrome (ARDS) or multiple-organ failure, is an important factor
that causes COVID-19 exacerbation or mortality (7). It is particularly important to
diagnosis COVID-19 early and identify biomarkers that can predict
the severity and recovery of the disease.
Serum amyloid A (SAA) is a plasma component and the
precursor of amyloid. SAA is an acute-phase protein and is mainly
produced by the liver in response to proinflammatory cytokines that
are secreted by the activated monocytes (8). SAA serves an important role in
inflammation and relates to the severity of inflammation (8). Yip et al (9) suggested that SAA could monitor the
extent of pneumonia in severe acute respiratory syndrome (SARS)
using protein chip array profiling. Currently, there are few
reports about the relationship between SAA and COVID-19. The aims
of the present study were to evaluate the value of SAA in COVID-19,
and compare the efficacy of SAA and C-reactive protein (CRP) in
predicting the severity and recovery of COVID-19.
Materials and methods
Patients and study design
The study was reviewed and approved by Institutional
Review Board of Wuhan No.1 Hospital. The participants in the
retrospective study were patients diagnosed with COVID-19 at Wuhan
No.1 Hospital located in the Qiaokou District. Data were collected
from patients hospitalized from January 21, 2020 to March 4, 2020.
Upon admission, the patients were diagnosed with COVID-19 using
reverse transcription-quantitative (RT-q) PCR, according to WHO
guidance (10). During
hospitalization, 3 ml fasting venous blood was collected in the
morning, and the serum sample was separated via high-speed
centrifugation at room temperature for 10-15 min at 2,000 x g. The
serum CRP and SAA levels were measured via immunoturbidimetry using
a Siemens BN-II analyzer (Siemens Healthineers) and
immunofluorescence chromatography using an AFS2000A analyzer (Henan
Wayray Biotech Co., Ltd.), respectively. The inclusion criteria
were as follows: i) A positive COVID-19 nucleic acid test; ii) A
lung CT exhibiting multiple patchy ground glass shadows or other
typical manifestations of both lungs; iii) Serum CRP and SAA levels
detected at least three times during hospitalization. The exclusion
criteria were as follows: i) Positive tests for other pathogens
such as Tuberculosis, Mycoplasma; ii) Those diagnosed with
autoimmune disorders; iii) Those diagnosed with arthritic diseases;
iv) Cancer patients and those with severe underlying diseases; v)
Patients with severe cognitive impairment who cannot follow
instructions to complete the treatment; vi) Individuals with
missing critical data. A total of 35 patients were enrolled in the
present study. Patient characteristics are presented in Table I.
 | Table IClinical characteristics of 35
patients with COVID-19 upon admission. |
Table I
Clinical characteristics of 35
patients with COVID-19 upon admission.
| Variables | Total (n=35) | Mild group
(n=22) | Severe group
(n=13) | P-value |
|---|
| Age, years | 47.94±15.00 | 40.77±9.06 | 60.08±15.51 | <0.001 |
| Sex (n, %) | | | | |
|
Male | 13 (37.1) | 11 (50.0) | 2 (15.4) | 0.070 |
|
Female | 22 (62.9) | 11 (50.0) | 11 (84.6) | |
| Signs and symptoms on
admission (n, %) | | | | |
|
Fever | 28 (80.0) | 18 (81.8) | 10 (76.9) | >0.999 |
|
Cough | 21 (60.0) | 10 (45.5) | 11 (84.6) | 0.034 |
|
Expectoration | 9 (25.7) | 3 (13.6) | 6 (46.2) | 0.050 |
|
Sore
throat | 9 (25.7) | 6 (27.3) | 3 (23.1) | >0.999 |
|
Dizziness
and headache | 10 (28.6) | 9 (40.9) | 1 (7.7) | 0.055 |
|
Muscle
soreness | 16 (45.7) | 9 (40.9) | 7 (53.8) | 0.503 |
|
Fatigue | 13 (37.1) | 9 (40.9) | 4 (30.8) | 0.721 |
|
Inappetence | 13 (37.1) | 9 (40.9) | 4 (30.8) | 0.721 |
|
Chest
tightness | 2 (5.7) | 0 (0) | 2 (15.4) | 0.131 |
|
Shortness of
breath | 5 (14.3) | 1 (4.5) | 4 (30.8) | 0.052 |
|
Diarrhea | 2 (5.7) | 1 (4.5) | 1 (7.7) | >0.999 |
| Comorbidity (n,
%) | | | | |
|
Hyperlipidemia | 1 (2.9) | 1 (4.5) | 0 (0) | >0.999 |
|
Diabetes | 3 (8.9) | 0 (0) | 3 (23.1) | 0.044 |
|
Hypertension | 5 (14.3) | 0 (0) | 5 (38.5) | 0.004 |
|
COPD | 1 (2.9) | 0 (0) | 1 (7.7) | 0.371 |
|
Cerebrovascular
disease | 1 (2.9) | 0 (0) | 1 (7.7) | 0.371 |
|
Chronic
hepatitis B virus infection | 2 (5.7) | 2 (9.1) | 0 (0) | 0.519 |
Detection of SARA-CoV-2
A throat swab was obtained from each patient. A
total of 200 µl throat swab from each patient was used to extract
total RNA. On the basis of the manufacturer's protocol, total RNA
was extracted using the Viral Nucleic Acid isolation kit (cat. no.
SDK60104) from BioPerfectus Technologies. To target the
nucleocapsid (N) and open reading frame lab (ORF1ab) genes, the
SARS-CoV-2 Fluorescent PCR kit was used (cat. no. GN7103109;
Maccura Biotechnology, Co., Ltd.), according to the manufacturers
protocol. The thermocycling conditions of RT-qPCR were as follows:
55˚C for 15 min and 95˚C for 2 min, followed by 40 cycles of
amplification at 95˚C for 15 sec and 58˚C for 35 sec. The primers
were as follows: N forward, 5'-GGGGAACTTCTCCTGCTAGAAT-3' and
reverse, 5'-CAGACATTTTGCTCTCAAGCTG-3'; ORF1ab forward,
5'-CCCTGTGGGTTTTACACTTAA-3' and reverse, 5'-ACGATTGTGCATCAGCTGA-3'.
Negative and positive control samples were included in the
SARS-CoV-2 Fluorescent PCR kit. The result was judged based on the
absolute cycle threshold (Ct) value of each sample. The test
results of SARS-CoV-2 were reported as positive (Ct ≤38) and
negative (Ct >38) (11). The
nucleic acid test was considered positive if the results of the
samples were positive. If results were negative, the samples would
be taken once a day for the next 2 days.
Data collection
Clinical information, including clinical symptoms,
medical history, laboratory blood routine, and serum CRP and SAA
levels were collected 1-2 days after admission. The patients were
divided into mild and severe groups according to the WHO guidance
(10). The mild group had clinical
symptoms of fever, fatigue, cough, anorexia, malaise, muscle pain,
sore throat, dyspnea, nasal congestion and headache. The severe
group had respiratory distress, respiratory rate (RR) ≥30 beats/min
in a resting state, a mean oxygen saturation of ≤93% and an
arterial blood oxygen partial pressure (PaO2)/oxygen
concentration (FiO2) ≤300 mmHg. The criteria for
clinical recovery was at least two consecutive negative RT-PCR
tests and ameliorated clinical symptoms.
Statistical analysis
Continuous variables of normal distribution were
expressed as the mean ± standard deviation and parameters between
the mild and severe group were compared using an independent sample
t-test. Continuous variables of skewed distribution were presented
as the median [interquartile range (IQR)] and the parameters
between the mild and severe group were compared using a
Mann-Whitney U test. Categorical values were expressed as
frequencies, and the differences were analyzed using Fisher's exact
test. A two-way ANOVA analysis was used to compare the serum CRP
and SAA levels between the mild and severe group. The Logistic
regression analysis and the area under curve (AUC) of the receiver
operator characteristic (ROC) curve were calculated to determine
the probability for predicting the severity of COVID-19. The
optimal cut-off points to predict the severity of COVID-19 were
determined by Youden's index of ROC (12). Linear regression was used to analyze
the relationship between the serum CRP, SAA levels and treatment
days in recovered patients. The Logistic regression analysis and
the AUC of the ROC curve were calculated to determine the
probability for predicting the recovery of COVID-19. The optimal
cut-off points to predict the recovery of COVID-19 were determined
by Youden's index of ROC. P<0.05 was considered to indicate a
statistically significant difference. All analyses were performed
using SPSS 23.0 software (IBM Corp.).
Results
Clinical characteristics of patients
with COVID-19 on admission
Within the 35 hospitalized patients included, 13
(37.1%) and 22 (62.9%) cases were categorized into severe and mild
groups, respectively. The mean age of patients was 47.9±15.0 years
old, and 13 (37.1%) cases were male (Table I). Compared with the mild group, the
severe group was significantly older (mean age 60.1±15.5 years vs.
40.8±9.1 years; P<0.001) and was more likely to exhibit a cough
[11 (84.6%) vs. 10 (45.5%)], diabetes [3 (23.1%) vs. 0 (0%)],
hypertension [5 (38.5%) vs. 0 (0%); Table I]. The most common symptoms of
illness onset were fever (80.0%), cough (45.8%), muscle soreness
(45.7%), fatigue (37.1%), inappetence (37.1%), dizziness and
headache (28.6%), expectoration (25.7%), sore throat and (25.7%),
shortness of breath (14.3%), chest tightness (5.7%) and diarrhea
(5.7%).
Laboratory findings of patients with
COVID-19 on admission
The lymphocyte count in the severe group was
significantly lower compared with the mild group. Among them, the
lymphocyte count in the severe group was lower than the normal
range, while the lymphocyte count of the mild group was within the
normal range (Table II). The
eosinophil count was lower compared with the normal range, but
there was no significant difference in the two groups. The serum
CRP and SAA levels of the patients were above the upper bound of
the normal range, and they were significantly higher in the severe
group. The counts of white blood cell, platelet, neutrophil and
monocyte were normal for all patients, and there were no
significant difference in the two groups (Table II).
 | Table IILaboratory data, CRP and SAA of 35
patients with COVID-19 upon admission. |
Table II
Laboratory data, CRP and SAA of 35
patients with COVID-19 upon admission.
| Variable | Normal range | Total | Mild group | Severe group | P-value |
|---|
| White blood cell
count (x109/l) | 3.50-9.50 | 4.50±1.78 | 4.80±1.31 | 4.00±2.36 | 0.204 |
| Platelet count
(x109/l) | 125-350 | 165.69±55.86 | 158.59±49.4 | 177.69±65.73 | 0.336 |
| Neutrophil count
(x109l) | 1.8-6.3 | 3.03±1.63 | 3.14±1.22 | 2.85±2.21 | 0.620 |
| Lymphocyte count
(x109/l) | 1.1-3.2 | 1.01±0.36 | 1.15±0.34 | 0.76±0.26 | 0.001 |
| Monocyte count
(x109/l) | 0.1-0.6 | 0.42±0.23 | 0.47±0.21 | 0.35±0.24 | 0.155 |
| Eosinophil count
(x109/l) | 0.02-0.52 |
0.01(0.01,0.04) |
0.01(0.01,0.03) | 0.01(0,0.08) | 0.832 |
| CRP (mg/l) | 0.0-5.0 | 21.12±23.92 | 12.95±11.08 | 34.93±32.84 | 0.035 |
| SAA (mg/l) | 0.0-10.0 | 110.03±61.04 | 89.78±54.75 | 144.29±57.33 | 0.009 |
Dynamic changes of CRP and SAA in
patients with COVID-19
Two-way ANOVA analysis demonstrated that disease
severity had statistical significance at the SAA level (F=7.789;
P=0.006) and CRP level (F=16.110; P<0.001) (data not shown). The
severe group exhibited higher CRP and SAA levels than the mild
group. Dynamic changes of CRP and SAA levels were presented in
Fig. 1. As presented in Fig. 2, Linear regression analysis
demonstrated that the CRP and SAA levels were negatively correlated
with treatment days in recovered patients (r=-0.761, -0.795,
respectively).
Effects of CRP and SAA on the
occurrence of the severe COVID-19
The severe COVID-19 was used as the dependent
variable (yes=1, no=0), and CRP and SAA were used as independent
variables for Logistic regression analysis. CRP [OR=1.052 (95% CI
1.007, 1.099), P=0.023], SAA [OR=1.019 (95% CI 1.000, 1.038),
P=0.049] were independent risk factors for the severity of COVID-19
(Table III). The regression
equation used was: Logit (P)=-4.692+0.051(CRP)+0.019(SAA), which
was statistically significant (χ2=17.04, P<0.001
(data not shown), and the prediction accuracy was 74.3%.
 | Table IIIAnalysis on the occurrence of severe
COVID-19 in CRP and SAA. |
Table III
Analysis on the occurrence of severe
COVID-19 in CRP and SAA.
| Value | B | SE | Wald | P-value | OR (95% CI) |
|---|
| CRP | 0.051 | 0.022 | 5.161 | 0.023 | 1.052 (1.007,
1.099) |
| SAA | 0.019 | 0.010 | 3.872 | 0.049 | 1.019 (1.000,
1.038) |
| Constant | -4.692 | 1.742 | 7.258 | 0.007 | |
The ROC curve was used to analyze the early-warning
efficiency and the optimal prediction threshold of COVID-19
intensification. The corresponding AUC of CRP and SAA was 0.804 and
0.818, respectively (Fig. 3). The
optimum critical point of CRP and SAA was 29.5 and 157.9 mg/l,
respectively (Table IV), which was
the upper limit of mild COVID-19. When CRP was over 29.5 mg/l, the
severity of COVID-19 could be predicted, with sensitivity and the
specificity of 61.5 and 90.9%, respectively. The severity of
COVID-19 was predicted when SAA was over 157.9 mg/l, with the
sensitivity and the specificity of 84.6 and 77.4%,
respectively.
 | Table IVAnalysis of the effectiveness of CRP
and SAA for predicting the occurrence of the severe COVID-19. |
Table IV
Analysis of the effectiveness of CRP
and SAA for predicting the occurrence of the severe COVID-19.
| Value | CRP | SAA |
|---|
| Sensitivity % | 61.5 | 84.6 |
| Specificity % | 90.9 | 77.4 |
| Youden index % | 52.5 | 61.9 |
| Cut-off points | >29.5 | >157.9 |
Effects of CRP and SAA for predicting
the recovery of COVID-19
The recovered COVID-19 was used as the dependent
variable (yes=1, no=0), and CRP and SAA were used as independent
variables for Logistic regression analysis. SAA [OR=0.968 (95% CI
0.945, 0.990), P=0.005] was an independent factor for predicting
the recovery of COVID-19. However, CRP [OR=0.791 (95% CI 0.615,
1.016), P=0.067] could not predict the recovery of COVID-19
(Table V).
 | Table VAnalysis CRP and SAA for predicting
the recovery of COVID-19. |
Table V
Analysis CRP and SAA for predicting
the recovery of COVID-19.
| Value | B | SE | Wald | P-value | OR (95% CI) |
|---|
| CRP | -0.235 | 0.128 | 3.361 | 0.067 | 0.791 (0.615,
1.016) |
| SAA | -0.033 | 0.012 | 7.776 | 0.005 | 0.968 (0.945,
0.990) |
| Constant | 3.249 | 0.864 | 14.155 | 0.000 | |
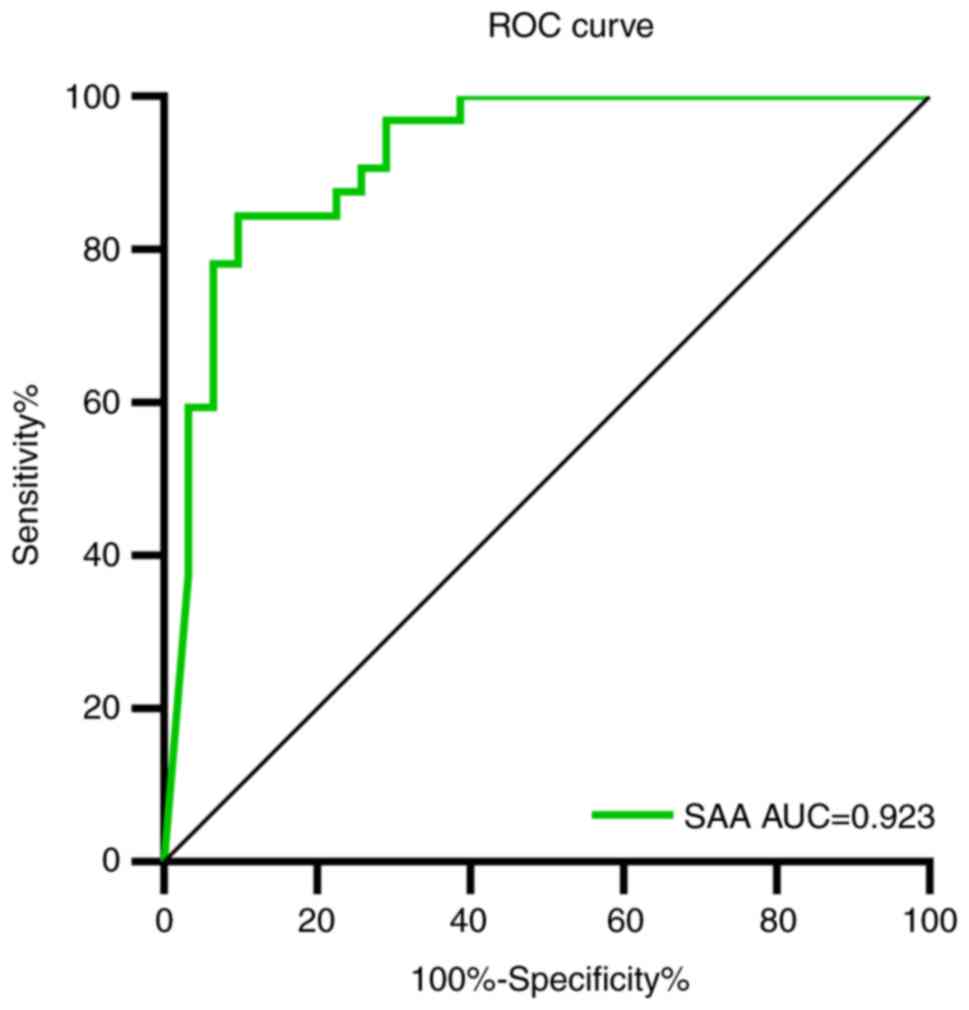
The ROC curve was used to analyze the early-warning
efficiency and the optimal prediction threshold of COVID-19
amelioration. The corresponding AUC of SAA was 0.923 (Fig. 4). The optimum critical point of SAA
was 27.7 mg/l, which was the upper limit of recovered patients.
When SAA was over 27.7 mg/l, the recovery of COVID-19 could be
predicted, with a sensitivity and specificity of 84.4 and 90.3%
respectively.
Discussion
The current study reported a cohort of 35 patients
with laboratory confirmed COVID-19. Within this cohort, the severe
group was older and had more comorbidities (such as diabetes,
hypertension) compared with the mild group, which was consistent
with previous research (13-17).
Fever, cough, muscle soreness, fatigue, inappetence, dizziness and
headache were the most common symptoms in patients with COVID-19,
and a cough was more common in the severe group compared with the
mild group. The primary symptoms were fever (80.0%) and cough
(60.0%), which are consistent with the results of recent research
(18,19).
The present study reported the results of blood
routine, and inflammation-related biomarkers of the patients with
COVID-19 upon hospital admission. The results indicated that white
blood cell, platelet, neutrophil, monocyte and eosinophil counts
were not significantly different between the severe group and the
mild group. White blood cell (severe group,
4.80±1.31x109/l; mild group, 4.00±2.36x109/l)
and neutrophil (severe group, 3.14±1.22x109/l; mild
group, 2.85±2.21x109/l) counts were close to the bottom
of the normal range. Lymphocyte counts were significantly lower in
the severe group. Eosinophil counts of the two groups were lower
than the normal range. These results suggested that a substantial
decrease in the total number of lymphocytes indicated that
coronavirus consumed many immune cells and inhibited the body's
cellular immune function (20,21). CRP
and SAA levels were significantly higher in the severe group upon
admission. The high CRP level was consistent with the results
gained by a recent study (22).
A two-way ANOVA result indicated the CRP and SAA
levels of the severe group were higher compared with the mild
group. Logistic regression analysis revealed that CRP and SAA
levels could predict severe COVID-19. ROC curve was used to analyze
the efficiency of CRP and SAA for predicting severe COVID-19. The
AUC of CRP and SAA were 0.804 and 0.818, respectively, which were
both higher than 0.800, indicating a high prediction efficiency.
The optimal cut-off point for CRP and SAA were 29.5 and 157.9 mg/l,
both of which had high sensitivity and specificity, indicating that
the cut-off point can be used to guide early clinical warnings of
severe COVID-19. In addition, the AUC of SAA was higher compared
with CRP, demonstrating that SAA was more efficient in predicting
severe COVID-19 than CRP.
A Linear regression result indicated the CRP and SAA
levels were negatively correlated with treatment days in the
recovered patients. Logistic regression results showed that the
P-value of CRP was 0.067, close to 0.05. It was hypothesized that
CRP may also be able to predict the recovery of COVID-19. Due to
the small sample size, CRP had no significance in the current
study. In future, the sample size should be expanded to further
verify the role of CRP in predicting COVID-19 rehabilitation.
However, although the sample size was small, SAA was indicated to
significantly predict recovery of COVID-19. These results suggested
that SAA was more accurate to reflect the recovery of patients with
COVID-19 than CRP. A ROC curve was used to analyze the efficiency
of SAA in predicting the recovery of COVID-19. The AUC of SAA was
0.923, which confirmed the high prediction efficiency. The optimal
cut-off point for SAA was 27.7 mg/l, with high sensitivity (84.4%)
and specificity (90.3%), indicating that the cut-off point could be
used to distinguish whether the patient had recovered and reached
the discharge standard. The majority of diagnostic tests exhibit
false positives. The false-positive results were expected to
increase with i) decreasing sample size; ii) increasing pursuit of
novelty; iii) various forms of multiple testing and researcher
flexibility; and iv) incorrect P-values (23). Therefore, it was necessary to combine
multiple testing methods for diagnosis to reduce misdiagnosis in
the clinic. This test was not used for the diagnosis of the
severity and recovery of COVID-19, and instead provided early
warning information for clinician to judge the outcome of the
disease.
The current study has a number of limitations.
First, the sample size was relatively small in a single center, and
a large sample with multicenter data should be used to validate the
results of the current study. Second, data of healthy patients were
lacking as blank controls due to the outbreak of the epidemic.
Finally, the current study was retrospective as not every patient
could be hospitalized in time for corresponding treatment in severe
epidemic areas. Due to the shortage in medical service in the early
stage of outbreak, some patients were self-isolated at home and
could not be admitted immediately. Therefore, the CRP and SAA
levels may have been affected upon admission. These limitations
need to be overcome in further research. However, the primary
results of the current study provided moderate yet important
information that can be used to predict COVID-19 outcome.
In conclusion, the CRP and SAA levels were higher in
the severe group, and SAA was more efficient in predicting severe
COVID-19 than CRP. For recovered patients, the CRP and SAA levels
were negatively correlated with treatment days, and SAA had a high
prediction efficiency for the recovery of COVID-19. These results
indicated that SAA may be considered to be a biomarker for
predicting the severity and recovery of COVID-19. Therefore, SAA
can be used for early warning of a poor outcome from COVID-19, as
well as monitoring the recovery process, which has important
clinical value.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
JF, PH and DZ designed the current study. JF, SZ, QY
and RH collected the clinical and laboratory data. PH, HL and YY
analyzed the data. JF, PH, SZ and DZ wrote the manuscript. All
authors read and approved the final manuscript.
Ethics approval and consent to
participate
The current study was approved by the Institutional
Review Board of Wuhan No. 1 Hospital. All data were anonymized to
comply with the provisions of personal data protection legislation.
Due to the retrospective nature of this study and due the fact that
only historical medical data were collected, written informed
consent was not required.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Huang C, Wang Y, Li X, Ren L, Zhao J, Hu
Y, Zhang L, Fan G, Xu J, Gu X, et al: Clinical features of patients
infected with 2019 novel coronavirus in Wuhan, China. Lancet.
395:497–506. 2020.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Zhu N, Zhang D, Wang W, Li X, Yang B, Song
J, Zhao X, Huang B, Shi W, Lu R, et al: A novel coronavirus from
patients with pneumonia in China, 2019. N Engl J Med. 382:727–733.
2020.PubMed/NCBI View Article : Google Scholar
|
|
3
|
World Health Organization: Statement on
the second meeting of the international health regulations (2005)
emergency committee regarding the outbreak of novel coronavirus
(2019-nCoV), 2020.
|
|
4
|
World Health Organization: Coronavirus
disease 2019 (COVID-19) situation report-74, 2020.
|
|
5
|
Calina D, Docea AO, Petrakis D, Egorov AM,
Ishmukhametov AA, Gabibov AG, Shtilman MI, Kostoff R, Carvalho F,
Vinceti M, et al: Towards effective COVID-19 vaccines: Updates,
perspectives and challenges (Review). Int J Mol Med. 46:3–16.
2020.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Nitulescu GM, Paunescu H, Moschos SA,
Petrakis D, Nitulescu G, Ion GND, Spandidos DA, Nikolouzakis TK,
Drakoulis N and Tsatsakis A: Comprehensive analysis of drugs to
treat SARS-CoV-2 infection: Mechanistic insights into current
COVID-19 therapies (Review). Int J Mol Med. 46:467–488.
2020.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Ye Q, Wang B and Mao J: The pathogenesis
and treatment of the ‘Cytokine Storm’ in COVID-19. J Infect.
80:607–613. 2020.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Vietri L, Fui A, Bergantini L,
d'Alessandro M, Cameli P, Sestini P, Rottoli P and Bargagli E:
Serum amyloid A: A potential biomarker of lung disorders. Respir
Investig. 58:21–27. 2020.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Yip TT, Chan JW, Cho WC, Yip TT, Wang Z,
Kwan TL, Law SC, Tsang DN, Chan JK, Lee KC, et al: Protein chip
array profiling analysis in patients with severe acute respiratory
syndrome identified serum amyloid a protein as a biomarker
potentially useful in monitoring the extent of pneumonia. Clin
Chem. 51:47–55. 2005.PubMed/NCBI View Article : Google Scholar
|
|
10
|
World Health Organization: Clinical
management of severe acute respiratory infection (SARI) when
COVID-19 disease is suspected: Interim guidance, 13 March 2020,
2020.
|
|
11
|
Livak KJ and Schmittgen TD: Analysis of
relative gene expression data using real-time quantitative PCR and
the 2(-Delta Delta C(T)) method. Methods. 25:402–408.
2001.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Hajian-Tilaki K: The choice of methods in
determining the optimal cut-off value for quantitative diagnostic
test evaluation. Stat Methods Med Res. 27:2374–2383.
2018.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Li K, Wu J, Wu F, Guo D, Chen L, Fang Z
and Li C: The clinical and chest CT features associated with severe
and critical COVID-19 pneumonia. Invest Radiol. 55:327–331.
2020.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Wang Z, Yang B, Li Q, Wen L and Zhang R:
Clinical features of 69 cases with coronavirus disease 2019 in
Wuhan, China. Clin Infect Dis. 71:769–777. 2020.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Wu C, Chen X, Cai Y, Xia J, Zhou X, Xu S,
Huang H, Zhang L, Zhou X, Du C, et al: Risk factors associated with
acute respiratory distress syndrome and death in patients with
coronavirus disease 2019 pneumonia in Wuhan, China. JAMA Intern Med
180: 1-11, Mar 13, 2020 (Online ahead of print).
|
|
16
|
Yang X, Yu Y, Xu J, Shu H, Xia J, Liu H,
Wu Y, Zhang L, Yu Z, Fang M, et al: Clinical course and outcomes of
critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China:
A single-centered, retrospective, observational study. Lancet
Respir Med. 8:475–481. 2020.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z,
Xiang J, Wang Y, Song B, Gu X, et al: Clinical course and risk
factors for mortality of adult inpatients with COVID-19 in Wuhan,
China: A retrospective cohort study. Lancet. 395:1054–1062.
2020.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Wang D, Hu B, Hu C, Zhu F, Liu X, Zhang J,
Wang B, Xiang H, Cheng Z, Xiong Y, et al: Clinical characteristics
of 138 hospitalized patients with 2019 novel coronavirus-infected
pneumonia in Wuhan, China. JAMA. 323:1061–1069. 2020.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Yu P, Zhu J, Zhang Z, Han Y and Huang L: A
familial cluster of infection associated with the 2019 novel
coronavirus indicating potential person-to-person transmission
during the incubation period. J Infect Dis, Feb 18, 2020 (Online
ahead of print).
|
|
20
|
de Wit E, van Doremalen N, Falzarano D and
Munster VJ: SARS and MERS: Recent insights into emerging
coronaviruses. Nat Rev Microbiol. 14:523–534. 2016.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Gao Y, Li T, Han M, Li X, Wu D, Xu Y, Zhu
Y, Liu Y, Wang X and Wang L: Diagnostic utility of clinical
laboratory data determinations for patients with the severe
COVID-19. J Med Virol. 92:791–796. 2020.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Chan JF, Yuan S, Kok KH, To KK, Chu H,
Yang J, Xing F, Liu J, Yip CC, Poon RW, et al: A familial cluster
of pneumonia associated with the 2019 novel coronavirus indicating
person-to-person transmission: A study of a family cluster. Lancet.
395:514–523. 2020.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Forstmeier W, Wagenmakers EJ and Parker
TH: Detecting and avoiding likely false-positive findings-a
practical guide. Biol Rev Camb Philos Soc. 92:1941–1968.
2017.PubMed/NCBI View Article : Google Scholar
|