Introduction
Acute kidney injury (AKI) is a potential
complication that may increase morbidity and mortality after any
percutaneous coronary intervention (PCI) or angiography procedure
(1). Several risk factors for AKI
following coronary catheterization have been recognized and they
may be broadly divided into patient-associated or procedure-related
factors. Patient characteristics, including old age, hypotension,
diabetes mellitus, pre-existing renal impairment, history of renal
transplantation, anemia and use of nephrotoxic drugs are known to
significantly increase the risk of post-procedural AKI. Similarly,
procedural factors, including contrast media properties, contrast
media volume and number of procedures within 72 h also influence
the probability of AKI (2,3).
The incidence of AKI following the use of contrast
media has been reported to be 0-24% (2). Although in most cases, AKI is
transient, irreversible renal injury may occur in a proportion of
patients, leading to progressive kidney damage, which may require
prolonged hospitalization and result in long-term adverse effects
(4). Of the several strategies to
reduce contrast-induced AKI, volume expansion has been most
commonly used. However, the benefits of prophylactic fluid
replacement have been questioned by recent reports, which suggest a
limited benefit in high-risk patients (5). Drugs including N-acetylcysteine and
bicarbonate have also been used, but with limited evidence of a
benefit (6).
To reduce the incidence of AKI following coronary
catheterization, the association of vascular access and the
incidence of AKI has been explored in the past decade (7). Trans-radial access for PCI or
angiography, which has gained popularity amongst interventional
cardiologists, is thought to reduce the incidence of AKI in the
immediate post-operative period. To date, several studies have
compared AKI following radial vs. femoral access in patients
undergoing coronary catheterization but with variable results
(8-10).
Certain meta-analyses have been published comparing AKI with the
two vascular access sites (1,7). In
the most recent meta-analysis, Andò et al (7) pooled results from 10 studies and
explored the association between radial access and AKI. The
authors, however, only compiled data on the absolute number of AKI
events from the included studies. Despite several retrospective
studies utilizing multivariate regression analysis to adjust for
baseline characteristics for reporting outcomes, no attempt has
been made to date to collate such data and analyze the overall
evidence on the incidence of AKI with radial vs. femoral access, to
the best of our knowledge. In addition, with further studies
published (8,11,12),
there is a requirement for an updated review and meta-analysis on
this important topic. Therefore, the purpose of the present study
was to perform a comprehensive updated review and meta-analysis
comparing AKI following the radial vs. femoral route of coronary
catheterization.
Materials and methods
Inclusion criteria
The Population, Intervention, Comparison, Outcome
and Study design model was used to select studies for this
systematic review (13).
Retrospective, as well as prospective studies, were included in the
analysis. To be included in the review, studies were required to
have been conducted on adult patients (Population) requiring
coronary catheterization for any reason (PCI or coronary
angiography). Studies were required to compare the radial route
(Intervention) with the femoral route (Comparison)
for catheterization. The Outcome of the study was required
to be the incidence of AKI. The definition of AKI was as per the
included study. Studies not reporting relevant data, studies
reporting duplicate data, single-arm studies, case series, case
reports, non-English language studies and review articles were
excluded. The Preferred Reporting Items for Systematic Reviews and
Meta-analyses guidelines were followed during the conduct of this
systematic review (13).
Search strategy
A computerized literature search of the PubMed,
BioMed Central, Scopus, Cochrane Central Register of Controlled
Trials and Google scholar databases was performed. The search was
conducted by two reviewers independently (CW and WC). Databases
were screened from inception up to 1st January 2020. MeSH terms, as
well as free-text keywords, were used in the literature search. The
entire search protocol, as well as the number of results obtained
from the PubMed database, is presented in Table SI. The entries obtained were
screened by their titles and abstracts for each database.
Potentially relevant articles were then extracted and subsequently
screened by their full text. Both reviewers assessed individual
studies based on the inclusion criteria and resolved any
disagreement by discussion. After screening, the bibliography of
included studies, as well as review articles on the subject, were
hand-searched for any additional references.
Data extraction and risk of bias
assessment
Using a pre-formatted abstraction form, the
reviewers extracted data from the included studies. Details
including the first author name, publication year, sample size,
demographic details, baseline characteristics of the study sample,
definition of AKI, contrast volume and incidence of AKI were
extracted.
The risk of bias of randomized controlled trials
(RCTs) was assessed using the Cochrane Collaboration risk
assessment tool for RCTs (14).
Every study was assessed regarding the following domains: Random
sequence generation, allocation concealment, blinding of
participants and personnel, blinding of outcome assessment,
incomplete outcome data, selective reporting and other biases. The
risk of a bias assessment tool for non-randomized studies was used
to assess non-RCTs (15). Studies
were rated as having low risk, high risk, or unclear risk of bias
for the following: Selection of participants, confounding
variables, intervention measurements, blinding of outcome
assessment, incomplete outcome data and selective outcome
reporting.
Statistical analysis
Considering the methodological heterogeneity of the
included studies, a random-effects model was used to calculate the
pooled effect size for all analyses. The incidence of AKI between
the radial and femoral routes was compared using the generic
inverse-variance method of DerSimonian and Laird. Odds ratios (ORs)
with 95% CI were calculated. Retrospective studies, case-control
studies using propensity score matching and RCTs were grouped
separately for calculating effect sizes (primary meta-analysis). A
sub-group analysis was also conducted for non-RCTs based on the
definition of AKI. Where available, multivariable-adjusted ORs of
AKI for radial vs. femoral route were also obtained from non-RCTs.
All study-specific ORs were then combined using inverse
variance-weighted averages of logarithmic ORs (secondary
meta-analysis). A sensitivity analysis was performed to assess the
influence of each study on the pooled effect size for both the
primary and secondary meta-analysis. Heterogeneity was assessed
using the I2 statistic. I2 values of 25-50%
represented low, values of 50-75% medium and >75% represented
substantial heterogeneity. Visual inspection of funnel plots was
performed to explore possible small-study and publication biases.
The software ‘Review Manager’ [version 5.3; Nordic Cochrane Centre
(Cochrane Collaboration)] was used for the meta-analysis.
Results
Study selection and
characteristics
After a comprehensive literature search, 19 studies
were found eligible for full-text analysis (Fig. 1). A total of 5 studies were then
excluded, as 2 reported data (16,17)
from an already included RCT and the other 3 studies (18-20)
did not report on the incidence of AKI. A total of 14 studies were
included in this systematic review and meta-analysis (8-12,21-29).
The characteristics of the included studies are
presented in Table I. Two studies
(8,10) were RCTs, while the remaining studies
were retrospective in nature. Furthermore, six retrospective
studies utilized propensity score matching to harmonize the
baseline characteristics of the study participants (9,12,22,25,27,29).
In the included studies, participants underwent coronary
catheterization for a variety of reasons. There was a wide
variation in the sample size of included studies ranging from 30
participants per group to a maximum of 8,857 patients per group.
The mean age of the study population was >60 years in all
included studies. AKI was either defined as creatinine levels of
≥0.3 or ≥0.5 mg/dl post-procedure. However, the time-lapse of AKI
was not coherent amongst the included studies. A total of five
studies measured creatinine levels within 48 h of the procedure,
while 4 studies defined AKI as an increase in creatinine levels
within 72 h of catheterization. The mean contrast volume was not
reported in 4 studies (8,9,12,25).
Baseline patient details of included studies are presented in
Table II.
 | Table ICharacteristics of included
studies. |
Table I
Characteristics of included
studies.
| | | Sample size | | Mean age
(years) | Male sex (%) | | Mean contrast
volume (ml) | Incidence of AKI
(%) | |
|---|
| Author (year) | Study type | Radial | Femoral | AKI definition | Radial | Femoral | Radial | Femoral | AKI time lapse | Radial | Femoral | Radial | Femoral | (Refs.) |
|---|
| Azzalini
(2014) | Retrospective | 172 | 49 | Creatinine increase
of ≥0.3 mg/dl or 1.5-2 fold | 61 | 65.9 | 80 | 73 | NR | 200 | 200 | 3 | 10 | (26) |
| Cortese (2014) | Retrospective with
propensity matching | 225 | 225 | Creatinine increase
of >0.5 mg/dl or 25% i | 64.4 | 64.3 | 76.4 | 75.2 | In <72 h | 193 | 198 | 8.4 | 16.9 | (27) |
| Damluji (2014) | Retrospective | 996 | 641 | Creatinine increase
of >0.5 mg/dl or 50% | 62 | 60 | 79 | 72 | In <72 h | 180 | 165 | 2.5 | 4.5 | (28) |
| Kooiman (2014) | Retrospective with
propensity matching | 8,857 | 8,857 | Creatinine increase
of >0.5 mg/dl | 63.9 | 63.8 | 69.5 | 69.6 | In <7 days | NR | NR | 1.4 | 1.9 | (25) |
| Kolte (2016) | Retrospective with
propensity matching | 254 | 254 | Creatinine increase
of >0.5 mg/dl or 25% | 60.09 | 60.59 | 71.7 | 70.1 | In <48 h | 184 | 186 | 5.5 | 8.3 | (29) |
| Andò (2017) | RCT | 4,109 | 4,101 | Creatinine increase
of >0.5 mg/dl or 25% | 65.5 | 65.9 | 74.5 | 72.6 | During
hospitalization | 183 | 183 | 15.4 | 17.4 | (10) |
| Feldkamp
(2018) | Retrospective | 1,141 | 1,796 | Creatinine increase
of >0.3 mg/dl or 50% | 71 | 73 | 69.4 | 63 | In <48 h | 180 | 180 | 10.1 | 15.9 | (23) |
| Gili (2017) | Retrospective with
propensity matching | 177 | 177 | Creatinine increase
of ≥0.3 mg/dl or 1.5-2 fold | 69.7 | 71 | NR | NR | NR | NR | NR | 2.8 | 1.7 | (9) |
| Pancholy
(2017) | Retrospective | 2,176 | 5,353 | Creatinine increase
of >0.5 mg/dl or 25% | 62 | 66 | 30 | 33 | In <48-72 h | 190 | 220 | 1.1 | 2.4 | (21) |
| Steinvil
(2017) | Retrospective with
propensity matching | 536 | 536 | Creatinine increase
of ≥0.3 mg/dl or 1.5-2 fold | 67.8 | 67.2 | 70.5 | 71.6 | NR | 157 | 155 | 4.3 | 10.4 | (22) |
| Barbieri
(2019) | Retrospective | 1,915 | 2,284 | Creatinine increase
of ≥0.5 mg/dl or 25% | 67.8 | 68.4 | 72.7 | 70 | In <48 h | 208.9 | 231.8 | 13.2 | 11.7 | (24) |
| Kanic (2019) | Retrospective with
propensity matching | 1,049 | 1,049 | Creatinine increase
of ≥0.5 mg/dl | 64.1 | 64.1 | 68.8 | 68.5 | In <48 h | NR | NR | 4.9 | 6.2 | (12) |
| Khalil (2019) | Retrospective | 45 | 45 | Creatinine increase
of >0.5 mg/dl or 25% | NR | NR | 80 | 66.7 | In <72 h | 220.4 | 208.4 | 4.4 | 17.7 | (11) |
| Samy (2019) | RCT | 30 | 30 | Creatinine increase
of ≥0.5 mg/dl or 25% | NR | NR | 86.7 | 63.3 | In <48 h | NR | NR | 13.3 | 16.6 | (8) |
 | Table IIBaseline patient characteristics in
included studies. |
Table II
Baseline patient characteristics in
included studies.
| | BMI
(kg/m2) | Diabetes | Hypertension | Congestive heart
failure | Prior PCI | Chronic kidney
disease | Hyperlipidemia | |
|---|
| Author (year) | Radial | Femoral | Radial | Femoral | Radial | Femoral | Radial | Femoral | Radial | Femoral | Radial | Femoral | Radial | Femoral | (Refs.) |
|---|
| Azzalini
(2014) | 28.4±5.1 | 26.8±4.3 | 13 | 24 | 46 | 57 | 2 | 8 | 9 | 18 | 6 | 14 | 49 | 63 | (26) |
| Cortese (2014) | 27.4±4.8 | 27.3±5.4 | 22 | 22 | 59.9 | 59.6 | NR | NR | 12.1 | 11.5 | NR | NR | 39.2 | 44.6 | (27) |
| Damluji (2014) | 29.9±NR | 29.7±NR | 32 | 41 | 78 | 82 | 12 | 15 | NR | NR | 16 | 18 | 79 | 82 | (28) |
| Kooiman (2014) | 31.5±7.5 | 30.9±7 | 39 | 39 | 85.8 | 85.7 | 14 | 14 | 42.5 | 43.1 | 20 | 21 | 84.6 | 84.2 | (25) |
| Kolte (2016) | NR | NR | 22 | 24 | 62.2 | 63.8 | NR | NR | 13 | 12.6 | 2 | 2 | 55.5 | 60.1 | (29) |
| Andò (2017) | NR | NR | 22 | 22 | NR | NR | 9 | 8 | NR | NR | NR | NR | NR | NR | (10) |
| Feldkamp
(2018) | 26.3±NR | 26.1±NR | 25 | 29 | NR | NR | 38 | 43 | 63 | 53 | 21 | 29 | NR | NR | (23) |
| Gili (2017) | NR | NR | 38 | 29 | 83.1 | 83.1 | NR | NR | 35.5 | 35.9 | NR | NR | 65 | 68.9 | (9) |
| Pancholy
(2017) | 29.9±NR | 29.4±NR | 32 | 33 | 74 | 71 | 10 | 9 | 29 | 28 | NR | NR | 72 | 78 | (21) |
| Steinvil
(2017) | 28.3±NR | 28.4±NR | 33 | 34 | 81.9 | 82.3 | 16 | 18 | 23.7 | 21.8 | NR | NR | 80.6 | 79.7 | (22) |
| Barbieri
(2019) | NR | NR | 31.8 | 36.3 | 74.5 | 71.8 | NR | NR | 34.3 | 21.8 | NR | NR | 56.1 | 55.8 | (24) |
| Kanic (2019) | NR | NR | 21.2 | 23.1 | 60.2 | 62 | NR | NR | NR | NR | 16.1 | 15.9 | 44.6 | 44.6 | (12) |
| Khalil (2019) | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | (11) |
| Samy (2019) | NR | NR | 66.7 | 50 | 66.7 | 80 | NR | NR | NR | NR | NR | NR | 56.7 | 63.3 | (8) |
Primary meta-analysis
The absolute incidence of AKI was extracted from
individual studies and pooled for the present meta-analysis. The
pooled effect size of the two RCTs included in this review
indicated that the radial route of coronary catheterization
significantly reduced the incidence of AKI as compared to the
femoral route (OR: 0.87, 95% CI: 0.77-0.98, P=0.02,
I2=0%; Fig. 2). Data of
a total of 22,196 patients in 6 studies were compared utilizing
propensity score matching. Sub-group analysis of these studies also
revealed significantly reduced AKI with the radial route of
catheterization (OR: 0.63, 95% CI: 0.48-0.83, P=0.0009,
I2=45%; Fig. 2).
Finally, analysis of 6 retrospective studies wherein the two groups
were not matched for baseline characteristics also demonstrated a
significant benefit of radial access in reducing AKI (OR: 0.57, 95%
CI: 0.36-0.90, P=0.02, I2=86%; Fig. 2). Overall, when the data of the
21,479 patients in the radial group and 25,337 patients in the
femoral group were compared, the analysis indicated a 35% reduced
incidence of AKI with the radial route (OR: 0.66, 95% CI:
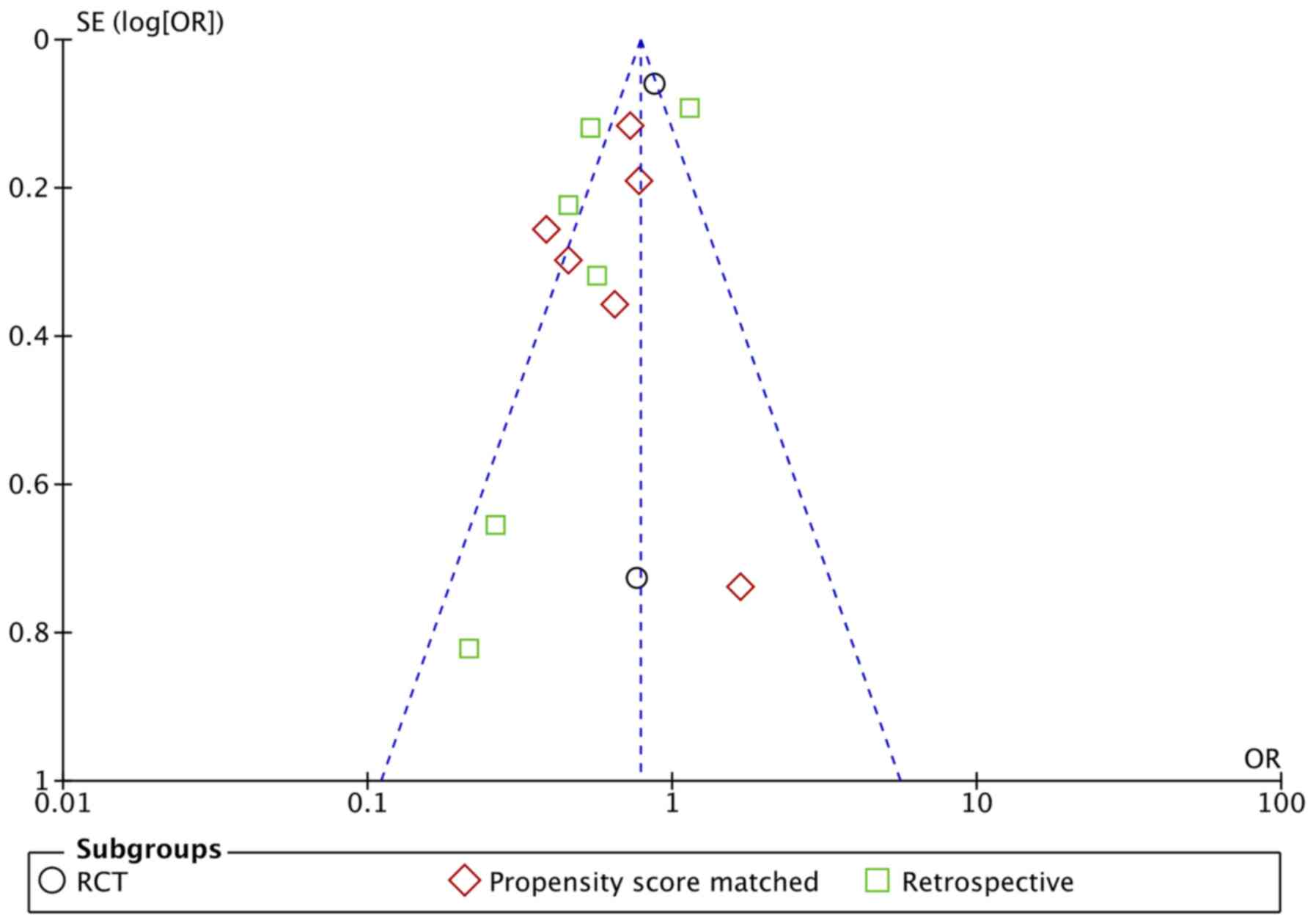
0.54-0.81, P<0.0001, I2=74%; Fig. 2). A certain amount of asymmetry was
identified on visual inspection of the funnel plot (Fig. 3).
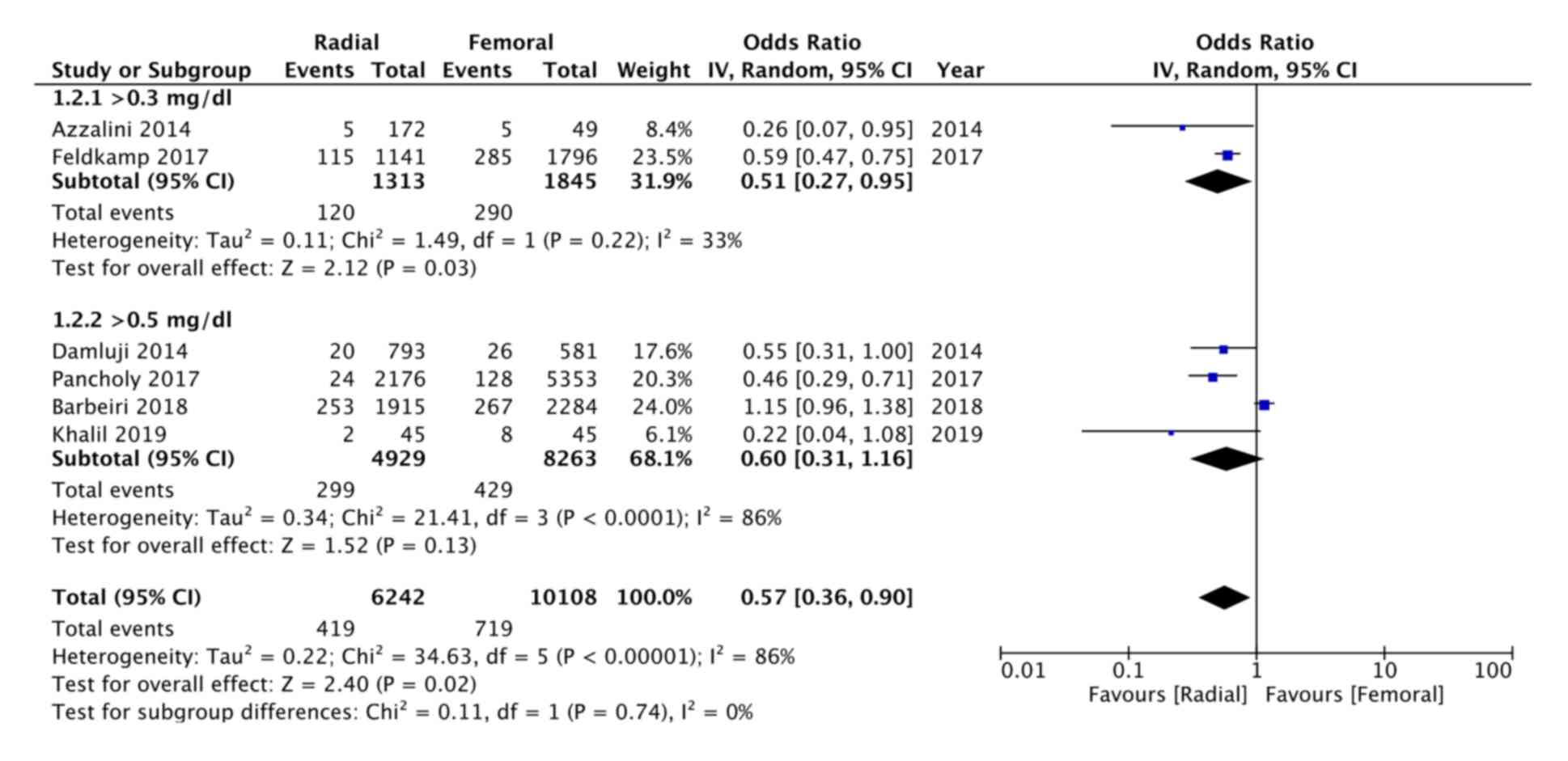
A subgroup analysis was performed for retrospective
studies based on the diagnostic criteria for AKI. Two retrospective
studies defined AKI as an increase of ≥0.3 mg/dl of creatinine,
while the remaining four considered >0.5 mg/dl of creatinine as
AKI. On subgroup analysis, there was a significant advantage of the
radial route when AKI was defined as ≥0.3 mg/dl of creatinine (OR:
0.51, 95% CI: 0.27-0.95, P=0.03, I2=33%), but not when
the criterion was ≥0.5 mg/dl (OR: 0.60, 95% CI: 0.31-1.16, P=0.13,
I2=86; Fig. 4). On the
contrary, in studies utilizing propensity-scored matched groups,
the present analysis indicated no difference in AKI between the two
groups when AKI was defined as ≥0.3 mg/dl of creatinine (OR: 0.68,
95% CI: 0.17-2.81, P=0.06, I2=72%), but a significantly
reduced odds of AKI when it was defined as >0.5 mg/dl of
creatinine (OR: 0.70, 95% CI: 0.59-0.84, P=0.0001,
I2=0%; Fig. 5).
Secondary analysis
Multivariable regression analysis was performed by 9
studies included in the review (12,21-25,27-29).
Adjusted ORs were extracted from these studies and pooled for a
meta-analysis. The results from the secondary meta-analysis
indicated a 30% reduced odds of AKI with the radial route of
catheterization as compared to the femoral route (OR: 0.70, 95% CI:
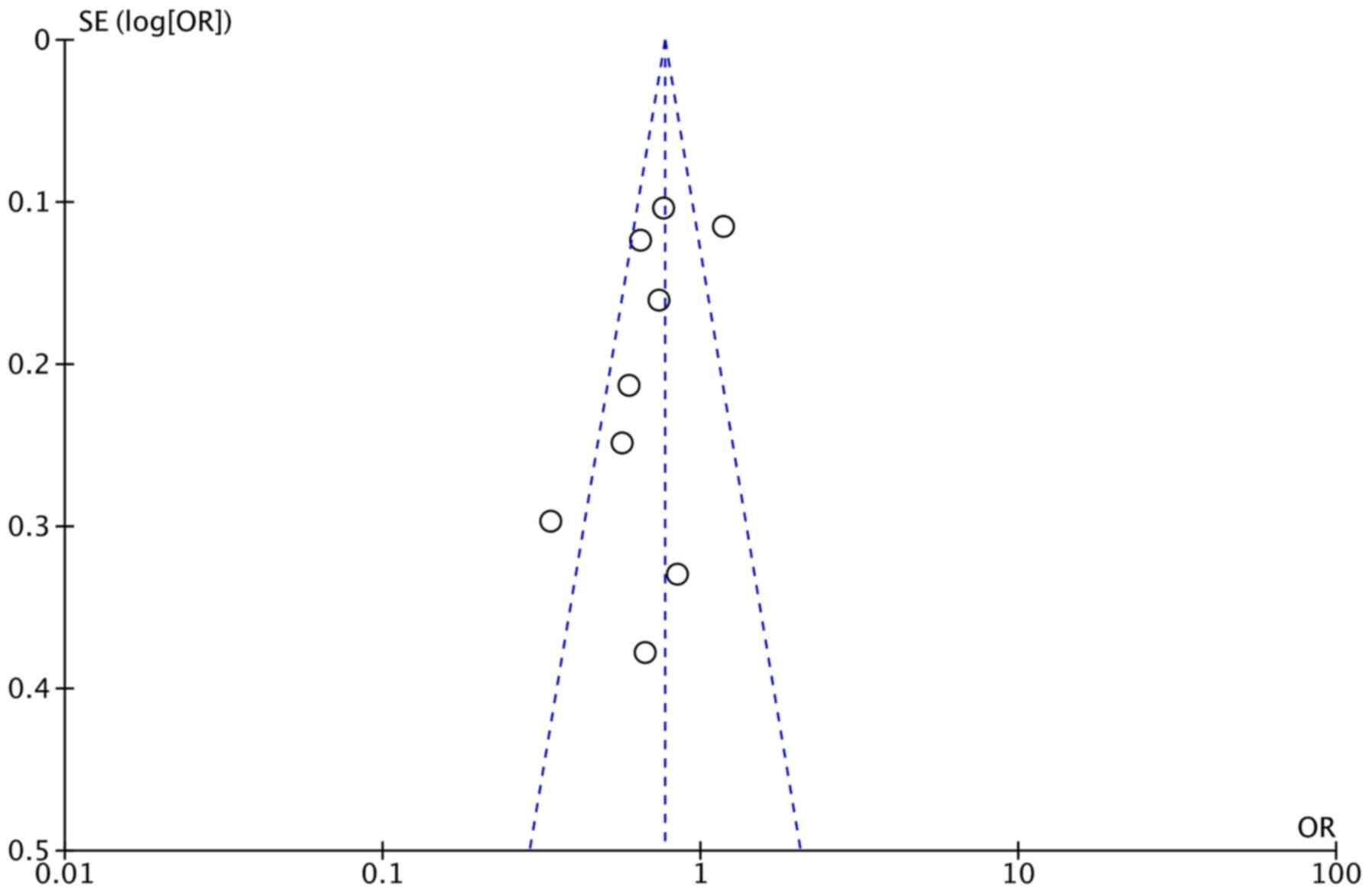
0.57-0.88, P=0.002, I2=70%; Fig. 6). The funnel plot of the analysis
demonstrated minimal asymmetry, with only two of the nine studies
outside the funnel plot (on either side) (Fig. 7).
Sensitivity analysis and risk of bias
assessment
Studies were sequentially excluded from both the
primary and secondary meta-analysis to assess the effect of
individual studies on the pooled effect size. Detailed results of
the sensitivity analysis are presented in Table III. For the primary meta-analysis,
there was no change in the significance of results with the
exclusion of any study in the propensity score-matched group.
However, for retrospective studies, when the studies of Feldkamp
et al (23) and Pancholy
et al (21) were excluded,
there was no significant difference in the incidence of AKI between
the two groups. For the secondary meta-analysis, there was no
change in the significance of results after the exclusion of any
study. The authors' judgement of risk of bias of included studies
is presented in Table SII. For
RCTs, sufficient information on allocation concealment and blinding
of personnel and participants was not available. For retrospective
studies, confounding variables were not taken into account in all
studies and none reported blinding of outcomes. Overall, the risk
of bias in the included studies was moderate.
 | Table IIIResults of the sensitivity
analysis. |
Table III
Results of the sensitivity
analysis.
| A, Propensity
score-matched studies | | | | |
|---|
| Study excluded | OR (95% CI) | P-value | I2
(%) | (Refs.) |
|---|
| Cortese et
al | 0.66
(0.50-0.89) | 0.006 | 46 | (27) |
| Kooiman et
al | 0.59
(0.41-0.86) | 0.005 | 48 | (25) |
| Kolte et
al | 0.62
(0.45-0.86) | 0.004 | 56 | (29) |
| Gili et
al | 0.61
(0.47-0.80) | 0.003 | 47 | (9) |
| Steinvil et
al | 0.71
(0.60-0.85) | 0.002 | 0 | (22) |
| Kanic et
al | 0.59
(0.41-0.84) | 0.004 | 52 | (12) |
| B, Retrospective
studies | | | | |
| Study excluded | OR (95% CI) | P-value | I2
(%) | (Refs.) |
| Damluji et
al | 0.57
(0.34-0.96) | 0.04 | 88 | (28) |
| Azzalini et
al | 0.62
(0.38-0.99) | 0.05 | 87 | (26) |
| Feldkamp et
al | 0.53
(0.28-1.01)a | 0.06 | 84 | (23) |
| Pancholy et
al | 0.61
(0.36-1.01)a | 0.05#6 | 86 | (21) |
| Barbieri et
al | 0.54
(0.45-0.66) | <0.00001 | 0 | (24) |
| Khalil et
al | 0.61
(0.38-0.97) | 0.04 | 88 | (11) |
| C, Studies
reporting multivariate-adjusted OR | | | | |
| Study excluded | OR (95% CI) | P-value | I2
(%) | (Refs.) |
| Cortese et
al | 0.72
(0.57-0.91) | 0.006 | 73 | (27) |
| Damluji et
al | 0.71
(0.56-0.89) | 0.003 | 74 | (28) |
| Kooiman et
al | 0.69
(0.52-0.90) | 0.007 | 74 | (25) |
| Kolte et
al | 0.69
(0.55-0.88) | 0.002 | 74 | (29) |
| Feldkamp et
al | 0.71
(0.55-0.91) | 0.008 | 72 | (23) |
| Pancholy et
al | 0.72
(0.57-0.91) | 0.006 | 72 | (21) |
| Steinvil et
al | 0.76
(0.62-0.92) | 0.006 | 63 | (22) |
| Barbieri et
al | 0.67
(0.58-0.77) | <0.00001 | 15 | (24) |
| Kanic et
al | 0.69
(0.54-0.89) | 0.005 | 74 | (12) |
Discussion
Coronary angiography and PCI are important
diagnostic and management tools for treating coronary artery
disease (CAD). With the increased incidence of CAD and improvements
in stent technology, a significantly larger number of patients are
undergoing coronary catheterization (30). Concurrently, there is a growing need
to limit post-procedural complications and enhance clinical
outcomes. The development of AKI after coronary catheterization is
multifactorial, including both patient and procedural factors
(3). The purpose of the present
study was to gather evidence on whether the vascular access site
influences the incidence of AKI in such patients. Analysis of 14
studies including a total of 46,816 patients revealed that compared
with femoral access, radial access for PCI or coronary angiography
may reduce the incidence of AKI by an estimated 34% (range:
19-46%).
It is important to note that the current
meta-analysis pooled a heterogeneous group of studies involving 2
RCTs, 6 retrospective studies without matching the baseline study
population and 6 studies utilizing propensity-scored matched data.
Individually, 7 studies (8,9,11,12,24,28,29)
did not report any association between the vascular access site and
AKI, while the remaining studies demonstrated a significantly
reduced incidence of AKI with the radial route (10,21-23,25-27).
Among the studies not reporting any difference between the radial
and the femoral route were 1 RCT, 3 retrospective studies and 3
propensity-scored matched studies.
Several factors, including age, hydration status,
pre-existing diseases, medications and procedural characteristics,
may influence AKI in a patient undergoing coronary catheterization.
It is therefore essential that baseline patient and procedural
factors are matched when assessing the difference in AKI between
the radial and the femoral route. RCTs are designed to provide
unbiased results, as they reduce the influence of confounding
factors and have lower chances of systematic errors (31). In the case of deficiency of RCTs,
the evidence is frequently generated from retrospective data using
either propensity score matching or multivariate logistic
regression adjustment (32).
Propensity score matching is a quasi-empirical correction strategy
that attempts to decrease bias of treatment estimates in
non-randomized studies by forming matched sets of study and control
groups (32,33). On the other hand, regression
analysis is a commonly used statistical tool to assess the impact
of an independent variable on a dichotomous dependent variable
(33). Both techniques have been
widely utilized in observation studies and have their own set of
advantages and drawbacks. The superiority of one technique over the
other is difficult to judge, as neither of them take into account
unknown confounding factors that may affect the outcome (32). Therefore, to provide a broad
perspective on the results of different study types and different
matching techniques, different sets of analyses were performed in
the present study. On subgroup analysis based on study type, the
pooled analysis of the two RCTs indicated a 23% reduced incidence
of AKI with the radial route of access. However, as the recent RCT
by Samy et al (8) included
just 30 patients in each group, the results were particularly
influenced by the larger AKI-MATRIX trial (10). Similar results were obtained on the
pooling of data from retrospective non-adjusted studies, albeit
with a wider 95% CI. The pooled analysis indicated a 43% reduced
odds of AKI varying from 10 to 64%. The wide range and superior
results were probably due to the influence of non-adjusted
confounding factors in these studies. Analysis of propensity
score-matched studies revealed a 37% reduced incidence of AKI
(range, 17-52%) with the use of the radial access site. These
figures closely concurred with the pooled multivariate-adjusted ORs
of 9 studies demonstrating a 30% (range, 12-43%) reduced chance of
AKI with radial as compared to the femoral route for coronary
catheterization. Near identical results obtained with both
propensity score and multivariate regression data in the present
analysis provided strong evidence that the use of the radial access
site significantly reduces the incidence of post-procedural
AKI.
Another important difference between the included
studies was the definition of AKI. Contrast-induced AKI as defined
by the Kidney Disease: Improving Global Outcomes workgroup in 2012
is an absolute increase in serum creatinine of ≥0.3 mg/dl within 48
h or an increase of ≥25% from baseline (34). Alternatively, the Contrast Media
Safety Committee of the European Society of Urogenital Radiology
defines AKI as ≥0.5 mg/dl or ≥25% of the baseline increase in serum
creatinine within 72 h of contrast exposure (35). To evaluate the influence of the
definition of AKI on study outcomes, studies defining AKI as a
creatinine increase of ≥0.3 or ≥0.5 mg/dl were grouped. In the
propensity score-matched studies, there was no difference between
the radial and femoral access site when AKI was defined as ≥0.3
mg/dl, but a significant advantage of radial access was observed
when AKI was defined as ≥0.5 mg/dl of creatinine. This may indicate
that there may be no difference in the milder form of AKI with the
use of either access site but a higher grade of AKI may be reduced
with the radial route. However, due to limited studies in the
analysis and contrasting results of the subgroup analysis of
retrospective studies, no strong conclusions can be drawn from this
difference.
Two important reasons are thought to reduce the
incidence of AKI with trans-radial access. Bleeding events and
access site complications are known risk factors for the
development of AKI following coronary catheterization. As bleeding
events are significantly reduced with the use of radial access, it
is likely that the radial route provides a reno-protective effect
by limiting renal hypoperfusion (24). Furthermore, it is also postulated
that the incidence of athero-embolization is higher with femoral as
compared to radial vascular access. Since the catheter passed via
the femoral route comes in contact with thoracic and abdominal
aortic atheroma, the catheter may scrape of plaque material,
resulting in embolization to the renal vasculature (36). Since the radial route completely
avoids these arteries, the risk of renal embolization is therefore
significantly reduced.
The results of the present study should be
interpreted considering the following limitations. First, only 2
RCTs were included in the analysis and majority studies were
retrospective in nature. The lack of RCTs reduced the level of
evidence and increased bias of the results. Despite using
propensity score matching and multivariate regression adjustment,
the influence of all confounding factors on the study outcomes is
not completely negated. Furthermore, there was methodological
heterogeneity between the included studies concerning factors such
as the study population, baseline patient characteristics, and
definition and time-lapse of AKI. Of note, the exact definition of
AKI varied among the included studies. This may have skewed the
results of the present analysis. Finally, data about
reno-protective measures, including the use of hydration, was not
available from the included studies. To what extent other AKI
preventive measures were utilized in the radial and femoral groups
is also not known.
As compared to the previous meta-analysis (7), the present study was able to
incorporate 4 further studies (8,11,12,24);
it included the data of a total of 46,816 patients and is therefore
a significant update. In addition to the subgroup analysis based on
study type, the influence of the definition of AKI on the pooled
effect size was also analyzed. Adjusted ORs from retrospective
studies were also subjected to a meta-analysis to provide
comprehensive evidence on the subject. Except for the retrospective
studies, the results of the present analysis were robust in terms
of effect size and direction after the sensitivity analysis.
Within the limitations of the present study, the
results indicated that, as compared to femoral access, the use of
trans-radial access for coronary catheterization significantly
reduced the incidence of AKI. A reduction of AKI by ~34% may be
expected with the use of radial access. In addition, there may be
no difference in the milder form of AKI with the use of either
access site and only a higher grade of AKI may be reduced with the
radial route. Further large-scale RCTs are required to strengthen
the current evidence.
Supplementary Material
Search strategy and PubMed
results.
Risk of bias assessment of included
studies.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the present
study are available from the corresponding author on reasonable
request.
Authors' contributions
CW conceived and designed the study. CW and WC
collected the data and performed the literature search. MY and PY
performed the meta-analysis. CW was involved in the writing of the
manuscript. All authors have read and approved the final
manuscript.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Andò G, Costa F, Boretti I, Trio O and
Valgimigli M: Benefit of radial approach in reducing the incidence
of acute kidney injury after percutaneous coronary intervention: A
meta-analysis of 22,108 patien. Int J Cardiol. 179:309–311.
2015.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Hossain MA, Costanzo E, Cosentino J, Patel
C, Qaisar H, Singh V, Khan T, Cheng JS, Asif A and Vachharajani TJ:
Contrast-induced nephropathy: Pathophysiology, risk factors, and
prevention. Saudi J Kidney Dis Transpl. 29:1–9. 2018.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Mehran R, Aymong ED, Nikolsky E, Lasic Z,
Iakovou I, Fahy M, Mintz GS, Lansky AJ, Moses JW, Stone GW, et al:
A simple risk score for prediction of contrast-induced nephropathy
after percutaneous coronary intervention: Development and initial
validation. J Am Coll Cardiol. 44:1393–1399. 2004.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Rihal CS, Textor SC, Grill DE, Berger PB,
Ting HH, Best PJ, Singh M, Bell MR, Barsness GW, Mathew V, et al:
Incidence and prognostic importance of acute renal failure after
percutaneous coronary intervention. Circulation. 105:2259–2264.
2002.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Nijssen EC, Rennenberg RJ, Nelemans PJ,
Essers BA, Janssen MM, Vermeeren MA, Ommen VV and Wildberger JE:
Prophylactic hydration to protect renal function from intravascular
iodinated contrast material in patients at high risk of
contrast-induced nephropathy (AMACING): A prospective, randomised,
phase 3, controlled, open-label, non-inferiority trial. Lancet.
389:1312–1322. 2017.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Feldkamp T and Kribben A: Contrast media
induced nephropathy: Definition, incidence, outcome,
pathophysiology, risk factors and prevention. Minerva Med.
99:177–196. 2008.PubMed/NCBI
|
|
7
|
Andò G, Gragnano F, Calabrò P and
Valgimigli M: Radial vs femoral access for the prevention of acute
kidney injury (AKI) after coronary angiography or intervention: A
systematic review and meta-analysis. Catheter Cardiovasc Interv.
92:E518–E526. 2018.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Samy NI, Walaafareed Ahmed AAS and Osama
M: Contrast Induced Nephropathy after radial or femoral access for
invasive management of acute coronary syndrome. World J Cardiovasc
Dis. 9:572–583. 2019.
|
|
9
|
Gili S, D'Ascenzo F, Di Summa R, Conrotto
F, Cerrato E, Chieffo A, Boccuzzi G, Montefusco A, Ugo F, Omedé P,
et al: Radial versus femoral access for the treatment of left main
lesion in the era of second-generation drug-eluting stents. Am J
Cardiol. 120:33–39. 2017.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Andò G, Cortese B, Russo F, Rothenbühler
M, Frigoli E, Gargiulo G, Briguori C, Vranckx P, Leonardi S,
Guiducci V, et al: Acute kidney injury after radial or femoral
access for invasive acute coronary syndrome management: AKI-MATRIX.
J Am Coll Cardiol, May 11, 2017 (Online ahead of print).
|
|
11
|
Khalil WA, Abdelhameed MG, Elmenshawy MD
and Elhelaly A: Serum cystatin c and renal dysfunction in
transradial versus transfemoral approaches in primary percutaneous
coronary intervention. J Indian Coll Cardiol. 9:88–94. 2019.
|
|
12
|
Kanic V, Kompara G, Šuran D, Tapajner A,
Naji FH and Sinkovic A: Acute kidney injury in patients with
myocardial infarction undergoing percutaneous coronary intervention
using radial versus femoral access. BMC Nephrol.
20(28)2019.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Moher D, Liberati A, Tetzlaff J and Altman
DG: PRISMA Group. Preferred reporting items for systematic reviews
and meta-analyses: The PRISMA statement. PLoS Med.
6(e1000097)2009.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Higgins JPT, Altman DG and Sterne JAC
(eds): Cochrane statistical methods group and the cochrane bias
methods group. Chapter 8: Assessing risk of bias in included
studies. In: Cochrane Handbook for Systemic Reviews of
Interventions, Version 5. The Cochrane Collaboration, 2011.
|
|
15
|
Kim SY, Park JE, Lee YJ, Seo HJ, Sheen SS,
Hahn S, Jang BH and Son HJ: Testing a tool for assessing the risk
of bias for nonrandomized studies showed moderate reliability and
promising validity. J Clin Epidemiol. 66:408–414. 2013.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Valgimigli M, Gagnor A, Calabró P, Frigoli
E, Leonardi S, Zaro T, Rubartelli P, Briguori C, Andò G, Repetto A,
et al: Radial versus femoral access in patients with acute coronary
syndromes undergoing invasive management: A randomised multicentre
trial. Lancet. 385:2465–2476. 2015.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Rothenbühler M, Valgimigli M, Odutayo A,
Frigoli E, Leonardi S, Vranckx P, Turturo M, Moretti L, Amico F,
Uguccioni L, et al: Association of acute kidney injury and bleeding
events with mortality after radial or femoral access in patients
with acute coronary syndrome undergoing invasive management:
Secondary analysis of a randomized clinical trial. Eur Heart J.
40:1226–1232. 2019.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Alonzo A, Rigattieri S, Giovannelli F, Di
Russo C, Sciahbasi A, Berni A and Volpe M: Transfemoral approach
with systematic use of FemoSeal™ closure device compared to
transradial approach in primary angioplasty. Catheter Cardiovasc
Interv. 87:849–854. 2016.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Ratib K, Mamas MA, Anderson SG, Bhatia G,
Routledge H, De Belder M, Ludman PF, Fraser D and Nolan J: British
Cardiovascular Intervention Society and the National Institute for
Cardiovascular Outcomes Research. Access site practice and
procedural outcomes in relation to clinical presentation in 439,947
patients undergoing percutaneous coronary intervention in the
United kingdom. JACC Cardiovasc Interv. 8:20–29. 2015.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Mamas MA, Ratib K, Routledge H, Neyses L,
Fraser DG, de Belder M, Ludman PF and Nolan J: British
Cardiovascular Intervention Society and the National Institute for
Cardiovascular Outcomes Research. Influence of arterial access site
selection on outcomes in primary percutaneous coronary
intervention: Are the results of randomized trials achievable in
clinical practice? JACC Cardiovasc Interv. 6:698–706.
2013.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Pancholy MS, Skelding K, Scott T,
Blankenship J and Pancholy SB: Effect of access site choice on
acute kidney injury after percutaneous coronary intervention. Am J
Cardiol. 120:2141–2145. 2017.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Steinvil A, Garcia-Garcia HM, Rogers T,
Koifman E, Buchanan K, Alraies MC, Torguson R, Pichard AD, Satler
LF, Ben-Dor I and Waksman R: Comparison of propensity score-matched
analysis of acute kidney injury after percutaneous coronary
intervention with transradial versus transfemoral approaches. Am J
Cardiol. 119:1507–1511. 2017.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Feldkamp T, Luedemann M, Spehlmann ME,
Freitag-Wolf S, Gaensbacher J, Schulte K, Bajrovic A, Hinzmann D,
Hippe HJ, Kunzendorf U, et al: Radial access protects from contrast
media induced nephropathy after cardiac catheterization procedures.
Clin Res Cardiol. 107:148–157. 2018.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Barbieri L, Verdoia M, Suryapranata H and
De Luca G: Novara Atherosclerosis Study Group (NAS). Impact of
vascular access on the development of contrast induced nephropathy
in patients undergoing coronary angiography and/or percutaneous
coronary intervention. Int J Cardiol. 275:48–52. 2019.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Kooiman J, Seth M, Dixon S, Wohns D,
LaLonde T, Rao SV and Gurm HS: Risk of acute kidney injury after
percutaneous coronary interventions using radial versus femoral
vascular access: Insights from the blue cross blue shield of
michigan cardiovascular consortium. Circ Cardiovasc Interv.
7:190–198. 2014.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Azzalini L, Khan R, Al-Hawwas M, Hatem R,
Fortier A, L'Allier PL and Ly HQ: Effect of radial-to-femoral
access crossover on adverse outcomes in primary percutaneous
coronary intervention. Am J Cardiol. 114:1165–1173. 2014.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Cortese B, Sciahbasi A, Sebik R,
Rigattieri S, Alonzo A, Silva-Orrego P, Belloni F, Seregni RG,
Giovannelli F, Tespili M, et al: Comparison of risk of acute kidney
injury after primary percutaneous coronary interventions with the
transradial approach versus the transfemoral approach (from the
PRIPITENA urban registry). Am J Cardiol. 114:820–825.
2014.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Damluji A, Cohen MG, Smairat R, Steckbeck
R, Moscucci M and Gilchrist IC: The incidence of acute kidney
injury after cardiac catheterization or PCI: A comparison of radial
vs. femoral approach. Int J Cardiol. 173:595–597. 2014.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Kolte D, Spence N, Puthawala M, Hyder O,
Tuohy CP, Davidson CB, Sheldon MW, Laskey WK and Abbott JD:
Association of radial versus femoral access with contrast-induced
acute kidney injury in patients undergoing primary percutaneous
coronary intervention for ST-elevation myocardial infarction.
Cardiovasc Revasc Med. 17:546–551. 2016.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Likosky DS, Van Parys J, Zhou W, Borden
WB, Weinstein MC and Skinner JS: Association between medicare
expenditure growth and mortality rates in patients with acute
myocardial infarction: A comparison from 1999 through 2014. JAMA
Cardiol. 3:114–122. 2018.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Burns PB, Rohrich RJ and Chung KC: The
levels of evidence and their role in evidence-based medicine. Plast
Reconstr Surg. 128:305–310. 2011.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Biondi-Zoccai G, Romagnoli E, Agostoni P,
Capodanno D, Castagno D, D'Ascenzo F, Sangiorgi G and Modena MG:
Are propensity scores really superior to standard multivariable
analysis? Contemp Clin Trials. 32:731–740. 2011.PubMed/NCBI View Article : Google Scholar
|
|
33
|
Baser O: Choosing propensity score
matching over regression adjustment for causal inference: When, why
and how it makes sense. J Med Econ. 10:379–391. 2007.
|
|
34
|
Kellum JA and Lameire N: KDIGO AKI
Guideline Work Group. Diagnosis, evaluation, and management of
acute kidney injury: A KDIGO summary (Part 1). Crit Care.
17(204)2013.PubMed/NCBI View
Article : Google Scholar
|
|
35
|
Morcos SK, Thomsen HS and Webb JA:
Contrast-media-induced nephrotoxicity: A consensus report. Contrast
media safety committee, european society of urogenital radiology
(ESUR). Eur Radiol. 9:1602–1013. 1999.PubMed/NCBI View Article : Google Scholar
|
|
36
|
Scolari F, Ravani P, Gaggi R, Santostefano
M, Rollino C, Stabellini N, Colla L, Viola BF, Maiorca P,
Venturelli C, et al: The challenge of diagnosing atheroembolic
renal disease: Clinical features and prognostic factors.
Circulation. 116:298–304. 2007.PubMed/NCBI View Article : Google Scholar
|