Introduction
Anorectal malignant melanoma (ARMM), a fatal
malignancy with high malignant degree and poor patient prognosis,
has shown increasing incidence rate in recent years (1,2). Since
the clinical symptoms of ARMM patients are inapparent and
non-specific, generally manifested as constipation, hematochezia,
diarrhea, proctalgia and pruritus, most patients tend to be at the
middle or advanced stage at diagnosis. In addition, ARMM is highly
invasive, with frequent local and distant metastases. The 5-year
survival rate of patients is relatively low (3,4). As
treatment for ARMM, radiotherapy, chemotherapy and surgical
resection are adopted, of which surgical resection is usually
considered the preferred option (5).
The dysfunction of immune system is closely related
to the occurrence and development of malignant tumors (6). The proportion and function of T
lymphocyte subsets can reflect the immune function (6,7).
CD3+ represents all T lymphocytes, CD4+
represents helper T lymphocytes, CD8+ represents
suppressive and cytotoxic T lymphocytes. Malignant tumors often
manifest with a decrease of CD3+ and CD4+
lymphocytes, an increase of CD8 lymphocytes and a decrease of the
CD4/CD8 ratio (7).
Inflammatory responses can participate in the
development and progression of many malignant tumors.
Interleukin-17 (IL-17) and IL-23 are cytokines that are abnormally
expressed in various malignant tumors and participate in the
development, progression and metastasis of such malignant tumors
(8,9). VEGF accelerates tumor angiogenesis,
promotes tumor growth and increases tumor invasiveness, thus having
a close relationship with metastasis (10).
In the present study, surgical treatment was adopted
for ARMM, the prognosis was observed, the levels of
CD3+, CD4+ and
CD4+/CD8+ was detected and expression of
serum VEGF, IL-23 and IL-17 of patients were analyzed, to provide a
basis for clinical treatment and prognosis evaluation.
Patients and methods
General data
A total of 64 ARMM patients treated in Linyi Cancer
Hospital from July 2010 to June 2014 were selected as the subjects.
Inclusion criteria: i) Patients meeting the diagnostic criteria for
ARMM (11); ii) those with complete
case data; and iii) those who signed an informed consent. Exclusion
criteria: i) Patients with mental disorder, or ii) those who
refused to cooperate and had extremely low compliance. The 64
patients were divided into the control group (n=32) and the
observation group (n=32) based on different therapeutic methods.
There was no statistically significant difference in the general
data of patients between the groups (P>0.05) (Table I). This study was approved by the
Ethics Committee of Linyi Cancer Hospital. Signed informed consents
were obtained from all participants before the study.
 | Table IGeneral data of the subjects. |
Table I
General data of the subjects.
| Item | Control group
(n=32) | Observation group
(n=32) | t/χ2 | P-value |
|---|
| Sex
(male/female) | 13/19 | 11/21 | 0.063 | 0.802 |
| Age (years) | 35-75 | 36-78 |
| Average age
(years) | 53.76±8.49 | 54.35±8.58 | 0.350 | 0.727 |
| BMI
(kg/m2) | 22.65±1.57 | 22.58±1.43 | 1.030 | 0.305 |
| Clinical stage [n
(%)] |
|
I-II | 15 (46.87) | 14 (43.75) | 0.012 | 0.922 |
|
III-IV | 17 (53.13) | 18 (56.25) | | |
Therapeutic methods
In control group, chemotherapy was adopted:
5-fluorouracil (Shanghai Xudong Haipu Pharmaceutical Co., Ltd.;
approval no: NMPN H31020593) was intravenously infused according to
the standard of 400 mg/m2 and then pumped through
peripheral veins for 46 h in accordance with the standard of 2400
mg/m2, once every 2 weeks. In observation group,
surgical treatment was employed: After general anesthesia with
tracheal intubation, Miles surgery was conducted, and patients with
lymph node metastasis received unilateral or bilateral inguinal
lymph node dissection.
Detection of indicators
Fasting venous blood (3-5 ml) was collected from the
two groups of patients for separation and extraction of serum.
Enzyme-linked immunosorbent assay (ELISA) was performed to measure
the levels of IL-17, IL-23 and vascular endothelial growth factor
(VEGF) using relevant kits (R&D Systems) according to the
instructions of the kits. Then, a microplate reader (Jiangsu Puyun
Biotechnology Co., Ltd.) was used to read the optical density (OD)
value at a wavelength of 450 nm, and the concentration of IL-17,
IL-23 and VEGF was calculated. The mononuclear cells were separated
via Ficoll stratified liquid method, collected, incubated with
anti-cluster of differentiation (CD3 (cat. no. AF1480), CD4 (cat.
no. AF1792), CD8 (cat. no. AF1417) antibodies (Beyotime Institute
of Biotechnology) in the dark at 4˚C for 30 min. Thereafter, a flow
cytometer (BD Biosciences) was utilized for detection, and the
value of CD4+/CD8+ was calculated.
Evaluation of indexes
The changes in the patient serum IL-17, IL-23 and
VEGF levels were compared before and after treatment. The immune
function of patients was observed after treatment. The patients
were followed up for 5 years, and the survival time and survival
rate of different groups of patients were recorded.
Statistical analysis
Statistical Product and Service Solutions (SPSS)
v19.0 software (SPSS Inc.) was employed for data processing.
Measurement data were expressed as mean ± standard deviation (mean
± SD), and t-test was utilized for intergroup comparison.
Comparison between multiple groups was done using two-way/mixed
ANOVA test followed by post hoc test (Bonferroni). Enumeration data
were expressed as ratio (%) and subjected to χ2 test or
Fisher's exact test. Kaplan-Meier method was applied for survival
analysis. P<0.05 was considered to indicate a statistically
significant difference.
Results
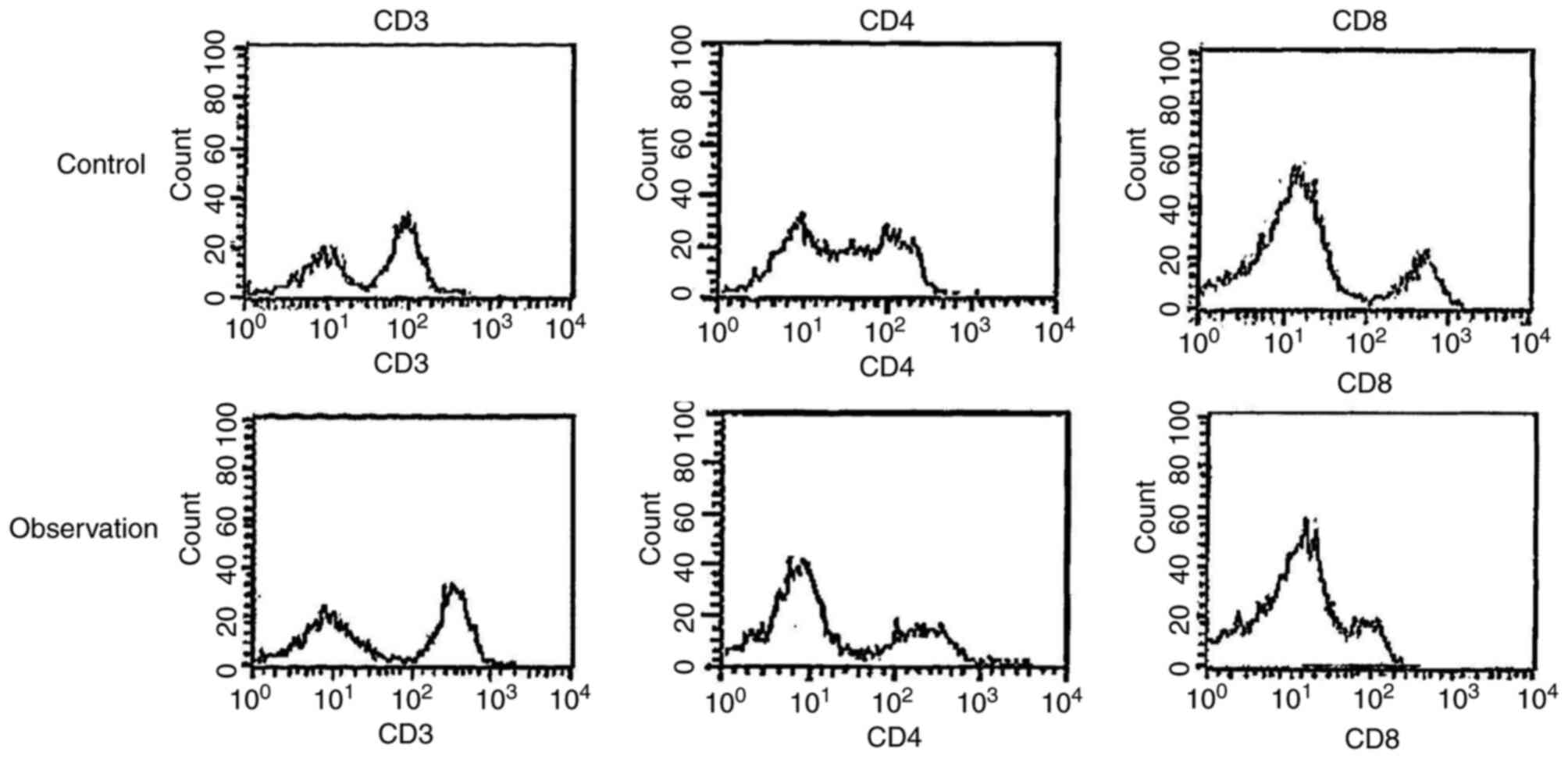
Immune function after treatment in
both groups of patients
After treatment, the levels of CD3+,
CD4+ and CD4+/CD8+ were higher in
the observation group than those in the control group, while the
level of CD8+ was lower in the observation group than
that in the control group (P<0.05; Fig. 1 and Table II).
 | Table IIComparison of T lymphocyte subset
levels between two groups of patients. |
Table II
Comparison of T lymphocyte subset
levels between two groups of patients.
| Group | n | CD3+ | CD4+ | CD8+ |
CD4+/CD8+ |
|---|
| Observation
group | 32 | 68.53±3.56 | 40.83±3.56 | 24.38±3.67 | 1.85±0.47 |
| Control group | 32 | 60.47±3.32 | 36.47±3.74 | 28.35±3.65 | 1.39±0.35 |
| t | | 5.503 | 2.974 | 2.664 | 2.895 |
| P-value | | <0.0001 | 0.003 | 0.009 | 0.004 |
Serum IL-17 and IL-23 and VEGF levels
of patients before and after treatment
The serum IL-17 and IL-23 and VEGF levels of
patients markedly declined in the groups at 4, 6 and 8 weeks after
treatment, and the decrease in the observation group was more
evident (P<0.05; Tables
III-V).
Comparison of recurrence rate and
survival of patients between the groups
Observation group exhibited longer average survival
time, a clearly lowered recurrence rate and a dramatically raised
5-year survival rate in comparison with the control group
(P<0.05; Table VI and Fig. 2).
 | Table VIComparison of 5-year follow-up
between two groups of patients. |
Table VI
Comparison of 5-year follow-up
between two groups of patients.
| Group | n | 5-year survival
rate [n (%)] | Recurrence rate [n
(%)] | Average survival
time [month(s)] |
|---|
| Observation
group | 32 | 8 (25.00) | 20 (62.50) | 22.76±6.74 |
| Control group | 32 | 1 (3.13) | 30 (93.75) | 12.83±5.63 |
| χ²/t | | - | 7.406 | 6.427 |
| P-value | | 0.026 | 0.006 | <0.001 |
Discussion
Malignant melanoma, a malignancy with high malignant
degree, occurs in organs such as the liver, skin, kidneys, eyes and
uterus and is mainly characterized by over proliferation of
melanocytes (5,12). Moreover, malignant melanoma in the
skin ascribes to excessive ultraviolet irradiation, but, there is
no ultraviolet irradiation in ARMM, and its pathogenesis is not
fully understood. It is generally assumed that ARMM occurs because
of the combined effects of environmental and genetic factors
(13). ARMM is prevalent in
middle-aged and elderly people, and its incidence rate is overtly
higher in women than that in men (14). In clinical practice, the treatment
of ARMM aims to prolong the survival time of patients as far as
possible, and radiotherapy, chemotherapy and surgery are mainly
employed, of which surgery is currently deemed as the preferred
therapeutic option (15).
Patients with ARMM often suffer immune dysfunction
(16). CD3+ can reflect
the level of all T lymphocytes in the body, and CD4+ can
positively modulate the immunity (6). CD8+ is able to kill and
destroy cells, which can inhibit CD4+ and aggravate the
immune dysfunction of patients (17). It was uncovered in the present study
that the observation group had elevated CD3+,
CD4+ and CD4+/CD8+ levels and
lower CD8+ level in comparison with the control group.
This is because surgical treatment can effectively remove the
tumor, control the metastasis of mesenteric lymph nodes, rapidly
reduce the tumor load, improving the impaired immune status.
Inflammatory response, an important part of body
immunity, occurs due to the stimulation of both internal and
external environment (18).
Inflammation has a close correlation with malignant tumors, which
is capable of providing a favorable environment for the development
of tumors and promoting their progression. IL-23, a member of the
IL family, is secreted by phagocytes, binding to cell surface
membrane receptor complexes to activate the NF-κB signaling pathway
and exerting its functions of regulating immune surveillance and
breaking immune balance, thus inducing tumors (19). IL-17, also a member of the IL
family, is a pro-inflammatory cytokine, which is one of the early
promoters of the inflammatory response amplifying the inflammatory
response (20). The results of this
study showed that the serum IL-17 and IL-23 levels of patients
markedly declined in the two groups after treatment, and the
decrease in the observation group was more evident (P<0.05).
This may be because the surgical treatment of tumor removal can
relieve tumor load, improve immune status and stimulate T cells to
exert anti-inflammatory effects, thus down-regulating the
expression levels of IL-17 and IL-23.
VEGF, a member of platelet-derived growth factor
family, plays a vital role in the development and progression of
ARMM, which accelerates the neovascularization at tumor sites and
promotes the growth of tumors, strengthening invasiveness of the
tumor and letting it break through the intestinal wall to invade
adjacent tissues, and thus resulting in regional lymph node
metastasis and even metastasis to distant organs i.e. the liver,
lungs, bones and the brain (10).
In the present study, the serum VEGF level markedly declined in
both groups after treatment, with a more evident decrease in the
observation group (P<0.05). Surgical treatment down-regulates
expression of VEGF, blocks tumor angiogenesis, and inhibits
metastasis, with more pronounced short-term curative effects.
ARMM progresses rapidly. It may be cured by surgery,
but the recurrence rate is still high, the patient prognosis is
poor, and the survival time remains short. The results of the
present study revealed that the recurrence rate was lower in the
observation group than in the control group, while the survival
time and survival rate were distinctly better in the observation
group than those in the control group (P<0.05). This is because
surgical treatment can effectively resect both the tumor and the
affected surrounding adjacent tissues, thus achieving a more
thorough treatment effect, and it can control the lymph node or
distant metastasis to a certain extent, thereby reducing the
recurrence rate and improving the survival rate of patients.
In conclusion, surgical treatment applied in ARMM
achieves better efficacy in comparison with non-surgical treatment,
lowering the serum IL-17 and IL-23 levels, improving patient
prognosis, reducing recurrence rate and prolonging patient survival
time, which is of positive significance in clinic. Unfortunately,
the comparison of these target parameters between low- and
high-grade of ARMM in the control and observation groups was not
included in the present study. We would like to further investigate
this topic in our next work.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
All data generated or analyzed during this study are
included in this published article.
Authors' contributions
MH and ZZ designed the study and performed the
experiments. MH and WT collected the data. ZZ and WT analyzed the
data. MH and ZZ wrote the manuscript. All authors read and approved
the final manuscript.
Ethics approval and consent to
participate
The present study was approved by the Ethics
Committee of Linyi Cancer Hospital. Signed informed consents were
obtained from the patients.
Patients consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Latteri S, Teodoro M, Malaguarnera M,
Mannino M, Currò G and La Greca G: Abdominal perineal resection or
Wilde local excision in primary anorectal malignant melanoma. Case
report and review. Ann Med Surg (Lond). 19:74–77. 2017.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Tokuhara K, Nakatani K, Tanimura H,
Yoshioka K, Kiyohara T and Kon M: A first reported case of
metastatic anorectal amelanotic melanoma with a marked response to
anti-PD-1 antibody nivolumab: A case report. Int J Surg Case Rep.
31:188–192. 2017.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Zaiem F and Alrifai A: Anorectal malignant
melanoma presenting as acute pancreatitis. Am J Med Sci.
354:327–328. 2017.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Ohta R, Inoue T, Goto M, Tachimori Y and
Sekikawa K: Combined laparoscopic abdomino-endoscopic perineal
total mesorectal excision for anorectal malignant melanoma: A case
report. Int J Surg Case Rep. 44:135–138. 2018.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Seo KI, Moon W, Kim SE, Park MI and Park
SJ: Malignant melanoma of the anus found during routine colonoscopy
in ulcerative colitis. Korean J Gastroenterol. 69:368–371.
2017.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Jesinghaus M, Steiger K, Slotta-Huspenina
J, Drecoll E, Pfarr N, Meyer P, Konukiewitz B, Bettstetter M,
Wieczorek K, Ott K, et al: Increased intraepithelial
CD3+ T-lymphocytes and high PD-L1 expression on tumor
cells are associated with a favorable prognosis in esophageal
squamous cell carcinoma and allow prognostic immunogenic
subgrouping. Oncotarget. 8:46756–46768. 2017.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Wang L and Shen Y: Imbalance of
circulating T-lymphocyte subpopulation in gastric cancer patients
correlated with performance status. Clin Lab. 59:429–433.
2013.PubMed/NCBI
|
|
8
|
Karabulut M, Usul AC, Serimez M and
Karabulut S: Serum IL-17 levels can be diagnostic for gastric
cancer. J BUON. 24:1601–1609. 2019.PubMed/NCBI
|
|
9
|
Tang WJ, Tao L, Lu LM, Tang D and Shi XL:
Role of T helper 17 cytokines in the tumour immune inflammation
response of patients with laryngeal squamous cell carcinoma. Oncol
Lett. 14:561–568. 2017.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Treskova I, Topolcan O, Windrichova J,
Simanek V, Slouka D, Treska V and Kucera R: OPG, OPN, EGF and VEGF
levels at individual Breslow score stages in malignant melanoma.
Anticancer Res. 38:4907–4911. 2018.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Kumar U and Singhal U: Anorectal melanoma:
An unusual cause of rectal bleeding. J Clin Diagn Res. 11:D12–D13.
2017.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Yang J, Xiao P, Sun J and Guo L:
Anticancer effects of kaempferol in A375 human malignant melanoma
cells are mediated via induction of apoptosis, cell cycle arrest,
inhibition of cell migration and downregulation of m-TOR/PI3K/AKT
pathway. J BUON. 23:218–223. 2018.PubMed/NCBI
|
|
13
|
Ranjith S, Muralee M, Sajeed A, Arun PM,
Cherian K, Nair CK, Augustine P and Ahamed I: Anorectal melanoma:
Experience from a tertiary cancer care centre in South India. Ann R
Coll Surg Engl. 100:185–189. 2018.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Bulut N, Dagistanli S, Yilmaz B and Atay
OF: Surgical approach to anorectal melanoma with PET-CT staging: A
case report. Surg J (NY). 3:e177–e180. 2017.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Cai ED and Kim J: Identification of novel
targetable mutations in metastatic anorectal melanoma by
next-generation sequencing. JAAD Case Rep. 3:539–541.
2017.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Virgilio E, Mercantini P, Santangelo G,
Canali G, Peritore V and Balducci G: Anorectal melanoma: A rare
aggressive type of melanoma. Anz J Surg. 87:421–422.
2017.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Sousa IG, Do AM, Simi KC, Bezerra MA,
Andrade RV, Maranhao AQ and Brigido MM: MicroRNA expression
profiles in human CD3(+) T cells following stimulation with
anti-human CD3 antibodies. BMC Res Notes. 10(124)2017.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Hofmann H: A foot tumour as late cutaneous
lyme borreliosis: A new entity or a variant of an inflammatory
proliferative reaction to borrelia burgdorferi? Br J Dermatol.
177:906–907. 2017.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Nie W, Yu T, Sang Y and Gao X:
Tumor-promoting effect of IL-23 in mammary cancer mediated by
infiltration of M2 macrophages and neutrophils in tumor
microenvironment. Biochem Biophys Res Commun. 482:1400–1406.
2017.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Amicarella F, Muraro MG, Hirt C, Cremonesi
E, Padovan E, Mele V, Governa V, Han J, Huber X, Droeser RA, et al:
Dual role of tumour-infiltrating T helper 17 cells in human
colorectal cancer. Gut. 66:692–704. 2017.PubMed/NCBI View Article : Google Scholar
|