Introduction
Syphilis is the most common sexually transmitted
disease whose worldwide incidence fluctuates annually or per
decade. Although syphilis is a curable disease with accessible
treatments and diagnostic tests, it still represents a serious
public health problem (1).
Syphilis, the great imitator, which can mimic many dermatological
conditions (psoriasis, pityriasis rosea, parapsoriasis, drug
reactions, lichen planus, sarcoidosis, infectious mononucleosis,
lymphoma, and others) (1,2) can have various clinical aspects, from
classical to particular forms (seronegative primary syphilis,
syphilitic balanitis without a chancre, ocular syphilis) (3-5).
Worldwide, about 6 million new cases of syphilis per year are
reported, with a mortality of about 5% in the neonatal or fetal
period (6). International
prevention programs for sexually transmitted diseases have focused
on 4 diseases (syphilis, gonorrhea, trichomoniasis and Chlamydia
infections). The target of these programs for 2030 is to reduce the
overall incidence of infections; to decrease congenital syphilis to
<50 cases per 100,000 newborns and the incidence of syphilis by
90% (7).
In the last decade, the increase in syphilis
incidence is based on unrestricted sexual behavior with unprotected
contact between multiple partners (8), including the same sex. In 2017, the
USA reported the highest rate of syphilis in the last 15 years
(9), the data being similar to some
European countries.
The high incidence of human immunodeficiency virus
(HIV) infection, especially in the MSM (men who have sex with men)
category, is also correlated with an increase in syphilis
incidence. Syphilis-HIV co-infection is higher in MSM. Karp et
al estimate that the risk of syphilis-HIV co-infection is 8
times higher in this category of patients (10).
In September 2019 at the International Union Against
Sexually Transmitted Infections (IUSTI) Conference in Tallinn,
Estonia, the latest results of the reported syphilis incidence in
Europe were announced. Georgia (33 cases per 100,000 inhabitants)
had the highest incidence, followed by Malta (18.6 cases per
100,000 inhabitants), Russia (16.8 cases per 100,000 inhabitants),
UK (13.6 cases per 100,000 inhabitants) and Switzerland (10.7 cases
per 100,000 inhabitants) (11).
Available data for Romania rank it among the
countries with less than 5 cases per 100,000 inhabitants (11). In Romania, between 2007 and 2017,
there was a downward trend in the incidence of syphilis from 20.1
to 4.1 cases per 100,000 inhabitants (12). This decrease may not be factual and
may be due to the elimination of certain filters that detect the
luetic infection. Currently, it is mandatory to perform these tests
only in marriage, pregnancy, blood donation and exposure to a
syphilis-infected person.
For proper assessment, it is necessary to implement
intensive population education programs, reintroduce the obligation
to perform specific serological investigations (at employment or
changing jobs), and actively detect latent, atypical and
asymptomatic syphilis cases. A delicate topic is represented by
untreated mothers infected with Treponema pallidum diagnosed
late in pregnancy or at birth (due to unregular check-ups during
pregnancy). Their newborns have a high risk of developing
congenital syphilis. In addition, the lack of benzathine-penicillin
G (BPG) on the Romanian pharmaceutical market has driven doctors to
adopt alternative treatment regimens with some oral antibiotics
having a possible lower efficacy than the classic schemes.
Our primary objective was to analyzed the evolution
of syphilis incidence in the last decade in Sibiu County, and we
correlated the results with national and international data. Our
secondary objectives were to correlated the demographic data with
clinical forms, disease stages, the serologic treatment response
and treatment followed by patients with syphilis, over a period of
10 years (2009-2018), in Sibiu County, Romania.
Patients and methods
Sample selection criteria
We conducted a retrospective study over 10 years
(from January 2009 to December 2018) which included 396 patients
with syphilis diagnosed, monitored, and treated at the
Dermato-Venerological Division of the Clinical Hospital of Sibiu.
In our group of patients, we analyzed: the syphilis incidence,
demographic data (sex, background, marital status, age group, level
of education and occupation), the sources of infection and the
number of declared contacts, the evolution of syphilis-HIV
co-infection cases, the disease stages and the followed treatment
schemes. To identify the sources of infection, the patients
answered questions regarding their sexual partners and the
prevention methods that they used. Epidemiological and clinical
data were included in a personal file. All the patients were tested
positive for non-treponemal [venereal disease research laboratory
(VDRL) or rapid plasma reagin (RPR)] and treponemal tests
[Treponema pallidum hemagglutination assay (TPHA)]. Non-treponemal
tests (VDRL or RPR) were used to determine the serologic treatment
response after 6 months and 1 year from diagnosis.
Statistical analysis
We analyzed the venerology records of 396 patients
diagnosed with syphilis in the last 10 years in Sibiu County.
Statistical analysis was performed using SPSS statistics software
(version 25.0; IBM Corp.) with alpha (α)=0.05 and CI (confidence
interval)=95%. The variables are expressed in numbers and
percentages. The results are presented as median ± standard
deviation (SD). To assess the statistical significance, we
calculated the P-value using the Kolmogorov-Smirnov test. P-value
<0.05 was considered as indicative of statistically
significance.
Statement of ethics
The clinical study received the approval of the
Ethics Commission of the Sibiu County Clinical Hospital (no.
25413/05.12.2019).
Results
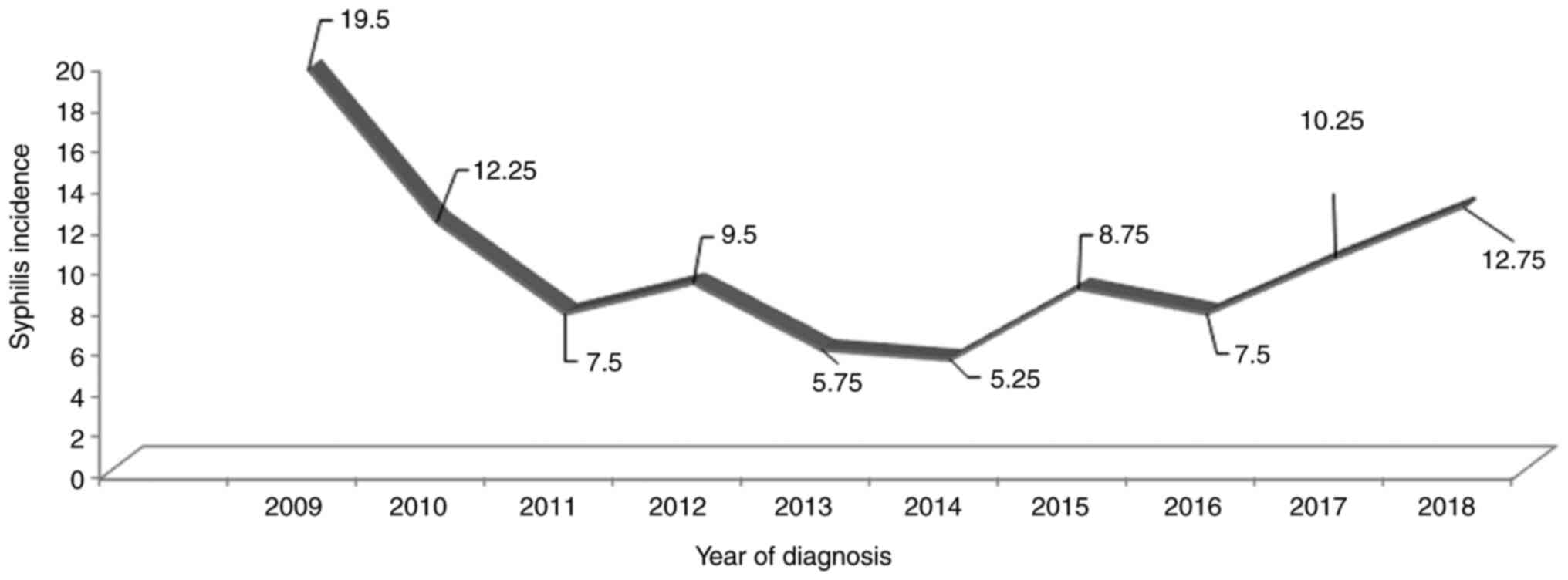
During the years 2009-2018 in Sibiu county (average
population of 400,000 inhabitants), the average syphilis incidence
was 9.90 new cases per 100,000 inhabitants. In this period, the
incidence of syphilis decreased from a maximum of 19.5 new
cases/100,000 (in 2009) to a minimum of 5.25/100,000 (in 2014), and
then increased to 12.75/100,000 (in 2018) (Fig. 1).
The average age (± SD) of the individuals diagnosed
with syphilis was 35.39±14.64 years, and 76.52% belonged to the age
group of 15-45 years. The majority of the syphilis patients were
men (54.29%), from urban areas (67.42%), with a degree of schooling
of grades 9-12 (51.01%), unmarried (41.92%), worker (34.60%) or
unemployed (32.32%) (Table I).
 | Table IDemographic profile of the individuals
diagnosed with syphilis over a period of 10 years (2009-2018) in
Sibiu County, Romania (N=396). |
Table I
Demographic profile of the individuals
diagnosed with syphilis over a period of 10 years (2009-2018) in
Sibiu County, Romania (N=396).
| Characteristic | Subcategory | n (%) | P-value |
|---|
| Sex | Male | 215 (54.29) | <0.001 |
| | Female | 181 (45.71) | |
| Area of
residence | Urban | 267 (67.42) | <0.001 |
| | Rural | 129 (32.58) | |
| Age groups
(years) | Under 1 year | 3 (0.76) | 0.001 |
| | 1-14 years | 1 (0.25) | |
| | 15-29 years | 157 (39.65) | |
| | 30-44 years | 146 (36.87) | |
| | 45-59 years | 54 (13.64) | |
| | 60-74 years | 33 (8.33) | |
| | Over 75 years | 2 (0.50) | |
| Degree of
schooling | Without | 18 (4.55) | <0.001 |
| | Grades 1-4 | 34 (8.59) | |
| | Grades 5-8 | 88 (22.22) | |
| | Grades 9-12 | 202 (51.01) | |
| | Higher education | 54 (13.64) | |
| Marital status | Married | 108 (27.27) | <0.001 |
| | Unmarried | 166 (41.92) | |
| | Divorced | 22 (5.56) | |
| | Widower | 12 (3.03) | |
| | Concubinage | 88 (22.22) | |
| Occupation | Unemployed | 128 (32.32) | <0.001 |
| | Worker | 137 (34.60) | |
| | Professional | 45 (11.36) | |
| | Retiree | 44 (11.11) | |
| | Driver | 9 (2.27) | |
| | Others | 33 (8.33) | |
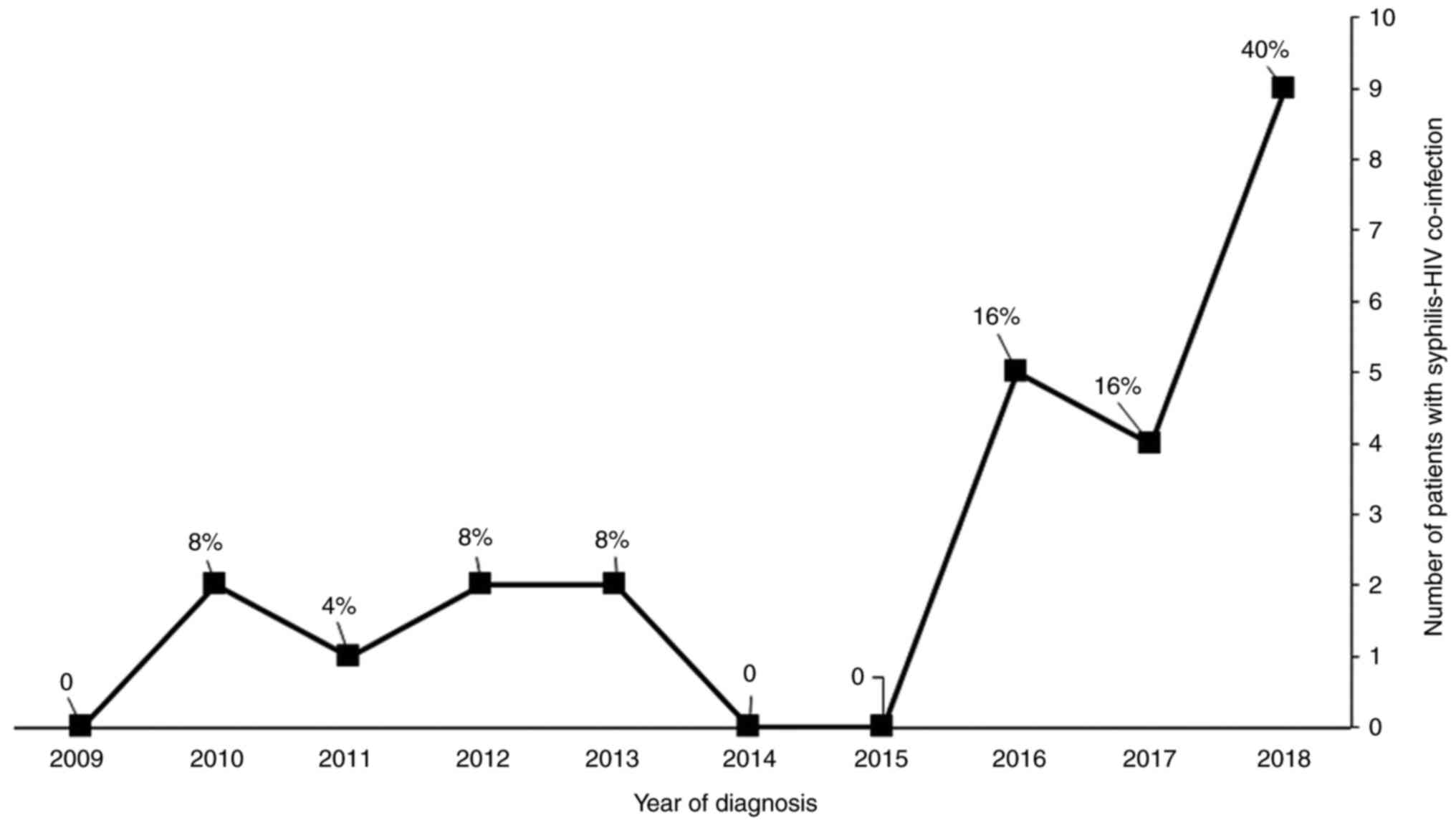
Out of the 396 syphilis patients, 25 were HIV
coinfected (6.31%). In this category of patients, over 50% declared
that they were MSM (56%), 40% were heterosexual, and 4% were female
sex workers. In this group of patients (syphilis-HIV co-infection),
an ascending progressive distribution was found; 40% of these cases
were confirmed in 2018 (Fig.
2).
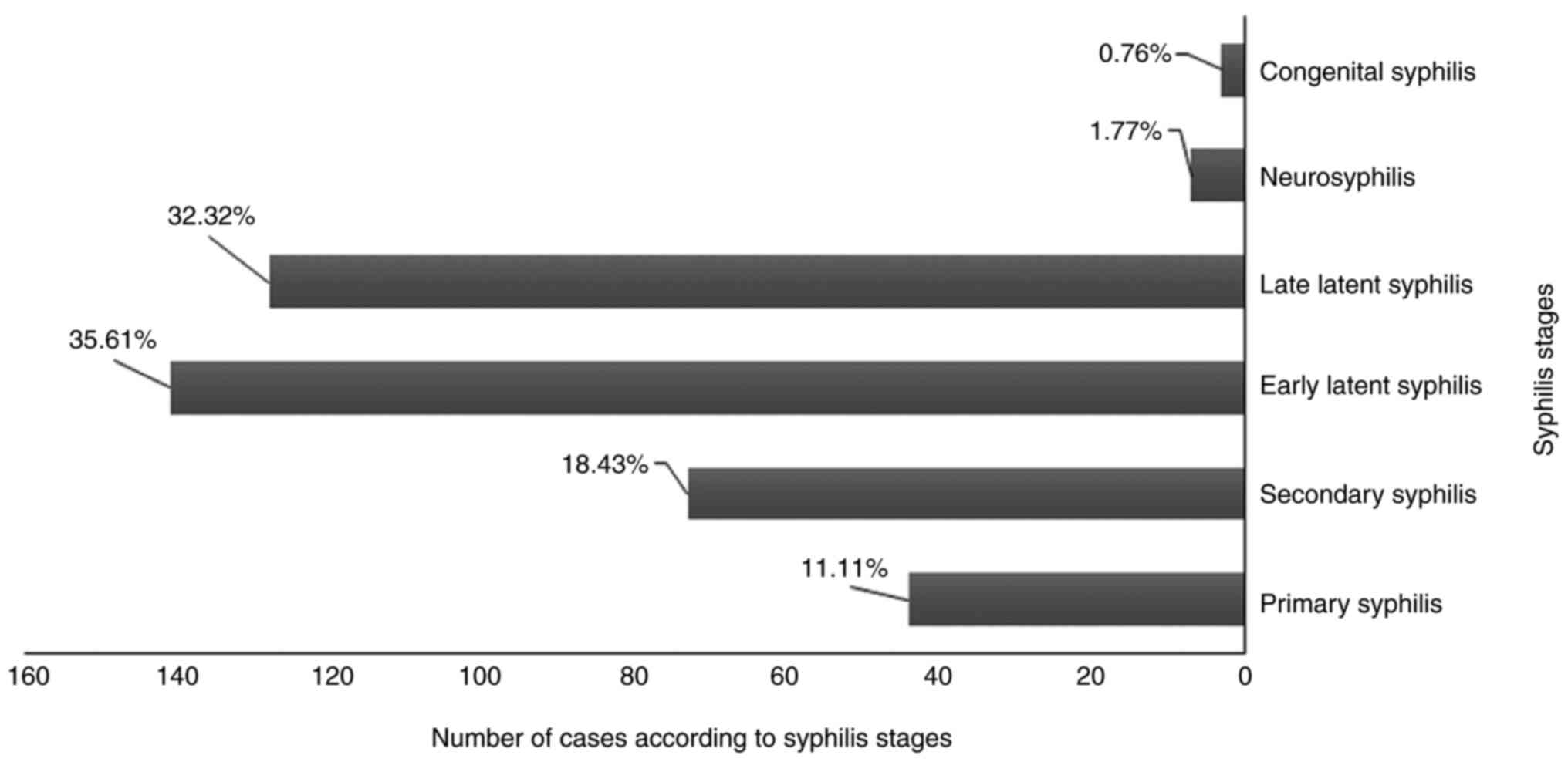
Analyzing the syphilis stages, we observed that
early (35.61%) and late latent syphilis (32.32%) were most common
(Fig. 3) (P<0.001).
Regarding the detection method, over 1/3 of the
cases were diagnosed by epidemiological investigation (39.65%),
respectively by investigating all the declared contacts of a new
case of syphilis. Other detection methods were: unspecified
(32.58%), pregnancy/birth (14.39%), blood donation (6.82%), tests
performed at employment (4.80%) and prenuptial assessment (1.77%)
(P<0.001). From the 396 syphilis patients, 276 contacts were
declared by epidemiological investigation, and 183 contacts out of
the 276 were found, the rest being accidental relationships with
unknown people.
Regarding the syphilis treatment scheme, the Health
Ministry's indications (adapted to each stage) were respected. In
the last decade, there was a transition from the classic scheme
with BPG/penicillin (100% in 2009) to alternative therapies, mainly
with cephalosporins in 2018 (56.86%) (P<0.001) (Table II).
 | Table IIThe therapy followed by our syphilis
patients over a period of 10 years (2009-2018). |
Table II
The therapy followed by our syphilis
patients over a period of 10 years (2009-2018).
| | No of | Classic schemes
(Benzathine-penicillin G/penicillin) | Cephalosporins
(Cefuroxime/ceftriaxone) | Macrolides
(Azithromycin/erythromycin) | Doxycycline |
|---|
| Year | patients | n (%) | n (%) | n (%) | n (%) |
| 2009 | 78 | 78(100) | 0 | 0 | 0 |
| 2010 | 49 | 46 (93.88) | 1 (2.04) | 2 (4.08) | 0 |
| 2011 | 30 | 27 (90.00) | 1 (3.33) | 0 | 2 (6.67) |
| 2012 | 38 | 36 (94.74) | 0 | 2 (5.26) | 0 |
| 2013 | 23 | 21 (91.30) | 2 (8.70) | 0 | 0 |
| 2014 | 21 | 17 (80.95) | 4 (19.05) | 0 | 0 |
| 2015 | 35 | 30 (85.71) | 5 (14.29) | 0 | 0 |
| 2016 | 30 | 25 (83.33) | 5 (16.67) | 0 | 0 |
| 2017 | 41 | 16 (39.02) | 18 (43.90) | 0 | 7 (17.07) |
| 2018 | 51 | 7 (13.73) | 29 (56.86) | 8 (15.69) | 7 (13.73) |
The serologic treatment response was evaluated at 6
months and 1 year, according to syphilis stages. The serologic
treatment response (STR) was relatively similar in all treatment
groups (56.32% for BPG/ penicillin; 61.11% for cephalosporins and
72.73% for doxycycline). Out of all of the groups, the
azithromycin/erythromycin had the lowest STR (50%).
Discussion
In Sibiu County, from January 2009 to December 2018,
the overall incidence of syphilis decreased from 19.75 new
cases/100,000 inhabitants in 2009 to 5.25/100,000 in 2014 but
reached 12.75/100,000 in 2018. There was a decrease of 35.90% per
decade if we compare the year 2009 with 2018. From January 2009 to
December 2018, the average syphilis incidence in our county was
9.90/100,000 inhabitants, above the national average (4.1/100,000
in 2017) (12). The downward trend
of the average incidence of syphilis in our county is in accordance
with the national data (20.1/100,000 in 2007 to 4.1/100,000 in
2017) (12), but in discordance
with the European data (12). An
incomplete report of the new cases of syphilis by the private
offices can be considered to explain these results.
The European Center for Disease Prevention and
Control analyzed the data that were reported by 30 European
countries in 2010-2017 and observed a significant increase in the
incidence of syphilis (between 123 and 876%) in some European
countries (Iceland, Ireland, UK, Germany, and Malta) and a decrease
of over 50% in other countries, including Romania (13). Furthermore, in the US, after the
year 2000, the incidence of syphilis increased in both men and
women (6). The largest increase in
luetic infection is cited by Chen et al in China, where
after 1970, in 25 years, the syphilis incidence increased by
250-1,000 times (14).
In our study group, the frequency of luetic disease
was higher in men (54.29%), with a male-to-female ratio of 1.18:1,
similar to that reported nationally (below 2:1) (12). Globally, men have a 6-8 times higher
risk of having syphilis than women. In Europe in 2013, the M:F
ratio was 8.4:1.6, and in the US, it was 15.6:1.9 in 2016; the risk
being higher for MSM (6). In our
study, the lower M:F ratio can be explained both by the lower
number of declared MSM (less than 20%) and by the higher number of
women diagnosed with syphilis during pregnancy/birth compared with
other countries (13).
The Centers for Disease Control and Prevention,
Atlanta, USA, published a study in which syphilis patients were
more frequently residing in urban areas while Thomas et al
observed a higher concentration of syphilis cases in rural areas in
North Carolina, USA (15,16). The patients with syphilis in our
study came mainly from urban areas (67.42%), where internet use is
more accessible, and sexual activity is more intense, with multiple
partners, sometimes of the same sex and with condomless sex.
Over three-fourths of our patients with syphilis
were aged between 15 and 45 years (76.52%), with a maximum
incidence between 15 and 30 years (4.1 cases per 100,000
inhabitants). The disease's maximum incidence in both women and men
was between 20 and 24 years, according to our National Institute of
Public Health (NIPH). In Europe, there is a maximum of cases in the
age groups 25-34 years (16/100,000) and 35-44 years (13/100,000)
(17). All data confirm the maximum
incidence of syphilis in the age groups with more intense sexual
activity.
Analyzing the degree of schooling of our syphilis
patients in the last decade, we noted that 51.01% of the patients
had an educational level of grade 9-12. We found that many patients
with syphilis had a medium level of education (grade 9-12) (51.01%)
compared to those with no or little education (0 or grades 1-4)
(13.14%), where we would have expected a higher incidence of the
disease.
Analyzing the marital status in our group of
patients, we noted that patients with syphilis were unmarried
(41.92%) or exhibited live-in cohabitation, usually from a poor
socioeconomic status and a low level of education (grades 5-8)
(22.22%). It should be noted that about 1/4 of patients (27.27%)
contacted the disease during marriage through extramarital affairs.
Worldwide, poor socioeconomic status is a recognized risk factor,
indirectly correlated with the syphilis prevalence, favoring some
sexual behaviors (ex. condomless sex), without awareness of the
possible consequences (17).
The distribution of the patients by disease stages
was as follows: latent (early, 35.61%; late, 32.32%), secondary
(18.43%), primary (11.11%), tertiary (1.77%) and congenital
syphilis (0.76%). In our country, most cases of syphilis are early
latent forms (12). Inexplicably,
in our study, the tertiary syphilis was three times higher (1.77%)
compared to data from our NIPH.
This fact could suggest the possibility that
tertiary syphilis may be underdiagnosed. Without the awareness of
medical specialists in the field about the existence of these
syphilis forms (that can occur silently or with neuropsychic
pleomorphic manifestations), and specific investigations
(cerebrospinal fluid serology for syphilis in dynamics), and
without interdisciplinary collaboration, neurosyphilis could remain
undiagnosed. We need to consider that tertiary syphilis can
manifest itself after 20 years from the moment of infection, in
individuals with low social and economic conditions (a vulnerable
category that also exists in Romania), without any specific
treatment. This could explain our result.
For the detection of syphilis in Romania, lifelong
analysis filters are used (at marriage, in pregnancy, at blood
donation or, a declaration of possible infected contacts by a
patient already diagnosed with syphilis). In our study, over 50% of
cases were diagnosed by an epidemiological investigation,
respectively by investigating all of the declared contacts of a new
case of syphilis (39.65%) and by mandatory testing of pregnant
women (14.39%). The high percentage of syphilis cases diagnosed
during pregnancy or at birth is concerning; this category of
patients exposing their fetus to the transplacental transmission of
the infection, with the possibility of developing congenital
syphilis in newborns. The epidemiological control of the syphilis
contacts is significant in order to stop the transmission of the
disease (through unidentified and untreated infected contacts). The
declaration of all contacts by the infected person is essential for
breaking the epidemiological chain in syphilis. From the group of
396 patients diagnosed with syphilis, we identified 276 contacts
through epidemiological investigation, of which 183 were identified
(66.30%). The unidentified individuals were accidental sexual
contacts with unknown persons from the country and/or from
abroad.
Syphilis in pregnant women is an extremely sensitive
topic for any society. The goal of the national health programs is
to reduce this category of patients to 0. In 2009 and 2018, we
analyzed the percentage of syphilis positivity in tested pregnant
women. The percentage varied between 1.87% and 1.11%, the average
being 1.82% per decade, except for 2011 (a peak at 5.02%). Given
the possibility that the pregnant woman's syphilis evolved to
congenital syphilis (with the transmission of the infection from
mother to fetus), the presented data are alarming.
From January 2009 to December 2018, out of the
30,000 newborns in Sibiu County, 3 cases of congenital syphilis
were diagnosed, this representing 0.76% of all cases of syphilis.
At the national level (in 2016), there were 6 cases declared. Of
all the congenital syphilis cases declared in Europe between 2007
and 2017, 11% were from Romania (12). Also, in Romania, the rate of
congenital syphilis decreased from 12.1 cases/100,000 newborns in
2007 to 3 cases/100,000 newborns in 2017(12). Internationally, by 2018, 11
countries have declared that they have eliminated the
transplacental transmission of luetic infection, Belarus and
Moldova being the ones from Europe (7). On the other hand, the incidence of
congenital syphilis in Romania is higher than other regions of
Europe (0.4/100,000 newborns) and Southeast Asia (0.9/100,000
newborns) and lower than those found in Africa (48.9/100,000
newborns) and some regions of America (22.8/100,000 newborns)
(7).
Pregnancy monitoring is accomplished through primary
care. The mother's responsibility to perform luetic serology in the
first and the last trimester of pregnancy and the pregnant woman's
education and her partner regarding healthy sexual behavior are
useful tools for preventing syphilis. In addition, pregnant women
with syphilis require a specific therapy that needs to be initiated
as early as possible to reduce the risk of congenital syphilis.
In the last 2 decades, in Europe, the increased
number of MSM has been reflected in the incidence of syphilis in
association with HIV infection, with a higher rate in urban areas.
Also, drug use and promiscuous life-style are correlated with the
statistical increase in syphilis-HIV co-infection cases. In
Romania, the number of MSM and extramarital relationships, with
unprotected contacts, with unknown people has increased in the last
years. In our study, over the 10-year period, the syphilis-HIV
coinfection was identified at 6.31% of the cases, with a maximum of
cases in 2018 (40%). From this category of patients, 56% were MSM.
The presented results urge us to relaunch national programs for the
prevention of sexually transmitted diseases. We need to disseminate
sexual health information to risk groups and the general
population, especially to young people, who have a higher risk of
contracting a sexually transmitted disease.
In our study, the syphilis treatment scheme was in
accordance with the Romanian Health Ministry, adapted to each stage
of the disease. Alternative therapies (ceftriaxone, doxycycline,
azithromycin) are recommended to be used only in case of allergy to
penicillin. In 2009, all patients received benzathine-penicillin G
treatment (BPG) (primary, secondary, late, and early latent
syphilis) or penicillin (congenital syphilis, neurosyphilis, or
pregnant women with syphilis). Since 2017, due to the lack of BPG
in the Romanian pharmaceutical market, the chosen second line of
treatment was cephalosporins (in 2018, 56.86% of the cases were
treated with cefuroxime or ceftriaxone).
Out of the 396 syphilis patients, 172 were lost to
follow-up (43.43%). We determined the serologic treatment response
(STR) for 224 patients after 6 months (primary, secondary, and
congenital syphilis) and 1 year from diagnosis (latent and tertiary
syphilis). We consider that STR was achieved when VDRL or RPR had a
≥4-fold decline (18). We compared
the STR obtained after BPG/penicillin (56.32%) vs. cephalosporins
(61.11%) or doxycycline therapy (72.73%), and we observed that this
was relatively similar in all treatment groups. Out of all of the
groups, treatment with azithromycin/erythromycin had the lowest STR
(50%). For primary, secondary, and early latent syphilis, Cao et
al demonstrated that STR to cephalosporins vs. BPG was
approximately similar (90.2 vs. 78%) after 6 months (19).
In conclusion, the incidence of syphilis from
January 2009 to December 2018 in Sibiu County showed a downward
trend, following the national data, but in antithesis with the
international data. Our county's syphilis patient demographic
profile is male, aged 15-30 years, from the urban area, with an
educational level of grades 9-12, unmarried, worker or unemployed.
During this period, our county's progressive increase in
syphilis-HIV co-infection and neurosyphilis cases is concerning.
Due to the lack of the pharmaceutical product, first-line therapy
with benzathine-penicillin G/penicillin or penicillin has been
replaced in the last 3 years with the 2nd line of treatment
(cephalosporins, doxycycline, macrolides). The serologic treatment
response was relatively similar to BPG/penicillin, cephalosporins,
and doxycycline, but lower for macrolides.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
All the data are available from the corresponding
author.
Authors' contributions
GMI conducted the research creation and design,
analysis and interpretation of patient data, manuscript drafting
and critical revision of the manuscript for important intellectual
content. MR conducted the design and critical revision of the
manuscript for important intellectual content. Both authors read
and approved the manuscript and agree to be accountable for all
aspects of the research in ensuring that the accuracy or integrity
of any part of the work are appropriately investigated and
resolved.
Ethics approval and consent to
participate
The study was approved by the Ethics Committee of
the County Emergency Hospital of Sibiu, Romania (no.
25413/05.12.2019).
Patient consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
References
|
1
|
Danescu SA, Szolga B, Georgiu C, Surcel A
and Senila SC: Unusual manifestations of secondary syphilis: Case
presentations. Acta Dermatovenerol Croat. 26:186–188.
2018.PubMed/NCBI
|
|
2
|
Rotaru M, Maniu H, Lisandru M and Iancu G:
Diagnostic difficulties in secondary syphilis associated with
psoriasis vulgaris-clinical case. Dermatovenerologia. 61:249–256.
2016.
|
|
3
|
Parker SR, Correnti C, Sikora K and Parker
DC: Seronegative syphilis: Another case for the great imitator. Int
J Infect Dis. 18:104–105. 2014.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Oanta A and Irimie M: Syphilitic balanitis
of follmann. Int J Dermatol. 53:830–831. 2014.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Etheridge T, Bowen RC, Raven M, Snow KB,
Urban AW and Chang JS: Ocular syphilis: Clinical manifestations and
treatment course. WMJ. 118:191–195. 2019.PubMed/NCBI
|
|
6
|
Kojima N and Klausner JD: Un update on the
global epidemiology of syphilis. Curr Epidemiol Rep. 5:24–38.
2018.PubMed/NCBI View Article : Google Scholar
|
|
7
|
World Health Organization: Sexually
Transmitted Infections (STIs). https://www.who.int/publications/data/gho/data/themes/sexually-transmitted-infections.
Accessed June 16, 2020.
|
|
8
|
Grad AI, Senila SC, Cosgarea R, Tataru AD,
Vesa SC, Vica ML, Matei HV and Ungureanu L: Sexual behaviors,
attitudes, and knowledge about sexually transmitted infections: A
cross-sectional study in Romania. Acta Dermatovenerol Croat.
26:25–32. 2018.PubMed/NCBI
|
|
9
|
Centers for Disease Control and
Prevention: Syphilis. https://www.cdc.gov/std/stats17/syphilis.htm. Accessed
July 2, 2020.
|
|
10
|
Karp G, Schlaeffer F, Jotkowitz A and
Riesenberg K: Syphilis and HIV co-infection. Eur J Intern Med.
20:9–13. 2009.PubMed/NCBI View Article : Google Scholar
|
|
11
|
International Union Against Sexually
Transmitted Infections 2019 European Congress: Abstract Book.
www.conference-expert.eu/en/iusti2019/en/abstract-book/1.
Accessed June 2, 2020.
|
|
12
|
European Centre for Disease Prevention and
Control: Syphilis and congenital syphilis in Europe-A review of
epidemiological trends (2007-2018) and options for response.
https://www.ecdc.europa.eu/sites/default/files/documents/syphilis-and-congenital-syphilis-in-Europe.pdf.
Accessed February 18, 2021.
|
|
13
|
European Centre for Disease Prevention and
Control: Syphilis notifications in the EU/EEA up by 70% since 2010.
https://www.ecdc.europa.eu/en/news-events/syphilis-notifications-eueea-70-2010.
Accessed October 11, 2020.
|
|
14
|
Chen ZQ, Zhang GC, Gong XD, Lin C, Gao X,
Liang GJ, Yue XL, Chen XS and Cohen MS: Syphilis in China: Results
of a national surveillance programme. Lancet. 369:132–138.
2007.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Singh AE and Romanowski B: Syphilis:
Review with emphasis on clinical, epidemiologic, and some biologic
features. Clin Microbiol Rev. 12:187–209. 1999.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Thomas JC, Kulik AL and Schoenbach VJ:
Syphilis in the South: Rural rates surpass urban rates in North
Carolina. Am J Public Health. 85:1119–1122. 1995.PubMed/NCBI View Article : Google Scholar
|
|
17
|
European Centre for Disease Prevention and
Control: Syphilis and congenital syphilis in Europe-A review of
epidemiological trends (2007-2018) and options for response.
https://www.ecdc.europa.eu/en/publications-data/syphilis-and-congenital-syphilis-europe-review-epidemiological-trends-2007-2018.
Accessed June 28, 2020.
|
|
18
|
Brown DL and Frank JE: Diagnosis and
management of syphilis. Am Fam Physician. 68:283–290.
2003.PubMed/NCBI
|
|
19
|
Cao Y, Su X, Wang Q, Xue H, Zhu X, Zhang
C, Jiang J, Qi S, Gong X, Zhu X, et al: A multicenter study
evaluating Ceftriaxone and Benzathine Penicillin G as treatment
agents for early syphilis in Jiangsu, China. Clin Infect Dis.
65:1683–1688. 2017.PubMed/NCBI View Article : Google Scholar
|