Introduction
Continuous refinement of percutaneous endoscopic
transforaminal discectomy (PETD) has resulted in the development of
an effective treatment for intraspinal herniation, intervertebral
foramen herniation, polar lateral herniation and intervertebral
disc prolapse (1). With the
invention and use of new tools, including the ring saw and the
microscopical abrasion drill, PETD has evolved from indirect
decompression, by removing only the central nucleus pulposus, to
direct decompression, by removing the intervertebral disc (2). PETD is widely used owing to its many
advantages, including minimal operative wound, minor effect on
spinal stability, reduced postoperative pain and local scar
formation and fast recovery (3).
However, operation at the L5-S1 segment is more difficult, owing to
the occlusion of the iliac crest, inclination of the intervertebral
disc, stenosis of the intervertebral foramen and the presence of
other complex anatomical structures (4).
Operation at the L5-S1 segment is challenging given
the anatomical structure of this region. A number of scholars
believe that the working casing cannot increase the angle with the
centre line from the horizontal plane of the L5-S1 segment;
therefore, it is impossible to overcome the occlusion of the
herniated disc by the facet joint (4). From the coronal point of view, the
working casing is not in the same horizontal plane as the
intervertebral space, making it more difficult to remove the disc
tissue. Lee et al (5)
suggest that the higher iliac crest and tilted L5-S1 intervertebral
disc increase the angle of the working casing and enable deviation
from the intervertebral disc and that whether the casing is in a
good position directly affects the success or failure of the
operation. Ahn et al (6)
believe that the special anatomical structure of the L5-S1 segment
often leads to prolonged operation time, increased radiation
exposure and even operation failure. A study has proposed moving
the iliac crest downwards by through changing the patient's
position may be beneficial, however, this operation still has many
difficulties in its practical applications (7).
To overcome the challenging anatomical factors,
percutaneous endoscopic interlaminar discectomy (PEID) is also a
common approach for operation at the L5-S1 segment. This method can
effectively avoid occlusion of the iliac crest (8). The most significant difference between
PETD and PEID is that PEID exposes the nerve tissue and then treats
the disc, whereas PTED treats the disc first and finally exposes
the nerve tissue. PEID causes greater stimulation of the nervous
tissue, and patients under local anaesthesia have poor
intraoperative tolerance and are more likely to have nerve injuries
(9). The endoscopic transiliac
approach proposed by Choi et al (10) can reduce the working channel
inclination and direct it to the L5-S1 intervertebral foramen,
lowering the possibility of damaging the exiting root nerve.
However, using this approach results in the casing developing a
narrow range of movement after the establishment of the working
channel, possibly resulting in ilium fractures, gluteal epithelial
nerve damage and uncontrollable bleeding (4,8,9). These
factors have limited the development of the endoscopic transiliac
approach.
Two percutaneous endoscopic operations, namely
endoscopic discectomy via the intervertebral foramen approach and
endoscopic discectomy via the posterior interlaminar approach, are
currently available for L5-S1 lumbar disc herniation; however, both
these approaches have advantages and disadvantages. Previous
studies have demonstrated that PETD is preferred for shoulder type
recurrent disc herniation that is centrally located, while PEID is
preferred for axillary type migrated discs, especially those of a
high grade (8,9). Numerous studies have proposed that a
high iliac crest is the major obstacle for PETD at the L5-S1
segment or even the L4-L5 segment (4,9,11,12).
However, a ‘high iliac crest’ itself is a vague definition without
quantitative standards. Furthermore, a study on the influence of
the iliac crest on L5-S1 segment surgery have rarely been reported
(4).
In the present study, the TESSYS technique in PTED
invented by Hoogland (13) was used
to treat 76 patients with L5-S1 lumbar disc herniation.
Furthermore, the clinical effects of this technique and the
influence of the iliac crest height on the clinical effects were
analysed.
Materials and methods
Inclusion criteria
The inclusion criteria were as follows: i) No lumbar
instability at the L5-S1 segments was shown on the X-ray films
taken in the lumbar dynamic position; ii) L5-S1 single-segment
lumbar disc herniation; iii) no complications of spinal diseases,
including lumbar spinal stenosis, spinal deformity and spinal
tuberculosis and iv) ineffective conservative treatment. A total of
76 patients with lumbar disc herniation, including 46 male and 30
female patients aged 19-69 (mean age, 47.8±6.4) years, met the
inclusion criteria and were treated with the THESSYS technique at
the Second Affiliated Hospital and Third Affiliated Hospital of
Xi'an Jiaotong University between January and December 2016. The
study was approved by the Medical and Biological Ethics Committee
of Xi'an Jiaotong University Health Science Center, and all
participants signed the informed consent to the clinical study.
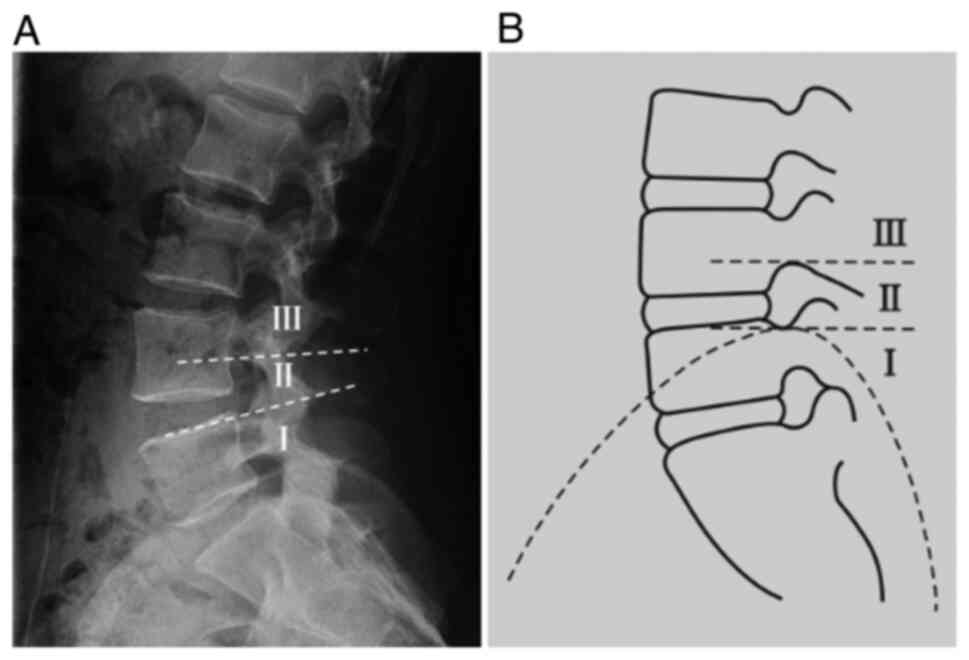
These patients were divided into the following three groups
according to the positional relation between the highest point of
the iliac crest and the L4 and L5 pedicles in the lateral lumbar
X-ray film: Group I, iliac crest height below the upper edge
horizontal line of the L5 pedicle (n=42); group II, with iliac
crest height between the lower edge horizontal line of the L4
pedicle and the upper edge horizontal line of the L5 pedicle (n=29)
and group III, iliac crest height above the lower edge horizontal
line of the L4 pedicle (n=5) (Fig.
1).
Operation methods
Patients were placed on their healthy side (or on
the side with mild symptoms if the patient has symptoms on both
sides). The puncture point was determined via anteroposter
fluoroscopy (10-12 cm in the midline after paraperitoneal opening
and 1 cm above the iliac crest). Then, 1% lidocaine was used for
local anaesthesia. A sharp knife was used to place the guide wire,
guide rod, casing and ring saw step by step at a site approximately
0.8 cm from the puncture point incision. Finally, a 7.5 cm working
casing was placed. The intervertebral foramen mirror was connected
to the light source and camera when the fluoroscope shows that the
normal position of the tip of the working casing is on the inner
edge of the vertebral pedicle and laterally on the posterior edge
of the vertebral body (TESSYS technique). The degenerated and
herniated disc tissues were completely removed using flexible
nucleus pulposus forceps by rotating the working channel during the
operation, followed by radio frequency haemostasis and ablation.
The criteria for ending the operation were S1 nerve root relaxation
after decompression and normal pulsation of the dural sac area or
collapse of the posterior longitudinal ligament.
Evaluation indicators
The duration of each operation was recorded,
perioperative complications were observed and the Oswestry
Disability Index (ODI) (14) and
Visual Analogue Scale (VAS) (15)
of the lower back and lower limbs before operation and 1 week and
1, 3 and 12 months after the operation were evaluated. Higher VAS
scores indicate more severe pain, and higher ODIs indicate more
serious dysfunction.
Statistical analysis
The statistical software SPSS 18.0 (IBM Corp.) was
used for data analysis. Data are presented as the mean ± SD.
Repeated measures analysis of variance was used for comparisons
before and after the operation, followed by a Tukey's post hoc test
for comparisons among groups. One-Way ANOVA was performed for the
comparisons between three groups, and the Tukey's post hoc test was
used for the comparisons among groups. The differences of sex
between three groups were examined using the χ2 test.
P<0.05 was considered statistically significant.
Results
Baseline data of patients
Differences in sex, age, disease course, VAS, ODI
and other general data among the three groups were not
statistically significant (all P>0.05). These data were
therefore comparable (Table I).
 | Table IComparison of the general data of
patients with disc herniation among the three groups. |
Table I
Comparison of the general data of
patients with disc herniation among the three groups.
| | Sex/number of
cases | |
|---|
| Group | Number of cases | Age/years | Male | Female | Course/month | VAS score/points | ODI/points |
|---|
| Group I | 42 | 46.9±7.2 | 19 | 23 | 12.3±2.6 | 7.8±1.2 | 52.1±9.0 |
| Group II | 29 | 48.3±6.6 | 13 | 16 | 11.2±3.1 | 7.7±1.3 | 53.0±8.1 |
| Group III | 5 | 47.7±8.2 | 2 | 3 | 13.0±2.9 | 7.9±2.5 | 55.9±9.9 |
| Statistical
tests | | F=0.342 |
χ2=0.050 | | F=1.695 | F=0.073 | F=0.339 |
| P-value | | 0.712 | 0.957 | | 0.191 | 0.929 | 0.714 |
Comparison of VAS and ODI scores
before and after the operation
All 76 patients successfully underwent surgery with
a mean operating time of 86.5±13.5 min and a mean intraoperative
haemorrhage of 23.01±1.45 ml. One patient had cerebrospinal fluid
leakage due to a mild tear of the dura mater during the operation,
which improved after symptomatic treatment. The same operation was
repeated in one patient due to recurrence of disc herniation, after
which the patient's condition improved. The follow-up period was
12-17 (mean 12.4±2.4) months. No complications, including epidural
haematoma, incision infection, lumbar instability and refractory
low back pain, occurred during the follow-up period. Among the 76
patients followed-up, 61 had low back pain and 68 had radiating
pain in the lower limbs before the operation. As shown in Table II, the VAS scores and ODI of the
lower back and lower limbs were significantly improved in both
groups after the operation (P<0.05).
 | Table IIComparison of VAS pain score and ODI
of patients with disc herniation before and after the operation
(mean ± SD, points). |
Table II
Comparison of VAS pain score and ODI
of patients with disc herniation before and after the operation
(mean ± SD, points).
| Parameter | Before OP | 1 week after OP | 1 month after OP | 3 months after
OP | 12 months after
OP | F value | P-value |
|---|
| VAS score of lower
back (n=61) | 7.9±1.1 |
3.6±1.3a |
2.4±0.9a |
1.3±1.0a |
1.5±1.3a | 434.80 | 0.001 |
| VAS score of lower
limbs (n=68) | 7.7±1.2 |
3.7±1.4a |
1.7±1.4a |
1.7±1.1a |
1.8±1.2a | 318.90 | 0.001 |
| ODI (n=76) | 52.3±9.6 |
11.6±7.8a | 10.9±8a |
9.2±7.9a |
10.0±9.0a | 367.30 | 0.001 |
Comparison of intraoperative
conditions and postoperative clinical effects between the three
groups
As shown in Table
III, the differences in the duration of operation, amount of
intraoperative bleeding and the VAS score and ODI of the lower back
and lower limbs at each time point after the operation between
group III and groups I and II were statistically significant
(P<0.05), while those between group I and group II were not
statistically significant (P>0.05). Intraoperative complications
occurred in two patients with high iliac crest in group III. One
had cerebrospinal fluid leakage due to a mild tear of the dura
mater during the operation, which improved after symptomatic
treatment. The same operation was repeated in another patient due
to recurrence of disc herniation, after which the condition of this
patient improved (Fig. 2).
 | Table IIIComparison of the effect of
evaluation indicators in patients with disc herniation before and
after the operation among the three groups (mean ± SD). |
Table III
Comparison of the effect of
evaluation indicators in patients with disc herniation before and
after the operation among the three groups (mean ± SD).
| | VAS/points | ODI/points |
|---|
| Group | No. of cases | Duration of
OP/min | Intraoperative
haemorrhage/ml | 1 week after
OP | 1 month after
OP | 6 months after
OP | 12 months after
OP | 1 week after
OP | 1 month after
OP | 6 months after
OP | 12 months after
OP |
|---|
| Group I | 42 | 85±12 | 23±7 | 2.34±0.42 | 1.83±0.34 | 1.73±0.67 | 1.57±0.45 | 16±8 | 12±8 | 13±8 | 11±6 |
| Group II | 29 | 87±14 | 24±8 | 2.16±0.24 | 1.62±0.21 | 1.65±0.63 | 1.61±0.29 | 18±8 | 13±7 | 11±6 | 11±5 |
| Group III | 5 | 95±16 | 28±7 |
3.41±0.37a,b |
3.23±0.32a,b |
2.75±0.57a,b |
2.17±0.37a,b | 30±8a,b | 27±8a,b | 20±7a,b | 18±7a,b |
| F value | | 1.360 | 1.372 | 25.900 | 63.280 | 6.258 | 5.273 | 7.560 | 8.684 | 3.376 | 4.417 |
| P-value | | 0.293 | 0.309 | 0.000 | 0.000 | 0.003 | 0.007 | 0.002 | 0.000 | 0.040 | 0.016 |
Discussion
Advantages and effects of the TESSYS
technique on the treatment of lumbar disc herniation
In 2002, Hoogland et al (13) proposed the TESSYS technique on the
basis of the Yenug Endoscopic Spine System technique, resulting in
advances in PETD. The TESSYS technique points the puncture target
to the posterior edge of the vertebral body, adding a special ring
saw at the same time to partially excise the bony structure of the
intervertebral foramen, and enters the spinal canal through the
enlarged intervertebral foramen. These steps achieve direct
decompression and spinal canal decompression, broaden the
indications and improve the treatment level of lumbar disc
herniation. At present, this technique can treat almost all types
of lumbar disc herniation (including giant, prolapsed and revision
operation) (16). The technique is
also suitable for treating lumbar spinal stenosis, nerve root canal
stenosis and other diseases (17,18).
Numerous studies have shown that the treatment of
lumbar disc herniation using PETD can achieve the same effect
observed using traditional open operation or microendoscopic
discectomy (19-22).
Furthermore, this technique is a safe and effective minimally
invasive method. The results of this study also showed only small
amounts of intraoperative bleeding, significantly improved VAS pain
scores and ODI of the lower back and the lower limbs at each time
point and low incidence of intraoperative complications, which is
similar to previous studies (21-23).
Patients' iliac crest height and
operative approaches
For patients with L5-S1 disc herniation, the
puncture angle of the intervertebral foramen approach to the
herniated nucleus pulposus is steep, due to the presence of
anatomical factors, such as high iliac crest, large zygopophysis at
S1 and large inclination of the L5-S1 intervertebral space,
resulting in certain difficulties during operation. Choi et
al (9) have suggested that the
highest point of the iliac crest above the L5 pedicle will make the
operation via the intervertebral foramen approach less effective.
Because the L5-S1 interlaminar space is relatively wide, scholars
have also suggested solving disc herniation caused by high iliac
crest via an interlaminar approach (24). Ruetten et al (25) reported that the interlaminar
approach was selected in 94.7% of the patients with L5-S1 disc
herniation and that the operative effects were excellent. However,
other scholars suggest that for L5-S1 intervertebral disc
herniation with upper and lower migration, the intervertebral
foramen or intervertebral lamina approach drilled through the ilium
may be more effective (26,27). The results of the present study
suggest that during the excision of the nucleus pulposus by the
interlaminar approach for the treatment of L5-S1 intervertebral
disc herniation, the effect of local anaesthesia was poor, and the
average VAS pain score was high. Therefore, the majority of
patients continued the operation after optimizing anaesthesia with
general anaesthesia. At present, the operation is usually performed
through an interlaminar approach under general anaesthesia to avoid
failure procedure (28,29), To encourage cooperation of patients
under local anaesthesia, the intervertebral foramen approach was
still adopted for patients with high iliac crest in the current
study.
Influence of patients' iliac crest
height on the operative effect of the TESSYS technique
A high iliac crest is a major obstacle to
percutaneous endoscopic lumbar discectomy at the L5-S1 segment
(4,24). However, a ‘high iliac crest’ itself
is a vague definition without quantitative standards. In the
present study, the height of the iliac crest above the horizontal
line of the lower edge of the L4 pedicle demonstrated a significant
influence on the postoperative effect of TESSYS. The postoperative
ODI and VAS scores of the lower back and lower limbs in group III
were much lower than that those in groups I and II, and the degree
of pain relief and functional recovery of the lower back and lower
limbs after operation in group III was also lower than those in
groups I and II; one patient with recurrence and one with dural
tear were also from the high iliac crest group. Choi and Park
(4) and Choi et al (9) suggest that, in lateral PETD, iliac
crest height has different effects on different types of herniation
in the treatment of L5-S1 intervertebral disc herniation and is
more effective for shoulder and lateral herniations; however, the
present study did not perform group comparison based on types of
herniations. The current study revealed that the operative space
was limited, as a lateral approach would be seriously obstructed by
the L5 transverse process or one sacral transverse process relic in
case of high iliac crest; therefore, it is difficult to adjust the
working casing during the operation.
In practice, the operation can usually be performed
successfully when iliac crest height is below the upper edge
horizontal line of the L5 pedicle in the present study. In
addition, the current study revealed that the operation can be
completed by experienced operators when iliac crest height is
between the lower edge horizontal line of the L4 pedicle and the
upper edge horizontal line of the L5 pedicle. Moreover, alternative
approaches are recommended when iliac crest height is above the
lower edge horizontal line of the L4 pedicle. The operative
position also has a certain effect on the puncture angle. In Choi
et al (9) study patients
were placed in a prone position. However, in the present study,
patients were placed in a lateral position with a cushion under the
lower back to open the intervertebral foramen to a certain extent.
In such a case, the upper edge of the ilium has a certain downward
movement relative to the level of L5-S1, which is conducive for the
removal of the prominent nucleus pulposus, which may be the main
reason for the good effects in group II in this study.
For L5-S1 disc herniation with a high iliac crest,
although the angle of the transforaminal puncture is high,
intervertebral foramen formation and the lateral position of the
patients can broaden the operative field. Therefore, the target is
easily reached and the range of decompression increases (4,30). As
a result, even for patients with high iliac crest, the VAS score
and ODI were significantly improved after the operation, fully
indicating the exact effect of the TESSYS technique. In the present
study, VAS score and ODI of patients showed an increase at 1 year
postoperatively, but there was no significant difference, which may
be due to application of drugs to relieve pain at an early stage,
tiredness after returning to work in the later stage, or it may be
caused by the small sample size. To avoid spinal instability, the
superior articular process was ground as much as was possible to
ensure that the range of resection of the S1 superior articular
process was less when the intervertebral foramen was formed.
Therefore, no spinal instability was observed during the 1-year
follow-up visit.
In the present study, only one patient had
cerebrospinal fluid leakage and one had postoperative recurrence,
which is consistent with the incidence of complications reported in
the literature (24). Both
complications occurred in patients with an iliac crest height above
the lower edge horizontal line of the L4 pedicle. For patients with
high iliac crest, operation should be performed carefully. Measures
such as complete decompression, delaying postoperative off-bed
activities, or expansion of the intervertebral foramen and
selection of the intervertebral lamina approach as appropriate
should be considered to reduce the incidence of complications.
The relationship between the iliac crest and L4 and
L5 pedicles in the lumbar lateral X-ray film was used to grade
iliac crest height, which effectively avoided individual anatomical
differences, such as sex, height and transitional vertebrae. It
objectively reflected the influence of the iliac crest on PETD,
which was convenient for the operator to evaluate the operation
difficulty and had an effective guiding role in the selection of
the surgical approach. However, one limitation of the present study
is that only the iliac wing height, not the wing area, was
considered, as the occlusion of the iliac wing margin from front to
back may also have a great impact on the operation of the L5-S1
segment. In addition, the sample size of group III in this study
was small, which may have biased the results. Therefore, future
studies will require an increased sample size and assess the
influence of the iliac wing on the operation to obtain more
convincing conclusions.
The present data suggest that the TESSYS technique
is effective in treating lumbar disc herniation. Whether the iliac
crest is higher than the lower edge horizontal line of the L4
pedicle is one of the factors influencing the operative
outcome.
Acknowledgements
Not applicable.
Funding
Funding: The present study was funded by the National Natural
Science Foundation of China, (grant no. 82002311).
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
QCS, ZBS and QYL contributed to the conception and
design. YZ, DL, QYL and LHF performed the experiments. YKZ and DPD
contributed to data acquisition and analysis. QCS and YZ wrote the
manuscript. QCS and ZBS confirmed the authenticity of all the raw
data. All authors have read and approved the final manuscript.
Ethics approval and consent to
participate
The study was approved by the Medical and Biological
Ethics Committee of Xi'an Jiaotong University Health Science Center
and all patients provided their written informed consent.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Choi G, Pophale CS, Patel B and Uniyal P:
Endoscopic spine surgery. J Korean Neurosurg Soc. 60:485–497.
2017.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Ahn Y, Lee SH, Park WM, Lee HY, Shin SW
and Kang HY: Percutaneous endoscopic lumbar discectomy for
recurrent disc herniation: Surgical technique, outcome, and
prognostic factors of 43 consecutive cases. Spine (Phila Pa 1976).
29:E326–E332. 2004.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Sairyo K, Egawa H, Matsuura T, Takahashi
M, Higashino K, Sakai T, Suzue N, Hamada D, Goto T, Takata Y, et
al: State of the art: Transforaminal approach for percutaneous
endoscopic lumbar discectomy under local anesthesia. J Med Invest.
61:217–225. 2014.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Choi KC and Park CK: Percutaneous
endoscopic lumbar discectomy for L5-S1 disc herniation:
Consideration of the relation between the iliac crest and L5-S1
disc. Pain Phys. 19:E301–E308. 2016.PubMed/NCBI
|
|
5
|
Lee SH, Choi KC, Baek OK, Kim HJ and Yoo
SH: Percutaneous endoscopic intra-annular subligamentous herniotomy
for large central disc herniation: A technical case report. Spine
(Phila Pa 1976). 39:E473–E479. 2014.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Ahn Y, Kim CH, Lee JH, Lee SH and Kim JS:
Radiation exposure to the surgeon during percutaneous endoscopic
lumbar discectomy: A prospective study. Spine (Phila Pa 1976).
38:617–625. 2013.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Ahn Y: Transforaminal percutaneous
endoscopic lumbar discectomy: Technical tips to prevent
complications. Expert Rev Med Devices. 9:361–366. 2012.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Nie H, Zeng J, Song Y, Chen G, Wang X, Li
Z, Jiang H and Kong Q: Percutaneous endoscopic lumbar discectomy
for L5-S1 disc herniation via an interlaminar approach versus a
transforaminal approach: A prospective randomized controlled study
with 2-year follow up. Spine (Phila Pa 1976). 41 (Suppl
19):B30–B37. 2016.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Choi KC, Kim JS, Ryu KS, Kang BU, Ahn Y
and Lee SH: Percutaneous endoscopic lumbar discectomy for L5-S1
disc herniation: Transforaminal versus interlaminar approach. Pain
Phys. 16:547–556. 2013.PubMed/NCBI
|
|
10
|
Choi G, Kim JS, Lokhande P and Lee SH:
Percutaneous endoscopic lumbar discectomy by transiliac approach: A
case report. Spine (Phila Pa 1976). 34:E443–E446. 2009.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Eun SS, Lee SH, Liu WC and Erken HY: A
novel preoperative trajectory evaluation method for L5-S1
transforaminal percutaneous endoscopic lumbar discectomy. Spine.
18:1286–1291. 2018.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Tezuka F, Sakai T, Abe M, Yamashita K,
Takata Y, Higashino K, Chikawa T, Nagamachi A and Sairyo K:
Anatomical considerations of the iliac crest on percutaneous
endoscopic discectomy using a transforaminal approach. Spine J.
17:1875–1880. 2017.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Hoogland T, Schubert M, Miklitz B and
Ramirez A: Transforaminal posterolateral endoscopic discectomy with
or without the combination of a low-dose chymopapain: A prospective
randomized study in 280 consecutive cases. Spine. (Phila Pa 1976)
31:E890–E897. 2006.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Fairbank JC and Pynsent PB: The oswestry
disability index. Spine. 25:2940–2952. 2000.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Myles PS: The pain visual analog scale:
Linear or nonlinear? Anesthesiology. 100:744–745. 2004.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Kim HS, Paudel B, Jang JS, Lee K, Oh SH
and Jang IT: Percutaneous endoscopic lumbar discectomy for all
types of lumbar disc herniations (LDH) including severely difficult
and extremely difficult LDH cases. Pain Phys. 21:E401–E408.
2018.PubMed/NCBI
|
|
17
|
Wen B, Zhang X, Zhang L, Huang P and Zheng
G: Percutaneous endoscopic transforaminal lumbar spinal canal
decompression for lumbar spinal stenosis. Medicine (Baltimore).
95(e5186)2016.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Ahn Y, Lee SH, Park WM and Lee HY:
Posterolateral percutaneous endoscopic lumbar foraminotomy for
L5-S1 foraminal or lateral exit zone stenosis. Technical note. J
Neurosurg. 99 (Suppl 3):S320–S323. 2003.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Choi KC, Kim JS and Park CK: Percutaneous
endoscopic lumbar discectomy as an alternative to open lumbar
microdiscectomy for large lumbar disc herniation. Pain Phys.
19:E291–E300. 2016.PubMed/NCBI
|
|
20
|
Liu X, Yuan S, Tian Y, Wang L, Gong L,
Zheng Y and Li J: Comparison of percutaneous endoscopic
transforaminal discectomy, microendoscopic discectomy, and
microdiscectomy for symptomatic lumbar disc herniation: Minimum
2-year follow-up results. J Neurosurg Spine. 28:317–325.
2018.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Ahn SS, Kim SH, Kim DW and Lee BH:
Comparison of outcomes of percutaneous endoscopic lumbar discectomy
and open lumbar microdiscectomy for young adults: A retrospective
matched cohort study. World Neurosurg. 86:250–258. 2016.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Shi R, Wang F, Hong X, Wang YT, Bao JP,
Liu L, Wang XH, Xie ZY and Wu XT: Comparison of percutaneous
endoscopic lumbar discectomy versus microendoscopic discectomy for
the treatment of lumbar disc herniation: A meta-analysis. Int
Orthop. 43:923–937. 2019.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Ahn Y: Endoscopic spine discectomy:
Indications and outcomes. Int Orthop. 43:909–916. 2019.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Chen J, Jing X, Li C, Jiang Y, Cheng S and
Ma J: Percutaneous endoscopic lumbar discectomy for L5S1 lumbar
disc herniation using a transforaminal approach versus an
interlaminar approach: A systematic review and meta-analysis. World
Neurosurg. 116:412–420.e2. 2018.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Ruetten S, Komp M, Merk H and Godolias G:
Surgical treatment for lumbar lateral recess stenosis with the
full-endoscopic interlaminar approach versus conventional
microsurgical technique: A prospective, randomized, controlled
study. J Neurosurg Spine. 10:476–485. 2009.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Patgaonkar P, Datar G, Agrawal U,
Palanikumar C, Agrawal A, Goyal V and Patel V: Suprailiac versus
transiliac approach in transforaminal endoscopic discectomy at
L5-S1: A new surgical classification of L5-iliac crest relationship
and guidelines for approach. J Spine Surg. 6 (Suppl 1):S145–S154.
2020.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Osman SG, Sherlekar S, Malik A, Winters C,
Grewal PK, Narayanan M and Gemechu N: Endoscopic trans-iliac
approach to L5-S1 disc and foramen-a report on clinical experience.
Int J Spine Surg. 8:20–31. 2014.PubMed/NCBI View
Article : Google Scholar
|
|
28
|
Hua W, Tu J, Li S, Wu X, Zhang Y, Gao Y,
Zeng X, Yang S and Yang C: Full-endoscopic discectomy via the
interlaminar approach for disc herniation at L4-L5 and L5-S1: An
observational study. Medicine (Baltimore). 97(e0585)2018.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Wang D, Xie W, Cao W, He S, Fan G and
Zhang H: A cost-utility analysis of percutaneous endoscopic lumbar
discectomy for L5-S1 lumbar disc herniation: Transforaminal versus
interlaminar. Spine (Phila Pa 1976). 44:563–570. 2019.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Choi KC, Kim JS, Lee DC and Park CK:
Percutaneous endoscopic lumbar discectomy: Minimally invasive
technique for multiple episodes of lumbar disc herniation. BMC
Musculoskelet Disord. 18(329)2017.PubMed/NCBI View Article : Google Scholar
|