Introduction
Also known as paraduodenal pancreatitis,
paraduodenal wall cyst, myoadenomatosis or cystic dystrophy, groove
pancreatitis represents a distinct form of inflammation of the
pancreatic groove and was first described by Becker in 1973
(1,2). The groove area refers to the narrow
space located between the pancreatic head medially, the duodenum II
laterally, the duodenum III and inferior vena cava posteriorly and
the duodenum I superiorly (3).
According to the study by Becker and Mischke (2), groove pancreatitis can present as
pure-type or as segmental-type. One of the most significant issues
which should be taken into consideration in cases in which groove
pancreatitis is suspected is related to the differential diagnosis
with groove pancreatic carcinoma (4-7).
Due to the extremely low number of such cases, the pre-operative
diagnosis is difficult to establish. In this respect, the majority
of cases are subjected to surgery with a pre-operative suspicion of
malignant disease, with the final diagnosis being established upon
a histopathological examination. Therefore, in such cases,
pancreatoduodenectomy has become the treatment of choice (4,5).
Case report
The present study describes the case of a
46-year-old male, with a previous history of alcoholic
pancreatitis, who was submitted to surgery for pre-operative
diagnosis of pancreatic cancer. The data of the patient were
retrospectively reviewed after obtaining the approval of the Ethics
Committee of ‘Fundeni’ Clinical Institute (approval no. 267/2020).
Patient consent for publication was obtained and signed by the
patient on March 19, 2020.
The 46-year-old patient with a known history of
heavy alcoholic intake and several episodes of acute pancreatitis
was self-referred to the ‘Fundeni’ Clinical Institute (Bucharest,
Romania) for weight loss, abdominal pain, nausea, vomiting and a
weight loss of 12 kg in the last 3 months. A computed tomography
scan revealed the presence of a hypodense mass at the level of the
pancreatic head, measuring 4/5/3 cm apparently with no vascular
invasion (Figs. 1 and 2).
The patient was further subjected to an endoscopic
ultrasound and biopsy examination, which revealed the presence of
chronic inflammation, as well as the absence of malignant cells.
However, the biological test results revealed an increase in the
levels of serum markers when compared to the determination which
had been performed 6 months prior; at this time, the serum level of
CA 19-9 was 78 U/ml, whereas 6 months prior, these levels were 33
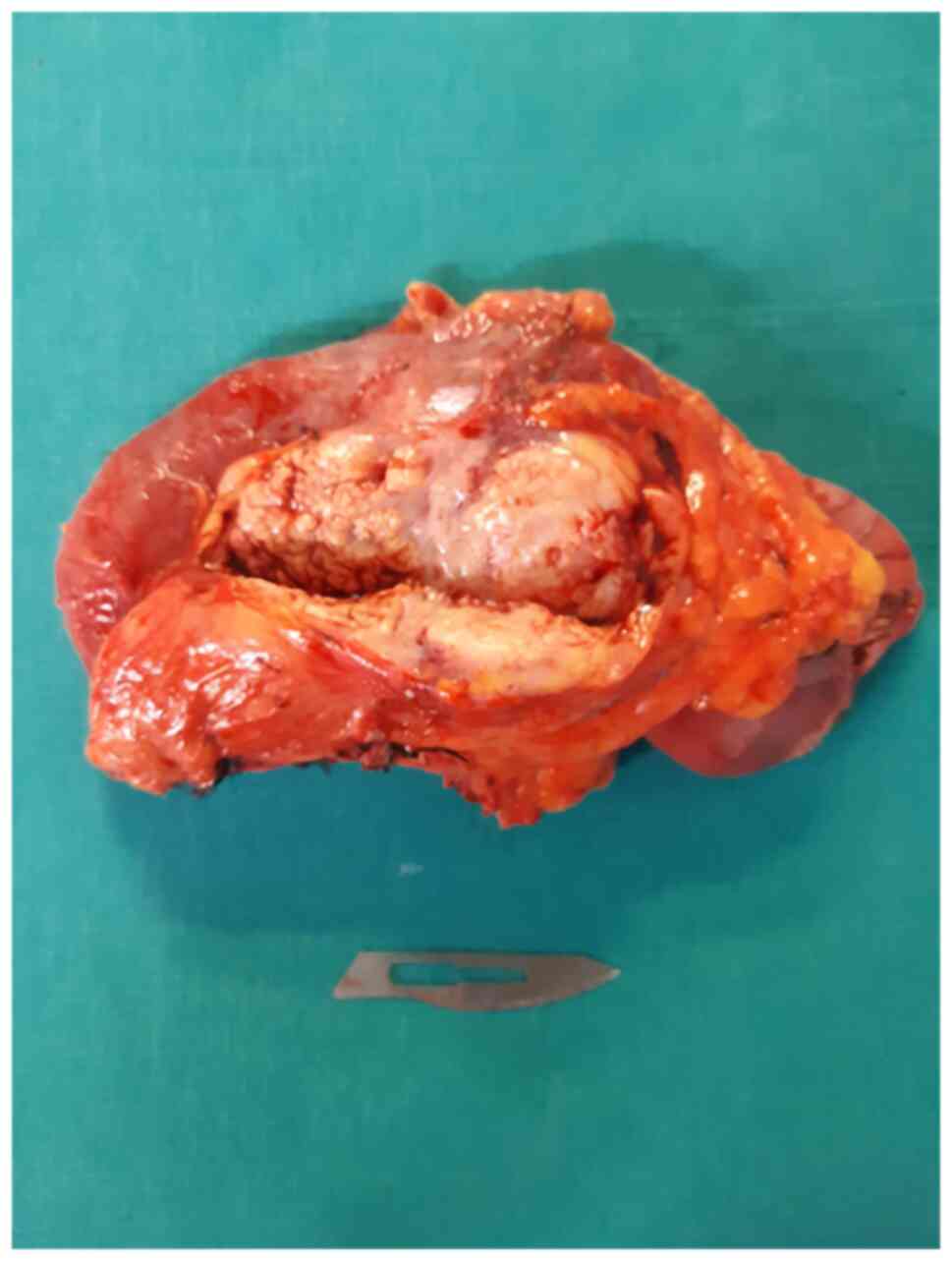
U/ml. Thus, the patient was submitted to surgery for a
pancreatoduodenectomy (Figs. 3 and
4).
The post-operative outcome was uneventful, with the
patient being discharged on day 10 post-operatively. However, the
histopathological examination confirmed the absence of malignant
cells in the specimen, and the finally diagnosis of groove
pancreatitis was made. At the 3-month follow-up period, the patient
reported a significant improvement in his clinical status, with the
alleviation of abdominal pain, as well as a weight gain of 4.5
kg.
Discussion
Initially described by Becker in 1973(1), groove pancreatitis was classified by
Stolte et al (7) as having
two forms: A pure one, which is characterized by the presence of
inflammatory and fibrous lesions affecting exclusively the virtual
space between the pancreatic head and the duodenum, and a segmental
form affecting the pancreatic head medially. In the latter
situation, the surrounding structures, such as the common biliary
duct, duct of Wirsung or duodenum are progressively involved,
leading to the development of jaundice, abdominal pain, weight loss
or post-prandial vomiting (8,9).
Mainly associated with chronic alcohol abuse, groove pancreatitis
has been also described in patients with duodenal peptic ulcers or
congenitally in children (3).
As regards the types of therapeutic strategies,
patients diagnosed with groove pancreatitis can be initially
subjected to medical therapies in order to provide an effective
analgesic effect and to provide an adequate substitution of
pancreatic function (10,11). In cases in which the symptoms are
solely produced by pancreatic duct obstruction, endoscopic
procedures in order to provide an effective drainage of the
pancreatic secretion via endoscopy may be taken in consideration
(12). However, this method may not
be applicable in cases presenting with severe duodenal stenosis or
in which the pre-operative investigations could not exclude the
association of malignant transformation (3). In cases in which conservative
treatment fails and symptoms recur, surgery should be taken in
consideration; in this respect, various procedures have been
proposed, ranging from duodenal and biliary bypass, duodenum
preserving pancreatic head resection or pancreatoduodenectomy
(13,14); however, conservative procedures,
such as bypass or segmental resections have been more commonly
proposed in pediatric patients, cases in which the diagnosis of
malignancy is not probable (3).
Moreover, the necessity of resecting large malignant tumors alone
or in association with vascular resections have led to the
widespread use of pancreatoduodenectomy as the primary therapeutic
option for patients with groove pancreatitis (15-18).
One of the first studies which demonstrated the
difficulties in differentiating groove pancreatic cancer from
groove pancreatitis was conducted by Yamaguchi and Tanaka (19) and was published in 1992. The study
included 8 patients from six institutions; in all the patients, a
pre-operative diagnosis could not be established. The main features
which made the diagnosis of malignant disease a very probable one
were represented by the presence of extensive duodenal stenosis,
common bile duct stenosis or vascular encasement. In all cases, a
pancreatoduodenectomy was performed and the histopathological
analyses demonstrated the absence of malignant disease (19).
One of the largest single institutional studies
conducted on groove pancreatitis was published in 2007 by Rahman
et al (20); the study
included 11 patients investigated for abdominal pain, gastric
outlet obstruction or jaundice. In all cases, pancreatoduodenectomy
was performed, with the analysis of the specimens demonstrating the
absence of malignant transformation; moreover, following a median
follow-up period of 52 weeks, all patients reported weight gain,
with a mean value of 3 kg at 2 months of follow-up, as well as a
significant alleviation of pain, demonstrating in this manner, the
effectiveness of resection in such cases (19). The benefit in terms of the
alleviation of abdominal pain was explained by the interruption of
the local fibrotic and inflammatory networks (20,21).
The widespread demonstration of the benefits of
pancreatoduodenectomy in the field of groove pancreatitis has led
to the inclusion of this procedure as standard of care in the
latest guidelines. Therefore, in the United European
Gastroenterology evidence-based guidelines for the diagnostic and
therapy of chronic pancreatitis, published in 2017, the interviewed
experts declared that in groove pancreatitis, pancreatoduodenectomy
represents the most suitable surgical option (the statement being
considered as strongly agreeable) (21).
In conclusion, groove pancreatitis represents a rare
entity, with only isolated cases being reported thus far; moreover,
the differential diagnosis with pancreatic groove cancer is usually
difficult to establish pre-operatively. Therefore, in the majority
of cases, the treatment of choice remains pancreatoduodenectomy,
with the final diagnosis being established at the time of the
histopathological examination. Furthermore, performing a wide
resection of the lesion seems to have an overall positive influence
on the quality of life of patients, with a significant alleviation
of pain, as well as weight gain being reported in the ensuing
months.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
NB contributed to the conception of the study,
collected, analyzed and interpreted data from the literature and
the data corresponding to the patient, and critically revised the
manuscript. IB contributed to the conception of the study,
performed the literature research and drafted the manuscript. SD
contributed to the conception of the study, performed the
literature research and drafted the manuscript. IP collected,
analyzed and interpreted the data corresponding to the patient and
critically revised the manuscript. IB and SD confirm the
authenticity of all the raw data. All authors have read and
approved the final manuscript.
Ethics approval and consent to
participate
The Ethics Committee of ‘Fundeni’ Clinical Institute
approved the study.
Patient consent for publication
Patient consent for publication was obtained and
signed by the patient on March 19, 2020.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Becker V: Bauchspeicheldrüse. In:
Spezielle pathologische Anatomie. Doerr W, Seifert G and Uhlinger E
(eds). Vol 4. Springer, Berlin, 1973 (In German).
|
|
2
|
Becker V and Mischke U: Groove
pancreatitis. Int J Pancreatol. 10:173–182. 1991.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Tahara K, Kanamor Y, Miyake K, Kudo Y,
Fujita T, Kutsukake M, Mori T, Yamada Y, Fujino A, Shimizu H, et
al: Groove pancreatitis treated by duodenal and biliary bypass. J
Pediatr Surg Case Rep. 59(101540)2020.
|
|
4
|
Yabuki K, Maekawa T, Satoh K, Tamasaki Y,
Maekawa H, Amano T, Ogawa K and Anouma K: A case of groove
pancreatitis with duodenal stenosis. Dig Endosc. 12:345–349.
2000.
|
|
5
|
Munthali Lovemore CE, Hsu JT, Chiu CT,
Chen HM and Chen MF: Groove pancreatitis: Case report and
literature review. Chang Gung Med J. 24:512–516. 2001.PubMed/NCBI
|
|
6
|
Dey R and Mannion R: Groove pancreatitis-A
case report and review of imaging features. Eur J Radiol Extra.
64:67–69. 2007.PubMed/NCBI
|
|
7
|
Stolte M, Weiss W, Volkholz H and Rosch W:
A special form of segmental pancreatitis: ‘Groove Pancreatitis’.
Hepatogastroenterology. 29:198–208. 1982.PubMed/NCBI
|
|
8
|
Manzelli A, Petrou A, Lazzaro A, Brennan
N, Soonawalla Z and Friend P: Groove pancreatitis. A mini-series
report and review of the literature. JOP. 12:230–233.
2011.PubMed/NCBI
|
|
9
|
Frutos-Perez JM, Perea-Ribis M,
Martinez-Pascual MA, Llopis-Sanchis M and Tornero-Estebanez C:
Constitutional syndrome, ascites and duodenal thickening presenting
as groove pancreatitis. Eur J Case Rep Intern Med.
5(000789)2018.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Aguilera F, Tsamalaidze L, Raimondo M,
Puri R, Asbun HJ and Stauffer JA: Pancreaticoduodenectomy and
outcomes for groove pancreatitis. Dig Surg. 35:475–481.
2018.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Balduzzi A, Marchegiani G, Andrianello S,
Romeo F, Amodio A, De Pretis N, Zamboni G, Malleo G, Frulloni L,
Salvia R and Bassi C: Pancreaticoduodenectomy for paraduodenal
pancreatitis is associated with a higher incidence of diabetes but
a similar quality of life and pain control when compared to medical
treatment. Pancreatology. 20:193–198. 2020.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Chantarojanasiri T, Isayama H, Nakai Y,
Matsubara S, Yamamoto N, Takahara N, Mizuno S, Hamada T, Kogure H
and Koike K: Groove pancreatitis: Endoscopic treatment via the
minor papilla and duct of santorini morphology. Gut Liver.
12:208–213. 2018.PubMed/NCBI View
Article : Google Scholar
|
|
13
|
Zhu C, Huang Q, Zhu J, Zhang X and Qin X:
Groove resection of pancreatic head in groove pancreatitis: A case
report. Exp Ther Med. 14:1983–1988. 2017.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Tezuka K, Makino T, Hirai I and Kimura W:
Groove pancreatitis. Dig Surg. 27:149–152. 2010.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Brasoveanu V, Anghel C, Barbu I, Pautov M,
Ionescu MI, Motthor M, Balescu I, Dima S and Bacalbasa N:
Pancreatoduodenectomy en bloc with portal and superior mesenteric
artery resection-a case report and literature review. Anticancer
Res. 35:1613–1618. 2015.PubMed/NCBI
|
|
16
|
Bacalbasa N, Balescu I, Dima S, Brasoveanu
V and Popescu I: Pancreatic resection as part of cytoreductive
surgery in advanced-stage and recurrent epithelial ovarian cancer-A
single-center experience. Anticancer Res. 35:4125–4129.
2015.PubMed/NCBI
|
|
17
|
Brasoveanu V, Dumitrascu T, Bacalbasa N
and Zamfir R: Splenic artery used for replaced common hepatic
artery reconstruction during pancreatoduodenectomy-a case report.
Chirurgia (Bucur). 104:499–504. 2009.PubMed/NCBI
|
|
18
|
Bacalbasa N, Balescu I, Tanase A, Pautov
M, Brezean I, Vilcu M and Brasoveanu V: Spleno-Pancreatectomy en
bloc with parcelar gastrectomy for splenic artery aneurysm-a case
report and literature review. In Vivo. 32:915–919. 2018.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Yamaguchi K and Tanaka M: Groove
pancreatitis masquerading as pancreatic carcinoma. Am J Surg.
163:312–316. 1992.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Rahman SH, Verbeke CS, Gomez D, McMahon MJ
and Menon KV: Pancreatico-duodenectomy for complicated groove
pancreatitis. HPB (Oxford). 9:229–234. 2007.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Löhr JM, Dominguez-Munoz E, Rosendahl J,
Besselink M, Mayerle J, Lerch MM, Haas S, Akisik F, Kartalis N,
Iglesias-Garcia J, et al: United European gastroenterology
evidence-based guidelines for the diagnosis and therapy of chronic
pancreatitis (HaPanEU). United European Gastroenterol J. 5:153–199.
2017.PubMed/NCBI View Article : Google Scholar
|