Introduction
Narrow-band imaging (NBI), an on-demand, real-time,
endoscopic imaging technique, was developed to enhance the
visualization of the mucosal vascular network and surface texture
for the purpose of improving tissue differentiation,
characterization and diagnosis (1).
The interaction of particular tissue structures with
light is wavelength-dependent and augmentation of particular
mucosal features via NBI is achieved through observation of light
transmission at selected wavelengths (or colors) (2).
In the NBI system, selective light transmittance is
conducted via optical filtering of white light (WL). Specifically,
NBI uses two discrete bands of light, a blue band at 415 nm and a
green band at 540 mm, to create a high-contrast image of the tissue
surface, which allows enhanced visualization of blood vessels
(3). The two bands correspond to
the peak light absorption of hemoglobin, thus permitting NBI to
visualize the blood vessels with greater clarity and accuracy on
the surface of the analyzed tissues than observation with WL
(3).
In clinical practice, there is currently widespread
use of NBI to provide an improved examination of the
gastrointestinal system, including the stomach and large intestine,
esophagus and pharynx, as well as of the lungs, urinary tract and
oropharynx. This technique, which has been termed ‘optical biopsy’,
has brought achievements of earlier diagnosis by substantially
improving the qualitative diagnosis of the depth and grade of
invasion of atypical lesions (4).
The aim of the present study was to perform a
systematic review of all available studies evaluating the use of
NBI in gynecology clinical practice for the detection of benign and
malignant lesions.
Materials and methods
Search strategy
The following electronic databases were searched:
PubMed (1950-2021), Google Scholar (2004-2021) and Cochrane Library
(2010-2021). The electronic literature search was mostly performed
between January 2020 to February 2021. The search included the
following medical subject headings or keywords: ‘Narrow-band
imaging’ and ‘gynecology’. The last search was performed on
08/02/2021.
The systematic review was performed and the
flowchart diagram was drawn according to the Preferred Reporting
Items for Systematic Reviews and Metanalyses statement (5).
Inclusion criteria
Full-text articles published in peer-reviewed
journals and written in the English language were deemed eligible
to be included in the review. Studies that did not fulfill the
following criteria were excluded from the review: i) Conference
abstracts and studies not providing sufficient clinical data; and
ii) studies reporting narrow-band imaging utilization in animals,
in surgical specimens or in an in vitro environment.
All types of studies were included, namely
randomized controlled or observational studies, case series and
case reports. The selected eligible articles were compared and
discrepancies were resolved by discussion. The final decision on
eligibility was made by the senior investigator (PP) whenever
discrepancies had not been resolved through discussion.
Data extraction
Two authors (PP and KK) independently extracted
information, while SS, CK, VA, PT and NA checked the extracted
information and tabulated the data. NV checked the results and
approved the study.
From the eligible studies, the following clinical
data were obtained: Author and year of publication; the time period
of enrolment of the study population; the country and city in which
the study was performed; the type of study; the setting of the
hospital (single- or multi-university study); the number of
patients; the age of the patients; the inclusion criteria for
surgery; the interventions performed; the endoscopic system used in
each study; the outcome of the studies; and comments on different
studies. The references of the selected studies were scrutinized
for additional information not obtained by the initial search.
The Quality Assessment of Diagnostic Accuracy
Studies 2 (QUADAS-2) tool was used to assess the quality of the
primary diagnostic accuracy studies. Via this tool, risks for bias
may be evaluated in the following four key domains: i) Selection of
participants; ii) index (diagnostic) test; iii) reference standard;
and iv) flow and timing of the study (6).
Through the use of the Case Report (CARE) guidelines
checklist, the information quality of case reports was evaluated,
specifically assessing the following items: Patient information,
the presence of timeline information, diagnostic assessment,
clinical findings, therapeutic intervention and outcomes (7,8).
Statistical analysis
Data obtained from the selected studies were entered
into an Excel v160 spreadsheet (Microsoft Corporation 2018).
Descriptive statistical analyses was performed using SPSS version
23 (IBM Corporation) and Excel version 16.0 (Microsoft Corporation,
2018). The number of publications were calculated per year and per
country, and the median age of participants in the selected studies
was also calculated.
Results
Literature search and selection
The literature search identified a total of 3,836
studies, i.e., 3,800 articles through Google Scholar, 32 articles
through the PubMed database and four through the Cochrane Library
database. The flowchart of the study selection process is displayed
in Fig. 1. After removing
duplicates and irrelevant articles, 256 articles were considered
for further evaluation. Further assessment excluded 215 articles
for various reasons (non-eligible, non-English literature, animal
studies and articles providing insufficient information). Finally,
31 studies reporting on a total of 3,128 female patients were
included in the review.
Of the selected studies, 10 (32%) were case reports
(9-18),
19 (61.2%) were prospective studies (11,12,18-32)
and two studies (6.4%) were randomized controlled trials (33,34).
The selected studies had publication dates ranging from 2007 to
2020.
The frequency of publications per year and the
percentage of publications by country are presented in Fig. 2. The years with the highest
frequency of publications were 2010 and 2011 with 5 studies
produced each year and the country which produced the highest
number of studies was Japan with 11 studies (13,18,21,22,28,31-33,35),
followed by Italy with 8 studies (9,10,15-17,19,20,36).
Study properties
A total of 11 studies described the use of NBI in
hysteroscopy for the detection of endometrial pathologies (9,10,19-25,36,37)
and another 11 studies reported the use of NBI in laparoscopy for
the detection of peritoneal endometriosis (11-13,26-30,33,34,37,38).
Furthermore, three articles dealt with the use of NBI in digital
colposcopy for the detection of lower genital tract pathologies
(14,31,32)
and three articles reported on the use of NBI in laparoscopy for
the detection of peritoneal metastases associated with ovarian
cancer and other gynecological malignancies (15-17).
NBI in endometrial pathology
Details on the selected studies reporting the use of
NBI in hysteroscopy are presented in Table I. A total of 11 studies were
included in the review, dating from 2009-2020 with a combined
cohort of 2,424 female patients (9,10,19-25,36,37).
Of these, eight studies were prospective studies (Canadian Task
Force classification, II-2) (19,23,36)
and two studies were case reports (9,10). All
studies were designed in university settings, two studies were
performed in multicentric university settings (20,36)
and two studies were reported at international congresses as
conference reports (10,24). All of the patients presented with
abnormal uterine bleeding (AUB). The median age of the patients was
45.5±10.5 years. A total of four studies were performed in
outpatient office settings using a vaginoscopic approach without
any general anesthesia (19,21,23,36).
Conventional hysteroscopy under general anesthesia was performed in
seven studies (10,24,25).
Operative hysteroscopy was performed in all cases and histology
specimens were obtained in each case. Olympus Exera II (Olympus
Corporation) was the main video system used in the majority of
studies.
 | Table IComparison of studies reporting on
the use of hysteroscopy with NBI. |
Table I
Comparison of studies reporting on
the use of hysteroscopy with NBI.
| Author (year) | Time period | Country, city | Type of study | Institutes | Number of
subjects | Age, years | Inclusion
criteria | Interventions | System | Outcomes | Conclusion | (Refs.) |
|---|
| Surico, et
al (2009) | 2009 | Italy, Novara | Case report | Single univ. | 1 | NS | AUB | Conventional
hysteroscopy 30˚ 4 mm WL&NBI in G2 endometrial CA | Olympus Exera
II | Detection of
atypical irregular microvessels | NBI was able to
increase accuracy in hysteroscopic detection of hyperplasia and
endometrial CA | (9) |
| Cicinelli, et
al (2010) | 2008-2009 | Italy, Bari | Prospective
controlled | Single univ. | 395 | 42.6±10.7 | AUB | Fluid
minihysteroscopy 105˚ 2.7 mm WL & NBI office setting without
anesthesia compared with histology | Olympus Exera
II | Increased
sensitivity of NBI vs. WL: Proliferating endometrium, 0.93 vs.
0.78, P<0.005; chronic endometritis, 0.88 vs. 0.70, P<0.005;
LRH, 0.88 vs. 0.70, P<0.05; HRH, 0.60 vs. 0.40, P<0.05 | NBI increased
sensitivity, decreased false negative biopsies and increased
sensitivity in detecting endometrial pathology | (19) |
| Surico, et
al (2010) | 2007-2008 | Italy, Novara | Prospective
controlled | Multi univ. | 209 | 59±11 | AUB PMB | Hysteroscopy 5 mm
WL&NBI with a 1.5 mm operating channel under general anesthesia
compared with histology | Olympus Exera
II | Increased
sensitivity of NBI vs. WL in endometrial CA detection 94.7 vs.
84.4% hyperplasia detection 78.38 vs. 64.86% slight decrease in
specificity (P>0.05) | NBI use by an
experienced surgeon may increase diagnostic accuracy | (20) |
| Kisu, et al
(2011) | 2009-2010 | Japan, Tokyo | Prospective
controlled | Single univ. | 104 | NS | AUB | Flexible
hysterofiberscope 3.1 mm WL&NBI office setting without
anesthesia compared with histology | Olympus Xenon
Light | Increased
sensitivity of NBI vs. WL for atypical endometrial hyperplasia 97.2
vs. 82.6% P<0.005 | NBI may be a useful
tool in the detection of malignant endometrial lesions | (21) |
| Kuroda, et
al (2011) | 2009 | Japan, Tokyo | Prospective
controlled | Single univ. | 14 | 40-42 | AUB | Rigid 3.8 mm
hysteroscopy Flexible 4 mm hysteroscopy with WL and NBI under GA in
6 cases with submucous myoma and 8 cases with normal
endometrium | Olympus Xenon
Light | Flexible scope in
WL showed greater vascular densities than with rigid scope NBI with
rigid and flexible scope did not show statistically significantly
increased vascular densities | NBI may be a useful
technology in the detection of malignant cells exhibiting
neoangiogenesis. NBI has superior ability in observing the
endometrial cavity because no high fluid pressure is required | (22) |
| Kisu, et al
(2011) | 2009-2010 | Japan, Tokyo | Prospective | Single univ. | 71 | 41.9±12.5 | AUB | Flexible
hysterofiberoscope 3.1 mm WL&NBI in office setting without
anesthesia compared with histology findings | Olympus Xenon
Light | Higher sensitivity
for hyperplasia and CA of endometrium for all raters with NBI.
Average sensitivity was significantly higher in NBI group compared
to WL (78.6 vs. 63.7%, P<0.001) | NBI system allows
better view of the mucosal blood vessels than WL. Larger studies
with randomization design required to establish conclusions | (23) |
| Tinelli, et
al (2011) | 2008-2010 | Italy, Bari | Prospective | Multi univ. | 801 | 41.9±9.8 | AUB | Fluid
minihysteroscopy 2.7 mm WL & NBI in office setting without
anesthesia compared with histology | Olympus Exera
II | NBI increased
sensitivity for endometrial CA to 93 vs. 81%, P<0.05; for LRH to
82 vs. 56%, P<0.05; and for HRH to 60 vs. 20%, P<0.005. No
alterations in specificity and NPV | NBI increased
sensitivity in detecting LRH, HRH and endometrial CA. A useful tool
for reducing missed pathologies and unnecessary biopsies. NBI
increased recognition of preneoplastic and neoplastic lesions
misdiagnosed as benign by WL hysteroscopy | (26) |
| Raimondo, et
al (2012) | 2012 | Italy, Rome | Case report | Single univer. | 1 | 54 | AUB | NBI-hysteroscopy
under GA anesthesia 30-degree 4-mm biopsy of endometrial
lesions | Olympus Exera
II | Exhibition of
vascular network consistent with adenomyosis. Histology confirmed
adenomyosis | NBI in hysteroscopy
may be a useful tool in the detection of adenomyosis | (10) |
| Kong, et al
(2015) | 2011-2013 | China, Beijing | Prospective | Single univ. | 213 | 43 | AUB | Conventional
hysteroscopy 5 mm WL&NBI under general anesthesia compared with
histology | NS | NBI increased
sensitivity for endometrial CA to 98.1 vs. 73.6% P<0.001; for
LRH to 79.6 vs. 49%, P=0.003; and for HRH to 93.5 vs. 82.6%,
P=0.006 | NBI increased
sensitivity in detecting LRH, HRH and endometrial CA | (24) |
| Ozturk, et
al (2016) | 2010-2011 | Turkey, Ankara | Prospective | Single univ. | 86 | 40 | AUB n=71 PMB
n=15 | Hysteroscopy 5 mm
WL&NBI with a 1.5 mm operating channel under general anesthesia
compared with histology | Olympus Exera
II | Detection of 7
cases of endometritis with NBI and of 1 case of endometritis with
WL (7/8, 87%, 95%CI 0.52-0.97) | NBI may be useful
combined with WL in detecting conditions such as chronic
endometritis | (25) |
| Wang, et al
(2020) | 2012-2014 | China, Beijing | Prospective | Single univ. | 529 | 40.3 | No symptoms | Hysteroscopy 5 mm
WL&NBI with a 1.5 mm operating channel under general anesthesia
compared with histology | Olympus Exera
II | Three levels of
trainees achieved higher diagnostic accuracy with NBI utilization
than with WL during hysteroscopy | NBI may increase
the skill of trainees, particularly those with previous
training | (37) |
NBI hysteroscopy demonstrated increased sensitivity
compared with WL imaging hysteroscopy for the detection of
endometrial cancer in four studies (20,23,24).
The sensitivity of NBI and WL hysteroscopy for
endometrial cancer reported by individual studies was 78.6 vs.
63.7%, P<0.001(23), 93 vs. 81%,
P<0.05(36), 94.7 vs. 84.4%,
P<0.05(20) and 98.1 vs. 73.6%
P<0.001(24). Increased
sensitivity of NBI vs. WL for the detection of atypical endometrial
hyperplasia - high-risk hyperplasia (HRH) was reported in five
studies (10,20-23).
The reported sensitivity of NBI vs. WL for HRH was 60 vs. 20%,
P<0.005(36), 78.38 vs. 64.86%,
P<0.005(20), 78.6 vs. 63.7%,
P<0.001(23), 93.5 vs. 82.6%,
P=0.006(24) and 97.2 vs. 82.6%,
P<0.005(21).
None of the 11 studies reported any adverse effects
or complications related to the surgical techniques in all
instances.
NBI in endometriosis
Details on the selected studies reporting on the use
of NBI in laparoscopy for the detection of peritoneal endometriosis
are provided in Table II. A total
of 11 studies were included in the present review, dating from 2007
to 2019 with a population of 626 female patients in total (11-13,26-30,33,34,38).
The mean age was 35.5±3.6 years. A total of three studies were case
reports (11,12,29),
three were studies with a randomized design (13,34,38)
and five were had a prospective design lacking randomization
(26-29,33).
In all studies, laparoscopy with a 0-degree 10-mm scope was
performed, except for two studies where intestinal endoscopy was
utilized (13), while one study
reported on the use of a 0-degree 12-mm scope (30). NBI improved the detection rate by
53% for smaller endometriotic lesions previously not detected on WL
imaging laparoscopy (26). Another
study reported that 82.7% of endometriotic lesions were detected
using NBI compared with 55.9% of lesions detected by WL imaging
(27). The detection rate of
endometriotic lesions with NBI was 100% in a randomized controlled
trial with 167 female patients (34). Another randomized controlled trial
assessed quality of life in two study groups: One group underwent
laparoscopy with WL and the other with NBI. No difference in pain
and quality of life was observed between the two study groups
(34). When combined with WL, NBI
was reported to provide an additional predictive value of 86% for
the detection of endometriotic lesions, if a positive diagnosis was
made under WL imaging alone (29).
NBI and WL combined with 3D imaging was able to increase the
sensitivity rate up to 91% (13).
 | Table IIComparison of studies reporting on
the use of NBI in patients with endometriosis. |
Table II
Comparison of studies reporting on
the use of NBI in patients with endometriosis.
| Author (year) | Time period | Location | Type of study | Institutes | Number of
subjects | Median age,
years | Inclusion
criteria | Interventions | System | Outcomes | Conclusion | (Refs.) |
|---|
| Farrugia, et
al (2007) | 2007 | UK, East Kent | Case report | Single univer. | 1 | NS | Suspected
endometriosis | Laparoscopy
0-degree 10-mm with WL&NBI; spectrum, 415 nm; excision of
lesions | Olympus Exera
II | Identification of
smaller lesions of endometriosis | NBI may help
distinguish active endometriosis from fibrosis and changes from
previous surgery | (11) |
| Barrueto, et
al (2008) | 2008 | USA, Baltimore | Prospective
oilot | Single univer. | 21 | 36 | Suspected
endometriosis | Laparoscopy
0-degree 10-mm with WL&NBI; spectrum, 415 & 540 nm;
excision of lesions | Olympus Exera
II | 14 patients had
lesions identified by NBI, previously not detected by WL. 38 biopsy
specimens were taken using NBI; 20 (53%) confirmed
endometriosis | NBI may be able to
better identify the smaller lesions and excise a maximum number of
lesions, thus delaying the recurrence of endometriosis | (26) |
| Chandakas, et
al (2008) | 2008 | Greece, Athens | Prospective
pilot | Multi univer. | 95 | 33.9 | Suspected
endometriosis | Laparoscopy
0-degree 10-mm with WL&NBI; spectrum, 415 & 540 nm;
excision of lesions | Olympus Exera
II | Lesions were
collected from 95 patients, 82.7% of the endometriotic lesions
detected by NBI and 55.9% detected by WL | NBI may detect
endometriotic lesions more easily than WL | (27) |
| Kuroda, et
al (2009) | 2009 | Japan, Tokyo | Prospective
pilot | Single univer. | 23 | 35 | Suspected
endometriosis | Laparoscopy
0-degree 10-mm with WL&NBI; measurement of vascular density
(red, black, white) lesions in peritoneal endometriosis with
vascular analysis software | Olympus Exera
II | 23 patients
diagnosed with peritoneal endometriosis. Median difference of
vascular density by NBI was significantly higher in red lesions
(4.5%, P<0.001) | NBI provides an
accurate objective evaluation of vascular density, particularly for
the red lesions, which are indicative of early-stage endometriosis
with angiogenesis | (28) |
| Kuroda, et
al (2010) | 2008 | Japan, Tokyo | Prospective
control | Single univer. | 73 | 24-49 | Suspected
endometriosis | Laparoscopy
0-degree 10-mm with WL&NBI; Patients allocated to 4 groups: i)
Endometriosis group with GnRH; ii) Endometriosis group no GnRH;
iii) non-endometriosis group with GnRH; iv) non-endometriosis group
no GnRH. Assessment of peritoneal vascular density with vascular
analysis software and cytokine concentration in peritoneal fluid in
4 groups | Olympus Exera
II | Increased vascular
density detected by NBI in patients with endometriosis (P<0.01).
Increased cytokine levels in patients with endometriosis | NBI may detect
early vascular lesions in patients with endometriosis | (33) |
| Barrueto, et
al (2015) | 2015 | USA, Baltimore | Randomized
controlled | Multi univer. | 167 | 30-33.6 | Suspected
endometriosis | Laparoscopy
0-degree 10-mm. All patients received WL/WL (Control arm) or WL/NBI
(Intervention arm). Spectrum, 415 & 540 nm; excision of
lesions | Olympus Exera
II | 255 lesions were
detected and confirmed as endometriosis. 255 (100%) were detected
by NBI | The contribution of
NBI to WL increased the detection of endometriotic lesions | (34) |
| Gallichio, et
al (2015) | 2011-2013 | USA, Baltimore | Randomized
controlled | Multi univer. | 167 | 30-33.2 | Suspected
endometriosis | Laparoscopy
0-degree 10-mm. All patients received WL (3:1 ratio) followed by
WL/NBI or WL/WL. Pain and quality of life assessment with
questionnaire EHP* | Olympus Winter | Pain and quality of
life similar in both study groups (WL vs. NBI) | WL and NBI have
similar pain and quality of life outcomes | (38) |
| Murnaghan, et
al (2017) | 2017 | Canada Ottawa | Case report | Single univer. | 1 | 39 | Suspected
endometriosis | Laparoscopy
0-degree 10-mm with WL/NBI; excision of lesions | Olympus Exera
II | Identification of
smaller lesions not visible with WL | Contribution of NBI
to WL increased the detection of endometriotic lesions | (12) |
| Ma, et al
(2019) | 2014-2015 | Australia,
Victoria | Prospective
control | Single univer. | 57 | 30 | Suspected
endometriosis | Laparoscopy
0-degree 5-mm with WL&NBI. Excision of lesions | Olympus Exera
II | Total 32 patients
with lesions detected by WL. 24 of them were positive for
Endometriosis. Assessment of these 24 with NBI led to diagnosis of
6 new positions of endometriosis. Additional predic tive value of
86% if a positive diagnosis was made under WL imaging | NBI appears
beneficial in identifying new areas of endometriosis that may be
missed if endometriosis is suspected by WL. NBI was not beneficial
if WL was negative | (29) |
| Kazama, et
al (2019) | 2018 | Japan, Saitama | Case report | Single univer. | 1 | 44 | Pelvic pain Occult
fecal blood | Intestinal
endoscopy with WL&NBI | NS | Lesions of rectal
endometriosis (Dienogest treatment) | NBI may assist in
the detection of small lesions in cases of intestinal
endometriosis | (13) |
| Lier, et al
(2020) | 2016-2017 | Netherlands,
Amsterdam | Prospective
randomized | Single univer. | 20 | 34.5 | Endometriosis
III-IV (ASRM) | Laparoscopy
0-degree 12-mm with WL, NBI, NIR-ICG and 3D imaging. Excision of
lesions | Olympus Exera
II | 3D increased the
sensitivity rate (P=0.0016). Combined 3D and NBI increased the
sensitivity rate 91.2% (P<0.001) | 3D WL combined with
NBI improved the detection rate of peritoneal endometriosis | (30) |
Olympus Exetera (Olympus Corporation) was the system
used for NBI in all of the studies. None of the 11 studies reported
any adverse effects or complications related to the surgical
techniques.
NBI in cervical pathology and
peritoneal implants
Details on the selected studies reporting on the use
of NBI in laparoscopy for the detection of cervical lesions and
gynecological malignancies are listed in Table III. A total of 9 studies were
included in the review, dating from 2010 to 2020. Of these, four
studies were prospective studies (31,32,35,39)
and five studies were case reports (14-18).
The total number of patients was 156 and the mean age was
43.3±17.25 years. Uterine cervical pathology was investigated with
NBI in five studies (14,18,31,32,35)
and peritoneal implants were investigated with NBI in four studies
(15-17,39).
 | Table IIIComparison of studies reporting on
the use of NBI in patients with cervical pathology and peritoneal
implants. |
Table III
Comparison of studies reporting on
the use of NBI in patients with cervical pathology and peritoneal
implants.
| Author (year) | Time period | Country, city | Type of study | Institute | Number of
subjects | Age, years | Inclusion
criteria | Interventions | System | Outcomes | Conclusion | (Refs.) |
|---|
| Fujii, et al
(2010) | 2007-2009 | Japan, Tokyo | Prospective
pilot | Single univer. | 21 | 36.3 | Patients with
diagnosis of in situ cervical adenoCA early cervical
adenoCA | NBI digital
colposcopy; biopsy of lesions and immunochemistry with CD31
antibody; evaluation of vascular pattern | Olympus | Vascular pattern
was classified as waste thread-like pattern, dot-like pattern and
root-like pattern. Vascular patterns were displayed in 18 (86%) of
cases of cervical adenoCA | Digital NBI
colposcopy depicts vascular pattern on cervix more clearly than
conventional colposcopy, thus diagnosing early disease | (31) |
| Fanfani, et
al (2010) | 2010 | Italy, Rome | Case report | Single univer. | 1 | NS | Borderline
ovary | Laparoscopy
0-degree 10-mm with WL&NBI. Excision of lesions | Olympus Exera
II | Identification of
peritoneal implants not clearly visible by WL | NBI in laparoscopy
a useful advancement for identifying early preneoplastic and
neoplastic lesions and assisting in making intraoperative
decisions | (15) |
| Fanfani, et
al (2011) | 2011 | Italy, Rome | Case report | Single univer. | 1 | NS | Cervical CA | Laparoscopy
0-degree 10-mm with WL&NBI. Excision of lesions | Olympus Exera
II | Identification of
peritoneal implants not clearly visible by WL in a case after
laparoscopic hysterectomy for cervical CA | NBI may a useful
tool in the detection of early neoplastic peritoneal implants | (16) |
| Gagliardi, et
al (2013) | 2013 | Italy, Roma | Case report | Single univer. | 2 | 1st 632nd 67 | Recurrent Ovarian
CA 1 case of FIGO IC and 1 case of FIGO IIIC | Laparoscopy
0-degree 10-mm with WL&NBI | Olympus Winter | Identification and
NBI target biopsy of peritoneal implants of recurrent disease | NBI facilitates
diagnosis of recurrence of malignant disease | (17) |
| Nishyama, et
al (2017) | 2014-2015 | Japan, Kagawa | Prospective
pilot | Single univer. | 10 | 39 | Patients with
squamous cervical pathology LGSIL-cervical CA | Flexible magnifying
endoscopy with NBI evaluating microvascular patterns. Colposcopy
and biopsy of lesions | Olympus Exera
II | Report of NBI-ME
microvascular findings as follows: -Presence of dots in 7 (70 %)
-Irregular arrangement of dots in 5 (50%) -High-density of dots in
5 (50%) -High vessel caliber in 2 (20%) -New tumor vessel in 1
(10%) -Detection rate, 90% (9/10 patients) | Establishment of a
novel microvascular classification system via NBI-ME of cervical
lesions | (32) |
| Aloisi, et
al (2018) | 2011-2014 | USA, New York | Prospective
Comparative | Single univer. | 94 | 55.5 | Patients undergoing
laparoscopic surgery for gynecologic CA of all types | Laparoscopy
0-degree 10-mm with WL&NBI | Olympus Exera
II | Higher number of
peritoneal abnormalities detected by NBI vs. WL (P=0.0239). No
scientific significance in the detection of peritoneal metastasis
(P=0.18) | NBI provides unique
contrast between peritoneum and microvascular patterns. NBI does
not provide better detection of peritoneal malignancy than WL | (39) |
| Uchita, et
al (2018) | 2016 | Japan | Prospective
diagnostic | Multi univer. | 24 | 40 | Patients underwent
colposcopy and NBI of cervix. Patients underwent conisation | NBI with
gastroscope | Olympus | NBI revealed 3
abnormal findings: -Light white epithelium -Heavy white epithelium
-Atypical intracapillary papillary loop | NBI demonstrated
100% sensitivity, specificity, accuracy, positive predictive value
for lesions >CIN-3 | (35) |
| Anko, et al
(2019) | 2020 | Japan,
Kanagawa | Case report | Single univer. | 1 | 54 | Patient with
melanoma of cervix | NBI digital
colposcopy | NS | Report of atypical
vessels and transparent mucosal surface | NBI colposcopy may
be useful in melanoma diagnosis | (14) |
| Kobara, et
al (2020) | 2020 | Japan, Kagawa | Case report | Multi univer. | 2 | 39, 37 | Patients with
cervical HGSIL | NBI with
gastroscope | Olympus | Detection of
atypical lesion not identified by colposcopy | NBI may assist in
the diagnosis of HGSIL if not identified by | (18) |
The vascular pattern of lesions was examined in 21
patients with early and in situ cervical adenocarcinoma
using NBI (13). The authors
classified the colposcopic lesions according to the pattern
described by Wright (40). The
vascular pattern was visualized in 18 patients (86%); the authors
concluded that NBI colposcopy depicts the vascular pattern on the
cervix in early glandular disease better than conventional
colposcopy. Nishiyama et al (32) proposed a novel microvascular
classification. They used flexible magnifying endoscopy with NBI in
10 patients with cervical lesions; the detection rate was 90%
(9/10) (32). NBI assisted in the
detection of a rare melanoma of the cervix in a case report
(14). Furthermore, NBI was
utilized in laparoscopy for the detection of peritoneal metastasis
in a series of 95 female patients undergoing surgery for various
gynecological malignancies, as reported by Aloisi et al
(39). They determined that NBI
increased the number of the detected peritoneal abnormalities;
however, no statistically significant differences were observed in
the identification of histologically confirmed metastatic disease
(P=0.18) (39).
A significantly greater number of peritoneal
abnormalities were identified with NBI than with standard WL
imaging. However, no statistically significant differences were
observed in the identification of histologically confirmed
metastatic disease (39). In
addition, NBI proved to be useful in the laparoscopic detection of
early peritoneal implants in three case reports (15-17).
Kobara et al (18) indicated
that NBI increased the sensitivity, specificity, accuracy and
positive predictive value for the detection of cervical
intraepithelial lesions-3 (CIN-3) in comparison with conventional
colposcopy. NBI with a gastroscope assisted the detection of
high-grade cervical intraepithelial lesions in two patients, while
these lesions were not identified by conventional colposcopy
(18,35). None of the nine studies reported any
adverse effects or complications related to the surgical
techniques.
Quality assessment of case
reports
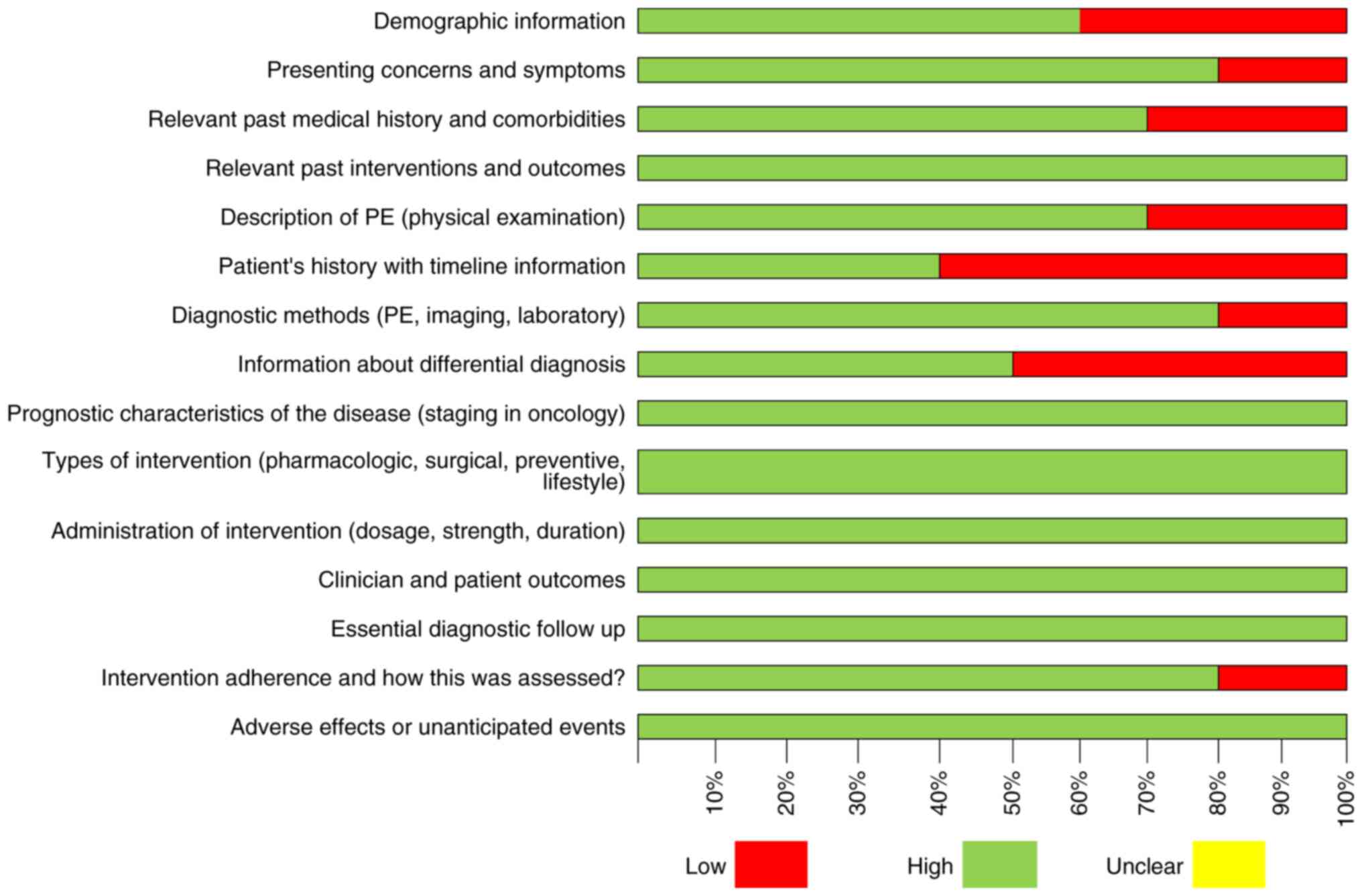
The CARE guidelines were followed to perform the
quality assessment of the case reports (7). A total of 10 case reports were
assessed for their quality (9-18).
The results are presented in Fig.
3. Approximately 30% of the case reports had a low quality in
terms of presentation of demographic information. In total, 55% of
the case reports included had low quality regarding the
presentation of the patients' history with timeline information.
Furthermore, 45% of the case reports were of poor quality in terms
of information about differential diagnosis.
Quality assessment with QUADAS-2
The QUADAS-2 tool was used to assess the risk of
bias in four domains. The results are presented in Fig. 4. In total, 19 studies were assessed.
Of these, 17 had a prospective design lacking randomization and two
were randomized controlled trials with control groups. A total of 9
studies were indicated to have a high risk of bias (24,25,27,29,30-32,34,36)
and 10 studies were determined to have a low risk of bias (19-21,23,28,30,32,37-39).
NBI in gynecological endoscopy and
special precautions in view of the Coronavirus Disease 2019
(COVID-19) pandemic
The outbreak of the COVID-19 pandemic caused by the
Severe Acute Respiratory Syndrome Coronavirus-2 (SARS-CoV-2) has
produced a public health emergency of international concern, with
all of the data demonstrating that the spread of the virus mainly
occurs via respiratory droplets during close contact (41,42).
During this ongoing pandemic, recommendations regarding laparoscopy
and endoscopy with NBI should follow the general international
recommendations for laparoscopy.
However, the potential risk of infection through
endoscopically generated bioaerosols may possibly be increased as a
result of three important factors pertaining to laparoscopy. These
are the following: i) Use of gas insufflation during entry and
intra-operatively; ii) generation of bioaerosols via
electrosurgery, which is a cornerstone of endoscopy; and iii) the
potential for gas leaks in the operation room, which may lead to
elevated viral loads in the air (41,42).
Precautions should be taken during gynecological endoscopy with
NBI, adhering to the international recommendations concerning
SARS-CoV-2 (41-43).
Regarding elective surgery, it is recommended that
universal testing for SARS-CoV-2 infection is conducted whenever
possible within 40 h preceding surgery. Should a case of SARS-CoV-2
be positively confirmed, it is advisable to delay surgery, although
exceptions may be made for urgent cases, e.g. malignancies.
It has been reported that laparoscopies have a
larger potential for aerosol spread than hysteroscopies (41-43),
while laparotomies have a lower risk of aerosol spread in
comparison to laparoscopies (41-43).
However, endoscopy is generally preferred due to the one-day stay
and the smaller exposure to a hospital environment.
Strict safety measures regarding the pressure of the
gas and pressure of the fluid should be applied to minimize the
possibility of spread. In cases where local anesthesia may be used,
it is expected to be beneficial for the patient, minimizing the
risk of infection, which may occur after the intubation and the
extubation procedure.
Further guidelines issued by the different medical
associations such as International Society for Gynecologic
Endoscopy (ISGE; www.isge.org) and American Society of
Gynecologic Laparoscopists (AAGL; https://www.aagl.org/) (42,43)
will provide additional pertinent and vital data during the current
fight against the pandemic.
Strengths and limitations
NBI, which is now regularly used in gynecology, is a
relatively new optical technology and the present systematic review
is, to the best of our knowledge, the most updated and extensive of
its kind that has been provided on this method to date. Due to the
relatively small number of randomized controlled trials,
observational studies were included in spite of providing a lower
level of evidence. While precise and clear inclusion criteria were
employed for the preparation of the present review, the small
sample size of the trials included and the overall absence of
definitions of primary outcomes inevitably reduced the quality of
the present review. Furthermore, risk of bias in the flow and
timing domains was frequently present. Therefore, it was not
possible to perform a pooled data-analysis or meta-analysis. While
case reports were included, the majority of these studies were
well-designed and mostly provided their evidence clearly and
accurately, according to the quality assessment using the CARE
(Case report) guidelines.
Discussion
The NBI system for image-enhanced endoscopy was
first conceived and developed in May 1999 and the product was
launched by Olympus Corporation in May 2006(21).
The major advantages of the NBI system are the
enhancement of endoscopic visualization of superficial neoplastic
lesions and their microvascular architecture. Conventional
endoscopic diagnosis using WL, by contrast, is based on subtle
morphological changes, e.g., superficially elevated, flat or
depressed lesions, and on minimal changes in color such as reddish
discoloration (19).
The present systematic review demonstrated that the
application of NBI in gynecological endoscopy has the potential to
improve the diagnosis of endometriosis. It may also have the
potential to enhance the diagnosis of premalignant and malignant
lesions in the fields of hysteroscopy, laparoscopy and
colposcopy.
While Kisu et al (44) performed a review in 2012, the
present systematic review is substantially updated and includes
quality assessment of the studies according to the QUADAS-2 and the
CARE guidelines (6,7).
NBI has proven to be an efficacious approach for the
diagnosis of endometrial cancer and hyperplasia, while thorough
training improves the trainee's diagnostic skills to an extent
depending on their previous hysteroscopic experience (37). However, it must be stressed that NBI
laparoscopy was not superior in the detection of peritoneal
metastases in comparison with standard WL laparoscopy alone, which
was reported by Aloisi et al (39) and Schnelldorfer et al
(45).
A significantly greater number of peritoneal
abnormalities were identified with NBI than with standard WL.
However, no statistically significant differences were observed in
the identification of histologically confirmed metastatic disease.
In fact, of the eight additional suspicious-appearing nodules
visualized with NBI, only three were confirmed as malignant on
final pathology, and none of the patients had surface malignancies
identified with NBI that were not also seen with WL, even if in a
different area (39). Aloisi et
al (39) pointed out that
further exploration of the use of NBI/3D WL imaging is required;
this will now be further evaluated in a large randomized clinical
trial with clinically relevant endpoints, with adequate power,
quality control and measures (44).
This will be according to the Idea, Development, Exploration,
Assessment and Long-term Study (IDEAL) framework, describing 5
stages of evolution for new surgical therapeutic interventions.
IDEAL is an important driver for future incremental and
evidence-based modifications (46).
Furthermore, another limitation is the extension of
the surgical time, particularly in laparoscopic procedures with the
use of NBI. Lier et al (30)
reported a median extension of surgical time of 30 min with NBI due
to thorough inspection of the peritoneum and histological sampling.
The clinical question is whether an improved detection of
endometriosis with NBI/3D imaging also affects the long-term
clinical outcomes after surgery, such as reintervention rates,
pain-free interval and quality of life (30).
A shortcoming, particularly with the methodology
reported by Barrueto et al (34), is the low specificity. This may
result in unnecessary resection of healthy tissue, producing
postoperative neuropathic pain and adhesion formation.
In the study by Surico et al (20), only a small number of patients were
recruited, while the study was performed at a single academic
institution. Furthermore, the accuracy of NBI hysteroscopy in the
prediction of histological findings via analysis of interobserver
variability was not assessed (20).
Wang et al (37) reported that the physician who
performs hysteroscopy must be familiar with endometrial lesions,
which are influenced by estrogen and progesterone secretion.
Endometrial necrosis may not only be observed in malignant lesions,
but also frequently appears in benign hyperplastic lesions
associated with abnormal uterine bleeding. These factors increase
the difficulty of hysteroscopic diagnosis; therefore, the learning
curve for the diagnosis of endometrial neoplasms is relatively
long. The authors report that >200 hysteroscopic cases are
required to be performed by physicians until proficiency is reached
(37).
The drawback of NBI colposcopy is that the system is
expensive; thus, widespread use of it is limited and is
particularly unsuitable for application in developing countries. It
may be appropriate to use for educational purposes in cancer center
hospitals or university hospitals (31).
In conclusion, conventional WL imaging in
gynecological endoscopy is now well-established as a highly
sensitive and specific technique for the diagnosis of intrauterine
diseases and the present study clearly indicated that the NBI
system, when applied by an expert and experienced surgeon, is
capable of enhancing diagnostic accuracy. Furthermore, NBI may
increase the diagnostic skills of trainees. Future directions of
research should take into consideration the reoperation rates,
recurrence and overall cost. Evidence-based frameworks such as
IDEAL should be implemented in order to improve clinical practice.
Certainly, there is a requirement for large-scale, multicenter,
randomized trials to substantiate the present results as to the
potential for use of NBI in gynecology, the application of which
may improve patients' oncological outcomes and thus their quality
of life.
Acknowledgements
The authors thank the Emeritus Professor George
Iatrakis of University of West Attica (Athens, Greece) for
assisting us in obtaining the full-text of articles.
Funding
Funding: No funding was received.
Availability of data and materials
All data generated or analyzed during this study are
included in this published article.
Authors' contributions
All authors contributed equally to the writing and
production of this manuscript. PP and KK extracted information, SS,
CK, EA, PT and NA interpreted the extracted information and
tabulated the data. NV checked the results and approved the study.
PP was the main author that formed the conception of the study. EA
checked for the eligibility of the studies. All authors read and
approved the final manuscript. PP and NV confirm the authenticity
of all the raw data.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Vincent BD and Fraig M: A pilot study of
narrow-band imaging compared to white light bronchoscopy for
evaluation of normal airways and premalignant and malignant airways
disease. Chest. 131:1794–1199. 2007.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Sano Y and Horimatsu T: Magnifying
observation of microvascular architecture of colorectal lesions
using a narrow-band imaging system. Dig Endosc. 18:44–51. 2006.
|
|
3
|
Watanabe A and Taniguchi M: The value of
narrow band imaging endoscope for early head and neck cancers.
Otolaryngol Head Neck Surg. 138:446–451. 2008.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Machida H, Sano Y, Hamamoto Y, Muto M,
Kozu T, Tajiri H and Yoshida S: Narrow-band imaging in the
diagnosis of colorectal mucosal lesions: A pilot study. Endoscopy.
36:1094–1098. 2004.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Liberati A, Altman DG, Tetzlaff J, Mulrow
C, Gøtzsche PC, Ioannidis JP, Clarke M, Devereaux PJ, Kleijnen J
and Moher D: The PRISMA statement for reporting systematic reviews
and meta-analyses of studies that evaluate healthcare
interventions: Explanation and elaboration. BMJ.
339(b2700)2009.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Whiting PF, Rutjes AW, Westwood ME,
Mallett S, Deeks JJ, Reitsma JB, Leeflang MM, Sterne JA and Bossuyt
PM: QUADAS-2 Group. QUADAS-2: A revised tool for the quality
assessment of diagnostic accuracy studies. Ann Intern Med.
155:529–536. 2011.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Gagnier JJ, Kienle G, Altman DG, Moher D,
Sox H and Riley D: CARE Group. The CARE guidelines: Consensus-based
clinical case report guideline development. J Clin Epidemiol.
67:46–51. 2014.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Tulandi T and Balayla J: Study designs and
the use of the canadian task force classification. J Obstet
Gynaecol Can. 40:1383–1384. 2018.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Surico D, Vigone A and Leo L: Narrow band
imaging in endometrial lesions. J Minim Invasive Gynecol. 16:9–10.
2009.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Raimondo I, Scarciglia ML, Amadio G,
Monterisi AF, Scambia G and Masciullo V: Narrow band imaging: А new
diagnostic tool in adenomyosis? Int J Gynaecol Obstet.
119:S531–S867. 2012.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Farrugia M, Nair MS and Kotronis KV:
Narrow band imaging in endometriosis. J Minim Invasive Gynecol.
14:393–394. 2007.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Murnaghan O, Rajakumar C, Bougie O and
Singh SS: Use of narrowband imaging for the surgical management of
endometriosis. J Obstet Gynaecol Can. 39(711)2017.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Kazama S, Hiramatsu T, Kuroda K, Hongo K,
Watanabe Y, Tanaka T and Kuriki K: A case of unique endoscopic
findings of intestinal endometriosis exposed to the mucosa:
Aggregation of papillary protruded bulges from the submucosal
elevation of the rectum. Clin J Gastroenterol. 12:166–170.
2019.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Anko M, Nakamura M, Kobayashi Y, Tsuji K,
Nakada S, Nakamura Y, Funakoshi T, Banno K and Aoki D: Primary
malignant melanoma of the uterine cervix or vagina which were
successfully treated with nivolumab. J Obstet Gynaecol Res.
46:190–195. 2020.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Fanfani F, Gallotta V, Rossitto C, Fagotti
A and Scambia G: Narrow band imaging in borderline ovarian tumor. J
Minim Invasive Gynecol. 17:146–147. 2010.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Fanfani F, Rossito C, Faggotti A, Gallotta
V, Gagliardi ML and Scambia G: Narrow-band imaging in laparoscopic
management of cervical carcinoma. J Minim Invasive Gynecol.
18:146–147. 2011.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Gagliardi ML, Polito S, Fagotti A, Fanfani
F and Scambia G: Narrow-band imaging in laparoscopic management of
recurrent platinum sensitive ovarian cancer. J Minim Invasive
Gynecol. 20:10–12. 2013.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Kobara H, Uchita K, Uedo N, Matsuura N,
Nishiyama N, Kanenishi K and Masaki T: Uterine cervical neoplasm
diagnosed by flexible magnifying endoscopy with narrow band
imaging. Diagnostics (Basel). 10(903)2020.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Cicinelli E, Tinelli R, Colafiglio G,
Pastore A, Mastrolia S, Lepera A and Clevin L: Reliability of
narrow-band imaging (NBI) hysteroscopy: A comparative study. Fertil
Steril. 94:2303–2307. 2010.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Surico D, Vigone A, Bonvini D, Tinelli R,
Leo L and Surico N: Narrow-band imaging in diagnosis of endometrial
cancer and hyperplasia: A new option? J Minim Invasive Gynecol.
17:620–625. 2010.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Kisu I, Banno K, Kobayashi Y, Ono A,
Masuda K, Ueki A, Nomura H, Hirasawa A, Abe T, Kouyama K, et al:
Flexible hysteroscopy with narrow band imaging (NBI) for endoscopic
diagnosis of malignant endometrial lesions. Int J Oncol.
38:613–618. 2011.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Kuroda K, Kitade M, Kikuchi I, Kumakiri J,
Matsuoka S, Tokita S, Kuroda M and Takeda S: A new instrument: A
flexible hysteroscope with narrow band imaging system: Optical
quality comparison between a flexible and a rigid hysteroscope.
Minim Invasive Ther Allied Technol. 20:263–266. 2011.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Kisu I, Banno K, Susumu N and Aoki D:
Magnifying hysteroscopy with narrow-band imaging for visualization
of endometrial lesions. Int J Gynaecol Obstet. 115(1):74–5.
2011.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Kong L, Duan H, Zhang Y, Wang Y and Guo Y:
Application of narrow-band imaging in the diagnosis of endometrial
lesions. J Minim Invasive Gynecol. 22(S45)2015.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Ozturk M, Ulubay M, Alanbay I, Keskin U,
Karasahin E and Yenen MC: Using narrow-band imaging with
conventional hysteroscopy increases the detection of chronic
endometritis in abnormal uterine bleeding and postmenopausal
bleeding. J Obstet Gynaecol Res. 42:67–71. 2016.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Barrueto FF and Audlin KM: The use of
narrowband imaging for identification of endometriosis. J Minim
Invasive Gynecol. 15:636–639. 2008.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Chandakas S, Salamalekis E and Erian J:
New narrow band imaging endoscopic system for the detectionof
surface pathology including endometriosis: A series of 95 patients.
J Minim Invasive Gynecol. 15:S1–S159. 2008.
|
|
28
|
Kuroda K, Kitade M, Kikuchi I, Kumakiri J,
Matsuoka S, Jinushi M, Shirai Y, Kuroda M and Takeda S: Vascular
density of peritoneal endometriosis using narrow-band imaging
system and vascular analysis software. J Minim Invasive Gynecol.
16:618–621. 2009.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Ma T, Chowdary P, Eskander A, Ellett L,
McIlwaine K, Manwaring J, Readman E and Maher P: Can narrowband
imaging improve the laparoscopic identification of superficial
endometriosis? A prospective cohort trial. J Minim Invasive
Gynecol. 26:427–433. 2019.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Lier MC, Vlek SL, Ankersmit M, van de Ven
PM, Dekker JJML, Bleeker MCG, Mijatovic V and Tuynman JB:
Comparison of enhanced laparoscopic imaging techniques in
endometriosis surgery: A diagnostic accuracy study. Surg Endosc.
34:96–104. 2020.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Fujii T, Nakamura M, Kameyama K, Saito M,
Nishio H, Ohno A, Hirao N, Iwata T, Tsukazaki K and Aoki D: Digital
colposcopy for the diagnosis of cervical adenocarcinoma using a
narrow band imaging system. Int J Gynecol Cancer. 20:605–610.
2010.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Nishiyama N, Kanenishi K, Mori H, Kobara
H, Fujihara S, Chiyo T, Kobayashi N, Matsunaga T, Ayaki M, Yachida
T, et al: Flexible magnifying endoscopy with narrow band imaging
for the diagnosis of uterine cervical tumors: A cooperative study
among gastrointestinal endoscopists and gynecologists to explore a
novel microvascular classification system. Oncol Lett. 14:355–362.
2017.PubMed/NCBI View Article : Google Scholar
|
|
33
|
Kuroda K, Kitade M, Kikuchi I, Kumakiri J,
Matsuoka S, Kuroda M and Takeda S: Peritoneal vascular density
assessment using narrow-band imaging and vascular analysis
software, and cytokine analysis in women with and without
endometriosis. J Minim Invasive Gynecol. 17:21–25. 2010.PubMed/NCBI View Article : Google Scholar
|
|
34
|
Barrueto FF, Audlin KM, Gallicchio L,
Miller C, MacDonald R, Alonsozana E, Johnston M and Helzlsouer KJ:
Sensitivity of narrow band imaging compared with white light
imaging for the detection of endometriosis. J Minim Invasive
Gynecol. 22:846–852. 2015.PubMed/NCBI View Article : Google Scholar
|
|
35
|
Uchita K, Kanenishi K, Hirano K, Kobara H,
Nishiyama N, Kawada A, Fujihara S, Ibuki E, Haba R, Takahashi Y, et
al: Characteristic findings of high-grade cervical intraepithelial
neoplasia or more on magnifying endoscopy with narrow band imaging.
Int J Clin Oncol. 23:707–714. 2018.PubMed/NCBI View Article : Google Scholar
|
|
36
|
Tinelli R, Surico D, Leo L, Pinto V,
Surico N, Fusco A, Cicinelli MV, Meir YJ and Cicinelli E: Accuracy
and efficacy of narrow-band imaging versus white light hysteroscopy
for the diagnosis of endometrial cancer and hyperplasia: a
multicenter controlled study. Menopause. 18:1026–1029.
2011.PubMed/NCBI View Article : Google Scholar
|
|
37
|
Wang W, Chen F, Kong L, Guo Y, Cheng J and
Zhang Y: Prospective evaluation of the accuracy of a training
program in image recognition by narrow-band imaging guided
hysteroscopy of endometrial neoplasms. Gynecol Obstet Invest.
85:284–289. 2020.PubMed/NCBI View Article : Google Scholar
|
|
38
|
Gallicchio L, Helzlsouer KJ, Audlin KM,
Miller C, MacDonald R, Johnston M and Barrueto FF: Change in pain
and quality of life among women enrolled in a trial examining the
use of narrow band imaging during laparoscopic surgery for
suspected endometriosis. J Minim Invasive Gynecol. 22:1208–1214.
2015.PubMed/NCBI View Article : Google Scholar
|
|
39
|
Aloisi A, Sonoda Y, Gardner GJ, Park KJ,
Elliott SL, Zhou QC, Iasonos A and Abu-Rustum NR: Prospective
comparative study of laparoscopic narrow band imaging (NBI) versus
standard imaging in gynecologic oncology. Ann Surg Oncol.
25:984–990. 2018.PubMed/NCBI View Article : Google Scholar
|
|
40
|
Wright VC: Cervical glandular disease:
Adenocarcinoma in situ and adenocarcinoma. In: Colposcopy
Principles and Practice. Barbara S, Apgar GL and Spitzer M (eds).
2nd edition. Saunders Elsevier, Philadelphia, PA, 283Y310,
2008.
|
|
41
|
Carugno J, Di Spiezio Sardo A, Alonso L,
Haimovich S, Campo R, De Angelis C, Bradley L, Bettocchi S, Arias
A, Isaacson K, et al: COVID-19 pandemic. Impact on hysteroscopic
procedures: A consensus statement from the global congress of
hysteroscopy scientific committee. J Minim Invasive Gynecol.
27:988–992. 2020.PubMed/NCBI View Article : Google Scholar
|
|
42
|
Thomas V, Maillard C, Barnard A, Snyman L,
Chrysostomou A, Shimange-Matsose L and Van Herendael B:
International Society for Gynecologic Endoscopy (ISGE) guidelines
and recommendations on gynecological endoscopy during the
evolutionary phases of the SARS-CoV-2 pandemic. Eur J Obstet
Gynecol Reprod Biol. 253:133–140. 2020.PubMed/NCBI View Article : Google Scholar
|
|
43
|
American Association of Gynecologic
Laparoscopists. COVID-19: Joint Society Statement on Elective
Surgery. Available from: http://www.aagl.org/news/covid-19-joint-statement-on-elective-surgeries/.
|
|
44
|
Kisu I, Banno K, Tsuji K, Masuda K, Ueki
A, Kobayashi Y, Yamagami W, Susumu N and Aoki D: Narrow band
imaging in gynecology: A new diagnostic approach with improved
visual identification (Review). Int J Oncol. 40:350–356.
2012.PubMed/NCBI View Article : Google Scholar
|
|
45
|
Schnelldorfer T, Jenkins RL, Birkett DH,
Wright VJ, Price LL and Georgakoudi I: Laparoscopic narrow band
imaging for detection of occult cancer metastases: A randomized
feasibility trial. Surg Endosc. 30:1656–1661. 2016.PubMed/NCBI View Article : Google Scholar
|
|
46
|
Hirst A, Philippou Y, Blazeby J, Campbell
B, Campbell M, Feinberg J, Rovers M, Blencowe N, Pennell C, Quinn
T, et al: No Surgical innovation without evaluation: Evolution and
further development of the IDEAL framework and recommendations. Ann
Surg. 269:211–220. 2019.PubMed/NCBI View Article : Google Scholar
|