Introduction
In December 2019, a new strain of virus causing
severe acute respiratory syndrome (SARS-CoV-2) appeared for the
first time in the city of Wuhan, Hubei province, China. The virus
spread rapidly and, at the time of writing this study, more than 10
million cases were reported in 216 countries (1).
Coronaviruses (CoV), generally known to cause acute
respiratory infections, are enveloped viruses that have a
single-stranded, positive-sense RNA genome (2). Although the majority of coronavirus
infections affecting humans are mild, there have already been two
important outbreaks of two types of coronaviruses causing multiple
severe pneumonias: The severe acute respiratory syndrome
coronavirus (SARS-CoV), with a mortality rate of up to 10%, and
Middle East respiratory syndrome coronavirus (MERS-CoV), with a
mortality rate of over 34% (3,4).
Although SARS-CoV-2 has exhibited similar phylogenetic and clinical
features with SARS-CoV, this new coronavirus appears to be
considerably more easily transmissible, albeit less deadly
(5). Typical symptoms, encountered
in over 40% of the cases include fever, cough, fatigue and
shortness of breath, and also less frequent common symptoms
including anosmia and ageusia (6).
As the SARS-CoV-2 pandemic unfolded, diabetes
mellitus (DM) was already one of the leading causes of morbidity
and mortality throughout the world, and it is known that DM
produces a plethora of macrovascular and microvascular
complications that ultimately impact overall patient survival
(7). In this new context, several
studies reported apparent associations between diabetes mellitus,
acute respiratory distress syndrome, more severe disease, and
increased mortality (8-11).
Multiple explanations have been put forth for this hypothesized
association between DM as the underlying disease and the increased
severity of SARS CoV-2 infection. Natural immunity, which is the
primary line of defense against SARS-CoV-2, is inevitably weakened
in patients that have uncontrolled DM; consequently, the virus
proliferates unrestricted within the host (12). In fact, it has been demonstrated
that even short-term hyperglycemia can briefly paralyze the natural
immune system (13). In addition,
DM promotes an increased pro-inflammatory cytokine response, mainly
involving interleukin (IL)-1, IL-6 and tumor-necrosis factor
(TNF)-α, which further aggravates the prognosis of a SARS-CoV-2
infection (14).
The development and manufacturing of a vaccine
against SARS-CoV-2 is an issue of utmost importance, however, it
must be taken into consideration that it is going to take numerous
months to produce a vaccine. Although several companies have
announced that a vaccine against COVID-19 will be ready soon, this
will be quite difficult to accomplish in reality considering that
short- and long-term safety have to be taken into account (15).
Materials and methods
A retrospective observational study on confirmed
SARS-CoV-2 patients admitted to ‘Sf. Parascheva’ Clinical Hospital
of Infectious Diseases, Iasi, Romania was conducted between March
4th (the first such admission) and June 30th (the writing of the
article). The primary inclusion criteria of the patients in the
present study was represented by confirmed SARS-CoV-2 infection
tested by RT-PCR assay which had as associated diagnosis type 1 or
2 DM. Patients that did not have a history of DM type 1 or 2 and/or
had a negative result with RT-PCR testing were excluded from the
present study.
The following data were collected: Demographic data,
medical history, clinical and paraclinical data, blood tests,
administered treatment and outcome. The RT-PCR tests were performed
by either a molecular biology hospital laboratory or other
accredited laboratories from Iasi county, Romania.
Results
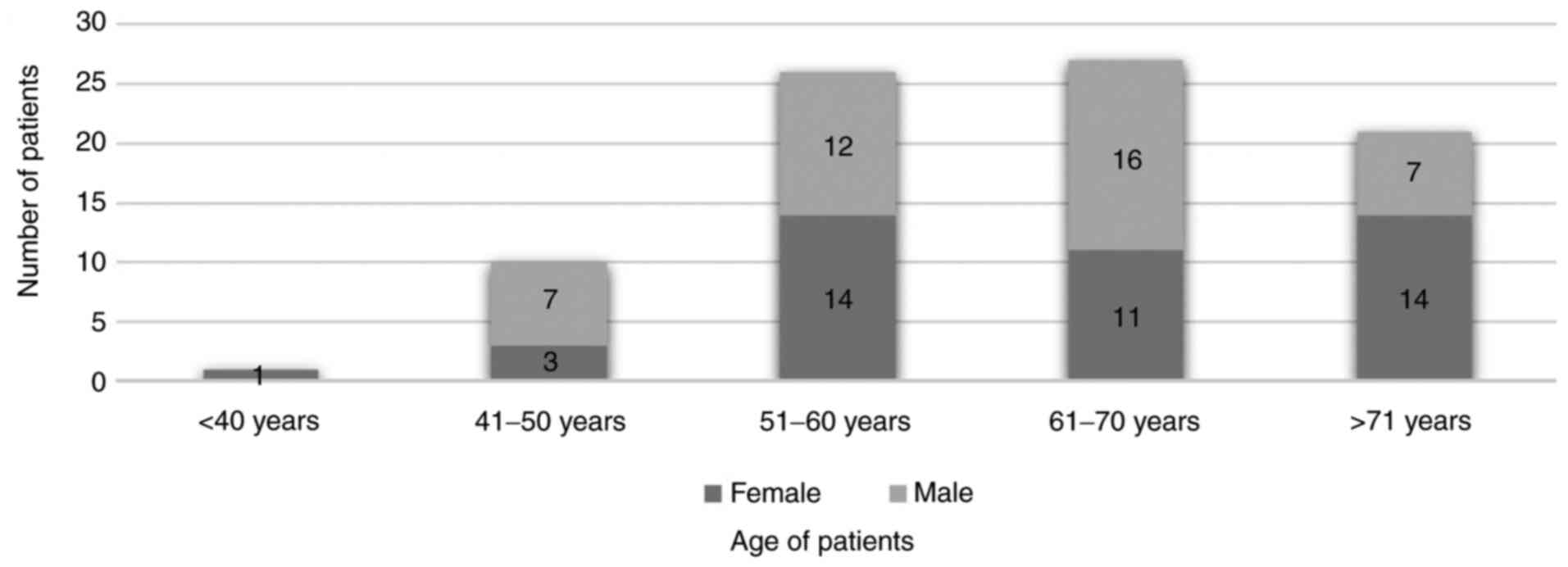
From the beginning of the outbreak, a total of 1,080
patients were admitted to ‘Sf. Parascheva’ Clinical Hospital of
Infectious Diseases of Iași, Romania. Of these patients, 85 (7.87%)
were known to be suffering from DM, mostly type 2 (82 cases,
96.46%). Diabetic patients between 51-70 years old were the most
affected by the SARS-CoV-2 infection, the mean age being 62
(Fig. 1), and they presented in
fairly equal proportions gender wise (42 were men, 49,41%).
Other associated pathologies were cardiovascular
(hypertension, heart failure, and atrial fibrillation),
neurological (stroke, epilepsy), neoplastic, renal (kidney failure
with or without chronic dialysis) (Fig.
2).
From the total of 1,080 patients admitted, 78 cases
involving patients with associated underlying diseases, intensive
care unit (ICU) therapy was required. Of these cases, 17 patients
had DM as one of the underlying diseases. The majority of these
patients (64 cases), presented with oxygen desaturation (Sp02
<89%), were dyspneic and polypneic, or they became
hemodynamically unstable with their arterial pressure level
dropping below 85/50 mmHg. Fifty-nine patients ultimately required
orotracheal intubation and mechanical ventilation due to multiple
complications including aspiration bronchopneumonia, sepsis, and
multiple organ dysfunction syndrome (MODS).
In addition, in all cases, chest CTs revealed
lesions specific for SARS-CoV-2 infection, described either as
ground-glass opacities or ‘crazy paving’ area patterns, linear
densities or consolidations.
The treatment was administered according to the
international and national guidelines available at the time and
included hydroxychloroquine (HCQ)/lopinavir + ritonavir/enoxaparin
sodium/tocilizumab/antibiotherapy. Each patient received
individualized treatment based on the clinical and paraclinical
data, as well as taking into consideration medical interactions.
During hospitalization, the management of associated
cardiovascular, neurologic, neoplastic and renal comorbidities was
ensured, alongside antibiotic treatment to address other types of
infectious diseases whenever present, including urinary tract
infections, sepsis, cellulitis, and Clostridium difficile
infection. In addition, psychological therapy was performed upon
request (16,17).
Regarding the paraclinical data of patients with DM,
glycemic levels over 200 mg/dl were observed in all the cases at
the admittance and a median glycated hemoglobin level of 7.2% was
calculated.
We took into consideration two groups of patients
admitted to the ICU, group A, patients without DM (61 patients) and
group B, patients with DM (17 patients). The fatality rate among
the patients in group B was considerably higher (88,23%, 15
patients) than the rate of mortality among group B (59.01%, 36
patients) (Fig. 3).
Regarding the glycemic levels of the patients with
DM admitted to the ICU correlated with the level of C reactive
protein (CRP), it was observed that CRP values >70 mg/l were
encountered in the patients that deceased. Patients admitted to the
ICU with a CRP <70 mg/l (patient 16 and 17) survived and were
later transferred to the clinic (Fig.
4).
Discussion
The latest studies in scientific literature have
been revealing a noteworthy association between increased mortality
and morbidity in patients with SARS-CoV-2 and advanced age, severe
obesity (BMI ≥40 kg/m2), hypertension and DM as
underlying diseases (8,10,14,18,19).
In the general population, the prevalence of DM is 8.5% (20) and among the admitted patients
considered for the present study it was 7.87%. In addition, the
literature states that, elder patients are more affected by DM and
often by other comorbidities, especially after the age of 60
(21-23),
a fact that can also be sustained by the present study in which
>50% of the patients (56.47%) were >60 years old. If we take
into consideration that hypertension as well as cardiovascular
disease are prevalent in DM patients, it is unclear whether DM
independently contributes to this increased risk. However, diabetes
has already been frequently reported to be associated with poor
prognosis in other respiratory viral infections, mainly seasonal
influenza, pandemic influenza A H1N1, SARS, and MERS (24,25).
In March 2020, an Italian health institute reported
2,003 patients that succumbed from SARS-CoV-2 infection (26). Their median age was 80.5, which was
considerably higher than the median age 67.84 of the patients
included in the present study. In addition, the same study stated
that the prevalence of diabetes was 35.5% and that 70% of the total
number of patients were men (26),
while in our study gender differences were negligible (49.41%
patients were men). Furthermore, in the largest case series
reported by the Chinese Center for Disease Control and Prevention,
performed on 72,314 cases of COVID-19, the patients with DM had a
higher mortality (7.3% in DM vs. 2.3% overall) (9).
Moutschen et al (27) and Knapp et al (28) acknowledge that poorly controlled
diabetes inhibits lymphocyte proliferation, and also modifies the
functions of neutrophils and monocytes/macrophages. Studies
(29,30) performed in vitro demonstrated
that pulmonary epithelial cells respond to high glucose levels by
significantly facilitating the replication of influenza virus. This
indicates that hyperglycemia may contribute to increased viral
replication in vivo (31),
which can also apply to the case of the SARS-CoV-2 virus.
Furthermore, endothelial dysfunction and increased
platelet aggregation have been associated with type 2 DM and
insulin resistance. These are flaws which support the development
of a hypercoagulable pro-thrombotic state (32). Last but not least, patients with
diabetes have also been revealed to have diminished forced vital
capacity (FVC) and forced expiratory volume in one second (FEV1),
which is associated with increased plasma glucose levels (33). This may explain the increased number
of patients that required ICU therapy (42.35%) and also the
increased fatality rate of the patients with underlying DM.
Multiple studies (7,34-36)
have determined the serum concentration of CRP in patients with
COVID-19 and the results revealed that increased levels of CRP were
observed in up to 86% of severe COVID-19 patients. CRP was found at
increased levels in the severe group at the initial stage than
those in the mild group (35) and
also Luo et al observed in their study that patients who
succumbed to COVID-19 had approximately 10-fold higher levels of
CRP than the recovered patients (37). In the present study, the patients
admitted to the ICU that succumbed had an increase of CRP value
between 14-88-fold (71.36-440.46 mg/l).
In conclusion, uncontrolled DM appears to be a
significant predictor of mortality, not only because of how it
modifies physiological mechanisms but also by how it predisposes
the patient to multiple complications. However, even in the
presence of advanced age and DM, 82.35% from the total number of
the patients included in the study were cured. Careful assessment
of the numerous components that contribute to poor prognosis of the
patients with diabetes infected with SARS-CoV-2 virus may represent
the best way to overcome the current situation.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
All data generated or analyzed during this study are
included in this published article and its supplementary files.
Authors' contributions
CM and GAL designed the study. DN and AV contributed
to data extraction and quality assessment. CM, DN and GAL were
responsible for the analysis and discussion of the data. CM and GAL
drafted the manuscript. AV and DN critically revised the manuscript
for important intellectual content. All authors read and approved
the final manuscript.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Coronavirus disease (COVID-19) Weekly
Epidemiological Update and Weekly Operational Update. https://www.who.int/docs/default-source/coronaviruse/20200630-covid-19-sitrep-162.pdf?sfvrsn=
e00a5466_2. Accessed June 30, 2020.
|
|
2
|
Cui J, Li F and Shi ZL: Origin and
evolution of pathogenic coronaviruses. Nat Rev Microbiol.
17:181–192. 2019.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Song Z, Xu Y, Bao L, Zhang L, Yu P, Qu Y,
Zhu H, Zhao W, Han Y and Qin C: From SARS to MERS, thrusting
coronaviruses into the spotlight. Viruses. 11(59)2019.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Docea AO, Tsatsakis A, Albulescu D,
Cristea O, Zlatian O, Vinceti M, Moschos SA, Tsoukalas D, Goumenou
M, Drakoulis N, et al: A new threat from an old enemy: Re-emergence
of coronavirus (Review). Int J Mol Med. 45:1631–1643.
2020.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Ceccarelli M, Berretta M, Venanzi Rullo E,
Nunnari G and Cacopardo B: Differences and similarities between
Severe Acute Respiratory Syndrome (SARS)-CoronaVirus (CoV) and
SARS-CoV-2. Would a rose by another name smell as sweet? Eur Rev
Med Pharmacol Sci. 24:2781–2783. 2020.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Tanasa IA, Manciuc C, Carauleanu A,
Navolan DB, Bohiltea RE and Nemescu D: Anosmia and ageusia
associated with coronavirus infection (COVID-19)-what is known? Exp
Ther Med. 20:2344–2347. 2020.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Williams R, Karuranga S, Malanda B, Saeedi
P, Basit A, Besançon S, Bommer C, Esteghamati A, Ogurtsova K, Zhang
P and Colagiuri S: Global and regional estimates and projections of
diabetes-related health expenditure: Results from the International
Diabetes Federation Diabetes Atlas, 9th edition. Diabetes Res Clin
Pract. 162(108072)2020.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He
JX, Liu L, Shan H, Lei CL, Hui DSC, et al: China medical treatment
expert group for Covid-19: Clinical characteristics of coronavirus
disease 2019 in China. N Engl J Med. 382:1708–1720. 2020.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Wu Z and McGoogan JM: Characteristics of
and important lessons from the coronavirus disease 2019 (COVID-19)
Outbreak in China: Summary of a Report of 72 314 cases from the
Chinese center for disease control and prevention. JAMA.
323:1239–1242. 2020.
|
|
10
|
Yang X, Yu Y, Xu J, Shu H, Xia J, Liu H,
Wu Y, Zhang L, Yu Z, Fang M, et al: Clinical course and outcomes of
critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China:
A single-centered, retrospective, observational study. Lancet
Respir Med. 8:475–481. 2020.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Wu C, Chen X, Cai Y, Xia J, Zhou X, Xu S,
Huang H, Zhang L, Zhou X, Du C, et al: Risk factors associated with
acute respiratory distress syndrome and death in patients with
coronavirus disease 2019 pneumonia in Wuhan, China. JAMA Intern
Med. 180:934–943. 2020.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Geerlings SE and Hoepelman AI: Immune
dysfunction in patients with diabetes mellitus (DM). FEMS Immunol
Med Microbiol. 26:259–265. 1999.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Jafar N, Edriss H and Nugent K: The effect
of short-term hyperglycemia on the innate immune system. Am J Med
Sci. 351:201–211. 2016.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Onder G, Rezza G and Brusaferro S:
Case-fatality rate and characteristics of patients dying in
relation to COVID-19 in Italy. JAMA. 323:1775–1776. 2020.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Calina D, Docea AO, Petrakis D, Egorov AM,
Ishmukhametov AA, Gabibov AG, Shtilman MI, Kostoff R, Carvalho F,
Vinceti M, et al: Towards effective COVID-19 vaccines: Updates,
perspectives and challenges (Review). Int J Mol Med. 46:3–16.
2020.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Manciuc C and Largu A: Impact and risk of
institutionalized environments on the psyho-emotional development
of the HIV-positive youth. Environ Eng Manag J. 13:3123–3129.
2014.
|
|
17
|
Manciuc C, Filip-Ciubotaru F, Badescu A,
Duceag LD and Largu AM: The patient-doctor-psychologist triangle in
a case of severe imunosupression in the HIV infection. Rev Med Chir
Soc Med Nat Iasi. 120:119–123. 2016.PubMed/NCBI
|
|
18
|
Centers for Disease Control and
Prevention: National Diabetes Statistics Report, 2020. Centers for
Disease Control and Prevention, US Department of Health and Human
Services, Atlanta, GA, pp9, 2020.
|
|
19
|
Yang J, Zheng Y, Gou X, Pu K, Chen Z, Guo
Q, Ji R, Wang H, Wang Y and Zhou Y: Prevalence of comorbidities and
its effects in patients infected with SARS-CoV-2: A systematic
review and meta-analysis. Int J Infect Dis. 94:91–95.
2020.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Emerging Risk Factors Collaboration.
Sarwar N, Gao P, Seshasai SR, Gobin R, Kaptoge S, Di Angelantonio
E, Ingelsson E, Lawlor DA, Selvin E, et al: Diabetes mellitus,
fasting blood glucose concentration, and risk of vascular disease:
A collaborative meta-analysis of 102 prospective studies. Lancet.
375:2215–2222. 2010.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Chentli F, Azzoug S and Mahgoun S:
Diabetes mellitus in elderly. Indian J Endocrinol Metab.
19:744–752. 2015.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Davis JW, Chung R and Juarez DT:
Prevalence of comorbid conditions with aging among patients with
diabetes and cardiovascular disease. Hawaii Med J. 70:209–213.
2011.PubMed/NCBI
|
|
23
|
Tyrovolas S, Koyanagi A, Garin N, Olaya B,
Ayuso-Mateos JL, Miret M, Chatterji S, Tobiasz-Adamczyk B, Koskinen
S, Leonardi M, et al: Diabetes mellitus and its association with
central obesity and disability among older adults: A global
perspective. Exp Gerontol. 64:70–77. 2015.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Hong KW, Cheong HJ, Choi WS, Lee J, Wie
SH, Baek JH, Kim HY, Jeong HW and Kim WJ: Clinical courses and
outcomes of hospitalized adult patients with seasonal influenza in
Korea, 2011-2012: Hospital-based Influenza Morbidity &
Mortality (HIMM) surveillance. J Infect Chemother. 20:9–14.
2014.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Schoen K, Horvat N, Guerreiro NFC, de
Castro I and de Giassi KS: Spectrum of clinical and radiographic
findings in patients with diagnosis of H1N1 and correlation with
clinical severity. BMC Infect Dis. 19(964)2019.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Istituto Superiore di Sanita: Report of
characteristics of patients died positive for COVID-19 in Italy.
Accesed May 21, 2020.
|
|
27
|
Moutschen MP, Scheen AJ and Lefebvre PJ:
Impaired immune responses in diabetes mellitus: Analysis of the
factors and mechanisms involved. Relevance to the increased
susceptibility of diabetic patients to specific infections. Diabete
Metab. 18:187–201. 1992.PubMed/NCBI
|
|
28
|
Knapp S: Diabetes and infection: Is there
a link?-A mini-review. Gerontology. 59:99–104. 2013.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Reading PC, Allison J, Crouch EC and
Anders EM: Increased susceptibility of diabetic mice to influenza
virus infection: Compromise of collectin-mediated host defense of
the lung by glucose? J Virol. 72:6884–6887. 1998.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Ilyas R, Wallis R, Soilleux EJ, Townsend
P, Zehnder D, Tan BK, Sim RB, Lehnert H, Randeva HS and Mitchell
DA: High glucose disrupts oligosaccharide recognition function via
competitive inhibition: A potential mechanism for immune
dysregulation in diabetes mellitus. Immunobiology. 216:126–131.
2011.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Kohio HP and Adamson AL: Glycolytic
control of vacuolar-type ATPase activity: A mechanism to regulate
influenza viral infection. Virology. 444:301–309. 2013.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Dunn EJ and Grant PJ: Type 2 diabetes: An
atherothrombotic syndrome. Curr Mol Med. 5:323–332. 2005.PubMed/NCBI View Article : Google Scholar
|
|
33
|
Lange P, Groth S, Kastrup J, Mortensen J,
Appleyard M, Nyboe J, Jensen G and Schnohr P: Diabetes mellitus,
plasma glucose and lung function in a cross-sectional population
study. Eur Respir J. 2:14–19. 1989.PubMed/NCBI
|
|
34
|
Chen N, Zhou M, Dong X, Qu J, Gong F, Han
Y, Qiu Y, Wang J, Liu Y, Wei Y, et al: Epidemiological and clinical
characteristics of 99 cases of 2019 novel coronavirus pneumonia in
Wuhan, China: A descriptive study. Lancet. 395:507–513.
2020.PubMed/NCBI View Article : Google Scholar
|
|
35
|
Chen T, Wu D, Chen H, Yan W, Yang D, Chen
G, Ma K, Xu D, Yu H, Wang H, et al: Clinical characteristics of 113
deceased patients with coronavirus disease 2019: Retrospective
study. BMJ. 368(m1091)2020.PubMed/NCBI View Article : Google Scholar
|
|
36
|
Gao Y, Li T, Han M, Li X, Wu D, Xu Y, Zhu
Y, Liu Y, Wang X and Wang L: Diagnostic utility of clinical
laboratory data determinations for patients with the severe
COVID-19. J Med Virol. 92:791–796. 2020.PubMed/NCBI View Article : Google Scholar
|
|
37
|
Luo X, Zhou W, Yan X, Guo T, Wang B, Xia
H, Ye L, Xiong J, Jiang Z, Liu Y, et al: Prognostic value of
C-reactive protein in patients with COVID-19. Clin Infect Dis: May
23, 2020 (Epub ahead of print). doi: 10.1093/cid/ciaa641.
|