Introduction
Conjunctival sac stenosis is the contraction of the
conjunctival sac as a result of trauma or disease. Conjunctival sac
stenosis is divided into congenital and posteriority, congenital
micro-ophthalmia or nonocular disease, which may be present in
combination with other deformities. The postnatal nature is largely
due to chemical burns, conjunctival tissue defects caused by
explosion injuries and the conjunctival sac stenosis caused by
subsequent scar healing. Conjunctival sac narrowing is further
classified into mild, moderate and severe: Mild conjunctival sac
stenosis is defined as sac narrowing to less than one-third of the
normal size and the sac and conjunctival dome becomes shallow;
moderate conjunctival sac stenosis is defined as conjunctival sac
narrowing to ~ one-half the usual size; and severe conjunctival sac
stenosis is defined as a conjunctival sac narrowing by more than
one-third of the normal sac size, disappearance of the fornix and
closure of the conjunctival sac (1).
At present, the standard treatment for conjunctival
sac stenosis primarily involves mucosal or scleral transplantation
and total eye reconstruction surgery (2,3). These
procedures are often unsuccessful due to infection, delayed orbital
implant vascularization, exposure of the prosthetic socket and
other disruptions of graft healing. In the present study, survival
of the implant, wound healing of the conjunctival sac and the
vascularization of the prosthesis were assessed, which are
associated with surgical outcomes of conjunctival sac stenosis and
postoperative complications (4,5).
Low-level laser therapy (LLLT) does not require subsequent physical
therapy. A number of studies have demonstrated positive outcomes of
LLLT, including the promotion of wound healing (6,7),
reduction of inflammation (8,9) and
increased blood flow to local blood vessels (10).
The aims of the present study were to observe the
clinical effects of LLLT combined with hydroxyapatite (HA)
implantation in the treatment of conjunctival sac stenosis.
Experiments in a rabbit model were simultaneously performed to
observe the effects of LLLT on the vascularization of the
prosthesis in animals. Together, the results of the present study
highlight a possible mechanism by which LLLT may prevent exposure
of the prosthesis.
Case report
Ethics
The protocols used in the present study were
approved by The Affiliated Eye Hospital of Nanchang University
Ethics Committee (Nanchang, China). All participating patients
provided informed written consent prior to inclusion in the present
study.
Observation of clinical efficacy of
LLLT in human patients
Clinical trial registration no: ChiCTR-DDT-12002660
(www.chictr.org/cn/). Between 2016 and
2017, 10 cases of conjunctival sac stenosis were investigated in 7
males and 3 females, aged 10-67 years old (average age, 36.5
years). Patients who had diseases which may have influenced wound
healing, including diabetes, uremia, chronic inflammatory disease
(acute or chronic infectious disease), endocrine disease,
autoimmune disease, blood disease or tumor diseases were excluded.
Patients were divided into mild, moderate and severe groups based
on the severity of conjunctival sac narrowing and all patients
underwent a scleral graft procedure, HA implantation combined with
the eye 18-20 mm diameter. Following bandage removal 3 days after
surgery, LLLT was administered. Patients in the moderate stenosis
group were treated using two courses of LLLT, whereas patients in
the severe group were treated using three courses of LLLT and the
time interval between all treatments was 2 days. Survival of the
sclera graft and conjunctival healing was observed at various time
points after the operation. Antibiotics and epidermal growth
factors were administered during laser treatment and follow-up and
weekly check-ins were conducted to monitor the conjunctival
incision until it was completely healed.
Postoperative LLLT following eye
removal and HA orbital implantation in a rabbit model
A total of 30 male and female New Zealand white
rabbits, weighing 2-3 kg, were used in the present study. HA
implantations were 12 mm in diameter, had a 500 µm pore size and a
100% interoperability rate (Beijing YHJ Science And Trade Co.,
Ltd.). The rabbits were randomly divided into the laser irradiation
group (groups B and C; n=20) and control group (group A, n=10).
Each animal underwent right eye removal and HA prosthesis
implantation. Irradiation groups B and C were treated with LLLT 3
days postoperatively; one course of treatment was given to group B
and two courses of treatment were given to group C and the time
interval between treatments was 1 week.
Laser probe and irradiation
procedure
A semiconductor laser (JAM2-II type; Jiangxi Teli
Anaesthesia & Respiration Equipment Co., Ltd.) was used to
issue radiation at a wavelength of λ=650 nm with an adjustable
power of 10 mW (0-20 mW). The spot diameter was 10 mm, with the
laser power density at 12.7 mW/cm2. Irradiation was
performed once daily for 5 min at a dose of ~3.8 J/cm2
over a period of 5 days.
99mTc-Methyl diphosphonate
(99mTc-MDP) bone imaging examination in the rabbit
model
To quantitatively assess the degree of
vascularization following HA prosthesis implantation, a
radionuclide scan was performed using single photon emission
computed tomography (SPECT) on all the experimental animals at 1,
2, 4, 6 and 8 weeks after surgery. SPECT pretreatment conditions
for peak 140 kev, window width is 15%, 256x256 static matrix, the
preset count to 5x105 and the orbital symmetry position
region of interest (ROI) was selected. The average radioactivity
ratio was presented as R/L and the experiments were repeated five
times to calculate the average radioactivity ratio. Intravenous
99mTc-MDP imaging agent 4mCi was injected and after 3 h
the rabbits were anesthetized by animal intramuscular injection
with ketamine (50 mg/kg) and chlorpromazine (25 mg/kg) (11) and laid on the test bench.
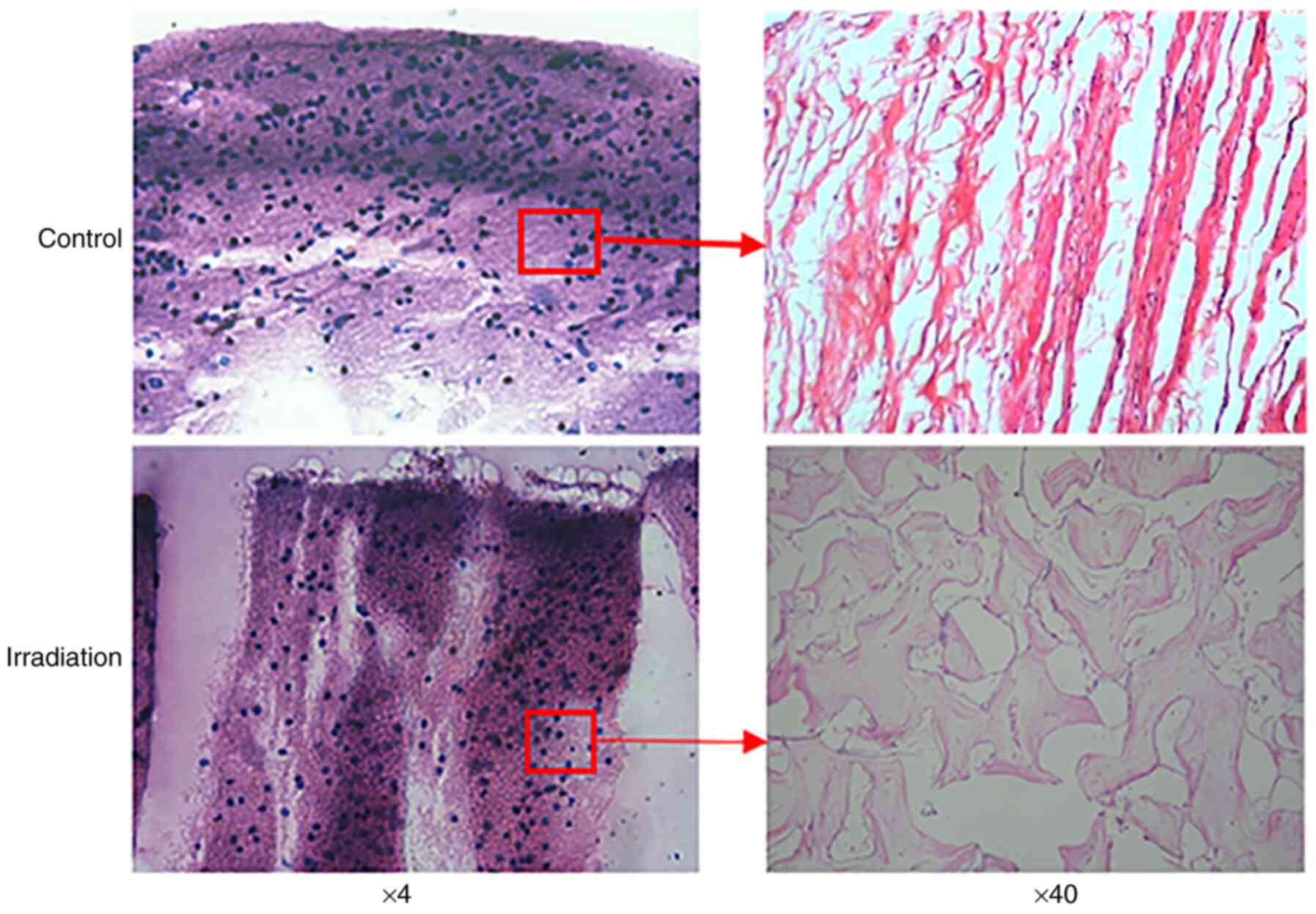
Histopathological examination of HA
orbital implantation
The animals were sacrificed during the 8th
postoperative week, with the connective tissue around their eyes
observed. The implant was fixed for 24 h with formaldehyde and
after 72 h the nitrate was removed. Conventional paraffin
embedding, sagittal section and H&E staining were all performed
respectively. The fibrovascular and inflammatory cell infiltration
in the LLLT groups and control group were observed under an optical
microscope (magnification, x4 and x40).
Statistical analysis
Statistical analyses were performed using SPSS
software (IBM Corp.). The data are expressed as the mean ± standard
deviation (unless otherwise shown). The average radioactivity count
ratio of ROI between surgical eyes and control eyes (R/L) in groups
A, B and C was compared at different time points using one-way
ANOVA. After the comparison, t-test was used between the groups.
P<0.05 was considered to indicate a statistically significant
difference.
Results
Patients treated with LLLT exhibit
favorable postoperative conjunctival healing
Patient information, diagnosis and treatment and
postoperative conjunctival healing data are presented in Table I and clinical manifestations of
conjunctival sac stenosis are depicted in Figs.
1-3. All 10 patients received LLLT on four different occasions.
Observation of conjunctival incision healing at different time
points following laser treatment revealed new blood vessel
formation, granulation tissue hyperplasia, reduced secretion and
relieved conjunctival congestion edema. After 2 weeks post LLLT, it
was observed that the conjunctival incision was fully healed in
patients with moderate conjunctival sac stenosis, whereas complete
healing of the incision in patients with severe conjunctival sac
stenosis was observed at 3 weeks following LLLT. During the
follow-up, the conjunctival wound healing of each group was
assessed, and all incisions were observed to be clean with no
secretions or complications.
 | Table IBasic information, diagnosis,
treatment and conjunctival sac healing at different times after
surgery among 10 patients with conjunctival sac stenosis. |
Table I
Basic information, diagnosis,
treatment and conjunctival sac healing at different times after
surgery among 10 patients with conjunctival sac stenosis.
| Patient basic
information | | Diagnosis and
treatment | Postoperative
conjunctival healing |
|---|
| Patient code | Sex | Age | Pathogeny | Diagnosis and
classification | Operation method | Courses of
irradiation/(week) | 1 week | 2 week | 4 week | 6 week |
|---|
| 01 | Female | 48 | Eye traumas | Recurrent
conjunctival sac stenosis(OD). (severe) | Allograft scleral
transplantation + conjunctiva scar relaxation + conjunctival sac
formation | 3 | The suture was in
place, the conjunctival was slightly edema, the sclera was in
place, and a little secretion was visible. | The peripheral
conjunctival tissue was formed by the formation of new blood
vessels, the granulation tissue was proliferated at the edge of the
implant, and the conjunctival tissue was covered by the implant,
and the secretion was significantly reduced, and the conjunctival
edema was less than before. | In the center, a
small amount of white scleral graft was still visible, with no
edema and no secretions. | The conjunctival
tissue was completely covered in the implant, and the conjunctival
sac incision reached the complete healing state. |
| 02 | Male | 43 | Atrophy of
eyeball | Conjunctival sac
stenosis(OD). (moderate) | Enucleate of ocular
component + hydroxyapatite orbital implants + conjunctiva scar
relaxation + conjunctival sac formation | 2 | The suture was in
place, the conjunctival was slightly edema, the sclera was in
place | The peripheral
conjunctival tissue was formed, and the granulation tissue was
proliferated at the edge of the implant, and the conjunctival
tissue was covered around the implant. | The conjunctival
tissue was completely covered in the implant, and the conjunctival
sac incision reached the complete healing state. | No complications |
| 03 | Male | 10 | Congenital
anophthalmia | Conjunctival sac
stenosis(OD). (severe) | Enucleate of ocular
component + orbital implant + hydroxyapatite orbital implants +
conjunctiva scar relaxation + conjunctival sac formation | 3 | The suture was in
place, the conjunctival was slightly edema, the sclera was in
place. | The peripheral
conjunctival tissue was formed by the formation of new blood
vessels, the granulation tissue was proliferated at the edge of the
implant, and the conjunctival tissue was covered by the implant,
and the secretion was significantly reduced, and the conjunctival
edema was less than before. | In the center, a
small amount of white scleral graft was still visible, and the
conjunctival was not edema | The conjunctival
tissue was completely covered in the implant, and the conjunctival
sac incision reached the complete healing state. |
| 04 | Male | 32 | Alkali burns | Conjunctival sac
stenosis(OS). (severe) | Enucleate of ocular
component + Eyelid ball separation + hydroxyapatite orbital
implants + conjunctiva scar relaxation + conjunctival sac
formation | 3 | The suture was in
place, the conjunctival was slightly edema, the sclera was in
place, and a little secretion was visible. | The peripheral
conjunctival tissue was formed by the formation of new blood
vessels, the granulation tissue was proliferated at the edge of the
implant, and the conjunctival tissue was covered by the implant,
and the secretion was significantly reduced, and the conjunctival
edema was less than before. | In the center, a
small amount of white scleral graft was still visible, with no
edema and no secretions. | The conjunctival
tissue was completely covered in the implant, and the conjunctival
sac incision reached the complete healing state. |
| 05 | Male | 49 | Atrophy of
eyeball | Conjunctival sac
stenosis(OS). (moderate) | Enucleate of ocular
component + hydroxyapatite orbital implants + conjunctiva scar
relaxation | 2 | The suture was in
place, the conjunctival was slightly edema, the sclera was in
place | The peripheral
conjunctival tissue was formed, and the granulation tissue was
proliferated at the edge of the implant, and the conjunctival
tissue was covered around the implant. | The conjunctival
tissue was completely covered in the implant, and the conjunctival
sac incision reached the complete healing state. | No complications |
| 06 | Female | 55 | Atrophy of
eyeball | Conjunctival sac
stenosis(OD). (moderate) | Enucleate of ocular
component + orbital implant + hydroxyapatite orbital implants +
conjunctival flap cover + conjunctival sac formation | 2 | The suture was in
place, the conjunctival was slightly edema, the sclera was in
place | The peripheral
conjunctival tissue was formed, and the granulation tissue was
proliferated at the edge of the implant, and the conjunctival
tissue was covered around the implant. | In the center, a
small amount of white scleral graft was still visible, and the
conjunctival was not edema | No complications |
| 07 | Female | 35 | Traumatic eyeball
removal. | Eye socket without
eyeball (OS); conjunctival sac stenosis(OS). (severe) | Reconstruction of
contracted socket + orbital implant + hydroxyapatite orbital
implants + conjunctival flap cover + conjunctival sac
formation | 3 | The suture was in
place, the conjunctival was slightly edema, the sclera was in
place. | The peripheral
conjunctival tissue was formed by the formation of new blood
vessels, the granulation tissue was proliferated at the edge of the
implant, and the conjunctival tissue was covered by the implant,
and the secretion was significantly reduced, and the conjunctival
edema was less than before. | In the center, a
small amount of white scleral graft was still visible, with no
edema and no secretions. | The conjunctival
tissue was completely covered in the implant, and the conjunctival
sac incision reached the complete healing state. |
| 08 | Male | 18 | Retinoblast- oma | Eye socket without
eyeball (OD); conjunctival sac stenosis(OD). (moderate) | Reconstruction of
contracted socket + orbital implant + hydroxyapatite orbital
implants + conjunctival flap cover + conjunctival sac
formation | 2 | The suture was in
place, the conjunctival was slightly edema, the sclera was in
place | The peripheral
conjunctival tissue was formed, and the granulation tissue was
proliferated at the edge of the implant, and the conjunctival
tissue was covered around the implant. | In the center, a
small amount of white scleral graft was still visible, with no
edema and no secretions. | No complications |
| 09 | Male | 47 | Alkali burns | Recurrent
conjunctival sac stenosis(OD). (severe) | Enucleate of ocular
component + orbital implant + hydroxyapatite orbital implants +
conjunctiva scar relaxation + conjunctival sac formation | 3 | The suture was in
place, the conjunctival was slightly edema, the sclera was in
place, and a little secretion was visible. | The peripheral
conjunctival tissue was formed by the formation of new blood
vessels, the granulation tissue was proliferated at the edge of the
implant, and the conjunctival tissue was covered by the implant,
and the secretion was significantly reduced, and the conjunctival
edema was less than before. | In the center, a
small amount of white scleral graft was still visible, with no
edema and no secretions. | The conjunctival
tissue was completely covered in the implant, and the conjunctival
sac incision reached the complete healing state. |
| 10 | Male | 28 | Eye traumas | Recurrent
conjunctival sac stenosis(OS). (moderate) | Enucleate of ocular
component + hydroxyapatite orbital implants + conjunctiva scar
relaxation + conjunctival sac formation | 2 | The suture was in
place, the conjunctival was slightly edema, the sclera was in
place | The peripheral
conjunctival tissue was formed, and the granulation tissue was
proliferated at the edge of the implant, and the conjunctival
tissue was covered around the implant. | In the center, a
small amount of white scleral graft was still visible, and the
conjunctival was not edema | No complications |
LLLT in a rabbit model demonstrates
favorable postoperative healing following HA implantation
All 30 animals survived the experiments. Following
HA implantation, good conjunctival wound healing was observed with
no secretions and the site was clean. No signs of infection, eye
exposure or other complications were observed. After 8 weeks post
LLLT, normal eye movement was observed.
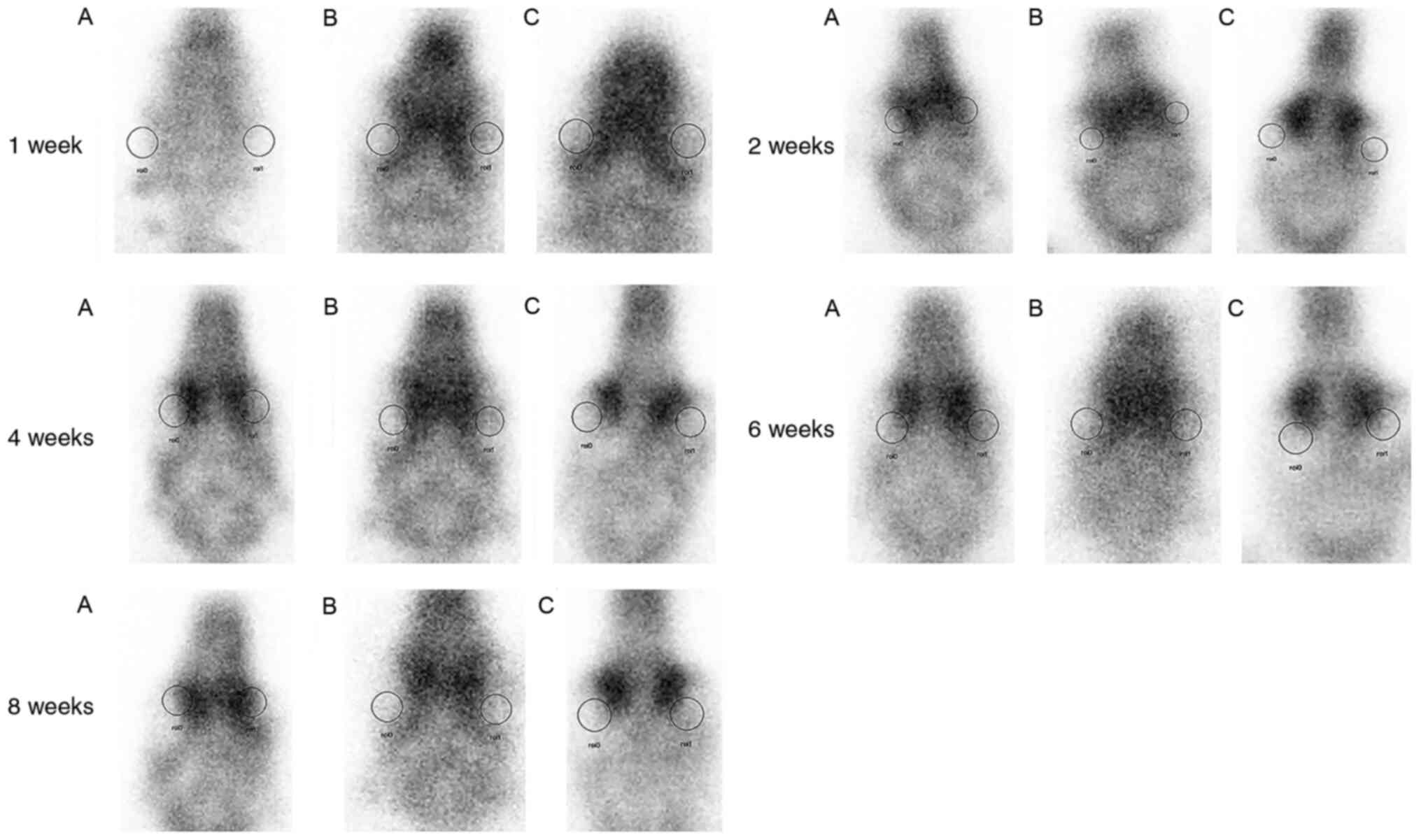
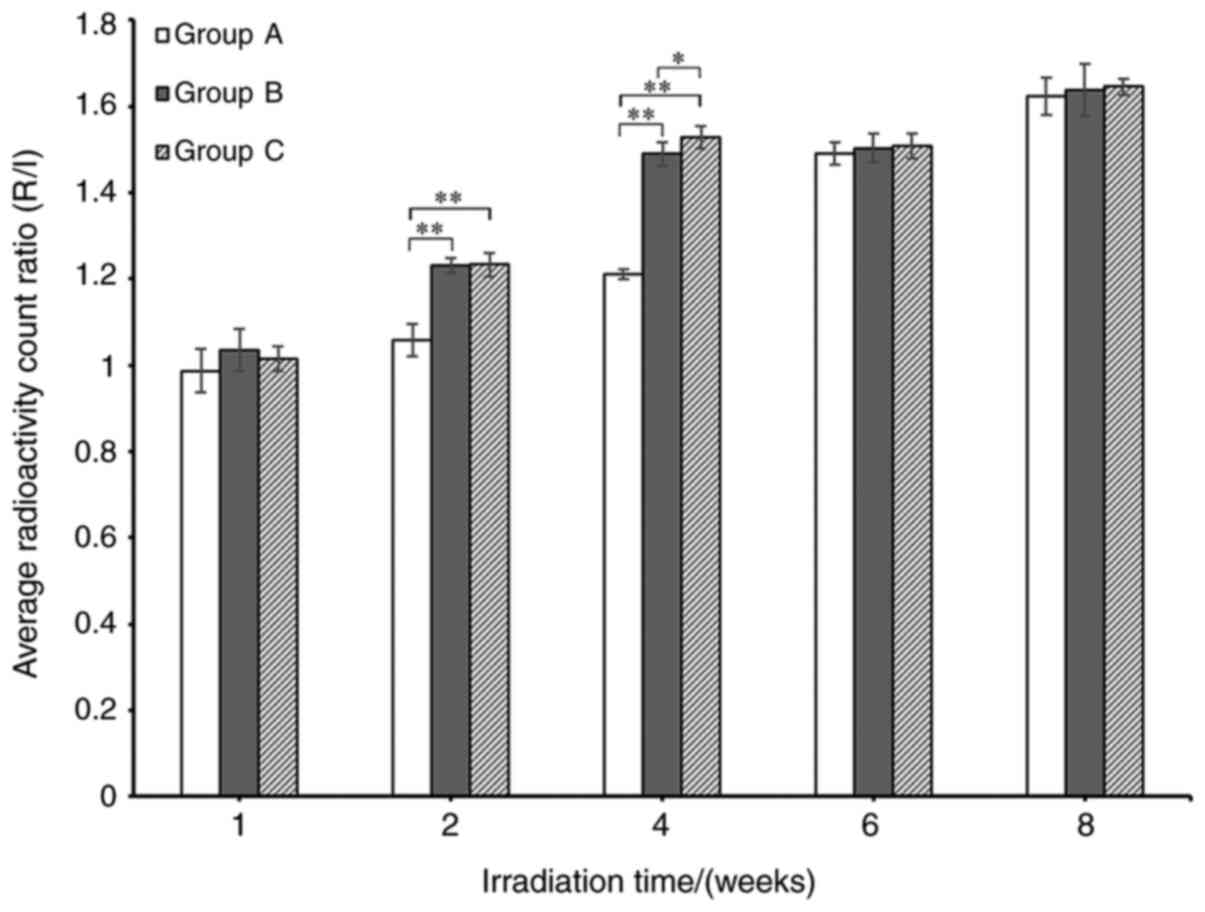
99mTc-MDP imaging in LLLT
treated rabbits increases the radioactivity count ratio in ROI
The average radioactivity count ratio in the ROI was
significantly increased in LLLT groups B and C compared with the
control group A at 1, 2 and 4 weeks post LLLT (P>0.05). There
was no significant difference in the average radioactivity count
ratio in the ROI between groups B and C. In addition, there was no
significant difference in the average radiological count (R/L) in
groups A, B and C at 6 and 8 weeks post-surgery (P<0.05;
Figs. 4 and 6). The average R/L values of LLLT groups B
and C were higher compared with the control group A between 1 and 4
weeks post-surgery, whereas at 6 and 8 weeks, no significant
difference was observed between the 3 groups.
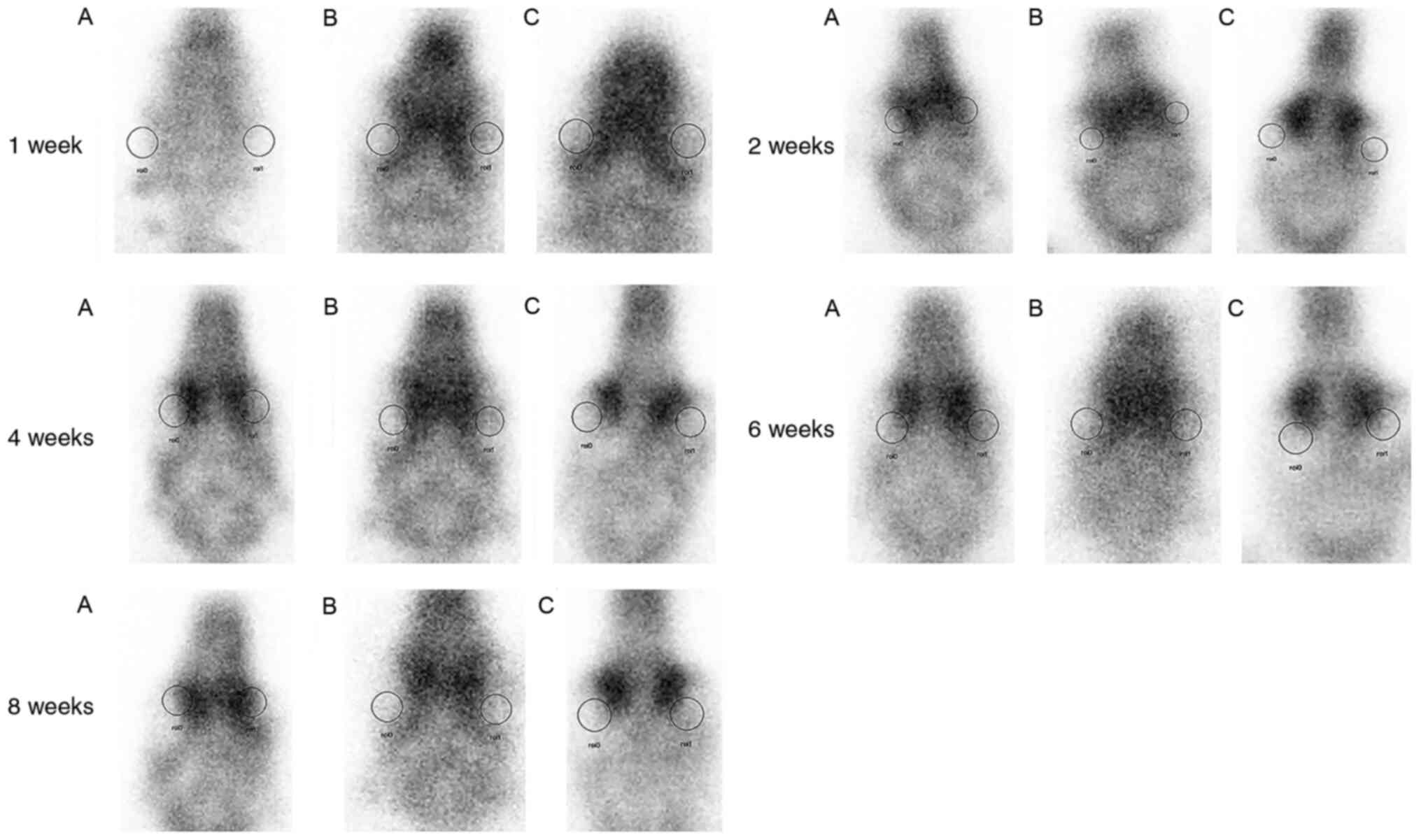 | Figure 4After 1 week post HA orbital
implantation, the average R/L of group B and C was higher compared
with group A. After 2 weeks post HA orbital implantation, the
average R/L of group B and C was higher compared with group A.
After 4 weeks post HA orbital implantation, the average R/L of
group B and C was higher compared with group A. After 6 weeks post
HA orbital implantation, there was no difference detected in
average R/L between 3 groups. After 8 weeks post HA orbital
implantation, there was no significant difference detected in
regard to the average R/L between three groups. HA, hydroxyapatite;
R/L, the average radioactivity count of the region of interest
between surgical (right) and control (left) eyes; group A; control
group underwent right eye removal and HA orbital implantation only
(n=10); group B, underwent right eye removal and HA orbital
implantation followed by one course of LLLT 3 days post-surgery
(n=10); group C, underwent right eye removal and HA orbital
implantation followed by two courses of LLLT with a time interval
of 1 week between treatments starting 3 days post-surgery (n=10);
roi0, region of interest 0; roi1, region of interest 1. |
Histopathological examination of HA
implants in LLLT rabbits demonstrated generation of new
fibrovascular tissue
In the 8th postoperative week, the HA implants were
examined, and the implants were surrounded by fibrovascular
tissues, sclera and inflammatory cells. Sagittal section H&E
staining displayed formation of new fibrovascular tissues in the HA
implants and no obvious inflammatory cell infiltration in LLLT
groups B and C. In the control group A, only new vascular fibrous
tissues were observed around the orbital implants (Fig. 5).
Discussion
The treatment of conjunctival sac stenosis is
difficult; a number of studies have reported the use of variants or
autologous tissue slices for repair, such as autologous sclera,
fascia, conjunctiva, hard palate mucosa, decellularized dermal,
amniotic membrane, temporal shallow artery temporalis fascia island
flap, but cases of postoperative restenosis in the conjunctival sac
and implant exposure continue to be reported (2). Additional factors also contribute to
the complexity of conjunctival sac stenosis, including a lack of
conjunctival epithelial cells around conjunctival epithelial
hyperplasia of the cell division that require repair, with several
patients possessing conjunctival tissues with slow growth rates
post injury. Often, the healing time and high conjunctival surface
tension results in dissolving of the allograft or autograph
phenomenon (3) and loss of
conjunctival tissue carrier support can lead to complete failure
due to postoperative infection.
In the event of extensive conjunctival destruction
caused by conjunctival sac narrowing, treatment is largely limited
to surgery with the severity of stenosis determining the procedure
performed. The primary purpose of treatment is to restore the form
of the patients conjunctival sac. Moderate and severe conjunctival
sac narrowing is commonly caused by chemical injury, burns or other
causes of conjunctival sac of scar contracture and is characterized
by narrowing of the dome, which is often repaired by
transplantation. Previous studies have investigated the use of an
allograft or autograft as a means for conjunctival sac repair;
however, as the transplant can only be used as a basement membrane,
a lack of conjunctival epithelial cell division and proliferation
can extend the conjunctival incision healing time (12). Meanwhile, in cases where the
conjunctival surface tension is increased due to excessive
allograft or autograft dissolution phenomena, exposure of orbital
implants can cause procedure failure (12,13).
In the present study, patients with moderate and
severe conjunctival sac stenosis received a conjunctival sac
scleral graft implantation and HA implants to fill the eye socket
and to restore conjunctival sac form. HA is a commonly used filling
material and its clinical application has permitted rapid
development in orbital plastic surgery. The porous structure of HA
is beneficial for the growth of vascular fibers and rapid
vascularization is the basis of successful orbital implantation. In
the present study, LLLT was performed post-surgery to promote the
biological effects of wound healing and to observe its clinical
therapeutic effect on conjunctival sac stenosis. The results showed
that the local inflammatory symptoms after treatment were
significantly reduced. The use of LLLT can stimulate conjunctival
blood vessels around the wound, increase the speed of local fascia
tissue formation and vascularization, promote conjunctival
epithelial cell growth to cover the surface of the implant, promote
faster wound healing and thus reduce postoperative follow-up
complications.
In the present study, LLLT was employed for adjuvant
treatment following application of the regular operation method and
the mechanism underlying promotion of tissue healing and the
accompanying curative effects have been previously reported
(14). Hornig et al
(15) demonstrated that LLLT
promoted tissue healing by stimulating fibroblast activity, whereas
de Araújo et al (16)
investigated the effects of He-Ne laser irradiation on wound
healing in mice demonstrating wound inflammation relief,
accelerated fibroblast activation and an increased number of
collagen fibers in irradiated areas. A previous study utilized LLLT
on traumatic tympanic membrane perforation and demonstrated that
LLLT influenced wound healing by inducing changes in tympanic
membrane proliferation activity, increasing squamous cell
hyperplasia, cell migration and fibroblast proliferation as well as
increasing vascularization and this study concluded that the use of
LLLT increased matrix and collagen synthesis and promoted fibrous
tissue regeneration, ultimately reducing the healing time post
tympanic membrane perforations (17).
Based on previous studies and the results obtained
in the present study, it was concluded that LLLT can be applied as
a postoperative adjuvant therapy to promote healing, improve graft
survival and conjunctival incision healing in patients with
conjunctival sac stenosis. The mechanisms underlying these
favorable postoperative outcomes may include: Promotion of
conjunctival epithelial cell proliferation and migration, thus
accelerating plant of conjunctival tissue to center around the
crawling; promotion of local microcirculation; promotion of
absorption of exudate in the human body and alleviation of
inflammation, stimulating fibroblast proliferation and collagen
formation beneficial for tissue repair and wound healing; and
promotion of vascularization of the HA implant. In the present
study, the influence of LLLT on the vascularization of the HA
implant was widely observed. The results of animal experiments
demonstrated that there were numerous new fibrous vascular tissues
formed around the eye seat of implant, sclera shell and the eye
muscle attachment and the surface of the sphere could be observed
in the perforation of the fiber vessels. Radionuclide scanning also
revealed that vascularization in the prosthetic eye following LLLT
was faster compared with the control group. Overall, it was found
that LLLT promotes the success of conjunctival grafts and
conjunctival incision healing in patients with conjunctival sac
stenosis. In addition, LLLT significantly promotes the early
vascularization of HA implants. However, further investigation to
resolve the underlying mechanism of LLLT promoting tissue healing,
prevention and the control of ocular surface exposure
postoperatively in patients with conjunctival sac stenosis is
required to further validate the findings of the present study.
Acknowledgements
Not applicable.
Funding
This research was supported by the Jiangxi
Provincial Key R& D Program (20181BBG70007) and the Jiangxi
Natural Science Foundation Project (20181BAB205035).
Availability of data and materials
The datasets used and/or analyzed during the present
study are available from the corresponding author on reasonable
request.
Authors' contributions
QX and YL performed experiments, data collation and
analysis, and writing the manuscript and modification of the study.
YJ and YL together completed the animal experimental part of the
manuscript, including the experimental process of animal feeding,
animal surgery and tissue section processing so YJ as the second
author of the article. HL designed the study, performed the
surgeries and revised the manuscript.
Ethical approval and consent to
participate
The study protocol was approved by The Affiliated
Eye Hospital of Nanchang University Ethics Committee (Nanchang,
China). All participating patients provided informed written
consent documentation prior to inclusion in the present study.
Patient consent for publication
Patients or patients’ guardians provided consent for
the publication of images in the present study.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Hong Y, Xu GX and Chen SD: Hydroxyapatite
orbital implantation combined with united skin grafting for
eye-socked depression with III° conjunctival sac stenosis,
2008.
|
|
2
|
Kolli S, Ahmad S, Lako M and Figueiredo F:
Successful clinical implementation of corneal epithelial stem cell
therapy for treatment of unilateral limbal stem cell deficiency.
Stem Cells. 28:597–610. 2010.PubMed/NCBI View
Article : Google Scholar
|
|
3
|
Li D, Jie Y, Liu H, Liu J, Zhu Z and Mao
C: Reconstruction of anophthalmic orbits and contracted eye sockets
with microvascular radial forearm free flaps. Ophthalmic Plast
Reconstr Surg. 24:94–97. 2008.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Tuby H, Maltz L and Oron U: Implantation
of low-level laser irradiated mesenchymal stem cells into the
infarcted rat heart is associated with reduction in infarct size
and enhanced angiogenesis. Photomed Laser Surg. 27:227–233.
2009.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Corazza AV, Jorge J, Kurachi C and Bagnato
VS: Photobiomodulation on the angiogenesis of skin wounds in rats
using different light sources. Photomed Laser Surg. 25:102–106.
2007.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Pinheiro AL, Meireles GC, de Barros Vieira
AL, Almeida D, Carvalho CM and dos Santos JN: Phototherapy improves
healing of cutaneous wounds in nourished and undernourished Wistar
rats. Braz Dent J. 15:SI21–SI28. 2004.PubMed/NCBI
|
|
7
|
Ankri R, Lubart R and Taitelbaum H:
Estimation of the optimal wavelengths for laser-induced wound
healing. Lasers Surg Med. 42:760–764. 2010.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Correa F, Lopes Martins RA, Correa JC,
Iversen VV, Joenson J and Bjordal JM: Low-level laser therapy (GaAs
lambda=904 nm) reduces inflammatory cell migration in mice with
lipopolysaccharide-induced peritonitis. Photomed Laser Surg.
25:245–249. 2007.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Mesquita-Ferrari RA, Martins MD, Silva JA
Jr, da Silva TD, Piovesan RF, Pavesi VC, Bussadori SK and Fernandes
KP: Effects of low-level laser therapy on expression of TNF-α and
TGF-β in skeletal muscle during the repair process. Lasers Med Sci.
26:335–340. 2011.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Bossini PS, Fangel R, Habenschus RM, Renno
AC, Benze B, Zuanon JA, Neto CB and Parizotto NA: Low-level laser
therapy (670 nm) on viability of random skin flap in rats. Lasers
Med Sci. 24:209–213. 2009.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Chen Q: Establishing and studying the
model of posterior capsule opacification in rabbits. Compilation of
the 9th Central and Southern Region Experimental Animal Science and
Technology Exchange Conference, pp1016-1021, 2009.
|
|
12
|
Gu J, Zhai J, Liao G and Chen J: Boston
type I keratoprosthesis implantation following autologous
submandibular gland transplantation for end stage ocular surface
disorders. Ocul Immunol Inflamm. 26:452–455. 2018.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Liu DY: Clinical analysis of 129 cases of
traumatic conjunctival sac stenosis. J Ocul Injury Occup
Ophthalmol. 32:770–771. 2010.
|
|
14
|
Nie YH, Xing YQ, Guo Y and Zhu J: Analysis
on the causes and management of exposure of orbital hydroxyapatite
implants. Recent Adv Ophthalmol, 2006-09.
|
|
15
|
Hornig C, Barleon B, Ahmad S, Vuorela P,
Ahmed A and Weich HA: Release and complex formation of soluble
VEGFR-1 from endothelial cells and biological fluids. Lab Invest.
80:443–454. 2000.PubMed/NCBI View Article : Google Scholar
|
|
16
|
de Araújo CE, Ribeiro MS, Favaro R, Zezell
DM and Zorn TM: Ultrastructural and autoradiographical analysis
show a faster skin repair in He-Ne laser-treated wounds. J
Photochem Photobiol B. 86:87–96. 2007.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Shen Y, Fang C, Huang Y, Li Z, Xue Z and
Li Y: Effects of low-power semiconductor laser irradiation on
healing of tympanic membrane perforations of guinea pigs. Chin J
Laser Med Surg. 7:386–392. 2008.(In Chinese).
|