Introduction
Coronary artery calcification is an integral process
in atherogenesis, occurring in ≥90% of men and ≥67% of women >70
years of age (1). The pathogenesis
of coronary calcification shares common pathways with bone
formation, and eventually results in reduced vascular compliance,
abnormal vasomotor responses and impaired myocardial perfusion.
Calcified lesions are often harder to traverse and dilate, which
pose higher risks of suboptimal stent deployment, angiographic
complications and procedural failure (2). Coronary calcification presents a
great challenge for percutaneous coronary intervention (PCI) and
has an adverse impact on stent expansion and immediate treatment
efficacy (3). The presence of
calcified lesions strongly predicts the occurrence of stent
thrombosis within a year of PCI and target lesion revascularization
(4). Therefore, it is necessary to
apply different approaches where calcified plaques are involved,
prior to stent implantation, to achieve successful expansion.
Optical coherence tomography (OCT) utilizes
near-infrared light directed at the vessel wall through a rotating
single optical fiber coupled with an imaging lens within a
short-monorail imaging sheath (5).
By measuring the amplitude and time delay of the backscattered
light, OCT generates high-resolution, cross-sectional and
three-dimensional volumetric images of the coronary microstructure,
which is an emerging intracoronary imaging modality that has been
documented to accurately identify calcified lesions whilst also
assessing the severity of calcification (6). A recent study reported that
OCT-guided PCI for calcified lesions resulted in improved stent
expansion (7). Furthermore, Fujino
et al (8) showed that
maximum calcium angle, maximum calcium thickness and calcium length
were independent predictors of stent underexpansion, and
demonstrated that calcium lesions with a maximum angle of >180˚
(defined as 2 points), a maximum thickness of >0.5 mm (1 point)
and a length >5 mm (1 point) may be at risk of stent
underexpansion in patients with relatively mild calcification. It
was also revealed that the lesions with calcium score of 0 to 3 had
excellent stent expansion, whereas the lesions with a score of 4
had stent underexpansion. However, whether this previously
established OCT-based scoring system can be applied to patients
with moderate and severe calcified lesions remains unclear.
Therefore, the present study aimed to develop a novel scoring
system for the prediction of stent underexpansion in patients with
moderate and severe calcified lesions.
Materials and methods
Study population
A total of 78 patients aged 18-90 years old (68.1%
male) were screened for the present study. These patients were
diagnosed with moderate or severe calcified coronary lesions using
coronary angiography or OCT and underwent OCT-guided stent
implantation at Peking University People's Hospital (Beijing,
China) between January 2016 and July 2021. The degree of
calcification on coronary angiography was classified according to
the Mintz criteria (9). The lesion
was considered to be moderate or severe calcified lesion on OCT if
it had multiple complex calcium imaging features, such as a maximum
calcium length >5 mm, a thickness >0.5 mm or an arc >180˚.
The exclusion criteria were as follows: i) Lack of pre-procedure or
post-stent OCT images; ii) in-stent restenosis and chronic total
coronary artery occlusion; iii) incomplete OCT images, in which
critical parameters could not be analyzed or quantified; and iv)
poor image quality.
Study design
The present retrospective study aimed to develop a
novel OCT-based calcium scoring system to predict stent
underexpansion in moderate and severe calcified lesions. Medical
records, including coronary angiography and OCT images, of the
eligible patients were reviewed. The patient demographic
information, clinical manifestation, past medical history, family
history of coronary heart disease, laboratory examinations and PCI
procedural characteristics were recorded. The present study was
approved by the Ethics Committee of Peking University People's
Hospital (Beijing, China; approval no. 2018PHB154-01) and was
performed according to the principles of The Declaration of
Helsinki.
PCI procedure and OCT imaging data
acquisition
Coronary angiography and stent implantation were
performed according to the standard protocols. Angiographic images
were recorded using 5-6F angiographic imaging catheter or guiding
catheter at 15 frames/sec by radiographic systems (Innova IGS 530,
GE Medical Systems; Azurion7 M12, Philips Healthcare). Angiographic
image runs at all standard projection views for each vessel were
saved. The contrast medium was injected manually at a constant
speed of approximately 4 ml/sec until the distal vessel was filled.
OCT imaging data were acquired using frequency-domain OCT
(C7-XR™ or OPTIS™) and the Dragonfly™ Duo
catheter (all purchased from Abbott Vascular; Abbott Pharmaceutical
Co., Ltd.). After administration of intracoronary nitroglycerin,
the Dragonfly™ Duo catheter was carefully advanced
distal to the target lesion under fluoroscopic guidance. Then an
automatic pullback OCT imaging was performed at a rate of 18 mm/sec
(HD mode) or 36 mm/sec (S mode) throughout the entire lesion.
During the session, contrast medium was flushed continuously with
an injection rate of >5 ml/sec for the left coronary artery and
>4 ml/sec for the right coronary artery depending on the vessel
size. Based on the angiographic and OCT results, the decision of
whether to perform rotational atherectomy (RA) or conventional
angioplasty through cutting, scoring or using a non-compliant
balloon prior to stent implantation was dependent on the discretion
and skill of the surgeon. Briefly, in the presence of a multitude
of complex calcium imaging features observable on the OCT image, an
aggressive strategy of active RA was utilized followed by balloon
angioplasty. Otherwise, the surgeon would first attempt a balloon
angioplasty, followed by the RA procedure promptly in cases of
inadequate balloon dilation. In cases of optimal balloon dilation
or the apparent formation of a calcium crack (indicating adequate
preparation of calcified lesions) after dilation on the OCT image,
the stent would be implanted directly without the use of RA.
Quantitative coronary angiography
(QCA) analysis
All angiography images were analyzed using the
QAngio® XA software (version 7.3; Medis Medical Imaging
Systems B.V.) by two independent interventional cardiologists (YM
and QL), who were blinded to the clinical presentation and OCT
results of the patients. The location, angulation and length of the
calcified lesions, reference vessel diameter, minimum lumen
diameter and diameter stenosis of the target lesions were
assessed.
OCT imaging analysis
All OCT data were analyzed using Off-line Review
Workstation software (version E.0.2; Abbott Vascular; Abbott
Pharmaceutical Co., Ltd.) and based on procedures/guidelines
described in dedicated expert consensus reports (10,11).
This analysis was performed by two independent interventional
cardiologists (YM and QL) who were blinded to the clinical and
angiographic patient information.
In the present study, only lesions with a calcium
arc ≥30˚ were included. Lesions were considered to be two separate
calcified lesions if there was >1 mm of non-calcified plaque
between the two. If the boundary of the calcified lesions was not
obvious, then the maximum visible thickness would be quantified.
Superficial calcification would be defined if the distance between
the lesion and the lumen was <100 µm. Stent edge dissection was
defined as the interruption of surface continuity at the stent edge
(within 5 mm distal and proximal to the stent). Stent malapposition
would be defined if the longitudinal distance from the stent
surface to the lumen was greater than the stent thickness, whereas
tissue protrusion would be defined if there was protrusion of the
tissue into the lumen following stent implantation. The percentage
of stenosis area and diameter were defined as the minimum lumen
area/mean reference lumen area and the mean lumen diameter at the
narrowest site/mean reference lumen diameter, respectively. The
stent expansion percentage was calculated as the minimum stent
area/mean reference vessel area x100. According to the determined
stent expansion, patients were divided into the adequate (stent
expansion ≥80%) and poor (stent expansion <80%) stent expansion
groups (11,12).
Statistical analysis
Statistical analysis was performed using the SPSS
software (version 24.0; IBM Corp.). Categorical variables are
presented as n (%) and were compared using either the χ2
or Fisher's exact tests, as appropriate. The Shapiro-Wilk test was
performed to examine the normality of distribution. Continuous
variables with a normal distribution are presented as the mean ±
standard deviation or are otherwise presented as the median and
interquartile range. These variables were statistically compared
using the unpaired Student's t-test or Mann-Whitney U test, as
appropriate. Subsequently, the univariate logistic regression model
was built and variables with P<0.10 were included in the
multivariate logistic regression model with a step-wise algorithm.
The maximum calcium length factor, which was deemed to be
clinically relevant, also entered into the multivariate analysis.
Significant variables were then included into the final calcium
scoring system. Similar to the method of risk score establishment
proposed in the Framingham Study, a novel calcium scoring system
was developed by assigning weighted points for each variable
(13). Receiver operating
characteristic (ROC) curve analysis was performed to determine the
optimal cut-off value for the novel scoring system for the
prediction of stent underexpansion. The area under the curve (AUC)
of the novel scoring system was compared with that proposed by
Fujino et al (8) using the
χ2 test for two associated ROC curves. The
inter-observer agreements for the OCT data were assessed by
determining the intraclass correlation coefficients (ICC).
P<0.05 (two-sided) was considered to indicate a statistically
significant difference.
Results
Clinical and procedural
characteristics
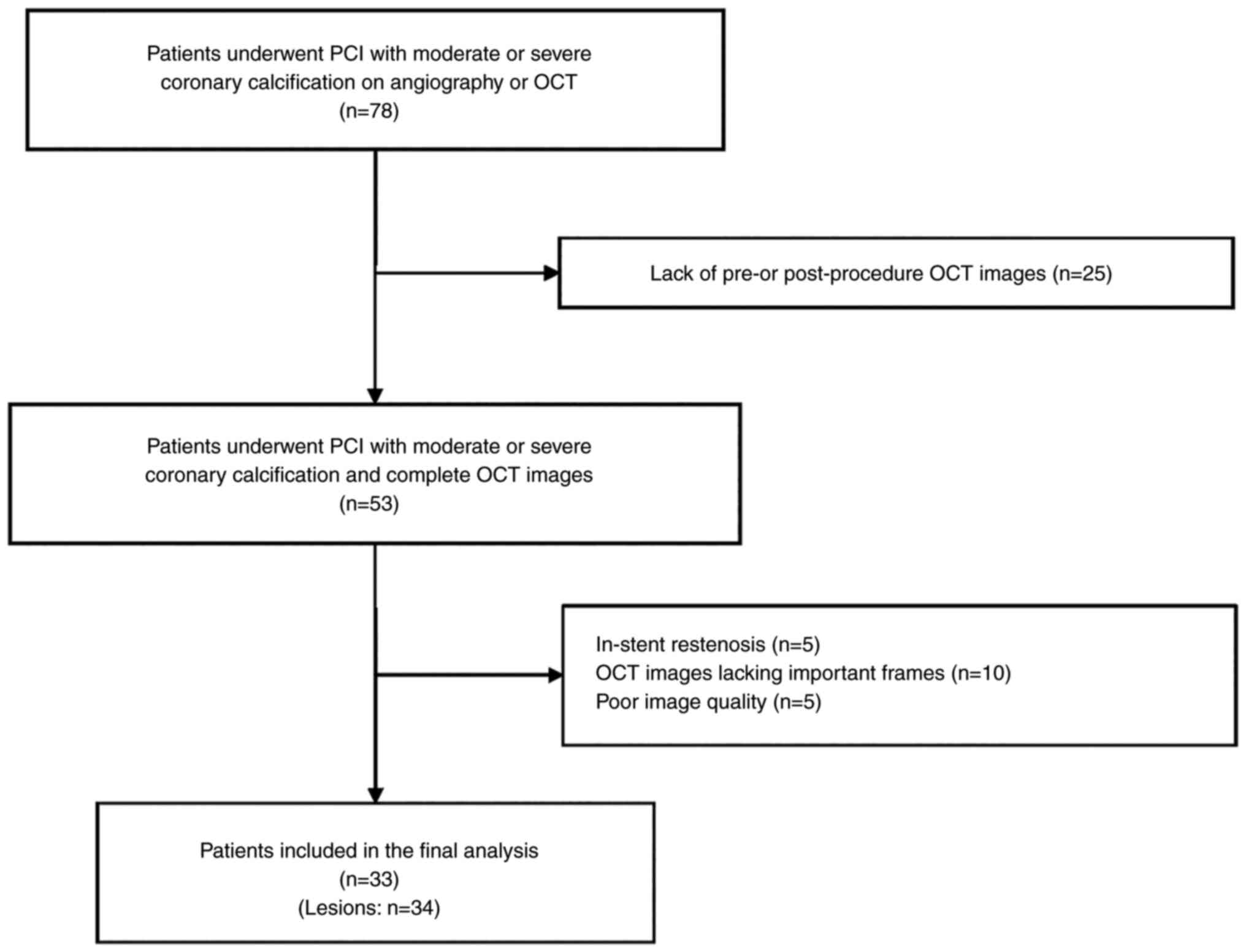
After excluding 25 patients due to paucity of
pre-procedure or post-stent OCT images, a total of 53 patients with
moderate or severe calcified lesions, identified using coronary
angiography or OCT, who underwent stent implantation with the
guidance of OCT and had complete OCT images, were included into the
present study. Among these patients, 33 (34 lesions) were finally
included according to the aforementioned exclusion criteria
(Fig. 1).
The mean age of the patients was 67±10 years and 20
of the patients were male. Furthermore, 23 (69.7%) patients had
coexisting hypertension and 25 (75.8%) had hyperlipidemia. Of all
33 patients, 7 (21.2%) were diagnosed with stable angina pectoris,
whereas 26 (78.8%) had acute coronary syndrome. Poor stent
expansion occurred in 22 patients (23 lesions). The patients in the
poor stent expansion group were significantly older compared with
those in the adequate stent expansion group (70±10 vs. 59±8 years,
respectively; P=0.003). In addition, the estimated glomerular
filtration rate was significantly lower in the poor stent expansion
group compared with that in the adequate stent expansion group
(82.16 vs. 93.95; P=0.036; Table
I). No significant difference was observed between the two
groups with regards to the remaining clinical characteristics
(Table I).
 | Table IClinical characteristics of the
patients. |
Table I
Clinical characteristics of the
patients.
| Variables | Poor stent expansion
(n=22) | Adequate stent
expansion (n=11) | P-value |
|---|
| Age, years | 70±10 | 59±8 | 0.003 |
| Male, n (%) | 12 (54.5) | 8 (72.7) | 0.456 |
| Body mass index,
kg/m2 | 25.91±3.80 | 25.08±1.58 | 0.496 |
| Hypertension, n
(%) | 16 (72.7) | 7 (63.6) | 0.696 |
| Diabetes, n
(%)a | 10 (45.5) | 4 (36.4) | 0.719 |
| Hyperlipidaemia, n
(%) | 16 (72.7) | 9 (81.8) | 0.687 |
| Chronic kidney
disease, n (%)a | 2 (9.1) | 1 (9.1) | >0.999 |
| Smoking, n (%) | 8 (36.4) | 6 (54.5) | 0.534 |
| Family history of
coronary heart disease, n (%)a | 4 (18.2) | 5 (45.5) | 0.121 |
| Prior percutaneous
coronary intervention, n (%)a | 8 (36.4) | 4 (36.4) | >0.999 |
| Clinical diagnosis, n
(%)a | | | >0.999 |
|
Stable
angina | 5 (22.7) | 2 (18.2) | |
|
Unstable
angina | 13 (59.1) | 7 (63.6) | |
|
Acute
myocardial infarction | 4 (18.2) | 2 (18.2) | |
| Left ventricular
ejection fraction, % | 69.03±5.71 | 66.32±6.04 | 0.298 |
| Low density
lipoprotein-cholesterol, mmol/l | 2.06±0.77 | 2.06±0.53 | 0.992 |
| Fasting plasma
glucose, mmol/l | 5.08
(4.52-5.58) | 5.07
(4.72-6.10) | 0.620 |
| Estimated
glomerular filtration rate, ml/min/1.73 m2 | 82.16
(71.37-93.25) | 93.95
(90.52-104.00) | 0.036 |
RA was performed in the modification of 19 (55.9%)
lesions. Furthermore, 13 (38.2%) lesions were treated with scoring
whereas 13 (38.2%) were treated with a non-compliant balloon prior
to stent deployment. The median number of stents implanted was two
and the median total length of stents was 44 mm. Compared with that
in patients in the adequate stent expansion group [2 (18.2%)], the
rate of RA performed during PCI was significantly higher in the
patients in the poor stent expansion group [17 (73.9%); P=0.003;
Table II]. There was no
significant difference regarding the usage of balloons and stents
between the two stent expansion groups (Table II).
 | Table IIProcedural characteristics of the
lesions. |
Table II
Procedural characteristics of the
lesions.
| Variables | Poor stent
expansion (n=23)a | Adequate stent
expansion (n=11)a | P-value |
|---|
| Scoring balloon, n
(%)b | 11 (47.8) | 2 (18.2) | 0.245 |
|
Maximum
pressure, atm | 14.00
(11.00-15.00) | 12.00
(12.00-12.00) | 0.545 |
|
Maximum
diameter, mm | 2.75
(2.50-2.88) | 2.50
(2.38-2.62) | 0.351 |
| Non-compliant
balloon, n (%)b | 11 (47.8) | 2 (18.2) | 0.245 |
|
Maximum
pressure, atm | 18.00
(17.00-24.00) | 13.50
(12.75-14.25) | 0.091 |
|
Maximum
diameter, mm | 2.50
(2.50-2.50) | 2.25
(2.12-2.38) | 0.098 |
| Semi-compliant
balloon, n (%) | 18 (78.3) | 8 (72.7) | >0.999 |
|
Maximum
pressure, atm | 16.00
(14.00-16.00) | 15.00
(13.50-16.50) | 0.686 |
|
Maximum
diameter, mm | 2.50
(2.12-2.50) | 2.50
(2.38-2.50) | 0.885 |
| RA, n
(%)b | 17 (73.9) | 2 (18.2) | 0.003 |
|
No. of RA
proceduresb | 5 (3-7) | 5 (4-5) | 0.893 |
|
Maximum burr
size, mm | 1.50
(1.38-1.50) | 1.50
(1.50-1.50) | 0.725 |
|
Speed of
burr, x104 r/min | 15.00
(15.00-16.00) | 16.60
(15.90-17.30) | 0.212 |
| Stent | | | |
|
Number of
stentsb | 2 (1-3) | 1 (1-2) | 0.126 |
|
Total stent
length, mm | 48.00
(37.50-69.00) | 32.00
(28.00-57.00) | 0.197 |
|
Maximum
diameter, mm | 3.00
(2.75-3.00) | 2.75
(2.50-3.00) | 0.165 |
Imaging analysis of the calcified
plaques
The majority of patients had multi-vessel disease.
The target lesions were mainly located in the left anterior
descending artery. The prevalence of moderate and severe coronary
calcification as assessed by angiography was up to 88.2% (30
lesions). All parameters of QCA analysis, including target vessel,
degree of calcification, angulation of lesions, calcium length,
minimum lumen diameter, minimum stent diameter and reference vessel
diameter were comparable between the two stent expansion groups
(Table III).
 | Table IIIQuantitative coronary angiography
analyses of calcified lesions. |
Table III
Quantitative coronary angiography
analyses of calcified lesions.
| A,
Pre-procedure |
|---|
| Variables | Poor stent
expansion (n=23)a | Adequate stent
expansion (n=11)a | P-value |
|---|
| Multivessel
disease, n (%) | 19 (82.6) | 11 (100.0) | 0.280 |
| Target vessel, n
(%)b | | | >0.999 |
|
Left
anterior descending | 19 (82.6) | 9 (81.8) | |
|
Left
circumflex | 1 (4.3) | 0 (0.0) | |
|
Right
coronary artery | 3 (13.0) | 2 (18.2) | |
| Degree of
calcification, n (%)b | | | 0.362 |
|
None or
mild | 2 (8.7) | 2 (18.2) | |
|
Moderate | 14 (60.9) | 8 (72.7) | |
|
Severe | 7 (30.4) | 1 (9.1) | |
| Bifurcation, n
(%)b | 2 (8.7) | 4 (36.4) | 0.070 |
| Angulation, n
(%)b | | | 0.203 |
|
≤90˚ | 22 (95.7) | 10 (90.9) | |
|
>90˚ | 1 (4.3) | 1 (9.1) | |
| Calcium length,
mm | 35.77±20.66 | 26.03±12.34 | 0.227 |
| RVD, mm | 2.63
(2.38-2.83) | 2.54
(2.32-2.64) | 0.597 |
| Minimum lumen
diameter, mm | 1.24±0.42 | 1.33±0.33 | 0.579 |
| Diameter stenosis,
% | 53.43±13.27 | 48.02±12.92 | 0.290 |
| B,
Post-procedure |
| Variables | Poor stent
expansion (n=23)a | Adequate stent
expansion (n=11)a | P-value |
| RVD, mm | 2.39
(2.12-2.53) | 2.50
(2.26-2.94) | 0.155 |
| Minimum stent
diameter, mm | 2.19
(2.02-2.44) | 2.33
(2.02-2.74) | 0.382 |
| Diameter stenosis,
% | 11.58
(6.45-15.02) | 10.71
(6.80-15.51) | 0.887 |
There were high levels of similarity between the two
observers for the interpretation of the OCT images and the
assessment of the maximum calcium arc (ICC=0.877), thickness
(ICC=0.874) and length (ICC=0.968) (data not shown). The lesions
all manifested as superficial calcifications, with a median maximum
calcium arc of 230˚, median maximum calcium length of 25.10 mm and
an average maximum calcium thickness of 1.18 mm. The overall final
post-PCI median stent expansion was 70.74%. Furthermore, the
maximum calcium arc (299 vs. 142˚; P=0.001; Table IV) and thickness (1.24 vs. 1.04
mm; P=0.029; Table IV) were
significantly larger in the poor stent expansion group compared
with those in the adequate expansion group, whereas the pre-stent
diameter stenosis determined using OCT was significantly lower
(52.76 vs. 66.29%; P=0.038; Table
IV). The proportion of stent malapposition was significantly
higher in the poor stent expansion group compared with that in the
adequate stent expansion group (60.9 vs. 9.1%; P=0.011; Table IV), whereas the mean stent
expansion was significantly lower in the poor stent expansion group
(63.39±12.72 vs. 86.10±4.59%; P<0.001; Table IV).
 | Table IVOptical coherence tomography data of
calcified lesions. |
Table IV
Optical coherence tomography data of
calcified lesions.
| A, Pre-stent |
|---|
| Variables | Poor stent
expansion (n=23)a | Adequate stent
expansion (n=11)a | P-value |
|---|
| Superficial
calcium, n (%) | 23(100) | 11(100) | - |
| Maximum calcium
length, mm | 33.15
(15.62-40.20) | 20.65
(14.78-25.10) | 0.094 |
| Maximum calcium
arc, degree | 299 (205-345) | 142 (104-216) | 0.001 |
| Maximum calcium
thickness, mm | 1.24±0.23 | 1.04±0.25 | 0.029 |
| Minimum lumen area,
mm2 | 1.64
(1.16-2.28) | 2.26
(1.65-2.71) | 0.217 |
| Reference vessel
area, mm2 | 6.47
(5.08-8.20) | 5.30
(5.11-6.92) | 0.429 |
| Diameter stenosis,
% | 52.76
(45.59-58.58) | 66.29
(55.66-71.74) | 0.038 |
| Area stenosis,
% | 81.73
(80.06-83.37) | 84.11
(82.44-86.80) | 0.063 |
| B, Post-stent |
| Variables | Poor stent
expansion (n=23)a | Adequate stent
expansion (n=11)a | P-value |
| Tissue prolapse, n
(%)b | 1 (4.3) | 0 (0) | >0.999 |
| Stent edge
dissection, n (%) | 0 (0) | 0 (0) | - |
| Stent
malapposition, n (%)b | 13 (60.9) | 1 (9.1) | 0.011 |
| Minimum stent area,
mm² | 4.25
(3.96-5.62) | 5.42
(4.60-6.77) | 0.146 |
| Reference vessel
area, mm2 | 8.02
(6.43-9.09) | 5.90
(5.33-8.64) | 0.217 |
| Stent expansion,
% | 63.39±12.72 | 86.10±4.59 | <0.001 |
Development of the novel calcium
scoring system and comparisons with the previous scoring
system
In the univariate analysis, age, maximum calcium arc
and diameter stenosis were found to be significant predictors of
stent underexpansion (P<0.05). Age [odds ratio (OR), 1.173; 95%
CI, 1.036-1.438; P=0.042] and maximum calcium arc (OR, 1.023; 95%
CI, 1.008-1.050; P=0.021) were demonstrated to be independent
predictors of stent underexpansion in the multivariate logistic
regression model (Table V). A
novel calcium scoring system was established as follows: (0.16 x
age) + (0.03 x maximum calcium arc), with the points of each
variable assigned based on β-coefficients in the aforementioned
multivariate analysis. In order to simplify the model and
facilitate the calculation, each β-coefficient was rounded from
0.159 to 0.16, and from 0.023 to 0.03.
 | Table VUnivariate and multivariate logistic
regression model of stent underexpansion. |
Table V
Univariate and multivariate logistic
regression model of stent underexpansion.
| A, Univariate
analysis |
|---|
| Variables | β-coefficient | Odds ratio | 95% CI | P-value |
|---|
| Age, years | 0.133 | 1.143 | 1.044-1.297 | 0.013 |
| Maximum calcium
arc, degree | 0.019 | 1.019 | 1.008-1.035 | 0.004 |
| Diameter stenosis,
% | -0.063 | 0.939 | 0.872-0.988 | 0.048 |
| B, Multivariate
analysis |
| Variables | β-coefficient | Odds ratio | 95% CI | P-value |
| Age, years | 0.159 | 1.173 | 1.036-1.438 | 0.042 |
| Maximum calcium
arc, degree | 0.023 | 1.023 | 1.008-1.050 | 0.021 |
Subsequently, the optimal threshold for the
prediction of stent underexpansion was identified using ROC curve
analysis. The optimal cut-off value for the scoring system was
determined to be 16.87 (sensitivity, 0.870; specificity, 0.909;
AUC, 0.925; 95% CI, 0.836-1.014; P<0.001; Fig. 2). Representative OCT images are
presented in Fig. 3. The
pre-procedure OCT image of a 67-year-old patient showed severe
coronary calcification with a maximum calcium arc of 290˚ at the
narrowest site. The calculated calcium score of the lesion was
19.42 according to the novel calcium scoring system, which
predicted the occurrence of stent underexpansion. The final
post-stent OCT image indicated poor stent expansion as anticipated
with a minimum stent area of 4.38 mm2.
A previous calcium scoring system developed by
Fujino et al (8) was also
applied, whereby the corresponding score for each patient was
calculated before ROC curve analysis was performed to investigate
the efficacy for the prediction of poor stent expansion. Compared
with that of the Fujino et al (8) scoring system, the novel system in the
present study, which incorporated age and the maximum calcium arc,
was found to be superior for the prediction of stent underexpansion
in the present study population, with a significantly larger AUC
for the ROC analysis (0.925 vs. 0.706, respectively; P=0.002;
Fig 2).
Discussion
The present study established a novel scoring system
to effectively predict stent underexpansion in moderate and severe
calcified lesions. The procedural characteristics and intracoronary
imaging data of patients with moderate and severe coronary
calcification who had undergone PCI were retrospectively analyzed.
The main findings of the present study were as follows: i) The
maximum calcium arc of lesions and patient age were independent
predictors of stent underexpansion in patients with moderate and
severe coronary calcification; and ii) the calcium scoring system
based on these parameters may accurately predict the risk of stent
underexpansion and guide the strategy of lesion modification, such
as RA, in patients with moderate and severe coronary
calcification.
It has previously been reported that the occurrence
of stent underexpansion is increased in patients with severe
calcified lesions, where incomplete stent expansion is known to be
a common risk factor for stent thrombosis and in-stent restenosis
(14-16).
Severe coronary calcification is also an independent predictor of
poor prognosis and increases the mortality rate (10.8 vs. 4.4%;
P<0.001) or 1-year other adverse cardiac events defined as
cardiac death, myocardial infarction, and target vessel
revascularization after the treatment procedure (24.4 vs. 4.7%;
P<0.001) (17,18). Therefore, a more aggressive
strategy of lesion modification is needed prior to stent deployment
to achieve efficient interventional treatment for this condition
(19). Matsuhiro et al
(20) previously reported that
maximum calcium thickness <880 µm was a useful predictor of
acceptable stent expansion (defined as 80% expansion) in moderate
calcified lesions. Furthermore, Maejima et al (21) demonstrated that larger calcium arcs
and a lower calcium thickness were associated with the formation of
calcium cracks, which are important determinants of optimal stent
expansion. However, in the present study it was demonstrated that
the maximum calcium arc and the age of patients, but not the
thickness of the lesions, actually had the more significant impact
on stent expansion.
The inconsistency in the inclusion criteria among
these studies may partially explain the different results observed.
Furthermore, the present study proposed a novel calcium scoring
system based on the aforementioned parameters, which displayed high
accuracy in predicting the risk of stent underexpansion.
OCT confers superior improved capability compared
with coronary angiography for the detection of calcium, with a
sensitivity ranging between 95 and 96% and a specificity of 97%
(22,23). In addition, compared with visual
angiographic assessment alone, intracoronary OCT images can provide
additional information on the parameters associated with the
calcification severity of target lesions, such as maximum calcium
arc, thickness, depth and longitudinal length (6). In the present study, the maximum
calcium arc determined from the OCT images was demonstrated to be a
potential independent predictor of stent underexpansion, whereas
parameters from QCA were not. These results highlighted the
importance and value of intravascular imaging modality for severe
calcified lesions in the interventional strategy-making process.
The Society for Cardiovascular Angiography and Interventions
position statement published in 2020 recommended that moderate and
severe calcium observed on coronary angiography, as well as
inadequate balloon expansion during lesion preparation before stent
implantation, should be evaluated by intravascular imaging
(24). In the present study,
angiographically visible moderate and severe calcified lesions were
found in 30 (88.2%) lesions. By contrast, the remaining four
lesions, which showed mild calcification on angiography, had poor
balloon expansion during lesion preparation. Therefore, OCT
evaluation of all lesions was performed according to the
recommendation in the aforementioned 2020 position statement.
The results of a previous study reported that for
lesions with none/mild calcification the rate of major adverse
cardiac events at 1-year is only 8.3%, whereas this increases to
14.6 and 17.7% for moderate and severe calcified lesions,
respectively (25). Fujino et
al (8) previously developed an
OCT-based calcium scoring system to identify lesions, which may be
at risk of stent underexpansion and benefit from plaque
modification prior to stent implantation. In this previous study,
only 29.7% of the patients enrolled had moderate and/or severe
calcified lesions as assessed using angiography. Furthermore, the
OCT characteristics of the patients tended to be relatively mild
calcification. Patients treated with RA or scoring balloon were
excluded. By contrast, in the present study 88.2% of the lesions
had angiographically visible moderate and severe calcification.
These two scoring systems were also compared. The present study's
population with moderate and severe coronary calcification
demonstrated that this newly-established system exhibited an
improved performance compared with the widely-used Fujino et
al (8) system in predicting
the immediate therapeutic outcome of PCI. The comparison of
predictive performance between the novel and the Fujino et
al (8) system in a patient
population with mild calcified plaques may be the aim of future
studies.
It is noteworthy that the proportion of RA during
PCI was significantly higher in patients with poor stent expansion,
which may potentially be the result of lesion calcification being
more severe in this group of patients. Furthermore, there was a
discrepancy between groups with adequate or poor stent expansion in
the present study. Compared with the patients who had adequate
stent expansion, patients in the poor stent expansion group were
significantly older. The maximum calcium arc and thickness were
also larger in the poor stent expansion group. However, the
variables showing significant difference between the two groups and
potential confounding factors, such as maximum calcium length, were
included into the univariate and multivariate logistic regression
analyses, to limit the influence of this discrepancy and to ensure
the accuracy of the results.
The present study also had several limitations. The
present study was retrospective, where leaving the interventional
strategy to the surgeons' discretion may have affected the stent
expansion and the final analysis. In addition, the relatively small
number of patients were enrolled, which made the conclusion drawn
from the study weaker. There was also a lack of a specific cohort
to validate the accuracy of the present calcium scoring system to
predict stent underexpansion. Furthermore, as the OCT images were
not read and analyzed by the same interventional cardiologist at
different times, the intra-observer concordance for the assessment
of the OCT data could not be assessed. Information regarding
peri-procedural complications, such as coronary dissection or
perforation and the balloon used for post-dilatation, was not
available. Finally, the capability of the calcium scoring system to
predict the long-term clinical outcome post-PCI in patients with
moderate and severe calcified lesions remains to be elucidated.
In conclusion, the novel OCT-based calcium scoring
system in the present study demonstrated a high accuracy for the
prediction of the occurrence of stent underexpansion in patients
with moderate and severe coronary calcification. However, the
present system requires further validation in a larger cohort.
Acknowledgements
The authors would like to thank Professor Zhuang Tao
(Shanghai MedStat Clinical Research Institute, Shanghai, China) for
his help in the statistical analysis of the present study.
Funding
Funding: The present study was supported by the National Natural
Science Foundation of China (grant no. 11832003 and 81970294) and
Peking University People's Hospital Scientific Research Development
Funds (grant no. RDL-2020-11).
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
CH and LY collected, analyzed and interpreted the
patient data. ZX and HL contributed to collection and analysis of
the data. YM and QL performed the analysis and interpretation of
angiographic and OCT data. ML and HZ confirm the authenticity of
all the raw data and revised the manuscript critically for
important intellectual content. CL and JL designed the present
study. YM, QL, ML, HZ and JL performed the operation. All authors
read and approved the final manuscript.
Ethics approval and consent to
participate
The present study was approved by the Ethics
Committee of Peking University People's Hospital (Beijing, China;
approval no. 2018PHB154-01) and conducted according to the
principles of the Declaration of Helsinki. Since this clinical
study was a retrospective analysis of the information of previous
cases, without direct contact with the subjects and subject privacy
protection, the risk borne by the subjects was not greater than the
minimum risk. The Ethics Committee of Peking University People's
Hospital waived the requirement for informed consent.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Madhavan MV, Tarigopula M, Mintz GS,
Maehara A, Stone GW and Généreux P: Coronary artery calcification:
Pathogenesis and prognostic implications. J Am Coll Cardiol.
63:1703–1714. 2014.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Tomey MI and Sharma SK: Interventional
options for coronary artery calcification. Curr Cardiol Rep.
18(12)2016.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Kobayashi Y, Okura H, Kume T, Yamada R,
Kobayashi Y, Fukuhara K, Koyama T, Nezuo S, Neishi Y, Hayashida A,
et al: Impact of target lesion coronary calcification on stent
expansion. Circ J. 78:2209–2214. 2014.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Généreux P, Madhavan MV, Mintz GS, Maehara
A, Palmerini T, Lasalle L, Xu K, McAndrew T, Kirtane A, Lansky AJ,
et al: Ischemic outcomes after coronary intervention of calcified
vessels in acute coronary syndromes. Pooled analysis from the
HORIZONS-AMI (harmonizing outcomes with revascularization and
stents in acute myocardial infarction) and ACUITY (acute
catheterization and urgent intervention triage strategy) TRIALS. J
Am Coll Cardiol. 63:1845–1854. 2014.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Ali ZA, Karimi Galougahi K, Mintz GS,
Maehara A, Shlofmitz RA and Mattesini A: Intracoronary optical
coherence tomography: State of the art and future directions.
EuroIntervention. 17:e105–e123. 2021.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Mehanna E, Bezerra HG, Prabhu D, Brandt E,
Chamié D, Yamamoto H, Attizzani GF, Tahara S, Van Ditzhuijzen N,
Fujino Y, et al: Volumetric characterization of human coronary
calcification by frequency-domain optical coherence tomography.
Circ J. 77:2334–2340. 2013.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Kobayashi N, Ito Y, Yamawaki M, Araki M,
Obokata M, Sakamoto Y, Mori S, Tsutsumi M, Honda Y, Makino K, et
al: Optical coherence tomography-guided versus intravascular
ultrasound-guided rotational atherectomy in patients with calcified
coronary lesions. EuroIntervention. 16:e313–e321. 2020.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Fujino A, Mintz GS, Matsumura M, Lee T,
Kim SY, Hoshino M, Usui E, Yonetsu T, Haag ES, Shlofmitz RA, et al:
A new optical coherence tomography-based calcium scoring system to
predict stent underexpansion. EuroIntervention. 13:e2182–e2189.
2018.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Mintz GS, Popma JJ, Pichard AD, Kent KM,
Satler LF, Chuang YC, Ditrano CJ and Leon MB: Patterns of
calcification in coronary artery disease. A statistical analysis of
intravascular ultrasound and coronary angiography in 1155 lesions.
Circulation. 91:1959–1965. 1995.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Prati F, Guagliumi G, Mintz GS, Costa M,
Regar E, Akasaka T, Barlis P, Tearney GJ, Jang IK, Arbustini E, et
al: Expert review document part 2: Methodology, terminology and
clinical applications of optical coherence tomography for the
assessment of interventional procedures. Eur Heart J. 33:2513–2520.
2012.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Tearney GJ, Regar E, Akasaka T,
Adriaenssens T, Barlis P, Bezerra HG, Bouma B, Bruining N, Cho JM,
Chowdhary S, et al: Consensus standards for acquisition,
measurement, and reporting of intravascular optical coherence
tomography studies: A report from the International working group
for intravascular optical coherence tomography standardization and
validation. J Am Coll Cardiol. 59:1058–1072. 2012.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Räber L, Mintz GS, Koskinas KC, Johnson
TW, Holm NR, Onuma Y, Radu MD, Joner M, Yu B, Jia H, et al:
Clinical use of intracoronary imaging. Part 1: Guidance and
optimization of coronary interventions. An expert consensus
document of the European association of percutaneous cardiovascular
interventions. Eur Heart J. 39:3281–3300. 2018.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Sullivan LM, Massaro JM and D'Agostino RB
Sr: Presentation of multivariate data for clinical use: The
Framingham study risk score functions. Stat Med. 23:1631–1660.
2004.PubMed/NCBI View
Article : Google Scholar
|
|
14
|
Mosseri M, Satler LF, Pichard AD and
Waksman R: Impact of vessel calcification on outcomes after
coronary stenting. Cardiovasc Revasc Med. 6:147–153.
2005.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Fujii K, Carlier SG, Mintz GS, Yang YM,
Moussa I, Weisz G, Dangas G, Mehran R, Lansky AJ, Kreps EM, et al:
Stent underexpansion and residual reference segment stenosis are
related to stent thrombosis after sirolimus-eluting stent
implantation: An intravascular ultrasound study. J Am Coll Cardiol.
45:995–998. 2005.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Kastrati A, Dibra A, Mehilli J, Mayer S,
Pinieck S, Pache J, Dirschinger J and Schömig A: Predictive factors
of restenosis after coronary implantation of sirolimus- or
paclitaxel-eluting stents. Circulation. 113:2293–2300.
2006.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Bourantas CV, Zhang YJ, Garg S, Iqbal J,
Valgimigli M, Windecker S, Mohr FW, Silber S, Vries TD, Onuma Y, et
al: Prognostic implications of coronary calcification in patients
with obstructive coronary artery disease treated by percutaneous
coronary intervention: A patient-level pooled analysis of 7
contemporary stent trials. Heart. 100:1158–1164. 2014.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Sharma SK, Bolduan RW, Patel MR, Martinsen
BJ, Azemi T, Giugliano G, Resar JR, Mehran R, Cohen DJ, Popma JJ
and Waksman R: Impact of calcification on percutaneous coronary
intervention: MACE-Trial 1-year results. Catheter Cardiovasc
Interv. 94:187–194. 2019.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Tang Z, Bai J, Su SP, Lee PW, Peng L,
Zhang T, Sun T, Nong JG, Li TD and Wang Y: Aggressive plaque
modification with rotational atherectomy and cutting balloon for
optimal stent expansion in calcified lesions. J Geriatr Cardiol.
13:984–991. 2016.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Matsuhiro Y, Nakamura D, Shutta R,
Yanagawa K, Nakamura H, Okamoto N, Egami Y, Sakata Y, Nishino M and
Tanouchi J: Maximum calcium thickness is a useful predictor for
acceptable stent expansion in moderate calcified lesions. Int J
Cardiovasc Imaging. 36:1609–1615. 2020.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Maejima N, Hibi K, Saka K, Akiyama E,
Konishi M, Endo M, Iwahashi N, Tsukahara K, Kosuge M, Ebina T, et
al: Relationship between thickness of calcium on optical coherence
tomography and crack formation after balloon dilatation in
calcified plaque requiring rotational atherectomy. Circ J.
80:1413–1419. 2016.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Yabushita H, Bouma BE, Houser SL, Aretz
HT, Jang IK, Schlendorf KH, Kauffman CR, Shishkov M, Kang DH,
Halpern EF and Tearney GJ: Characterization of human
atherosclerosis by optical coherence tomography. Circulation.
106:1640–1645. 2002.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Wang X, Matsumura M, Mintz GS, Lee T,
Zhang W, Cao Y, Fujino A, Lin Y, Usui E, Kanaji Y, et al: In vivo
calcium detection by comparing optical coherence tomography,
intravascular ultrasound, and angiography. JACC Cardiovasc Imaging.
10:869–879. 2017.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Riley RF, Henry TD, Mahmud E, Kirtane AJ,
Brilakis ES, Goyal A, Grines CL, Lombardi WL, Maran A, Rab T, et
al: SCAI position statement on optimal percutaneous coronary
interventional therapy for complex coronary artery disease.
Catheter Cardiovasc Interv. 96:346–362. 2020.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Copeland-Halperin RS, Baber U, Aquino M,
Rajamanickam A, Roy S, Hasan C, Barman N, Kovacic JC, Moreno P,
Krishnan P, et al: Prevalence, correlates, and impact of coronary
calcification on adverse events following PCI with newer-generation
DES: Findings from a large multiethnic registry. Catheter
Cardiovasc Interv. 91:859–866. 2018.PubMed/NCBI View Article : Google Scholar
|