Introduction
Rheumatoid arthritis (RA) is a systemic autoimmune
disease that is characterized by inflammation in the synovial
tissues, including joints, cartilage, bone and extra-articular
sites (less frequently) (1). RA is
the most prevalent form of arthritis, which is associated with high
rates of disability, the patients with which are particularly
susceptible to numerous comorbidities such as interstitial lung
disease and cardiovascular disease (2,3). It
has been previously reported that 84.8% patients with RA typically
suffer from ≥ one comorbidity (4).
Among the comorbidities associated with RA, hyperlipidemia (HL) is
one of the most frequently observed. Tthe proportion of RA
complicated with hyperlipidemia (RA-HL) can be as high as 41.3%
(4). In addition, other previous
studies have reported that 53.5% of patients with RA are afflicted
with dyslipidemia, which is mainly manifested by elevated
triglyceride (TG) levels and decreased high-density lipoprotein
cholesterol levels (5,6). Immunomodulation during the active
phase of RA promotes the release of inflammatory factors, such as
TNF-α, IL-1 and IL-6, from the joint synovium into the systemic
blood circulation, thereby increasing the levels of these
inflammatory factors in the bloodstream (7). A variety of inflammatory factors have
been reported to lead to the abnormal activity and expression of
lipoprotein esterase, a key enzyme in the process of lipid
metabolism (8,9). This in turn alters the metabolism of
nutrients, especially proteins and lipids, in the body, causing
abnormalities in blood lipid levels (8,9).
Therefore, a feasible method for improving the dyslipidemia of
patients whilst alleviating their symptoms remains in demand.
It has been previously reported that Chinese herbal
decoctions combined with Chinese herbal medicine (CHM) used in
certain hospital preparations can effectively reduce the risk of
readmission in patients with RA combined with HL (RA-HL) (10,11).
In particular, Xinfeng capsule (XFC; patent no. ZL201310011369.8)
is one such Chinese medicine preparation that has been previously
developed (12). Our preliminary
studies revealed that XFC can regulate immunity, inhibit
inflammatory analgesia and improve blood viscosity, thereby
improving cell metabolism and promoting joint function recovery to
achieve satisfactory clinical results (13-15).
Accumulating evidence from earlier clinical studies has also found
that XFC is highly effective for the treatment of RA, with little
to no toxic or adverse side effects (16,17).
Therefore, this suggests that XFC is a clinically viable Chinese
medicine for the treatment of RA (18). A previous study demonstrated that
XFC can alleviate the clinical symptoms of RA in patients (19). Huangqin chubi capsule (HQC; patent
no. ZL20110095718.X) is another characteristic Chinese medicine
preparation that was developed in the First Affiliated Hospital,
Anhui University of Chinese Medicine (20). Previous studies have revealed that
HQC yielded satisfactory results in clinical practice for RA
treatment (21,22). HQC can modulate oxidative stress
and effectively improve immune inflammation, mainly by inhibiting
the secretion of proinflammatory factors, such as IL-1β, whilst
promoting the secretion of IL-4(23). In addition, our team previously
conducted systematic studies on the fingerprint and
pharmacokinetics of XFC and HQC (24-28).
Relatively complete chromatographic information was obtained, and
the relative peak area ratio of each substance was within a certain
range. In terms of the fingerprint, it could not only reflect the
type and quantity of chemical components in XFC and HQC, but also
describe and evaluate XFC and HQC to control its quality in an
all-round way. Therefore, it can be used as one of the quality
control methods of XFC and HQC.
CHM has conferred promising clinical outcomes in
alleviating the clinical symptoms of RA patients (29). However, there remains to be a lack
of sufficient evidence-based data on whether CHM treatment can
reduce the risk of readmission and improve endpoint outcomes in
patients with RA-HL. Therefore, to further explore the clinical
results of patients with RA-HL and a clinical evidence-based
strategy for the treatment of patients with RA-HL with CHM, the
present study analyzed the risk of readmission in patients with
RA-HL. This was performed by extracting the clinical data of
patients with RA-HL between 2014 and 2015 from the electronic
medical record database of the First affiliated hospital of Anhui
University of Chinese Medicine (Hefei, China).
Materials and methods
Patients
Participants in the present study were identified by
collecting the data of patients with RA admitted to the Department
of Rheumatology and Immunology of the First Affiliated Hospital of
the Anhui University of Chinese Medicine from June 2014 to June
2015, who were followed up until the end of 2021. The data of
patients consisted of the following information: i) The use of CHM;
and ii) disease-associated laboratory indicators [rheumatoid factor
(RF), high-density lipoprotein cholesterol (HDL-C), total
cholesterol (TC), TG and low-density lipoprotein cholesterol
(LDL-C) during admission; inflammatory markers, namely C-reactive
protein (CRP), erythrocyte sedimentation rate (ESR), immunoglobulin
A (IgA), immunoglobulin G (IgG), immunoglobulin M (IgM) and immune
indicators (C3 and C4)].
Inclusion and exclusion criteria
Fig. 1 shows the
flow chart of patient selection. The inclusion criteria of the
patients were as follows: i) Patients diagnosed with RA at first
visit (conforming to the RA classification standard of American
College of Rheumatology/European League Against Rheumatism in 2010)
(30) and combined with
dyslipidemia (including serum TC levels ≥5.2 mmol/l; TG levels ≥1.7
mmol/l; LDL-C levels ≥3.4 mmol/l; and HDL-C levels <1.0 mmol/l)
(31); ii) patients receiving CHM
treatment or routine western medicine treatment in the hospital,
with complete case data available.
Patients were excluded if they fulfilled the
following criteria: ii) Patients lost to follow-up; and ii)
patients with incomplete medical records.
Subsequently, the included patients were clarified
into the following two cohorts: CHM users and non-CHM (those who
never used any CHM after being diagnosed with RA-HL). Variables,
including age, sex and diagnosis year of the patients with RA-HL
were adjusted by matching one patient treated with CHM to a patient
in the non-CHM group with propensity score matching.
The Ethics Committee of the First Affiliated
Hospital of Anhui University of Traditional Chinese Medicine
approved the present study and exempted patients from providing
informed consent (approval no. 2022MCZQ01). A total of 425 patients
with RA, including female (n=287) and male (n=138), the mean ± SD
age is 60.41±11.52 were included who had a complete dataset of
laboratory examination indices.
Study design and terminologies
The present study was a retrospective propensity
score-matched cohort design, which investigated the effect of
adjuvant CHM on the risk of readmission in patients with RA-HL. The
age, sex and diagnosis year between one patient treated with CHM
and one who was not treated with CHM were subjected to propensity
score matching (PSM) (32) to
increase the precision of the present study. PSM was performed
using SPSS Statistics (version 23; IBM Corp). Subsequently,
differences in sex, age, medication, combined diseases and the risk
of readmission between the two groups were observed.
According to whether the patients received CHM
treatment in this hospital, patients were allocated into either the
CHM or non-CHM (referring to the patients who only underwent
conventional western medicine treatment) groups. For the treatment
of patients in the non-CHM group, patients in the CHM group were
additionally subjected to CHM treatment, including oral CHM
decoction combined with Chinese patented medicine (XFC and HQC).
The oral CHM decoction mainly included the following five
categories: Baihu-Guizhi decoction (33), Shuanghe decoction (34), Duhuo Jisheng decoction (35), Yiyiren decoction (36) and modified Simiao powder (37). In addition, patients in the two
groups were further grouped in accordance with the time of CHM
exposure as follows: i) Non-CHM, referring to 0-4 weeks of CHM
treatment; ii) low exposure, referring to 4-12 weeks of CHM
treatment; iii) moderate exposure, referring to 12-48 weeks of CHM
treatment; and iv) high exposure, referring to ≥48 weeks of CHM
treatment (38).
The endpoint index used for the present study is
referring to the main evaluation index during the clinical trials
(39). Clinically, the risk of
possible adverse reactions is a concern for the majority of
patients who were administered with the same western medicine for
long periods of time due to the lack of clinical guidance. Based on
the comprehensive analysis of the previous follow-up, the following
four endpoint events with the highest incidence were identified:
Readmission for RA is active; extra-joint lesions; surgical
treatment; and all-cause mortality (40). In particular, readmission was found
to be the endpoint event with the highest incidence and was of
particular concern (40).
Therefore, this event was utilized as an endpoint indicator to
evaluate the prognosis of RA in the present study.
Methods. Telephone follow-up
Telephone follow-up is a simple and effective health
service model used to facilitate the compliance of patients with
drug treatment and to understand the circumstances regarding the
prognosis of patients (41).
The present study was conducted by researchers (XL,
FFW, QH and YYF), where the main follow-up information included the
following: i) Basic information, namely sex, age and course of
disease; ii) the occurrence of RA-associated comorbidities,
including HL, interstitial lung disease, rheumatic heart disease,
atrophic gastritis and Sjogren's syndrome; iii) endpoint events,
including readmission for aggravation, extra-joint lesions,
surgical treatment and all-cause mortality; and iv) the use of
drugs, including the type, dosage and treatment period of CHM,
Chinese patent medicine and western medicine.
Kaplan-Meier (KM) curve
It is of importance to focus on both the occurrence
of readmission in patients and the time required for readmission in
patients to occur. Therefore, the present study used KM curve to
analyze the occurrence of readmission in CHM and non-CHM groups,
RA-HL and RA-non-HL groups of patients. The product-limit method is
also called the KM method, with the curve of which named the KM
curve. It is commonly conducted using the log-rank test, where
there is typically a statistically significant difference when
P<0.05 is found (42). The
formula is as follows:
Where, for the specified time point, tn, S
represents the proportion of no readmissions, d represents the
number of event outcomes at this time point and r represents the
number of remaining follow-up cases before this time point. Through
the KM estimation method, the probability of readmission can be
obtained at the corresponding time point on the survival curve.
Logistics regression
In logistics regression analysis, a logistic
regression model was developed with sex, age, duration, use of
Chinese medicine, inflammatory indices (ESR and high-sensitivity
CRP) and immune indices (IgA, IgG, IgM, C3, C4 and RF) as
independent variables (x) and readmission as the dependent variable
(y) (43). The formula is as
follows:
Association rules. The Chinese medicine
prescribed for each of the individual patients were named 1,
whereas those who did not receive Chinese medicine were named 0.
Additionally, any improvement in the laboratory indices was also
assigned 1, otherwise 0. Subsequently, the ‘Apriori’ module
(44) in the software SPSS
Clementine v. 11.1 (IBM Corp.) (45) was utilized to determine the
association between CHM treatment and the laboratory indicators,
with a minimum support rate of 25%, a confidence level of 60% and a
lift of >1, before visualizing the association results.
‘Apriori’ was used to identify associations among each of the
items. Individual drugs and indices were used as variables. The
formula used is as follows (46):
Where X→Y is an association rule, X represents the
set of herb items and Y represent the set of laboratory indices, N
is the sum of itemset, σ(X) is the frequency of itemset X, X ∪ Y is
the union of itemsets X and Y, σ(X ∪Y) is the frequency with which
itemsets X and Y appear together, support (X→Y) is the frequency
with which X and Y appear together and confidence (X→Y) is the
probability that itemset Y appears in the presence of X. Lift is
the ratio of the probability that itemset Y appears in the presence
of itemset X to the frequency of itemset Y. Support and confidence
are often used to eliminate meaningless combinations. Lift
indicates the validity of the association rules.
χ2 test
The χ2 test was used to assess the
difference between groups in terms of sex, comorbidity, medicine
treatment duration and recurrent exacerbation. Specifically, the
larger the χ2 test value, the greater the degree of
deviation between the two. If the two values are completely equal,
the χ2 test value would then be 0, indicating that the
theoretical value is completely consistent. The formula is as
follows (47):
Statistical analysis
All data were analyzed with SPSS v.21.0 (IBM Corp.).
Count data were presented as numbers or percentages. Two
independent samples t-test was used to analyze differences in age
and course of disease, where the data are presented as the mean ±
standard deviation. Differences between each group were compared
using the χ2 test. In addition, Wilcoxon
signed-rank test was used to analyze the laboratory indicators
before and after treatment of patients, which were presented as the
median (interquartile range). P<0.05 was considered to indicate
a statistically significant difference.
Results
Demographic characteristics of
patients with RA
Fig. 1 exhibits the
process of patient selection (the data of the proportions are not
shown). Specifically, there were original 839 with patients RA, of
whom 425 (50.66%) had complete data on their laboratory indicators.
Among these RA patients, 263 patients (31.70%) fulfilled the
diagnostic criteria of HL, of whom ~16.21% (n=136) received CHM
treatment and 15.13% (n=127) were not treated with CHM. The nine
cases in the CHM user group were excluded due to age and sex
mismatch after propensity score matching analysis. Finally, 127
patients were assigned into the CHM group whereas 127 patients were
assigned into the non-CHM group after propensity score matching
analysis.
According to Table
I, differences were observed in sex between the RA-HL and
RA-non-HL groups (P<0.05). However, there were no significant
differences in age, sex, drug treatment or course of disease
between the RA-HL and RA-non-HL groups after propensity score
matching (Table I).
 | Table ICharacteristics of patients with
RA-HL and RA-non-HL matched by propensity scores. |
Table I
Characteristics of patients with
RA-HL and RA-non-HL matched by propensity scores.
| A, Unmatched |
|---|
| Parameter | Total (n=425) | RA-HL (n=263) | RA-non-HL
(n=162) |
P-valuea |
|---|
| Age, years | 60.41±11.52 | 60.36±11.69 | 60.43±11.54 | 0.517 |
| Sex, N (%) | | | | 0.015 |
|
Female | 287 | 189 (71.86) | 98 (60.49) | |
|
Male | 138 | 74 (28.14) | 64 (39.51) | |
| Course of disease,
months | 5.86±1.34 | 5.81±1.98 | 5.91±1.65 | 0.476 |
| CHM, N (%) | 341 | 192 (73.00) | 149 (91.97) | <0.001 |
| NSAIDs, N (%) | 402 | 250 (95.06) | 152 (93.82) | 0.586 |
| GCs, N (%) | 413 | 256 (97.33) | 157 (96.91) | 0.797 |
| DMARDs, N (%) | 398 | 248 (94.29) | 150 (92.59) | 0.484 |
| B, Matched |
| Parameter | Total (n=302) | RA-HL (n=151) | RA-non-HL
(n=151) |
P-valuea |
| Age, years | 60.43±11.53 | 60.45±11.59 | 60.41±11.51 | 0.532 |
| Sex, N (%) | | | | 0.934 |
|
Female | 173 | 85 (56.29) | 88 (58.27) | |
|
Male | 129 | 64 (42.38) | 65 (43.05) | |
| Course of disease,
months | 5.75±1.48 | 5.73±1.45 | 5.76±1.53 | 0.571 |
| CHM, N (%) | 225 | 113 (74.83) | 112 (74.17) | 0.895 |
| NSAIDs, N (%) | 292 | 147 (97.35) | 145 (96.02) | 0.520 |
| GCs, N (%) | 296 | 150 (99.34) | 146 (96.69) | 0.099 |
| DMARDs, N (%) | 290 | 144 (95.36) | 146 (96.69) | 0.556 |
Results in Table
II suggested that the percentage of female patients (50.48%)
was higher compared with that of male patients (25.00%) in the CHM
group (P<0.05). Additionally, the percentage of patients with RA
combined with interstitial lung disease (35.29%), rheumatic heart
disease (40.00%), atrophic gastritis (37.50%) or Sjogren's syndrome
(41.66%) were lower in the CHM group compared with that in the
non-CHM group (P<0.01). In addition, the number of patients who
were treated with both Chinese patent medicine (84.25%) and
external drugs (70.59%) was higher in the CHM group compared with
that in the non-CHM group (29.41%) (Table II). This shows that patients in
CHM user group tended to adopt the combination of oral CHM and
external plaster. However, no significant differences could be
found between the CHM group and the non-CHM group in terms of age
and course of disease.
 | Table IIDemographic characteristics of
patients in the CHM and non-CHM groups matched by propensity
scoring. |
Table II
Demographic characteristics of
patients in the CHM and non-CHM groups matched by propensity
scoring.
| Parameter | Total (n=254) | CHM (n=127) | Non-CHM
(n=127) |
P-valuea |
|---|
| Age, years | 60.35±11.69 | 60.39±11.77 | 60.33±11.62 | 0.487 |
| Sex, N (%) | | | | |
|
Female | 206 | 104 (50.48) | 102 (49.51) | 0.043 |
|
Male | 48 | 12 (25.00) | 25 (75.00) | |
| Course of disease,
months | 5.77±1.53 | 5.80±1.49 | 5.76±1.56 | 0.537 |
| Comorbidity, N
(%) | 54 | 21 (40.74) | 33 (59.26) | <0.01 |
|
Interstitial
lung disease | 16 | 5 (35.29) | 11 (64.71) | |
|
Rheumatic
heart disease | 21 | 8 (40.00) | 13 (60.00) | |
|
Atrophic
gastritis | 8 | 3 (37.50) | 5 (62.50) | |
|
Sjogren's
syndrome | 12 | 5 (41.66) | 7 (58.33) | |
|
Chinese
Patent Medicine, N (%) | 162 | 107 (84.25) | 37 (29.13) | <0.01 |
|
Xinfeng
Capsule | 118 | 97 | 21 | |
|
Wuwei
Wentong capsule | 66 | 62 | 4 | |
|
HuangQin
Capsule | 103 | 89 | 14 | |
| External
medication, N (%) | 34 | 24 (70.59) | 10 (29.41) | 0.317 |
|
Hibiscus
ointment | 23 | 17 (73.91) | 6 (26.08) | |
|
Xiaoyu Jiegu
powder | 6 | 6(100) | 0 (0) | |
|
Wuwei gujuba
poison powder | 5 | 1 (20.00) | 4 (80.00) | |
| Western medicine, N
(%) | 178 | 62 (34.83) | 126 (65.17) | 0.142 |
|
Methylprednisolone | 149 | 36 (24.16) | 113 (75.83) | |
|
Leflunomide | 121 | 24 (19.83) | 97 (80.17) | |
|
Lornoxicam | 106 | 22 (20.75) | 84 (79.25) | |
Influencing factors for the
readmission of patients with RA-HL
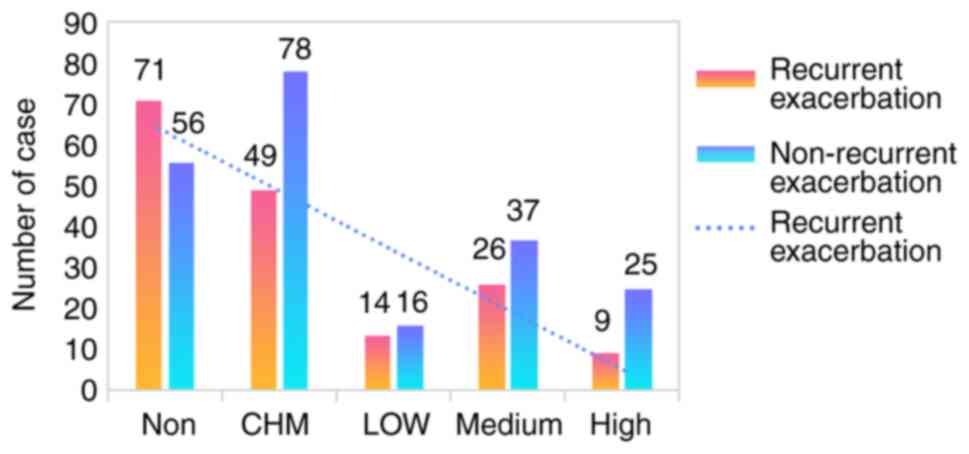
As shown in Fig. 2,
the proportion of patients with recurrent exacerbation was lower in
the CHM group (38.58%) compared with that in the non-CHM group
(55.91%), and the longer the use of CHM, the lower the proportion
of readmission. In addition, results of the χ2 test for
readmission demonstrated that the proportion of aggravation was
higher in the RA-HL group (60.22%) compared with that in the
RA-non-HL group (37.01%; P<0.05; Table III) and lower in the CHM group
(38.58%) compared with that in the non-CHM group (55.91%;
P<0.01; Table IV). These
findings suggested that HL is a risk factor, but traditional
Chinese medicine is a preventive factor against readmission in
patients with RA. However, the differences of readmission were not
significant in CHM and non-CHM groups and RA-HL and RA-non-HL
groups of patients according to the KM curves (Figs. 3 and 4).
 | Table IIIResults of the χ2 test of
readmission among patients in the RA-HL and RA-non-HL groups. |
Table III
Results of the χ2 test of
readmission among patients in the RA-HL and RA-non-HL groups.
| Group | N | Recurrent
exacerbation | Non-Recurrent
exacerbation | Recurrent
exacerbatio n (%) | χ2
value | P-value |
|---|
| RA-HL | 181 | 109 | 72 | 60.22 | 5.385 | 0.020 |
| RA-non-HL | 181 | 87 | 94 | 37.01 | | |
| Total | 362 | 176 | 186 | 48.62 | | |
 | Table IVResults of the χ2 test of
readmission among patients in the CHM and non-CHM groups. |
Table IV
Results of the χ2 test of
readmission among patients in the CHM and non-CHM groups.
| Group | N | Recurrent
exacerbation | Non-Recurrent
exacerbation | Recurrent
exacerbatio n (%) | χ2
value | P-value |
|---|
| CHM | 127 | 49 | 78 | 38.58 | 7.645 | 0.006 |
| Non-CHM | 127 | 71 | 56 | 55.91 | | |
| Total | 254 | 120 | 134 | 47.24 | | |
The results of the logistic regression analysis
(Fig. 5) revealed that ESR was a
risk factor [OR (95% CI)=1.544 (1.284-2.198)] whereas CHM was a
protective factor [OR (95% CI)=0.619 (0.302-0.931)] against
readmission for patients with RA-HL.
Effects of TCM on the immune
inflammatory and lipid metabolism indices in patients with
RA-HL
Subsequently, the laboratory indicators of the
patients with RA-HL were compared to further ascertain how CHM
affected the pathophysiology of RA-HL (Table V). Compared with those before
treatment, the levels of TC, TG, HDL-C, ESR, CRP, IgA, IgG, C3, C4
and RF were all significantly decreased in patients with RA-HL
after two weeks of treatment (P<0.01).
 | Table VDifferences in laboratory indicators
before and after treatment of patients with RA-HL in the CHM
group. |
Table V
Differences in laboratory indicators
before and after treatment of patients with RA-HL in the CHM
group.
| Indices | Pre-treatment
(n=127) | Post-treatment
(n=127) | P-values |
|---|
| Total cholesterol,
mmol/l | 4.92 (4.04,
5.69) | 4.39 (3.77,
5.09) | <0.001 |
| Triglyceride,
mmol/l | 1.46 (1.03,
2.11) | 1.10 (0.78,
1.60) | <0.001 |
| High-density
lipoprotein-Cholesterol, mmol/l | 1.27 (1.03,
1.65) | 1.34 (1.05,
1.72) | <0.001 |
| Low-density
lipoprotein-Cholesterol, mmol/l | 2.85 (2.27,
3.46) | 2.75 (2.19,
3.38) | 0.006 |
| Rheumatoid factor,
U/ml | 97.60 (19.8,
245.80) | 92.50 (20.00,
197.40) | 0.001 |
| C-reactive protein,
mg/l | 17.05 (3.54,
40.14) | 1.65 (0.42,
5.69) | <0.001 |
| Erythrocyte
sedimentation rate, mm/h | 34.00 (19.00,
58.00) | 22.00 (13.00,
40.00) | <0.001 |
| IgG, g/l | 12.28 (9.53,
16.04) | 12.03 (9.5,
15.60) | 0.009 |
| IgM, g/l | 1.07 (0.80,
1.55) | 1.13 (0.80,
1.58) | 0.237 |
| IgA, g/l | 2.60 (1.83,
3.25) | 2.43 (1.82,
3.20) | <0.001 |
| C3, g/l | 113 (98.4,
135.2) | 110.4 (98.2,
123.1) | <0.001 |
| C4, g/l | 26.5 (21.7,
31.8) | 23.9 (19.7,
29.7) | <0.001 |
Association rules analysis of the
association between TCM treatment and laboratory indicators in
patients with RA-HL
Association rules were utilized to analyze the
association of CHM and Chinese patent medicines used to treat
patients with RA-HL, with laboratory indicators, using the support
threshold of >20%, the confidence threshold of CHM for the
improvement of laboratory indicators of >80% and the lift
threshold of >1. The results of the association rules were then
visualized. In the complex network diagram, each node represents
the drugs and laboratory indicators used. The drugs appearing in
the same prescription and the related drugs and indicators are
connected by lines. The stronger the association, the darker the
lines are. The results (Table VI
and Fig. 6) demonstrated that XFC,
HQC, Plantaginis Herba, Sinomenii Caulis, Alismatis Rhizoma,
Hedyotis diffusa Clematidis Radix et Rhizoma and other drugs were
strongly correlated with the improvement of ESR, RF, CRP, C3, TC
and TG.
 | Table VIAssociation rules for the association
assessment between Chinese herbal medicine and laboratory
indicators in patients with rheumatoid arthritis and
hyperlipidemia. |
Table VI
Association rules for the association
assessment between Chinese herbal medicine and laboratory
indicators in patients with rheumatoid arthritis and
hyperlipidemia.
| Items (left hand
side ⇒ right hand side) | Support (%) | Confidence (%) | Lift |
|---|
| {HQC & XFC
& ALISMATIS RHIZOMA} ⇒ {rheumatoid factor↓} | 47.29 | 97.75 | 1.22 |
| {XFC &
ALISMATIS RHIZOMA} ⇒ {Erythrocyte sedimentation rate↓} | 44.40 | 93.89 | 1.11 |
| {HQC & Hedyotis
diffusa} ⇒ {C-reactive protein↓} | 42.59 | 91.47 | 1.13 |
| {HQC &
CLEMATIDIS RADIX ET RHIZOMA} ⇒ {C3↓} | 53.06 | 89.09 | 1.11 |
| {XFC &
PLANTAGINIS HERBA} ⇒ {total cholesterol↓} | 20.58 | 87.69 | 1.02 |
| {XFC &
SINOMENII CAULIS} ⇒ {triglyceride↓} | 24.18 | 86.56 | 1.05 |
Discussion
RA is a chronic and systemic autoimmune disease with
symmetrical and erosive polyarthritis as one of the principal
clinical manifestations (48). The
main pathological changes associated with RA include synovitis,
vasculitis and the gradual destruction of articular cartilage and
bones (49). In addition to
arthropathy, patients with RA also frequently suffer from
cardiovascular lesions and lipid metabolism disorders long before
RA is diagnosed (50-52).
In particular, results from a previous large cohort study involving
400 confirmed patients with RA found that 51% patients with RA also
suffered from blood lipid disorders, which was higher compared with
that in the non-RA population (53). Furthermore, it has been reported
that lipid metabolism disorders are associated with the disease
activity of RA (54).
Specifically, the development of lipid metabolism disorders can be
facilitated by the release of inflammatory factors, which can in
turn result in the aberrant expression of lipoprotein esterase, a
key enzyme in the process of lipid metabolism (55). In addition, previous studies
(56) have shown that patients
with RA have lipoprotein metabolism disorder, and that HDL-C,
Apolipoprotein (APO)-A1 is decreased, while LDL-C and APO-B is
increased.
Previously, through retrospective data mining
research, CHM has been found to improve immune (C3, C4, IGA and
IGG) and inflammatory indicators (ESR and CRP) in patients with RA
(57), where the efficacy of CHM
combined with prescription drugs such as Tripterygium wilfordii
polyglycosides tablets, Furong ointment and XFC, and HQC is
superior compared with that mediated by CHM alone (58-60).
Another previous retrospective cohort study in Taiwan found that
compared with that in the non-TCM group, the prognosis of the
circulatory system of inpatients was more favorable in the
auxiliary TCM group, which was accompanied by a ~66% reduction in
the readmission rate due to events in the circulatory system
(61). Our previous studies
demonstrated that intervention with traditional Chinese medicine
has been associated with the occurrence of endpoint events
(including re-admission, extra-articular lesions, surgery and
all-cause death) in patients with RA, such that the longer the
patient takes CHM, the lower the incidence of endpoint events
(62).
In previous RA cohort follow-up studies, the types
of comorbidities that can affect RA activity was focused upon
(63,64). Although they have investigated the
influence of circulatory system diseases and lipoprotein metabolic
disorder on RA activity (65),
none have explored the influence of TCM on the readmission of
patients with RA-HL. Therefore, the present cohort study was
performed to clarify the impact of dyslipidemia on the readmission
of patients and the relationship between TCM treatment and
readmission of patients with RA-HL.
In the present study, the collected information of
patients was subjected to propensity score matching. The results
demonstrated that differences in sex existed between the RA-HL and
RA-non-HL groups. Following propensity score matching, no notable
differences could be found between the RA-HL group and the
RA-non-HL group in terms of age, sex, used drugs, course of disease
or readmission. It was then observed that the proportion females as
higher compared with males in the CHM group after propensity score
matching. The proportion of patients with RL also suffering from
interstitial lung disease, rheumatic heart disease, atrophic
gastritis and Sjogren's syndrome was lower in the CHM group
compared with that in the non-CHM group. In addition, there was a
lower proportion of patients treated with NSAIDs in the CHM group
compared with that in the non-CHM group. By contrast, there was a
higher proportion of patients administered with both Chinese patent
medicine and external drugs in the CHM group compared with that in
the non-CHM group. Age, sex and course of disease did not differ
between the CHM group and the non-CHM group.
In the present study, the results of the
χ2 test and logistic regression analysis suggest that HL
was a risk factor whereas CHM is a protective factor against
readmission in patients with RA-HL. The laboratory indicators of
patients with RA-HL were compared to assess the mechanism of action
of CHM. The levels of TC, TG, HDL-C, ESR, CRP, IgA, IgG, C3, C4 and
RF were all significantly lower in patients with RA-HL after
treatment compared with those prior to treatment. Afterwards,
association rule analysis was conducted to determine the
association of CHM and Chinese patent medicines utilized for
patients with RA-HL, with laboratory indicators, with the support
degree set at >20%, the confidence degree of CHM for the
improvement of laboratory indicators set at >80% and the lift
degree set at >1. The results showed that the combination of CHM
and hospital preparations (XFC and HQC) in this hospital
effectively ameliorated the serum TC and TG levels and
immune-inflammation indicators C3, ESR and CRP.
The combined use of CHM is a common method of
treating diseases in China (66),
which is associated with increased efficiency (67). Multiple components and multiple
targets appear to form the treatment characteristics of CHM for the
treatment of RA-HL (68,69). A previous study assessed the
potential effects of CHM on RA treatment based on the association
rule and a random walking-based model (70), which demonstrated that the CHM
constituents likely exert synergistic effects, such that various
combinations of a particular CHM can produce different therapeutic
effects on RA treatment (70).
Wang et al (71) explored
the characteristics of compound prescription of TCM acting through
‘multi-component-multi-target-multi-pathway’ through establish a
network pharmacology-based model.
The association rules analysis in the present study
found that Alismatis Rhizoma, Hedyotis diffusa,
Angelicae Sinensis, clematidis radix et rhizoma and
the Chinese patent medicine HQC were tightly associated with the
improvement of the immune inflammatory indicators. In addition,
Alismatis Rhizoma, Plantaginis Herba, Sinomenii
Caulis and XFC were associated with improvements in the lipid
metabolism indices. TCM believes that these herbs have significant
effects on relieving the clinical symptoms of RA (72-75),
especially Alisma orientalis. In addition, a previous study
found that Alisma orientalis extract can reduce blood lipid
level (TC, TG and LDL-C) in hyperlipidemia model rats (76).
XFC is a hospital preparation of the First
Affiliated Hospital of Anhui University of Traditional Chinese
Medicine and also the most frequently used Chinese patent medicine
in the present study. The preparation consists of four traditional
Chinese medicines, namely Astragali Radix, Coicis Semen,
Tripterygium wilfordii and Scolopendea. Among them,
Astragalus polysaccharide, the main active ingredient of
Astragali Radix, has been reported to exhibit favorable
anti-inflammatory effects (77).
By contrast, Coix oil, the main active ingredient of Coicis
Semen, has been previously observed to exert an
anti-inflammatory and analgesic role, by diminishing capillary
permeability (78). Thunder male
vine and centipede are effective in promoting blood circulation and
relieving pain (79,80). In addition, triptolide, the main
active ingredient of Tripterygium wilfordii, has been found
to suppress inflammation by decreasing IL-1 and TNF levels in the
peripheral blood of rats with AA (81). A previous study (19) demonstrated that XFC could improve
disease activity score (DAS28) and iron reserve in patients with RA
during the active period.
HQC is mainly comprised of five Chinese medicines,
including Scutellariae radix, Coicis Semes, Persicae Semen,
Gardeniae Fructus and Clematidis Radix ET Rhizoma. A previous
study revealed that HQC inhibited secondary joint inflammation in
AA rats as a result of lowering the serum levels of inflammatory
cytokines (IL-1β and IL-6) (82).
Another study previously reported that HQC markedly attenuated the
clinical symptoms and inflammation of patients with RA, with
superior efficacy compared with leflunomide (83). Data mining results revealed that
XFC combined with HQC may be effective in ameliorating aberrant
immune inflammation in patients with RA (84). In addition, a previous
multi-center, parallel-group, double-blind and randomized
controlled trial reported that the most common adverse reactions
caused by XFC and HQC were hepatic impairment, anemia,
leukocytopenia, epigastric discomfort and phalacrosis. However, no
severe adverse reactions occurred and no subjects withdrew due to
adverse reactions (85,86). It should be emphasized here that
only two Chinese medicine preparations were investigated in the
present study, meaning that the results obtained in the present
study may not be fully representative of all CHM.
In terms of methods and study design, propensity
score matching was utilized in the present study to increase the
comparability of patients in the CHM and non-CHM groups, which
reduced the analysis of confounding factors, such as age, sex and
disease course of the patients in the CHM and non-CHM groups.
However, the number of limitations remain. The present study
remains to be only a single-center clinical study and cannot be
applied to fully reflect the effect of CHM treatment on the risk of
readmission in patients with RA-HL in the ‘real world’. In
addition, only the time of treatment with prescribed CHM were
collected as treatment period of CHM. Therefore, it was difficult
to exclude patients with unknown, potentially combined medication,
such as those receiving CHM treatment in other hospitals.
In conclusion, the results of the present cohort
study generated a conclusion that the risk of readmission was
increased in patients with RA-HL compared with that in patients
with RA-non-HL. However, CHM treatment may decrease this risk in
patients with RA-HL. This conclusion indicates that CHM is a
protective factor against readmission in patients with RA-HL
long-term.
Acknowledgements
Not applicable.
Funding
Funding: The present study was funded by The 12th batch of ‘115’
Innovation team of Anhui Province [Anhui Talent Office (2019) No.
1], Anhui Famous Traditional Chinese Medicine Liu Jian Studio
Construction Project [Traditional Chinese Medicine Development
Secret (2018) No. 11], University Collaborative Innovation Project
of Anhui Province (grant no. GXXT-2020-025), and Anhui Province
Major and difficult Diseases [Traditional Chinese Medicine
Development Secret (2021) No.70].
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
MH and JL contributed to the conception and design
of this study. MH, YF, XL, QH and FW were responsible for the data
collection and analysis. All authors read and approved the final
manuscript. MH, YF and JL confirm the authenticity of all the raw
data.
Ethics approval and consent to
participate
The Ethics Committee of the First Affiliated
Hospital of Anhui University of Traditional Chinese Medicine
approved this study and exempted patients from the right of
informed consent (approval no. 2022MCZQ01).
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Scherer HU, Häupl T and Burmester GR: The
etiology of rheumatoid arthritis. J Autoimmun.
110(102400)2020.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Yang X, Bao L, Tang H, Ling L, Meng F, Yin
J, Zhang H and Pengjiang C: Clinical Study on 4238 Cases of
Rheumatoid Arthritis Comorbidities. Rheumatology and Arthritis.
11:18–23. 2022.(In Chinese).
|
|
3
|
Avina-Zubieta JA, Thomas J, Sadatsafavi M,
Lehman AJ and Lacaille D: Risk of incident cardiovascular events in
patients with rheumatoid arthritis: A meta-analysis of
observational studies. Ann Rheum Dis. 71:1524–1529. 2012.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Chen JL, Jin YB, Wang YF, Zhang XY, Li J,
Yao HH, He J and Li C: Clinical characteristics and risk factors of
cardiovascular disease in patients with elderly-onset rheumatoid
arthritis: A large cross-sectional clinical study. Beijing Da Xue
Xue Bao Yi Xue Ban. 52:1040–1047. 2020.PubMed/NCBI View Article : Google Scholar : (In Chinese).
|
|
5
|
Erum U, Ahsan T and Khowaja D: Lipid
abnormalities in patients with rheumatoid arthritis. Pak J Med Sci.
33:227–230. 2017.PubMed/NCBI View Article : Google Scholar
|
|
6
|
He M, Liu J, Xin L, Han X, Sun Y and Zhang
Y: Changes and correlation analysis of lipoprotein metabolism in
patients with active rheumatoid arthritis. Rheumatism and
Arthritis. 9:7–11. 2020.(In Chinese).
|
|
7
|
Liu L, Yu XF and Zong RK: Change in
Apolipoprotein of Patients with Rheumatoid Arthritis in Active
Phase and Correlation Analysis. Chin J Rehabilitation. 24:95–97.
2009.(In Chinese).
|
|
8
|
Atzeni F, Turiel M, Caporali R, Cavagna L,
Tomasoni L, Sitia S and Sarzi-Puttini P: The effect of
pharmacological therapy on the cardiovascular system of patients
with systemic rheumatic diseases. Autoimmun Rev. 9:835–839.
2010.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Navarro-Millán I, Charles-Schoeman C, Yang
S, Bathon JM, Bridges SL Jr, Chen L, Cofield SS, Dell'Italia LJ,
Moreland LW, O'Dell JR, et al: Changes in lipoproteins associated
with methotrexate or combination therapy in early rheumatoid
arthritis: Results from the treatment of early rheumatoid arthritis
trial. Arthritis Rheum. 65:1430–1438. 2013.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Liu J, Wan L, Huang CB, Wang Y, Pan YZ and
Xie XL: Effect of Xinfeng capsule on lipoprotein metabolism of
rheumatoid arthritis patients. Zhongguo Zhong Xi Yi Jie He Za Zhi.
35:1060–1064. 2015.PubMed/NCBI
|
|
11
|
Guo J, Liu J, He L, Ling X, Zhou Q, Huang
D and Song Q: Clinical data and association rules of the
combination of the external application of furong ointment and the
oral administration of herbal medicines for active rheumatoid
arthritis. World Journal of Integrated Medicine. 13:608–612.
2018.(In Chinese).
|
|
12
|
Liu J, Han M, Fang Z and Cui Y: Clinical
study on the treatment of rheumatoid arthritis with Xinfeng
capsule. Chin J Integrated Traditional and Western Med. 202–205.
2001.(In Chinese).
|
|
13
|
Tan B, Liu J and Zhang P: XingFeng capsule
alleviates hypercoagulable state in knee osteoarthritis patients by
inhibiting NF-κB signaling pathway. Immunol J. 32:781–803. 2016.(In
Chinese).
|
|
14
|
Tan B, Liu J, Zhang PH, Fang L and Zhu FB:
Effect of Xinfeng capsule in improving blood stasis state of OA
patients. Zhongguo Zhong Xi Yi Jie He Za Zhi. 36:1449–1455.
2016.PubMed/NCBI(In Chinese).
|
|
15
|
Bao B, Liu J, Wan L, Zhang Y, Long Y and
Sun G: Xinfeng capsule inhibits immune inflammation in
osteoarthritis by inhibiting the miR23a-3p/PETN/PI3K/AKT/mTOR
pathway. Nan Fang Yi Ke Da Xue Xue Bao. 41:483–494. 2021.PubMed/NCBI View Article : Google Scholar : (In Chinese).
|
|
16
|
Lin Z, Wang Y, Huang C, Zhang W, Wang G,
Chen R, Sun Y and Gong X: Clinical Effect of Xinfeng Capsule on
Patients with Rheumatoid Arthritis and Vascular Endothelial Growth
Factor and Tumor Necrosis Factor-α. Clin Res Traditional Chin Med.
13:91–94. 2021.(In Chinese).
|
|
17
|
Liu J, Liu X and Han M: Xinfeng Capsule in
the treatment of 20 cases of active rheumatoid arthritis. J Anhui
College of Traditional Chin Med. 3:12–16. 2003.(In Chinese).
|
|
18
|
Jiang H, Liu J, Meng M, Dai M and Dong L:
The toxicity of continuous perfusion of Xinfeng capsule in rats.
Chin J Clin Health Care. 19:72–78. 2016.(In Chinese).
|
|
19
|
Huang C, Liu J, Chen X, Wang Y, Zhang W,
Chen R, Wang G and Fan H: Observation on the curative effect of
Xinfeng capsule in treating rheumatoid arthritis. Chin J Integrated
Traditional Chin Western Med. 33:1599–1602. 2013.(In Chinese).
|
|
20
|
Hou A, Liu J, Guo J and Ling X: Clinical
study of Huangqin Qingre Chubi Capsule on improving SOD and immune
inflammatory blood indicators in RA patients. J Jinzhou Med Univ.
40:12–16+117. 2019.(In Chinese).
|
|
21
|
Xu C, Cao Y and Huang C: A parallel
comparative study of Huangqin Qingre Chubi capsule combined with
methotrexate in the treatment of active rheumatoid arthritis.
Guangming Traditional Chin Med. 37:3569–3572. 2022.(In
Chinese).
|
|
22
|
Ding B, Huang C, Fu P and Chen L: Clinical
Observation on the Treatment of 30 Cases of Rheumatoid Arthritis
with Damp heat Obstruction Syndrome with Huangqin Qingre Chubi
Capsule and Damp heat Obstruction Waixi Formula. J Gansu Univ
Traditional Chin Med. 39:53–57. 2022.(In Chinese).
|
|
23
|
Guo J, Liu J, Zhang X, Zhou Q and Huang D:
Huangqin Qingre Chubi Capsule regulates PPAR-γ/Effect of CD36/MnSOD
axis on oxidative stress in patients with rheumatoid arthritis. J
Beijing Univ Traditional Chin Med. 45:201–207. 2022.(In
Chinese).
|
|
24
|
Meng M, Duan FE, Wang XY, Chen L, Wei L
and Wuxi L: A preliminary study on the fingerprint of Xinfeng
capsule with Astragalus as a reference. Clin J Tradit Chin Med.
23:545–547+565. 2011.(In Chinese).
|
|
25
|
Wu M, Duan F, Fenge D and Wang X:
Preliminary study on reference fingerprint of Xinfeng capsule.
CJTCM. 23:545–547. 2011.(In Chinese).
|
|
26
|
Hu Shun Li: Classified and Integrated
Pharmacokinetic Study of Multipe Effective Components Contained in
XinfengCapsule. Anhui Univ Chin Med, 2015 (In Chinese).
|
|
27
|
Liu C, Liu X, Liu J, Zhang Y, Wang U and
Zhou A: Preliminary study on HPLC fingerprint of Huangqin Qingre
Chubi Capsule and determination of three components. China Med
Biotechnol. 17:56–58. 2022.(In Chinese).
|
|
28
|
Dong X, Gan P, Ke J, Chen F, Wu H, Chen J
and Liu J: Simultaneous determination of six active components in
Huangqin Qingre Chubi Capsule by UHPLC-MS/MS. Anhui Univ
Traditional Chin Med News. 40:97–102. 2021.(In Chinese).
|
|
29
|
Chang C, Zhang R, Shi Y and Ho TL:
Research progress in the treatment of rheumatoid arthritis with
traditional Chinese medicine [J/OL]. Chin J Traditional Chin Med.
10:1–8. 2022.(In Chinese).
|
|
30
|
Aletaha D, Neogi T, Silman AJ, Funovits J,
Felson DT, Bingham CO III, Birnbaum NS, Burmester GR, Bykerk VP,
Cohen MD, et al: 2010 Rheumatoid arthritis classification criteria:
An American College of Rheumatology/European league Against
Rheumatism collaborative initiative. Ann Rheum Dis. 69:1580–1588.
2010.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Zhu J, Gao R, Zhao P, Lu G, Zhao D and Li
J: Guidelines for the prevention and treatment of dyslipidemia in
Chinese adults(2016)Revised edition. Chin J Circulation.
31:937–950. 2016.(In Chinese).
|
|
32
|
Lai KW, Zhang L, Chen Y, Chen Y, Wang X
and Wu D: The application of propensity scoring method in
observational research. Chin J Evidence Based Med. 21:469–474.
2021.(In Chinese).
|
|
33
|
Wang J: Analysis of clinical efficacy and
feasibility of Baihu-Guizhi Decoction in the treatment of
rheumatoid arthritis with moist heat arthralgia spasm syndrome.
China Modern Medicine Application. 16:204–206. 2022.(In
Chinese).
|
|
34
|
Zhang C, Yin X, Mei Y and Deng A: Efficacy
of Shuanghe Decoction in Treating Acute Stage of Rheumatoid
Arthritis (Syndrome of Phlegm and Stasis Blockade). Chin J
Emergency. 30:1237–1240. 2021.(In Chinese).
|
|
35
|
Zhao H, Zhang H, Guo D and Zhang X:
Effects of Duhuo Jisheng Decoction on Th17/Treg Balance in
Rheumatoid Arthritis of Liver-kidney Insufficiency, Cold-dampness
Obstruction Pattern. Western Chin Med. 34:8–12. 2021.(In
Chinese).
|
|
36
|
Tong T: Clinical efficacy of Yiyiren
decoction in the treatment of rheumatoid arthritis. Asia Pacific
Traditional Medicine. 10:123–124. 2014.(In Chinese).
|
|
37
|
Wang K: Clinical observation on Modified
Simiao Powder in the treatment of rheumatoid arthritis. Chin Med
Sci. 8:54–56. 2018.(In Chinese).
|
|
38
|
Wen J, Liu J, Wan L, Ling X, Dong W and
Fang Y: A cohort study of endpoint events in 1468 patients with
rheumatoid arthritis. J of Anhui Universityof Trad Chin Med.
36:2017.(In Chinese).
|
|
39
|
Wang F, Dai G and Lou H: The follow-up
design of the evidence-based TCM cohort study. Shandong J
Traditional Chin Med. 35:14–17. 2016.(In Chinese).
|
|
40
|
Fang Y, Liu J, Wan L, Ling X, Dong W and
Wen J: The formulas of cohort study of rheumatoid arthritis with
spleen wet application. Chin J Clin Healthc. 21:2018.(In
Chinese).
|
|
41
|
Du H and Chen H: Effect of follow-up by
phone call on medication compliance of patients with cancer pain.
Clin Nursing. 13:2014.(In Chinese).
|
|
42
|
Mantel N: Evaluation of survival data and
two new rank order statistics arising in its consideration. Cancer
Chemother Rep. 50:163–170. 1966.PubMed/NCBI
|
|
43
|
Sun Y, Jian L, Ling X, Wan L, Wen J, Fang
Y and Dong W: Risk factors of changes of RBC parameters in 2716
patients with rheumatoid arthritis and anemia based on Logistic
regression analysis. Chin J Immunol. 35:2019.(In Chinese).
|
|
44
|
Chi M, Hou X, Zhou Yu and Chen X: Design
optimization of data acquisition scheme based on Apriori
association rules mining of test data. Fire and Command and
Control. 47:142–149. 2022.(In Chinese).
|
|
45
|
Sun D: Research on Web Data Mining
Technology Based on Apriori Algorithm. Information Technol
Informatization. 91–94. 2022.(In Chinese).
|
|
46
|
Xie J, Wang N, Ding R, Guo J, Xin L and
Liu J: Association learning of Chinese herbal medicines and disease
treatment efficacy. Int J Prod Res. 57:683–702. 2019.(In
Chinese).
|
|
47
|
Shi D, DiStefano C, McDaniel HL and Jiang
Z: Examining Chi-Square test statistics under conditions of large
model size and ordinal data. Structural Equation Modeling: A
Multidisciplinary J. 25:924–945. 2018.(In Chinese).
|
|
48
|
Mcinnes IB and Schett G: The pathogenesis
of rheumatoid arthritis. N Engl J Med. 365:2205–2219.
2011.PubMed/NCBI View Article : Google Scholar
|
|
49
|
Petrelli F, Mariani FM, Alunno A and
Puxeddu I: Pathogenesis of rheumatoid arthritis: One year in review
2022. Clin Exp Rheumatol. 40:475–482. 2022.PubMed/NCBI View Article : Google Scholar
|
|
50
|
Montecucco F, Favari E, Norata GD, Ronda
N, Nofer JR and Vuilleumier N: Impact of systemic inflammation and
autoimmune diseases on ApoAI and HDL plasma levels and functions.
Handb Exp Pharmacol. 224:455–482. 2015.PubMed/NCBI View Article : Google Scholar
|
|
51
|
Pan L, Wang T and Wang L: Characteristics
of Blood Lipid Disorder in Patients with Rheumatoid Arthritis and
Its Correlation with Disease Activity. Chin J Arterioscler.
24:54–58. 2016.(In Chinese).
|
|
52
|
Eneuve E, Nam J and Emery P: 2010
ACR-EULAR classification criteria for rheumatoid arthritis. Rev
Bras Reumatol. 50:481–483. 2010.PubMed/NCBI
|
|
53
|
Toms TE, Panoulas VF, Douglas KM,
Nightingale P, Smith JP, Griffiths H, Sattar N, Symmons DP and
Kitas GD: Are lipid ratios less susceptible to change with systemic
inflammation than individual lipid components in patients with
rheumatoid arthritis? Angiology. 62:167–175. 2011.PubMed/NCBI View Article : Google Scholar
|
|
54
|
Xie X, Liu J, Sheng C and Wan L: Protein
metabolism changes and correlation in active rheumatoid arthritis.
Chin J Clin Health. 13:15–18. 2010.(In Chinese).
|
|
55
|
Spîrchez M, Samasca G, Lancu M, Bolba C
and Miu N: Relationof interleukin-6, TNF-alpha and interleukin-1
alpha with disease activity and severity in juvenile idiopathic
arthritis patients. Clin Lab. 58:253–260. 2012.PubMed/NCBI
|
|
56
|
Mingyu H, Liu J, Ling X, et al:
Lipoprotein metabolism changes and correlation analysis in patients
with active rheumatoid arthritis. Rheumatol Arthritis. 9:7–11.
2020.(In Chinese).
|
|
57
|
Duan S, Liu J, Zhang F and Xin L: Mining
the effect of Chinese spleen invigorating drugs on immune
inflammation in patients with rheumatoid arthritis based on
association rules. Chin J Clin Health. 20:96–99. 2017.(In
Chinese).
|
|
58
|
Dong W, Liu J, Xin L, Fang Y and Wen J: To
study the effect of Tripterygium wilfordii polyglycosides tablets
combined with traditional Chinese medicine on immune inflammatory
liver and kidney function in patients with rheumatoid arthritis
based on data mining. Chinese J Trad Chin Med. 44:3526–3532.
2019.(In Chinese).
|
|
59
|
Guo J, Liu J, Xin L, Huang D, Zhou Q and
Song Q: To evaluate the effect of Furong ointment combined with
traditional Chinese medicine on inflammatory indexes in patients
with active rheumatoid arthritis based on random walking model.
Chin J Immunol. 34:854–860. 2018.(In Chinese).
|
|
60
|
Sun Y, Liu J, Ling X, Zhang Y, Long Y, Bao
B and Sun G: Data mining research on Huangqin Qingre Chubi Capsule
combined with Xinfeng Capsule to improve the immune inflammatory
indicators of rheumatoid arthritis patients with damp heat
syndrome. Rheumatol Arthritis. 9:5–9. 2020.(In Chinese).
|
|
61
|
Chiu HE, Hong YC, Chang KC, Shih CC, Hung
JW, Liu CW, Tan TY and Huang CC: Favorable circulatory system
outcomes as adjuvant traditional Chinese medicine (TCM) treatment
for cerebrovascular diseases in Taiwan. PLoS One.
9(e86351)2014.PubMed/NCBI View Article : Google Scholar
|
|
62
|
Dong W, Liu J, Wan L, Ling X, Fang Y and
Wen J: Cohort study on the occurrence of endpoint events during
follow-up of rheumatoid arthritis patients treated with traditional
Chinese medicine. Rheumatol Arthritis. 7:18–22. 2018.(In
Chinese).
|
|
63
|
Samhouri BF, Vassallo R, Achenbach SJ,
Kronzer VL, Davis JM III, Myasoedova E and Crowson CS: Incidence,
risk factors, and mortality of clinical and subclinical rheumatoid
arthritis-associated interstitial lung disease: A population-based
cohort. Arthritis Care Res (Hoboken): Jan 7, 2022 (Epub ahead of
print).
|
|
64
|
Miura T, Miyakoshi N, Kashiwagura T,
Tsuchie H, Sugimura Y and Shimada Y: The association between
comorbidities and disease activity in patients with rheumatoid
arthritis: A multicenter, cross-sectional cohort study in Japan
with the highest proportion of elderly individuals. Egypt Rheumatol
Rehabil. 49:2022.(In Chinese).
|
|
65
|
Liu J, Yu X and Zong R: Change and
correlation analysis of apolipoprotein in active rheumatoid
arthritis. China Rehabilitation. 24:95–97. 2009.(In Chinese).
|
|
66
|
Guo J, Liu J, Sun Z and Zhang X: Analysis
of prescription drug use pattern of traditional Chinese medicine
for rheumatic arthritis based on data mining. Pharmacol Clin
Traditional Chin Med. 36:258–264, 65. 2020.(In Chinese).
|
|
67
|
Wen J, Xin L, Wan L, Fang Y, Dong W and
Liu J: Evaluation of the effect of Chinese spleen strengthening
unit therapy on inflammatory indicators of patients with
osteoarthritis based on random walking model. Chin J Traditional
Chin Med. 44:1053–1057. 2019.PubMed/NCBI View Article : Google Scholar : (In Chinese).
|
|
68
|
Huang DN, Wu FF, Zhang AH, Sun H and Wang
XJ: Efficacy of berberine in treatment of rheumatoid arthritis:
From multiple targets to therapeutic potential. Pharmacol Res.
169(105667)2021.PubMed/NCBI View Article : Google Scholar
|
|
69
|
Bua S, Lucarini L, Micheli L, Menicatti M,
Bartolucci G, Selleri S, Di Cesare Mannelli L, Ghelardini C, Masini
E, Carta F, et al: Bioisosteric Development of multitarget
nonsteroidal anti-inflammatory drug-carbonic anhydrases inhibitor
hybrids for the management of rheumatoid arthritis. J Med Chem.
63:2325–2342. 2020.PubMed/NCBI View Article : Google Scholar
|
|
70
|
Fang Y, Liu J, Xin L, Sun Y, Wan L, Huang
D, Wen J, Zhang Y and Wang B: Identifying compound effect of drugs
on rheumatoid arthritis treatment based on the association rule and
a random walking-based model. Biomed Res Int.
2020(4031015)2020.PubMed/NCBI View Article : Google Scholar
|
|
71
|
Wang KX, Gao Y, Lu C, Li Y, Zhou BY, Qin
XM, Du GH, Gao L, Guan DG and Lu AP: Uncovering the complexity
mechanism of different formulas treatment for rheumatoid arthritis
based on a novel network pharmacology model. Front Pharmacol.
11(1035)2020.PubMed/NCBI View Article : Google Scholar
|
|
72
|
Zhang L: Research on the clinical
medication rule and mechanism of traditional Chinese medicine for
rheumatism based on data mining [D]. Beijing University of
Traditional Chinese Medicine, 2019 (In Chinese).
|
|
73
|
Zhang W, Han D and Li J: Research progress
on chemical constituents and pharmacological effects of
Alismatis Rhizoma. J Traditional Chin Med. 49:98–102.
2021.(In Chinese).
|
|
74
|
Chen Q: Research progress of
Plantaginis Herb. Electronic J Cardiovascular Diseases of
Integrated Traditional Chinese and Western Med. 7:151–152. 2019.(In
Chinese).
|
|
75
|
Yu K, Sun Y, Xue L, He J, Li F, Yin M, Li
Z, Yan X, Guo J, Li G and Wang C: Compounds with NO inhibitory
effect from the Rattan stems of Sinomenium acutum, a kind of
Chinese folk medicine for treating rheumatoid arthritis. Chem
Biodivers. 19(e202200334)2022.PubMed/NCBI View Article : Google Scholar
|
|
76
|
Hu H, Zhu Y, Yu C, Yuan B, Chen X, Guan Y,
Deng y and Shao F: Effects of hawthorn, cassia seed and
Alismatis Rhizoma extracts on blood lipid level, liver
function and HMGCR expression in hyperlipidemia rats. Chin Patent
Med. 43:2830–2834. 2021.(In Chinese).
|
|
77
|
Li B and Geng G: Research Progress on
Chemical Constituents and Pharmacological Effects of Astragalus.
Research on Integrated Traditional Chinese and Western Medicine.
14:262–264. 2022.(In Chinese).
|
|
78
|
Tao X, Yan Y, Xu Z, Li H and Lei X: Study
on Anti-inflammatory and detumescence Effect of coix seed Oil. J
Liaoning Univ Traditional Chin Med. 17:45–46. 2015.(In
Chinese).
|
|
79
|
Xu L and Ho TY: Research progress in the
efficacy and mechanism of Tripterygium wilfordii and its
derivatives on rheumatoid arthritis. Shi Zhen Traditional Chin Med.
33:1703–1706. 2022.(In Chinese).
|
|
80
|
Ji L, Lv S and Yang Z: Research progress
on chemical constituents and pharmacological effects of centipede.
Specialty Research. 42:75–84. 2020.(In Chinese).
|
|
81
|
Faming T, Liu Y, Chen M and Hu W:
Experimental study on the anti-inflammatory effect of triptenide in
rats with adjuvant arthritis. New Traditional Chinese Medicine
Drugs And Clinical Medicine. 25:176–178. 2014.(In Chinese).
|
|
82
|
Ge P, Zhang H, Sun X, Liu J, Wang X, Jiang
H and Meng M: Effect of Huangqin Qingre Chubi Capsule on serum IL-1
in adjuvant arthritis rats β And IL-6. New Chin Med Clin Pharmacol.
25:8–10. 2014.(In Chinese).
|
|
83
|
Guo J: Data mining study of improving SOD
in rheumatoid arthritis patients and its influence on
AMPK-FoxO3a-MnSOD signaling pathway [D]. Hefei: Anhui University of
Traditional Chinese Medicine, 2018 (In Chinese).
|
|
84
|
Sun Y, Liu J, Ling X, Zhang Y, Long Y, Bao
B and Sun G: Data mining study on the improvement of immune
inflammation index in patients with rheumatoid arthritis by Xinfeng
Capsule. Rheumatism and Arthritis. 9:5–9. 2020.(In Chinese).
|
|
85
|
Liu J, Wang Y, Huang C, Xu J, Li Z, Xu L,
He L, Sun Y, Wang Y, Xu S, et al: Efficacy and safety of Xinfeng
capsule in patients with rheumatoid arthritis: A multi-center
parallel-group double-blind randomized controlled trial. J Tradit
Chin Med. 35:487–498. 2015.PubMed/NCBI View Article : Google Scholar
|
|
86
|
Cao Y and Liu J: Clinical Efficacy of
Heat-clearing and Diuresis-promoting Prescription Combined with
Western Medicine Treatment for Damp-heat Rheumatoid Arthritis. J
Anhui Univ Traditional Chin Med. 33:19–21. 2014.(In Chinese).
|