Introduction
Achalasia is a neurodegenerative disease affecting
the inhibitory neurons in the myenteric plexus, which synthesize
nitric oxide and vasoactive intestinal peptide The inhibitory
neurons in the muscular layer of the esophagus are affected by
chronic inflammation and/or an autoimmune process, which leads to
aganglionosis (1). The consequence
of this defect is the incomplete relaxation and high pressure of
the lower esophageal sphincter (LES) and the impaired peristalsis
of the esophagus (2).
Over time, technical advances have allowed a shift
from conventional esophageal manometry to high-resolution manometry
(HRM) devices, increasing the diagnostic accuracy in esophageal
motor disorders (3). By increasing
the number of recording sites and reducing the space between them,
either by water-perfused catheters or incorporated pressure
sensors, esophageal HRM offers a functional mapping of the
esophagus (3). HRM has been
successfully used in adults, and it has led to the Chicago
Classification (CC) of esophageal motor disorders (3). Soon after the studies in adults,
pediatric studies followed (2).
However, the small number of cases in the pediatric population
makes it more difficult to standardize this procedure (2). HRM is a valuable tool in this age
group, being easily and quickly performed, with good accuracy in
identifying abnormal esophageal motor patterns (2).
The management of achalasia in children depends on
the clinical experience and available diagnostic investigations in
different centers (4). Access to
esophageal HRM is still lacking in numerous parts of the world. In
the past year, the Clinical Emergency Hospital for Children
(Cluj-Napoca, Romania) had the opportunity to collaborate with
colleagues from an adult gastroenterology department in order to
diagnose achalasia in suspected pediatric cases using esophageal
HRM.
The most effective therapeutic options in children
with achalasia are pneumatic dilation and Heller myotomy
(laparoscopic or classic) (2).
Peroral endoscopic myotomy (POEM) is a relatively new procedure
that is being used more frequently in children (2); however, there are only a few centers
in the world where this treatment procedure is available (4).
The present study aimed to analyze the data from the
first children diagnosed with achalasia using esophageal HRM,
thanks to a collaboration between the Third Pediatric Department,
Clinical Emergency Hospital for Children and the Gastroenterology
Department, Second Medical Clinic, Emergency Clinical County
Hospital, in Cluj-Napoca, Romania. A series of 7 cases is reported,
which were evaluated between March 2021 and May 2022. The clinical
data and results of the investigations are reviewed. All patients
were assessed using conventional manometry and/or esophageal HRM.
Both types of investigation were performed without sedation of the
patients, after a fasting period of 8 to 12 h. We also present the
treatment procedures applied in these patients and the immediate
complications after the treatment.
Case series
Patients
The patients included in this study were sent to the
Third Pediatric Department, Clinical Emergency Hospital for
Children, Cluj-Napoca from all across Romania with the suspicion of
achalasia. The present study included pediatric patients diagnosed
with achalasia with HRM and to which a treatment procedure was
already applied after being diagnosed with HRM. Patients who were
not assessed with HRM and were only diagnosed based on conventional
manometry were excluded. In addition, patients who were not yet
treated after being diagnosed with HRM were excluded from the
study.
Clinical data
Table I describes
the clinical and demographic data of the patients. All the patients
were newly diagnosed with achalasia, except for case 4 who had been
previously diagnosed and was admitted to the Third Pediatric
Department, Clinical Emergency Hospital for Children, 2 months
after treatment with bougie dilation.
 | Table IDemographic, clinical and laboratory
data of the patients. |
Table I
Demographic, clinical and laboratory
data of the patients.
| Charateristics | Case 1 | Case 2 | Case 3 | Case 4 | Case 5 | Case 6 | Case 7 |
|---|
| Demographic data | | | | | | | |
|
Age,
years | 13 | 17 | 11 | 17 | 14 | 13 | 17 |
|
Sex | Male | Female | Male | Male | Male | Female | Male |
| Clinical
variables | | | | | | | |
|
BMI
(percentile, Z score), kg/m2 | 20.1 (69th,
0.50) | 17.5 (6th,
-1.54) | 22.7 (93rd,
1.47) | 20.2 (29th,
-0.54) | 13.5 (0,
-3.98) | 17.0 (22nd,
-0.79) | 19.9 (30th,
-0.51) |
|
Disease
evolution, months | 4 | 7 | 12 | 24 | 12 | 24 | 6 |
|
Chest
pain | Yes | No | Yes | Yes | No | Yes | Yes |
|
Dysphagia
for solids | Yes | Yes | Yes | No | Yes | Yes | Yes |
|
Dysphagia
for liquids | Yes | Yes | Yes | Yes | Yes | No | Yes |
|
Regurgitations | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
|
Heartburn | Yes | No | No | Yes | No | Yes | No |
|
Cough | No | Yes | No | No | No | Yes | No |
|
Weight
loss | No | Yes | No | No | Yes | Yes | Yes |
|
Eckardt
score | 6 | 6 | 5 | 5 | 7 | 11 | 6 |
| Laboratory data and
preoperative diagnostic studies | | | | | | | |
|
Neutrophil
to lymphocyte ratio | 1.15 | 5.39 | 2.82 | 1.47 | 0.58 | 0.88 | 1.66 |
|
Barium
swallow-dilation of the esophagus, mm | 40.0 | 30.0 | 50.0 | 37.0 | -a | -a | 34.8 |
|
Histopathology
exam of the biopsy fragments from the esophagus | No changes | 3rd grade
esophagitis | Esophageal
candidosis | 1st grade
esophagitis | Not performed | 1st grade
esophagitis | 3rd grade
esophagitis |
In all patients, the Eckardt score was calculated
(5). This score assesses the
presence and frequency (occasionally, daily or after each meal) of
dysphagia, regurgitation and chest pain, and the weight loss
(<5, 5-10, and >10 kg) (5).
For each parameter and its severity, the patients received a score
between 0 and 3. The maximum value of the Eckardt score is
12(5).
The male patient described as case 1 first presented
with dysphagia for solids and then for fluids. No weight loss was
recorded and development had been normal. The patient had been
diagnosed with bronchial asthma at 2 years of age and had no family
medical history of digestive or autoimmune diseases.
The female patient described as case 2 had
experienced weight loss of 6 kg in the 7 months since symptom
onset. No data regarding any significant family health history was
found, and there was no previous personal medical history.
Regarding the male patient described as case 3, the
patient's mother had autoimmune thyroiditis with hyperthyroidism
and vitiligo. The antithyroid peroxidase antibodies of the patient
were slightly increased, yet normal thyroid function was
recorded.
Case 4 was a male patient previously diagnosed with
autoimmune thyroiditis. A diagnosis of achalasia had been made 2
years before presenting to the department. The patient was treated
using bougie dilation, but dysphagia, regurgitations and thoracic
pain reappeared 2 months after this procedure. No weight loss was
exhibited and none of the family members had been diagnosed with
chronic diseases.
In the patients described as cases 2 and 4, total
antinuclear antibodies were assessed, and the results were
negative.
Cases 5, 6 and 7 had no family medical background or
personal medical history of autoimmune disorders. The male patient
described as case 5 had experienced weight loss of 3 kg in 3 weeks.
The female patient described as case 6 had experienced weight loss
of 15 kg in 6 months, and had the highest Eckardt score (5) of all of the patients. The male
patient described as case 7 also presented with weight loss of 4.5
kg in 6 months.
Investigations
The neutrophil to lymphocyte ratio was calculated in
all patients, by dividing the neutrophil count by the lymphocyte
count. Normal ranges were considered between 0.99 and 1.76(6). The ratio was assessed based on the
results of the complete blood count obtained in the evaluation
preceding treatment. Venous blood samples were collected from the
patients in tubes with dipotassium ethylenediamine tetraacetic acid
(concentration, 1.2-2.0 mg/ml blood). The complete blood count
parameters were analyzed by an automatic hematological analyzer,
the LabXpert 6800 (Shenzhen Mindray Bio-medical Electronics Co.
Ltd.). The results are included in Table I. The mean ± SD value of all
patients was 1.99±1.66 and the median was 1.47.
All patients were evaluated with a barium swallow,
and they all presented with a ‘bird's beak’ appearance of the
esophagus. The dilation of the esophagus was also measured in most
of the patients, and the maximum value of these measurements is
included in Table I. All patients
underwent an upper digestive endoscopy and, in most of them, biopsy
fragments were taken from the esophagus. The results are summarized
in Table I.
Conventional esophageal manometry. A total of
4 patients were also investigated using conventional esophageal
manometry. The device used for conventional manometry had a water
perfusion system and was a Model PIP 48220S5 (Mui Scientific). The
measured parameters were as follows: Resting pressure of the LES
and upper esophageal sphincter (UES); amplitude, duration and
length of the peristaltic waves in the esophageal body; and
relaxation of the LES after wet swallows. The resting pressure of
the LES in the 4 patients who were initially investigated with
conventional esophageal manometry ranged between 44 and 50 mmHg,
and that of the UES ranged between 55 and 80 mmHg. Relaxations of
the LES were incomplete in all the patients. Patients had absent
peristalsis in the esophageal body. Low amplitude waves were
recorded in the esophageal body (20-30 mmHg). Most of these waves
were measured with no propagation along the esophagus.
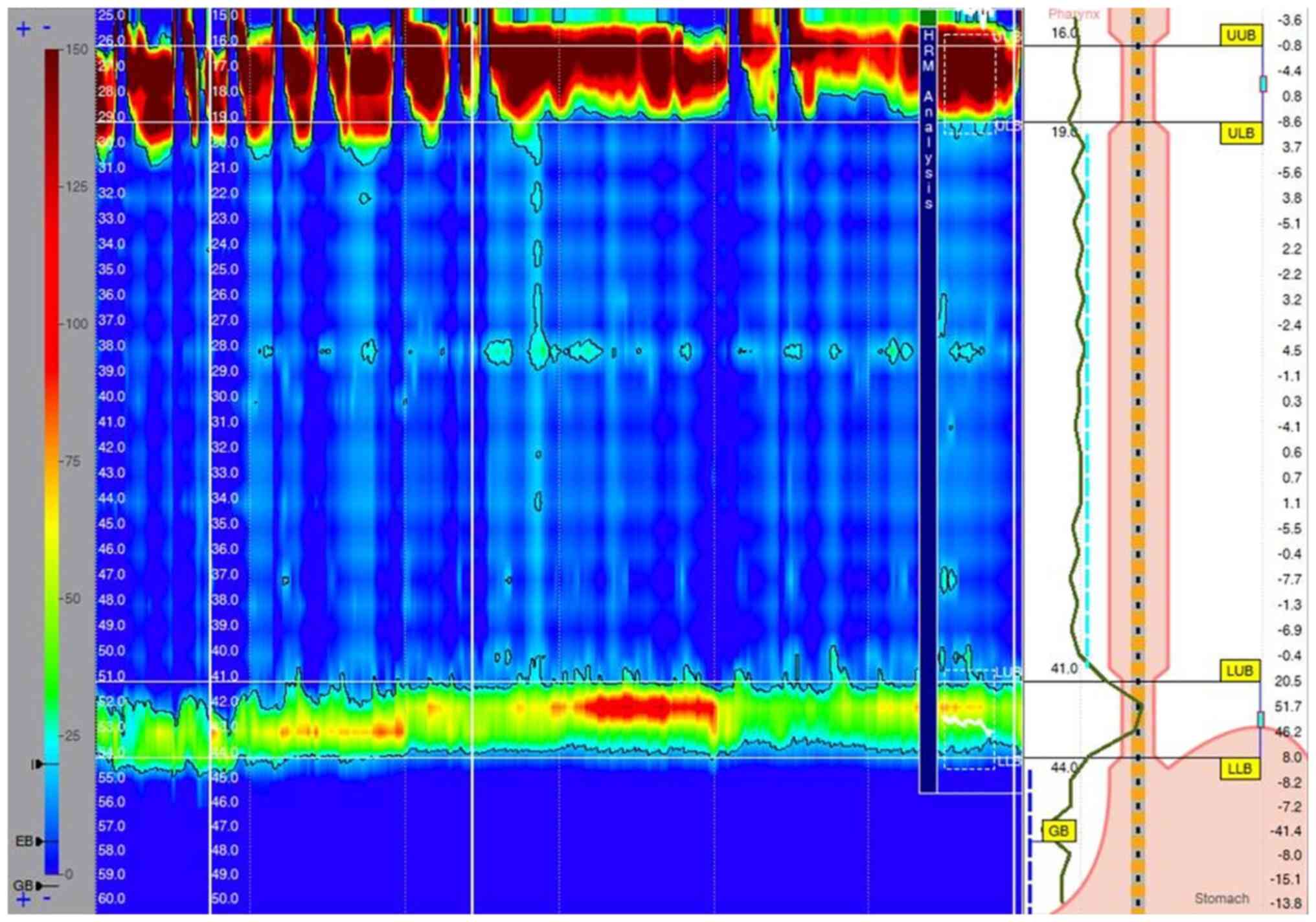
Esophageal HRM. Esophageal HRM recordings
were performed in the Gastroenterology Department, Second Medical
Clinic, Emergency Clinical County Hospital (Cluj-Napoca, Romania)
for all of the aforementioned patients. The system used was the
ISOLAB HR manometry system (Standard Instruments GmbH) attached to
a solid-state catheter (Unisensor AG) with 36 sensors. The catheter
was inserted transnasally and positioned with ≥3 sensors in the
stomach. After a baseline recording of 2 min, 10 wet 5-ml swallows,
spaced 30 sec apart, were performed. The manometry was performed in
the supine position with the thorax angulated at 30˚. The upper
normal limit for integrated relaxation pressure (IRP), measured
using the Unisensor AG probe, was set at 28 mmHg, according to the
CC of esophageal motility disorders v3.0 criteria used at the time
of diagnosis (5). The main
parameters measured during esophageal HRM (Table II) were IRP and the number of
swallows followed by pan-esophageal pressurization.
 | Table IIResults of the high-resolution
esophageal manometry, achalasia subtype, treatment and immediate
complications after the treatment. |
Table II
Results of the high-resolution
esophageal manometry, achalasia subtype, treatment and immediate
complications after the treatment.
| Case | Case 1 | Case 2 | Case 3 | Case 4 | Case 5 | Case 6 | Case 7 |
|---|
| Resting pressure of
the LES, mmHg | 95.10±23.92 | 102.26±12.05 | 60.55±22.85 | 35.89±4.80 | 66.93±12.49 | 57.16±5.77 | 44.96±7.92 |
| Median IRP,
mmHg | 61 | 82 | 50 | 28 | 60 | 47 | 40 |
| Peristalsis | 6/8 swallows with
panesophageal pressurization | 3/10 swallows with
panesophageal pressurization | 6/10 swallows with
panesophageal pressurization | No
pressurization | 6/9 swallows with
panesophageal pressurization | 2/9 swallows with
panesophageal pressurization | No
pressurization |
| Resting pressure of
the UES, mmHg | 218.65±57.40 | 147.42±54.47 | 393.10±144.27 | 202.43±98.28 | 222.18±64.13 | 167.84±49.70 | 243.49±27.88 |
| Achalasia
subtype | II | II | II | I | II | II | I |
| Previous
treatment | No | No | No | Dilation with
bougies | No | No | No |
| Treatment | POEM | POEM | POEM | Pneumatic
dilation | Pneumatic
dilation | POEM | Pneumatic
dilation |
| Immediate
complications after the treatment | Minimal
pneumoperitoneum | Mild
pneumomediastinum | Minimal
pneumoperitoneum | None | None | None | None |
| Medical treatment
after the procedure | PPI | PPI | PPI | None | None | PPI | PPI |
Cases 1-3 and cases 5 and 6 had increased resting
LES pressure, increased IRP and pan-esophageal pressurization, and
were classified as having type II achalasia based on the CC v3.0
classification of esophageal motility disorders. A representative
wet swallow recorded for case 1 is presented in Fig. 1, and several swallows of case 2 are
presented in Figs. 2 and 3. In the fourth case (Fig. 4), esophageal HRM was performed
after endoscopic dilation. In this case, the resting LES pressure
was normal, the IRP was at the upper normal limit (28 mmHg) and
there was no pan-esophageal pressurization. These measurements
would be compatible with type I achalasia, according to the CC v3.0
classification, but this classification is intended to be used for
patients who were not previously treated.
The treatment options and immediate complications
after the treatment are also depicted in Table II.
Patients were/are followed up at 1, 6 and 12 months
(for patients who were treated more recently, these data are
incomplete). Clinical data were/are assessed at all visits. At 6
and 12 months, the patients were/are evaluated using upper
digestive endoscopy and esophageal pH/impedance monitoring. In
total, 2 patients (cases 2 and 4) were transferred to an adult
gastroenterologist within 5 and 4 months, respectively, after the
procedure due to Romanian legislation only allowing a pediatrician
to follow patients until 18 years of age. Since the results of the
follow-up assessments are yet to be available for all of the
patients, they were not reported in the present study.
The present study was approved by the Ethics
Committee of ‘Iuliu Hațieganu’ University of Medicine and Pharmacy
(Cluj-Napoca, Romania) and written informed consent was obtained
from both the parents of the patients and the patients
themselves.
Discussion
Achalasia is an uncommon esophageal motor disorder
that is rare in children (2).
Although, its diagnosis has progressed markedly with the advent of
esophageal HRM, there are few centers globally in which there is
experience with new investigation methods and treatment options in
children with achalasia (4).
Therefore, the aim of the present study was to highlight the
particularities of the diagnosis of pediatric achalasia based on
esophageal HRM, as well as its treatment, by contributing data from
a series of cases recruited from across Romania.
The CC of esophageal motility disorders is based on
the changes of the parameters assessed by HRM (3). However, the CC was conceived for
adults, and there is still debate as to whether it can be applied
in children (3).
Evaluating patients using esophageal HRM is
essential, as the therapeutic approach and prognosis are different
in the various subtypes of achalasia (3). Certain parameters determined in HRM
are dependent on the age and length of the esophagus (7). A total of 7 patients, aged <18
years, were diagnosed with achalasia in our University Center and
their cases reported in the present study. Evaluation of children
with HRM was performed in the Gastroenterology Department, Second
Medical Clinic, Emergency Clinical County Hospital (Cluj-Napoca,
Romania). A total of 6 patients were newly diagnosed and had no
previous treatment, while one patient had already received dilation
with bougies (with esophageal HRM having been performed after this
procedure), but had persisting symptoms.
The symptom duration was between 4 months and 2
years in the newly diagnosed patients, and 2 years in the patient
who had already received bougie endoscopic dilation (case 4).
Dysphagia for solids and liquids was the most frequently reported
symptom in the patients. Patel et al (8) found that weight loss in adult
patients was correlated with phenotype, as patients with type II
disease were more likely to have weight loss than type I. It was
also noted that patients with a longer duration of symptoms did not
have any weight loss. It was hypothesized that this was due to a
lack of adaptation in patients with a shorter disease course. In
the present study, 3 of the patients (cases 2, 6 and 7) had weight
loss of between 4.5 and 15 kg in a period of 6-7 months.
In studies on a large number of patients, Nurko
(9,10) found that 80% of children present
with vomiting (most probably regurgitation, but interpreted as
vomiting by parents), 76% with dysphagia, 61% with weight loss, 44%
with respiratory symptoms (more frequent in younger ages), 38% with
thoracic pain, 31% with growth failure and 21% with nocturnal
regurgitations. All of the patients in the present study presented
with dysphagia, a cough was present in 2 patients and 1 patient
reported bothersome nocturnal regurgitations.
The Eckardt score (5) is used in adult patients to evaluate
the severity of achalasia. It has been argued that it has been
developed for adults and that it does not take into consideration
the impact of the disease on growth or insufficient weight gain
(2,4). The etiology and physiopathology of
achalasia are not fully understood. Studies showing autoantibodies
against the myenteric plexus and infiltration of Auerbach's plexus
predominantly with CD8+ T lymphocytes suggest an
autoimmune mechanism in patients with achalasia (1). A study conducted by Romero-Hernández
et al (11) identified an
autoimmune disease in 16.7% of the adult patients with achalasia,
and 68.4% of these patients had a familial history of autoimmunity.
A positive family background for autoimmune diseases was identified
in 1 patient in the present study (case 3), as the mother had been
diagnosed with autoimmune thyroiditis with hyperthyroidism and
vitiligo. This patient had a slightly increased number of
antithyroid peroxidase antibodies. Another patient (case 4) has
been diagnosed with autoimmune thyroiditis. The neutrophil to
lymphocyte ratio has been reported as increased in adult patients
with achalasia compared with that in healthy controls (12). In the current study, 2 of the
patients (cases 2 and 3) had higher values (5.39 and 2.82,
respectively) of this parameter than the mean value reported in
healthy controls by López-Verdugo et al (12) The patients described as cases 5 and
6 had a neutrophil to lymphocyte ratio <1. As compared with
cases 2 and 3, cases 5 and 6 had higher Eckardt scores (7 and 11,
respectively). There was no difference between these two categories
of patients regarding the subtype of achalasia. Case 2 had the
highest LES pressure and IRP. van Lennep et al (4) performed a survey regarding current
practices in managing pediatric achalasia. Access and experience in
esophageal HRM limit its use in children with achalasia, and only
one-third of the responders in this survey would change their
therapeutic approach based on the evaluation by HRM and achalasia
subtype.
Achalasia is a chronic, progressive disease, and
treatment does not currently provide a cure (10). At present, the treatment options
available are aimed at reducing the obstruction caused by the
incomplete relaxation of the LES (10). Choosing the right treatment option
can be challenging. The latest guidelines regarding management of
achalasia in adults state that pneumatic endoscopic dilation,
laparoscopic Heller myotomy and POEM are equally effective in type
I and II achalasia, while POEM would be a better treatment option
for type III achalasia, as it allows a more extensive myotomy
(13). In children, there is no
clear consensus thus far.
The novel therapeutic approach, POEM, was utilized
in 4 of the patients described in the present study. POEM was first
used in 2008 as a treatment option for adults with achalasia
(14). A total of 14 years later,
an increasing number of centers are reporting good results from
this procedure in children affected by achalasia. In a review by
van Lennep et al (4), POEM
was available in children in only 11 (29%) of the reporting
centers; 7 in Europe, 3 in North America and 1 in Asia. As opposed
to Heller myotomy, POEM has the advantage of a shorter time needed
for the procedure, a lower rate of complications and a shorter time
spent in the hospital (15). The
long-term clinical success rate of POEM in children with achalasia
is higher than in adults, as shown by a meta-analysis by Zhong
et al (16). The main
long-term complication after POEM is gastroesophageal reflux
disease (GERD). Inoue et al (17) suggested in a pilot study that
completing POEM with endoscopic fundoplication might reduce the
incidence of GERD. Given the high risk of GERD after POEM (in up to
60% of cases), the current guidelines for adults recommend
endoscopic monitoring for GERD, and lifelong proton pump inhibitor
therapy after POEM (18). GERD
appears to be equally common as in adults after POEM in children
after 4 years of follow-up, as reported in the study by Nabi et
al (19). In systematic
reviews, Sharp and St Peter (20)
and Goneidy et al (21)
concluded that no treatment option can yet be considered a standard
in children with achalasia, as comparative data are still lacking.
Goneidy et al (21)
documented reports of 94 patients who underwent POEM. Even though
the success rate has been shown to be high for this procedure
(99.3%), it is nonetheless a new technique, and data regarding
long-term follow-up are inconsistent (21). In the current study, the
complication rate after this procedure was higher compared with
that after Heller myotomy and endoscopic esophageal dilatation
(24.4 vs. 12.8 and 5%, respectively). In the patients of the
present study, adverse events after POEM were minor and resolved
spontaneously (2 patients had a pneumoperitoneum and 1 had a
pneumomediastinum).
Miao et al (22) reported observations on 21 patients
diagnosed with achalasia, with a mean age of 5.5 years. All the
patients were treated with POEM. Only one-half of the children were
assessed by esophageal manometry (22). The mean pressure of the resting LES
was 25.4 mmHg, with a range between 18.5 and 40 mmHg, which was
lower than the values detected in the patients in the present
study. It was suggested that POEM should be performed as soon as
possible, before causing distension of the esophagus, since the
complete incision of the circular muscle seemed to be therapeutic
in children (22). In a more
recent study, 17/19 patients (89%) experienced sustained
symptomatic relief after POEM (23). As concluded by a recent review
(24), POEM is a promising
technique in the pediatric population, with a high efficacy and low
rate of adverse events.
The clinical data and results of the investigations
in 7 children with achalasia were reviewed in the present study,
which is a small number of cases. A total of 4 patients were
evaluated with both conventional and esophageal HRM. Both of these
methods evaluate the motor function of the esophagus, but
esophageal HRM allows a more accurate description of the relaxation
of the LES and a global assessment of peristalsis (9).
There are still few centers with all the necessary
resources (both technical and human) to evaluate and treat children
with achalasia properly. The merit of the present study is that it
demonstrates the novel investigations and treatment options
currently available for children with achalasia. The 4 children
with type II achalasia were the first patients treated with POEM in
Cluj-Napoca in which a subtype was also established with esophageal
HRM. The results from the present study and other studies (15,16,19-22,24,25)
support this treatment option for children with achalasia. The team
that contributed to the management of the patients in the present
study comprised multiple specialists: Pediatric gastroenterologists
(who performed the diagnostic endoscopy and conventional esophageal
manometry), gastroenterologists specializing in adults (including
one trained in POEM and pneumatic dilation), radiologists and a
nurse who performed the esophageal HRM. POEM has been performed in
adults in the center since 2013(26) and in children since 2016(25). A significant limitation of the
present case series is its small number of subjects. The patients
were not investigated for previous viral infections, and
investigations for autoimmune disorders were incomplete. In
addition, the follow-up data of the patients were not reported. The
study will be completed in the future, with follow-up clinical data
of the patients and surveillance endoscopy and esophageal
pH-impedance monitoring for GERD included in an upcoming study.
In summary, the first cases of pediatric patients in
our Cluj-Napoca, Romania, diagnosed with achalasia using esophageal
HRM were reported in the present study. POEM was successfully
performed in 4 children with type II achalasia, with only minor
adverse events after the procedure.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
DP made substantial contributions to the conception
and design of the study, acquisition of clinical data and
conventional esophageal manometry results, analysis and
interpretation of the data, drafting of the manuscript, and
ensuring that questions of accuracy or integrity of the work were
appropriately investigated and resolved. RP also made a substantial
contribution to the conception and design of the study, as well as
the acquisition of clinical data, conventional esophageal manometry
results and high-resolution esophageal manometry results, analysis
and interpretation of the data. TB performed the high-resolution
esophageal manometries, analyzed and interpreted the results,
selected the images and contributed to the critical revision of
intellectual content. LD performed the high-resolution esophageal
manometries, and analyzed and interpreted the results. CA performed
the barium-swallow tests in the patients and interpreted the
images. DD performed the high-resolution esophageal manometries,
analyzed and interpreted the results, and revised the work for
important intellectual content. MT performed the peroral endoscopic
myotomy and pneumatic dilatations in the patients, and also revised
the work for important intellectual content. DF made a substantial
contribution to the conception and design of the study, and the
acquisition, analysis and interpretation of the data, revised the
work for important intellectual content, and ensured that questions
of accuracy or integrity of the work were appropriately
investigated and resolved. DP and DF confirm the authenticity of
all the raw data. All authors have read and approved the final
manuscript.
Ethics approval and consent to
participate
The present study was approved by the Ethics
Committee of 'Iuliu Hațieganu' University of Medicine and Pharmacy
(Cluj-Napoca, Romania) and written informed consent was obtained
from the parents of the patients (approval no AVZ80; approval date,
28.03.2022).
Patient consent for publication
Written informed consent for the publication of the
data was obtained from the parents of the patients and from the
patients.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Furuzawa-Carballeda J, Aguilar-León D,
Gamboa-Domínguez A, Valdovinos MA, Nuñez-Álvarez C,
Martín-del-Campo LA, Enríquez AB, Coss-Adame E, Svarch AE,
Flores-Nájera A, et al: Achalasia-An autoimmune inflammatory
disease: A cross-sectional Study. J Immunol Res.
2015(729217)2015.PubMed/NCBI View Article : Google Scholar
|
|
2
|
van Lennep M, van Wijk MP, Omari TIM,
Benninga MA and Singendonk MMJ: Clinical management of pediatric
achalasia. Expert Rev Gastroenterol Hepatol. 12:391–404.
2018.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Kahrilas PJ, Bredenoord AJ, Fox M, Gyawali
CP, Roman S, Smout AJ and Pandolfino JE: International High
Resolution Manometry Working Group. The chicago classification of
esophageal motility disorders, v3.0. Neurogastroenterol Motil.
27:160–174. 2015.PubMed/NCBI View Article : Google Scholar
|
|
4
|
van Lennep M, van Wijk MP, Omari TIM,
Salvatore S, Benninga MA and Singendonk MMJ: European Society for
Paediatric Gastroenterology, Hepatology and Nutrition Motility
Working Group. Clinical management of pediatric achalasia: A survey
of current practice. J Pediatr Gastroenterol Nutr. 68:521–526.
2019.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Eckardt VF, Aignherr C and Bernhard G:
Predictors of outcome in patients with achalasia treated by
pneumatic dilation. Gastroenterology. 103:1732–1738.
1992.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Moosmann J, Krusemark A, Dittrich S, Ammer
T, Rauh M, Woelfle J, Metzler M and Zierk J: Age- and sex-specific
pediatric reference intervals for neutrophil-to-lymphocyte ratio,
lymphocyte-to-monocyte ratio, and platelet-to-lymphocyte ratio. Int
J Lab Hematol. 44:296–301. 2022.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Singendonk MM, Smits MJ, Heijting IE, van
Wijk MP, Nurko S, Rosen R, Weijenborg PW, Abu-Assi R, Hoekman DR,
Kuizenga-Wessel S, et al: Inter- and intrarater reliability of the
Chicago Classification in pediatric high-resolution esophageal
manometry recordings. Neurogastroenterol Motil. 27:269–276.
2015.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Patel DA, Naik R, Slaughter JC,
Higginbotham T, Silver H and Vaezi MF: Weight loss in achalasia is
determined by its phenotype. Dis Esophagus. 31:1–8. 2018.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Nurko S: Motility Disorders in Children.
Pediatr Clin North Am. 64:593–612. 2017.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Nurko S: The Esophagus: motor disorders.
In: Pediatric Gastrointestinal disease. Walker WA (ed). B.C. Decker
Inc, Philadelphia, PA, pp317-350, 2000.
|
|
11
|
Romero-Hernández F, Furuzawa-Carballeda J,
Hernández-Molina G, Alejandro-Medrano E, Núñez-Álvarez CA,
Hernández-Ramírez DF, Azamar-Llamas D, Olivares-Martínez E, Breña
B, Palacios A, et al: Autoimmune comorbidity in achalasia patients.
J Gastroenterol Hepatol. 33:203–208. 2018.PubMed/NCBI View Article : Google Scholar
|
|
12
|
López-Verdugo F, Furuzawa-Carballeda J,
Romero-Hernández F, Coss-Adame E, Valdovinos MA, Priego-Ranero A,
Olvera-Prado H, Narváez-Chavez S, Peralta-Figueroa J and
Torres-Villalobos G: Hematological indices as indicators of silent
inflammation in achalasia patients: A cross-sectional study.
Medicine (Baltimore). 99(e19326)2020.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Vaezi MF, Pandolfino JE, Yadlapati RH,
Greer KB and Kavitt RT: ACG clinical guidelines: Diagnosis and
management of achalasia. Am J Gastroenterol. 115:1393–1411.
2020.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Inoue H, Minami H, Kobayashi Y, Sato Y,
Kaga M, Suzuki M, Satodate H, Odaka N, Itoh H and Kudo S: Peroral
endoscopic myotomy (POEM) for esophageal achalasia. Endoscopy.
42:265–271. 2010.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Lee Y, Brar K, Doumouras AG and Hong D:
Peroral endoscopic myotomy (POEM) for the treatment of pediatric
achalasia: A systematic review and meta-analysis. Surg Endosc.
33:1710–1720. 2019.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Zhong C, Tan S, Huang S, Peng Y, Lü M and
Tang X: Clinical outcomes of peroral endoscopic myotomy for
achalasia in children: A systematic review and meta-analysis. Surg
Endosc. 34(doaa112)2021.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Inoue H, Ueno A, Shimamura Y, Manolakis A,
Sharma A, Kono S, Nishimoto M, Sumi K, Ikeda H, Goda K, et al:
Peroral endoscopic myotomy and fundoplication: A novel NOTES
procedure. Endoscopy. 51:161–164. 2019.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Oude Nijhuis RAB. Zaninotto G, Roman S,
Boeckxstaens GE, Fockens P, Langendam MW, Plumb AA, Smout A,
Targarona EM, Trukhmanov AS, et al: European guidelines on
achalasia: United European Gastroenterology and European Society of
Neurogastroenterology and Motility recommendations. United European
Gastroenterol J. 8:13–33. 2020.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Nabi Z, Ramchandani M, Basha J, Goud R,
Darisetty S and Reddy DN: POEM is a durable treatment in children
and adolescents with Achalasia Cardia. Front Pediatr.
10(812201)2022.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Sharp NE and St Peter SD: Treatment of
idiopathic achalasia in the pediatric population: A systematic
review. Eur J Pediatr Surg. 26:143–149. 2016.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Goneidy A, Cory-Wright J, Zhu L and
Malakounides G: Surgical management of esophageal achalasia in
pediatrics: A systematic review. Eur J Pediatr Surg. 30:13–20.
2020.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Miao S, Wu J, Lu J, Wang Y, Tang Z, Zhou
Y, Huang Z, Ying H and Zhou P: Peroral endoscopic myotomy in
children with achalasia: A relatively long-term single-center
study. J Pediatr Gastroenterol Nutr. 66:257–262. 2018.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Tashiro J, Petrosyan M and Kane TD:
Current management of pediatric achalasia. Transl Gastroenterol
Hepatol. 6(33)2021.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Mencin AA, Sethi A, Barakat MT and Lerner
DG: Peroral endoscopic myotomy (POEM) in children: A state of the
art review. J Pediatr Gastroenterol Nutr. 75:231–236.
2022.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Choné A, Familiari P, von Rahden B, Desai
P, Inoue H, Shimamura Y, Eleftheriadis N, Yamashita K, Khashab MA,
Shiwaku H, et al: Multicenter evaluation of clinical efficacy and
safety of per-oral endoscopic myotomy in children. J Pediatr
Gastroenterol Nutr. 69:523–552. 2019.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Tefas C, Boroș C, Ciobanu L, Surdea-Blaga
T, Tanțău A and Tanțău M: POEM: Five years of experience in a
single East European Center. J Gastrointestin Liver Dis.
29:323–328. 2020.PubMed/NCBI View Article : Google Scholar
|