Introduction
Proximal humerus fracture has a prevalence of 5-10%
and is among the 10 most frequent fractures in the adult population
(1-3).
Proximal fracture of the humerus comprises humeral head fracture,
fractures of the anatomical as well as surgical neck, and fractures
of the greater and lesser tubercles (4). More severe and complex fracture cases
may involve all of these parts of the humerus and are coupled with
subluxation of the humeroscapular joint (4,5).
These types of fracture are largely caused by low-intensity trauma
and are more common in older women due to underlying osteoporosis
(6,7).
Current treatment strategies for proximal humerus
fracture range from conservative treatment to surgical management
comprising open reduction along with internal fixation,
arthroplasty, intramedullary nailing and minimal invasive
percutaneous plate osteosynthesis (8-10).
It has been indicated that quality of life (QOL)-related outcomes
are improved with surgical management, compared to conservative
treatment. However, the comparative efficiency of various surgical
modalities has remained to be determined (11). The deltopectoral (DP) approach is
one of the most common methods of open reduction and internal
fixation. However, this approach involves substantial dissection of
the soft tissue and retraction of the muscle to gain access to the
lateral aspect of the humerus (12,13).
As an alternative approach, deltoid splitting (DS) is comparatively
less invasive; however, studies suggested that the DS approach may
be associated with an increased risk of damage to the blood supply
of the humerus and on certain occasions, may also injure the
axillary nerve (8,10,14).
Schematics illustrating these two surgical approaches are provided
in Fig. 1.
There is still no consensus regarding which of these
two surgical modalities is more clinically efficacious and
associated with fewer complications. A systematic review by Xie
et al (15) that included
six studies [three randomized controlled trials (RCTs) and three
prospective follow-up studies] indicated that the risk of avascular
necrosis (AVN) of the humeral head was significantly lower in
patients receiving DS surgery. Furthermore, the duration of surgery
was lower in the DS group as compared to the DP approach. No
statistically significant differences were reported for other
outcomes, such as the complication rate and functional outcome. The
present study conducted a comprehensive search and included all the
contemporary studies relevant for this review. The intent was to
provide a reliable and updated evidence on the issue at hand. The
review by Xie et al (15)
included only six studies whereas the present study identified and
included 14 studies. Some of these studies have been conducted
after the review by Xie et al (15) was published (n=5) and some of them
were published before the review by Xie et al (15) but the review did not include those
studies. Relevant details of the included studies have been
presented later in the manuscript. Additionally, the present study
also provided pooled estimates on important outcomes that were not
considered in the review by Xie et al (15), such as the range of movement and
time to bone union. There is a need to provide updated evidence on
this issue and, therefore, the main goal of the current
meta-analysis was to include all relevant studies comparing
outcomes of DP and DS surgeries in patients with proximal humerus
fracture.
Materials and methods
Search strategy
The protocol of the study was registered in the
International Prospective Registry of Systematic Reviews
(registration no. CRD42021290759). The Preferred Reporting Items
for Systematic Reviews and Meta-analyses 2020 guidelines were
followed while conducting the literature review (16). A systematic thorough search, using
a pre-defined and pilot-tested search strategy, was performed in
the PubMed, Scopus, EMBASE and Cochrane Central Register of
Controlled Trials databases for papers published in the English
language until 31 January 2023. The following search strategy was
used: ‘deltoid-split approach OR deltopectoral approach’ AND
‘humerus fracture OR proximal humerus fracture’ AND ‘outcomes OR
functional outcomes OR complications OR blood loss OR operative
time’. Studies that compared the outcomes of interest among
patients with proximal humerus fractures that were managed using DS
and DP approaches were identified. The primary outcome of interest
included functional outcomes such as constant shoulder score (CSS)
and disabilities of the arm, shoulder and hand (DASH) score.
Secondary outcomes of interest included risk of complications,
range of movement in the postoperative period, pain, QOL,
activities of daily living (ADL) score, duration of surgery, blood
loss during surgery, length of hospital stay and time required for
bone union.
Selection criteria and methods
The studies identified by the literature search were
retrieved and duplicates were removed. Titles and abstracts were
then screened by two authors, followed by a review of the full
texts of the remaining studies. Disagreements were resolved through
discussions among the authors. Reference lists of the included
studies were also reviewed to identify additional relevant
manuscripts.
The inclusion criteria were as follows: i) RCT and
observational studies including case-control studies; ii) studies
with prospective follow-ups and retrospective studies that analysed
data using clinical records; iii) studies that involved patients
with fracture of the proximal humerus and reported relevant
outcomes based on DS and DP surgical approaches.
Exclusion criteria were as follows: i) Case-reports
or review articles; ii) studies that did not report findings based
on the two management modalities (DS and DP); iii) studies that did
not report the outcomes of interest.
Data extraction and quality
assessment
Data from the included studies were extracted
independently by two authors using a pretested data extraction
sheet. The quality of the included studies was assessed
independently by two authors using the Newcastle-Ottawa Quality
Assessment Scale for observational studies (17).
Statistical analysis
STATA version 16.0 (StataCorp LP) was used for
statistical analysis. Pooled relative risk (RR) was used for
categorical outcomes. For continuous outcomes, weighted mean
difference (WMD) was used where the outcomes were reported on the
same scales. In instances where outcomes were reported based on
assessment using different tools/scales, e.g. pain scores, standard
mean difference (SMD) was used to report pooled effect sizes. All
effect sizes were reported along with 95% CIs. For all the
analyses, I2 was used to measure heterogeneity. In cases
of I2 >40%, the random-effects model was used
(18). P<0.05 was considered to
indicate a statistically significant difference. Egger's test was
used to detect publication bias (19).
Results
Selection of articles, study
characteristics and quality of the included studies
A total of 288 citations were identified by the
systematic literature search after removing any duplicates
(Fig. 2). An additional 249
citations were excluded based on the screening of the titles and
abstracts. Full texts of the remaining 39 studies were read and 25
studies were excluded. Finally, a total of 14 studies were
considered for inclusion (20-33).
The details of the 14 studies included are presented in Table I. There were seven prospective
studies, four RCTs and three retrospective studies. A total of four
studies were conducted in Germany, two in India and one each in
Switzerland, Turkey, Canada, Croatia, China, South Korea, Thailand
and Taiwan. The mean follow-up period ranged from 12-47 months. The
results of the quality evaluation indicated that the studies were
of modest to good quality (Table
SI).
 | Table ICharacteristics of the studies
included in the meta-analysis. |
Table I
Characteristics of the studies
included in the meta-analysis.
| First author(s),
year | Study design | Country | Participant
characteristics | Sample size | Timing of reporting
of outcomes/follow-up period | (Refs.) |
|---|
| Borer et al,
2020 | Prospective
follow-up | Switzerland | -Median age, 64 years
-Females, 75% -Majority with two- or three-parts fracture, 85%
-Mean BMI, 26.6 kg/m2 | DS (n=39); DP
(n=23) | Outcomes reported at
minimum 1-year follow-up Median follow-up, 47 months | (30) |
| Büyükkuşcu et
al, 2020 | Prospective
follow-up | Turkey | -Mean age, 48 years
-Males, 60% | DS (n=21); DP
(n=27) | Mean follow-up,18
months | (29) |
| Rouleau et
al, 2020 | RCT | Canada | -Mean age, 62 years
-Females, 78% -Varus displacement, 70% -Mean BMI, 21
kg/m2 | DS (n=44); DP
(n=41) | Mean follow-up, 26
months | (32) |
| Vijayvargiya et
al, 2016 | Prospective
follow-up | India | -Mean age, 46 years
-Majority were males, (58%) -Time between injury and operation, ~7
days Neer's type 3 fracture, 46% | DS (n=13); DP
(n=13) | Minimum follow-up,
≥6 months | (27) |
| Bandalović et
al, 2014 | Prospective
follow-up | Croatia | -Patients aged
>65 years -All with closed proximal humerus fracture | DS (n=25) DP
(n=42) | Mean follow-up,
14.7 months | (24) |
| Bhayana et
al, 2021 | Prospective
follow-up | India | -Mean age, 45 years
-Majority were males, 66% -Patients with either Neer's type 3 or 4
fracture | DS (n=42) DP
(n=42) | Mean follow-up, 23
months | (33) |
| Buecking et
al, 2014 | RCT | Germany | -Mean age, ~68
years; -Females, 77% -Neer's type 3 or 4 fracture, 75% | DS (n=60) DP
(n=60) | Mean follow-up, 12
months | (23) |
| Zhao et al,
2017 | RCT | China | -Mean age, 64 years
-Male, 58.3% -Mean BMI, 25.9 kg/m2 -All with either
Neer's type 2 or 3 fracture | 17 DS 19 DP | Mean follow-up, 12
months | (28) |
| Martetschläger
et al, 2012 | RCT | Germany | -Mean age, ~58
years -Male, 49% -Neer's type 3 or 4 fracture (87%) | DS (n=37) DP
(n=33) | Mean follow-up, 33
months | (22) |
| Hepp et al,
2008 | Prospective | Germany | -Median age, 65
years -Female, 77% -Majority with Neer's type 2 or 3 fracture
-Right upper limb was affected in the majority of cases | DS (n=39) DP
(n=44) | Follow-up at 3, 6
and 12 months post- operatively | (20) |
| Fischer et
al, 2016 | Prospective | Germany | -Mean age, ~60
years -Females, 65% -AO fracture classification, B/C (78%) | DS (n=20) DP
(n=30) | Follow-up, ~24
months | (26) |
| Kim et al,
2020 | Retrospective
analysis of medical records | South Korea | -Mean age, 68 years
-Females, 85% -All with either Neer type 2 or 3 fracture | DS (n=39) DP
(n=38) | Mean follow-up, ~16
months Outcomes assessed at 12 months post-operative period | (31) |
| Siripong et
al, 2015 | Retrospective
analysis of medical records | Thailand | -Age range, 50-60
years -Females, 57% -All with either Neer type 2 or 3 fracture | DS (n=12) DP
(n=16) | Follow up period
not reported in the study | (25) |
| Wu et al,
2011 | Retrospective
analysis | Taiwan | -Mean age, 58
years; -Females, 75% -With high energy injury, ≥60% -Type C
fracture, 42% | DS (n=28) DP
(n=32) | Minimum follow-up,
24 months Mean follow-up, 32 months | (21) |
Functional outcomes
Compared with patients treated using the DP
approach, those treated with the DS approach had an improved
shoulder function, as indicated by the CSS at 3 months post-surgery
(WMD 6.36; 95% CI, 1.06 to 11.65; n=2; I2=30.6%)
(Fig. 3). There was no significant
difference between the DP and the DS groups in the CSS at 6 (WMD
1.52; 95% CI, -4.27 to 7.31; n=2; I2=82.0%], 12 (WMD
1.27; 95% CI, -1.67 to 4.22; n=6; I2=85.5%) and 24
months (WMD 3.25; 95% CI, -1.88 to 8.38; n=5; I2=86.6%)
after the surgery (Fig. 3).
Furthermore, there were no statistically significant differences in
the DASH scores between the two groups at 3 (WMD -2.90; 95% CI,
-8.74 to 2.94; n=1), 12 (WMD 0.29; 95% CI, -0.62 to 1.19; n=3;
I2=57.8%) and 24 months (WMD 3.27; 95% CI, -2.87 to
9.41; n=4; I2=73.8%) post-surgery (Fig. 3). The ADL score was significantly
improved in the DS group, compared with that in the DP group, at 3
(WMD 1.23; 95% CI, 0.40 to 2.06; n=2; I2=44.2%), 6 (WMD
0.99; 95% CI, 0.72 to 1.25; n=2; I2=0.0%) and 12 months
(WMD 0.83; 95% CI, 0.18 to 1.47; n=2; I2=38.5%) after
the operation (Table II). At 24
months, there was only one study reporting the ADL score, and it
did not indicate any difference between the two groups of patients.
The pooled effect size for the range of movement (degrees) at the
latest follow-up (the reported mean follow-up was 12-26 months in
the included studies) was comparable between the two groups in
terms of external rotation (WMD 0.09; 95% CI, -0.31 to 0.48; n=4;
I2=9.3%), internal rotation (WMD 0.33; 95% CI, -0.08 to
0.75; n=3; I2=0.0%) and abduction (WMD -1.73; 95% CI,
-5.83 to 2.38; n=3; I2=97.2%) (Table II). Similarly, no significant
differences were noted between the two groups in physical (WMD
2.10; 95% CI, -4.81 to 9.01; n=3; I2=82.9%) and mental
components (WMD 0.52; 95% CI, -10.93 to 11.97; n=2;
I2=87.5%) of the QOL score 24 months after the surgery
(Table II). Publication bias was
not detected for any of the functional outcomes (P>0.05; data
not shown) using Egger's test.
 | Table IIOutcomes in subjects undergoing
deltoid-splitting approach, compared to deltopectoral approach. |
Table II
Outcomes in subjects undergoing
deltoid-splitting approach, compared to deltopectoral approach.
| Outcome | Number of
studies | Pooled effect
size | I2,
% |
|---|
| Duration of
surgery, min | 10 | WMD -16.44 (95% CI,
-25.25 to -7.63)a | 98.0 |
| Duration of
hospital stay, days | 4 | WMD -0.04 (95% CI,
-0.28 to 0.21) | 49.6 |
| Blood loss, ml | 5 | WMD -57.99 (95% CI,
-102.74 to -13.23)a | 87.3 |
| Time to union,
weeks | 4 | WMD -1.66 (95% CI,
-2.30 to -1.02)a | 94.4 |
| QOL (physical
component), 24 months | 3 | WMD 2.10 (95% CI,
-4.81 to 9.01) | 82.9 |
| QOL (mental
component), 24 months | 2 | WMD 0.52 (95% CI,
-10.93 to 11.97) | 87.5 |
| Range of movement
(degrees) at latest follow-up | | | |
|
External
rotation | 4 | WMD 0.09 (95% CI,
-0.31 to 0.48) | 9.3 |
|
Internal
rotation | 3 | WMD 0.33 (95% CI,
-0.08 to 0.75) | 0.0 |
|
Abduction | 3 | WMD -1.73 (95% CI,
-5.83 to 2.38) | 97.2 |
| Activity of daily
living score | | | |
|
Within 3
months | 2 | WMD 1.23 (95% CI,
0.40 to 2.06)a | 44.2 |
|
At 6
months | 2 | WMD 0.99 (95% CI,
0.72 to 1.25)a | 0.0 |
|
At 12
months | 2 | WMD 0.83 (95% CI,
0.18 to 1.47)a | 38.5 |
|
At 24
months | 1 | WMD 0.00; 95% CI,
(-0.30 to 0.30) | - |
Additional outcomes
The DS approach was associated with a comparatively
lower duration of surgery (in minutes) (WMD -16.44; 95% CI, -25.25
to -7.63; n=10; I2=98.0%) and the amount of blood loss
(in ml) (WMD -57.99; 95% CI, -102.74 to -13.23; n=5;
I2=87.3%) (Table II).
Time to bone union (in weeks) (WMD -1.66; 95% CI, -2.30 to -1.02;
n=4; I2=94.4%) was also lower in the patients that
received the DS approach treatment. The duration of hospital stay
(in days) (WMD -0.04; 95% CI, -0.28 to 0.21; n=4;
I2=49.6%) was similar in both groups (Table II). There were no statistically
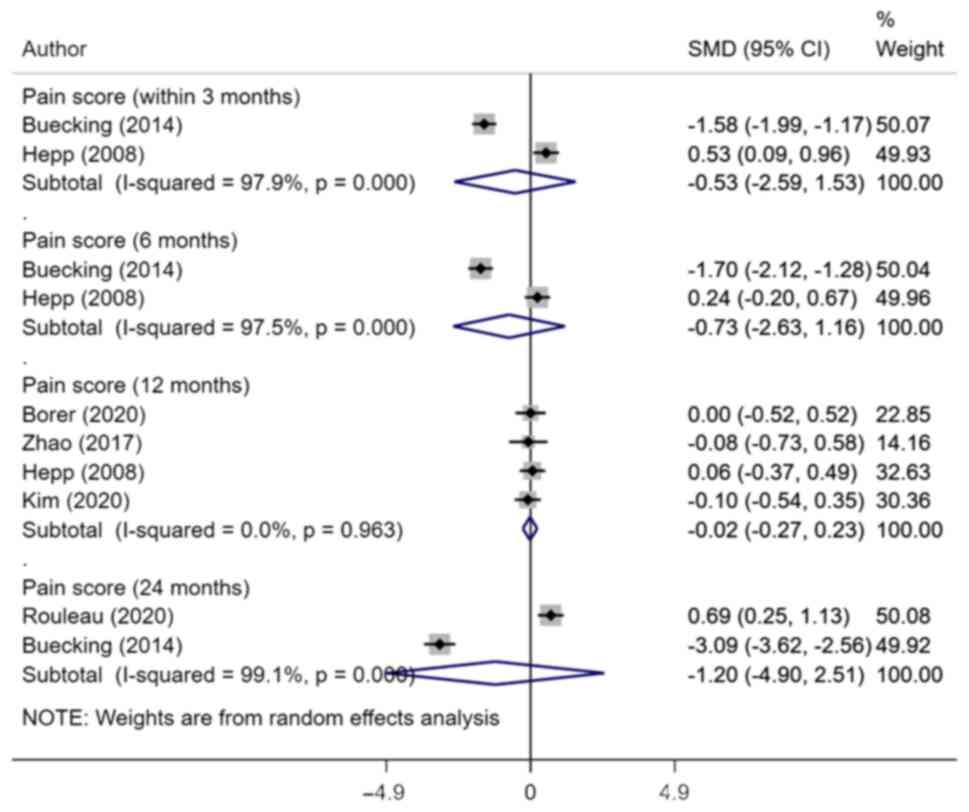
significant differences in the pain scores between the two groups
at 3 (SMD -0.53; 95% CI, -2.59 to 1.53; n=2; I2=97.9%),
6 (SMD -0.73; 95% CI, -2.63 to 1.16; n=2; I2=97.5%), 12
(SMD -0.02; 95% CI, -0.27 to 0.23; n=4; I2=0.0%) and 24
months (SMD -1.20; 95% CI, -4.90 to 2.51; n=2; I2=99.1%)
post-surgery (Fig. 4). We found no
statistical evidence of publication bias for the above-mentioned
outcomes on Egger's test (P>0.05; data not shown).
Complications
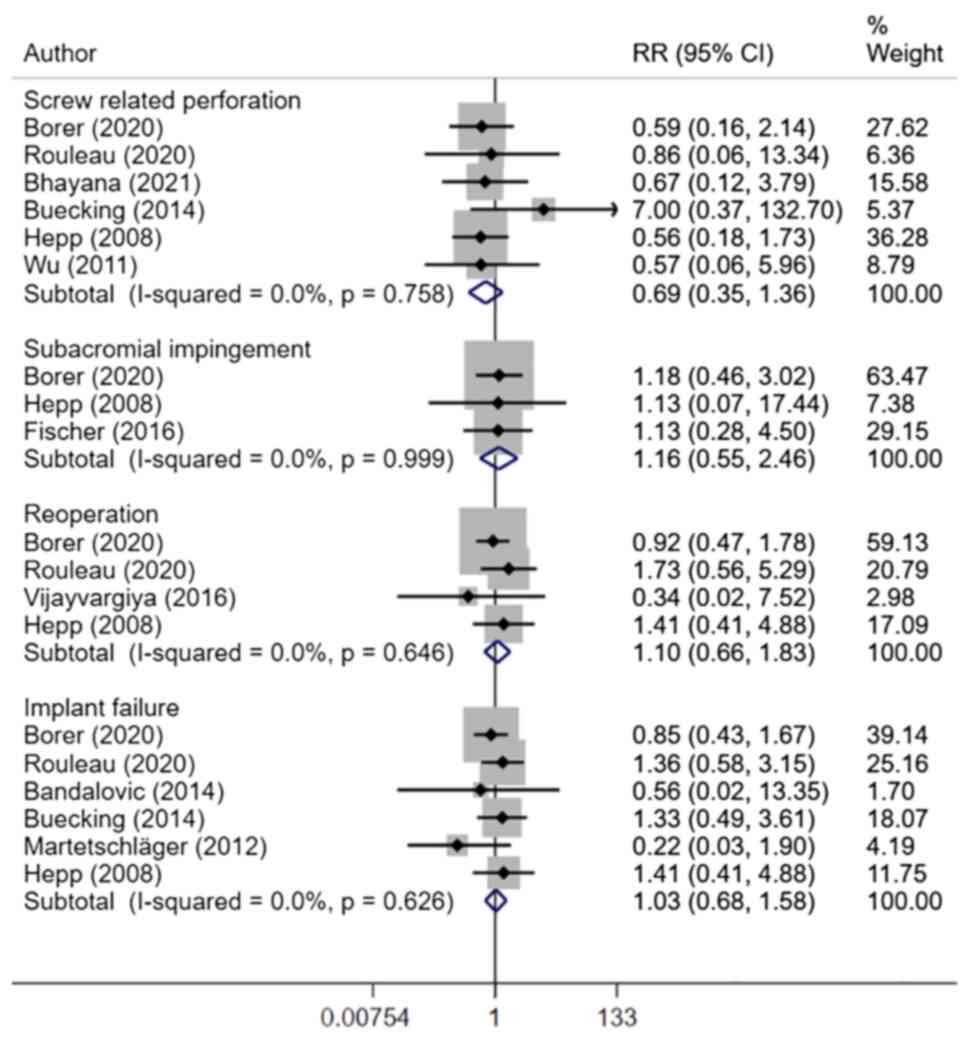
There were no statistically significant differences
in the risk of ‘any’ complication (RR 0.93; 95% CI, 0.65 to 1.34;
n=8; I2=0.0%), AVN (RR 0.88; 95% CI, 0.46 to 1.68; n=9;
I2=0.0%), non-union (RR 1.22; 95% CI, 0.32 to 4.64; n=4;
I2=0.0%), malunion (RR 0.92; 95% CI, 0.49 to 1.73; n=5;
I2=0.0%) and infection (RR 0.58; 95% CI, 0.16 to 2.12;
n=5; I2=0.0%) between the DS and the DP group (Fig. 5). All of the studies that reported
on outcomes related to axillary nerve found no axillary nerve
damage in the two groups of patients. The risk of screw-related
perforation (RR 0.69; 95% CI, 0.35 to 1.36; n=6;
I2=0.0%), subacromial impingement (RR 1.16; 95% CI, 0.55
to 2.46; n=3; I2=0.0%), need for reoperation (RR 1.10;
95% CI, 0.66 to 1.83; n=4; I2=0.0%) and implant failure
(RR 1.03; 95% CI, 0.68 to 1.58; n=6; I2=0.0%) was also
similar in both groups (Fig. 6).
Egger's test did not indicate the presence of publication bias for
any of the complications mentioned above (P>0.05; data not
shown).
Discussion
The current meta-analysis aimed to provide updated
evidence on two surgical methods, DP and DS, for the management of
proximal humerus fracture, and to compare clinical and functional
outcomes associated with these approaches. The time to bone union
was comparatively lower in patients who underwent surgery using the
DS approach. Furthermore, the DS approach was associated with
improved shoulder function at 3 months but not at 12 and 24 months
after the surgery. The ADL in patients treated with the DS approach
was significantly improved at the 3-, 6- and 12-month follow-ups as
compared with that in the DP group. There were no statistically
significant differences in the pain and QOL scores, as well as in
the ranges of movement and risk of complications between the two
groups. Although the duration of surgery and amount of blood loss
were lower in the DS group, this difference was not statistically
significant.
A previous review by Xie et al (15) compared the outcomes of DS and DP
approaches in patients with proximal humerus fracture and indicated
that the risk of AVN of the humeral head was significantly lower in
those patients subjected to the DS approach. In addition, they
reported no significant difference in functional outcomes between
the two approaches. These results were different from the outcomes
observed in the present meta-analysis. The present results
indicated no significant difference in the risk of necrosis between
the two groups. At the same time, improved functional outcome was
reported in patients that were managed with the DS approach, which
was reflected by the CSS and ADL score. The difference in the
results may be explained by the fact that the present meta-analysis
included a higher number of peer-reviewed studies. Furthermore, the
current study also provided pooled estimates on important outcomes
that were not considered in the review by Xie et al
(15), such as the range of
movement and time to bone union. The present study suggested that
patients that were managed using the DS approach had a
significantly lower time to bone union compared with that in the DP
group. There is still a need for studies with improved follow-up
data to make strong and reliable recommendations for clinicians
treating patients with proximal humerus fractures.
One possible explanation for the improved functional
score in patients treated with the DS approach discovered by the
present meta-analysis may be that this approach involves a lesser
degree of soft tissue manipulation and injury, possibly due to the
shorter duration of surgery and fairly direct access to the
fracture. On the other hand, the DP approach required extensive
dissection and retraction of the soft tissue (34). Furthermore, the DP approach also
required a partial release of deltoid insertion and retraction of
the deltoid muscle (35). This may
potentially lead to functional deficits. In addition, there was a
risk of damage to the anterior humeral circumflex artery,
particularly the anterolateral branch (36). In general clinical practice, the
traditional DP approach is commonly used and most surgeons are
familiar with this technique, compared to the DS approach (4,15,23).
The choice between these two surgical techniques, to a large
extent, may depend on the choice and skill of the treating surgeon
and the quality of healthcare facilities available.
The present meta-analysis had certain limitations.
For several of the outcomes, the number of studies pooled was
small, which may potentially lead to low power of the tests. This
made identifying a real effect challenging, as there was limited
information to aid in clinical reasoning and establish a more solid
foundation for causal inferences. The majority of the included
studies (n=10/14) were observational; therefore, the possibility of
not having data on important confounders or the inability to adjust
for them in the present analytic model could not be excluded. The
clinical and functional outcomes may also depend on the nature of
the fracture, e.g. the number of fractures. The included studies
did not provide data stratified by the nature of fracture and
therefore, such a subgroup analysis could not be performed. In
addition, the majority of the included studies did not provide
baseline information and characteristics of the patients in both
groups. Furthermore, data on whether these variables were
statistically similar or different were not provided. Therefore, it
was unclear if the studies were adjusted for these baseline
differences if any of or how these differences could have impacted
the final effect sizes.
The current meta-analysis indicated certain
advantages of the DS over the DP approach in patients with proximal
humerus fracture in terms of improved functional outcomes and
reduced time to bone union. There was neither a difference in the
risk of complications, pain and QOL scores, nor in the range of
movements between the two approaches. With the available data and
findings, it was not possible to conclusively elucidate which of
the two approaches had improved clinical efficacy and the choice of
the procedure should largely depend on the skills of the treating
surgeon. A larger number of RCTs with a robust methodology and
adequate sample size would be required to provide conclusive
answers on the comparative efficacy of the two approaches.
Supplementary Material
Judgements of the authors about study
quality using the adapted Ottawa-Newcastle Risk of Bias Assessment
tool.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The datasets used and/or analysed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
ZW conceived and designed the study. ZW and WS
performed the literature search and data collection. ZW and WS
analysed the data. WS wrote the paper. All authors have read and
approved the final manuscript. Data sharing is not applicable.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Launonen AP, Lepola V, Saranko A,
Flinkkilä T, Laitinen M and Mattila VM: Epidemiology of proximal
humerus fractures. Arch Osteoporos. 10(209)2015.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Bergdahl C, Ekholm C, Wennergren D,
Nilsson F and Möller M: Epidemiology and patho-anatomical pattern
of 2,011 humeral fractures: Data from the Swedish Fracture
Register. BMC Musculoskelet Disord. 17(159)2016.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Passaretti D, Candela V, Sessa P and
Gumina S: Epidemiology of proximal humeral fractures: A detailed
survey of 711 patients in a metropolitan area. J Shoulder Elbow
Surg. 26:2117–2124. 2017.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Khmelnitskaya E, Lamont LE, Taylor SA,
Lorich DG, Dines DM and Dines JS: Evaluation and management of
proximal humerus fractures. Adv Orthop. 2012(861598)2012.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Bahrs C, Stojicevic T, Blumenstock G,
Brorson S, Badke A, Stöckle U, Rolauffs B and Freude T: Trends in
epidemiology and patho-anatomical pattern of proximal humeral
fractures. Int Orthop. 38:1697–1704. 2014.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Lee SH, Dargent-Molina P and Bréart G:
EPIDOS Group. Epidemiologie de l'Osteoporose Study. Risk factors
for fractures of the proximal humerus: Results from the EPIDOS
prospective study. J Bone Miner Res. 17:817–825. 2002.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Iglesias-Rodríguez S, Domínguez-Prado DM,
García-Reza A, Fernández-Fernández D, Pérez-Alfonso E,
García-Piñeiro J and Castro-Menéndez M: Epidemiology of proximal
humerus fractures. J Orthop Surg Res. 16(402)2021.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Maier D, Jäger M, Strohm PC and Südkamp
NP: Treatment of proximal humeral fractures-a review of current
concepts enlightened by basic principles. Acta Chir Orthop
Traumatol Cech. 79:307–316. 2012.PubMed/NCBI
|
|
9
|
Vachtsevanos L, Hayden L, Desai AS and
Dramis A: Management of proximal humerus fractures in adults. World
J Orthop. 5:685–693. 2014.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Schumaier A and Grawe B: Proximal humerus
fractures: Evaluation and management in the elderly patient.
Geriatr Orthop Surg Rehabil. 9(2151458517750516)2018.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Mao F, Zhang DH, Peng XC and Liao Y:
Comparison of surgical versus non-surgical treatment of displaced
3- and 4-part fractures of the proximal humerus: A meta-analysis. J
Invest Surg. 28:215–224. 2015.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Mauro CS: Proximal humeral fractures. Curr
Rev Musculoskelet Med. 4:214–220. 2011.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Berkes MB, Little MT and Lorich DG: Open
reduction internal fixation of proximal humerus fractures. Curr Rev
Musculoskelet Med. 6:47–56. 2013.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Gavaskar AS, Chowdary N and Abraham S:
Complex proximal humerus fractures treated with locked plating
utilizing an extended deltoid split approach with a shoulder strap
incision. J Orthop Trauma. 27:73–76. 2013.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Xie L, Zhang Y, Chen C, Zheng W, Chen H
and Cai L: Deltoid-split approach versus deltopectoral approach for
proximal humerus fractures: A systematic review and meta-analysis.
Orthop Traumatol Surg Res. 105:307–316. 2019.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Moher D, Liberati A, Tetzlaff J and Altman
DG: PRISMA Group. Preferred reporting items for systematic reviews
and meta-analyses: The PRISMA statement. PLoS Med 6. doi:
10.1371/journal.pmed.1000097, 2009.
|
|
17
|
Wells G, Shea B, O'Connell D, Peterson J,
Welch V, Losos M and Tugwell P: The Newcastle-Ottawa Scale (NOS)
for Assessing the Quality of Nonrandomized Studies in
Meta-Analysis. 21.
|
|
18
|
Higgins JP and Green S: Cochrane Handbook
for Systematic Reviews of Interventions. 2nd Edition. John Wiley
& Sons, Chichester (UK), 2019.
|
|
19
|
Egger M, Davey Smith G, Schneider M and
Minder C: Bias in meta-analysis detected by a simple, graphical
test. BMJ. 315:629–634. 1997.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Hepp P, Theopold J, Voigt C, Engel T,
Josten C and Lill H: The surgical approach for locking plate
osteosynthesis of displaced proximal humeral fractures influences
the functional outcome. J Shoulder Elbow Surg. 17:21–28.
2008.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Wu CH, Ma CH, Yeh JJ, Yen CY, Yu SW and Tu
YK: Locked plating for proximal humeral fractures: Differences
between the deltopectoral and deltoid-splitting approaches. J
Trauma. 71:1364–1370. 2011.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Martetschläger F, Siebenlist S, Weier M,
Sandmann G, Ahrens P, Braun K, Elser F, Stöckle U and Freude T:
Plating of proximal humeral fractures. Orthopedics. 35:e1606–e1612.
2012.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Buecking B, Mohr J, Bockmann B, Zettl R
and Ruchholtz S: Deltoid-split or deltopectoral approaches for the
treatment of displaced proximal humeral fractures? Clin Orthop
Relat Res. 472:1576–1585. 2014.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Bandalović A, Cukelj F, Knežević J,
Ostojić M, Pavić A, Parać Z and Rošin M: The results of internal
fixation of proximal humeral osteoporotic fractures with PHILOS
locking plate. Psychiatr Danub. 26 (Suppl 2):S376–S381.
2014.PubMed/NCBI
|
|
25
|
Siripong S and Tangsripong P: Locking
plate fixation of proximal humeral fracture: Minimally invasive vs.
standard delto-pectoral approach. J Med Assoc Thai. 98:196–200.
2015.PubMed/NCBI
|
|
26
|
Fischer C, Frank M, Kunz P, Tanner M,
Weber MA, Moghaddam A, Schmidmaier G and Hug A: Dynamic
contrast-enhanced ultrasound (CEUS) after open and minimally
invasive locked plating of proximal humerus fractures. Injury.
47:1725–1731. 2016.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Vijayvargiya M, Pathak A and Gaur S:
Outcome analysis of locking plate fixation in proximal humerus
fracture. J Clin Diagn Res. 10:RC01–RC05. 2016.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Zhao L, Yang P, Zhu L and Chen AM: Minimal
invasive percutaneous plate osteosynthesis (MIPPO) through
deltoid-pectoralis approach for the treatment of elderly proximal
humeral fractures. BMC Musculoskelet Disord. 18(187)2017.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Büyükkuşcu MÖ, Kulduk A, Mısır A,
Çetinkaya E, Çamurcu İY and Gürsu ŞS: Effect of surgical approaches
on deltoid innervation and clinical outcomes in the treatment of
proximal humeral fractures. Jt Dis Relat Surg. 31:515–522.
2020.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Borer J, Schwarz J, Potthast S, Jakob M,
Lenzlinger P, Zingg U and Babians A: Mid-term results of minimally
invasive deltoid-split versus standard open deltopectoral approach
for PHILOSTM (proximal humeral internal locking system)
osteosynthesis in proximal humeral fractures. Eur J Trauma Emerg
Surg. 46:825–834. 2020.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Kim JY, Lee J and Kim SH: Comparison
between MIPO and the deltopectoral approach with allogenous fibular
bone graft in proximal humeral fractures. Clin Shoulder Elb.
23:136–143. 2020.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Rouleau DM, Balg F, Benoit B, Leduc S,
Malo M, Vézina F and Laflamme GY: Deltopectoral vs. deltoid split
approach for proximal HUmerus fracture fixation with locking plate:
A prospective RAndomized study (HURA). J Shoulder Elbow Surg.
29:2190–2199. 2020.PubMed/NCBI View Article : Google Scholar
|
|
33
|
Bhayana H, Chouhan DK, Aggarwal S, Prakash
M, Patel S, Arora C and Dhillon MS: Outcomes of plate
osteosynthesis for displaced 3-part and 4-part proximal humerus
fractures with deltopectoral vs. deltoid split approach. Eur J
Trauma Emerg Surg. 48:4559–4567. 2022.PubMed/NCBI View Article : Google Scholar
|
|
34
|
Hawkins RJ and Kiefer GN: Internal
fixation techniques for proximal humeral fractures. Clin Orthop
Relat Res. (223):77–85. 1987.PubMed/NCBI
|
|
35
|
Morgan SJ, Furry K, Parekh AA, Agudelo JF
and Smith WR: The deltoid muscle: An anatomic description of the
deltoid insertion to the proximal humerus. J Orthop Trauma.
20:19–21. 2006.PubMed/NCBI View Article : Google Scholar
|
|
36
|
Hintermann B, Trouillier HH and Schäfer D:
Rigid internal fixation of fractures of the proximal humerus in
older patients. J Bone Joint Surg Br. 82:1107–1112. 2000.PubMed/NCBI View Article : Google Scholar
|