Introduction
Branchial cysts are relatively uncommon lesions,
accounting for approximately 1% of neck masses (1). Since Ascherson's report (2) in 1832 that branchial cysts are caused
by the remnants of branchiogenic organs, there have been ongoing
debates regarding the etiology. There are two major theories
regarding the etiology of branchial cysts: the branchial
arch-derived theory, wherein the cysts are thought to arise from
remnants of embryonic branchial organs (3), and the glandular epithelial theory,
wherein the glandular epithelium that has strayed into the lymphoid
tissue may have become cystic (4).
Nonetheless, there is still no established theory.
Histopathologically, a branchial cyst typically presents as a cyst
wall covered with squamous epithelium, lymphoid tissue, and
lymphoid follicles with germinal centers found under the epithelium
(4), and complete surgical
resection is the first-line treatment for branchial cysts (5).
Branchial cysts often occur above the neck at the
anterior margin of the sternocleidomastoid muscle (5), but there have also been reports of
cysts in the oral cavity, including in the tongue, oral floor, soft
palate, buccal mucosa (6), and
parotid gland (7). Onset has been
reported in both the young and old (8-11),
with the most common age reported to be in the 20-30s (8-10,12).
Some reports indicate that there is no gender difference (13), but branchial cysts are slightly
more common in women (8-12).
Furthermore, while some reports indicate that there is no
difference in incidence between left and right sides of the body
(9,10), other reports indicate that it is
more common on the left side (12). Branchial cysts are not a
progressive disease, but in most cases, they cause cosmetic
problems and recurrent infections and do not spontaneously remit,
thus requiring treatment (14,15).
Although rare, squamous cell carcinoma may arise from the
epithelium of this cyst (16).
Although there are numerous reports of branchial
cysts in literature, to the best of our knowledge, there have been
no reports of calcification in the cystic cavity of branchial
cysts. We believe that the presence of calcification in branchial
cysts is an extremely rare occurrence. Therefore, herein, we
describe a unique case of branchial cyst of the submandibular
region with calcification, along with a review of the literature on
the factors contributing to calcification.
Case report
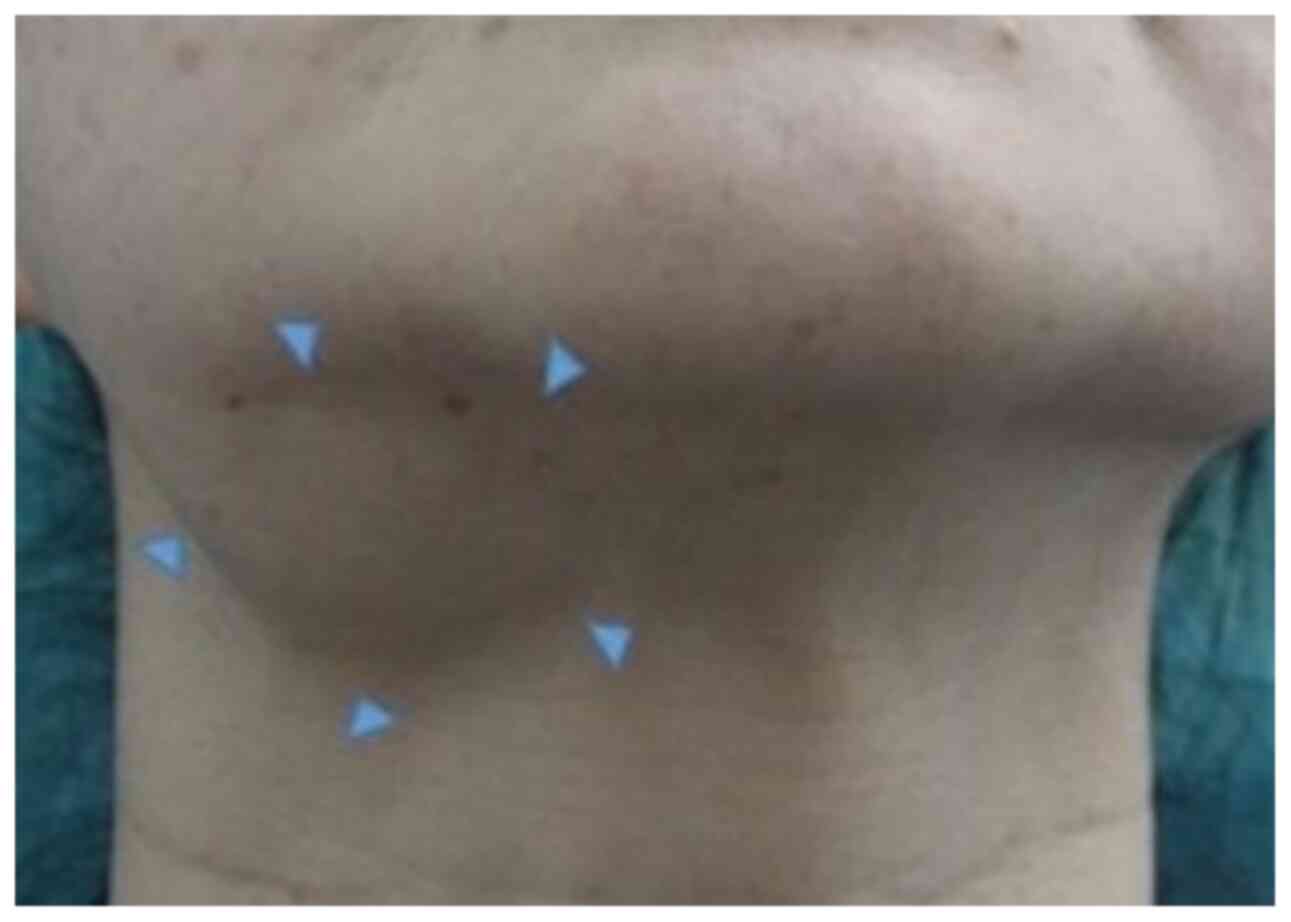
A 49-year-old woman presented to our department with
a complaint of swelling in the right submandibular region. The
patient initially became aware of a mass in the same location 9
years prior but opted out of active treatment and was instead
placed under observation. However, the swelling had increased
several months before the first visit to our department, prompting
a thorough examination.
The patient's medical and family history was
unremarkable. Upon physical examination, an elastic and soft cyst
with no tenderness measuring 24x37 mm that was clearly demarcated
from the surroundings was found in the right submandibular region
(Fig. 1). A panoramic radiograph
further revealed a cystic lesion with a well-circumscribed border
in the same region and a crescent-shaped radiopaque finding in the
base of the lesion (Fig. 2).
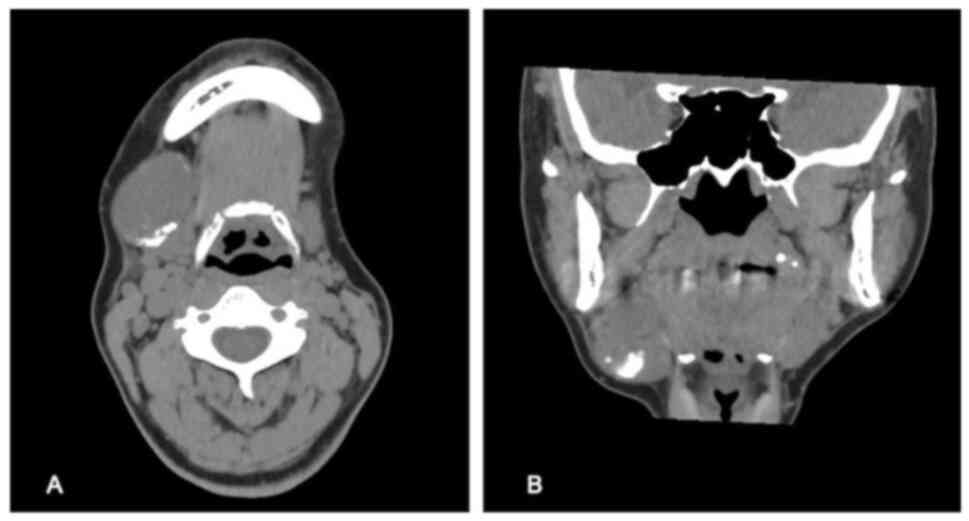
Computed tomography showed well-circumscribed cystic
lesions with similar density to soft tissue. The lesion was located
anterior to the sternocleidomastoid muscle, outside the hyoid bone,
and in front of the submandibular gland. A high-density image of
calcification was observed at the bottom of the lesion (Fig. 3). Ultrasonography revealed that the
inside of the hypoechoic region was uniform and surrounded by a
hyperechoic region that appeared to be a single layer of the cyst
wall. Fine-needle aspiration of the cyst contents yielded pale
yellow and serous fluid, which microscopic examination identified
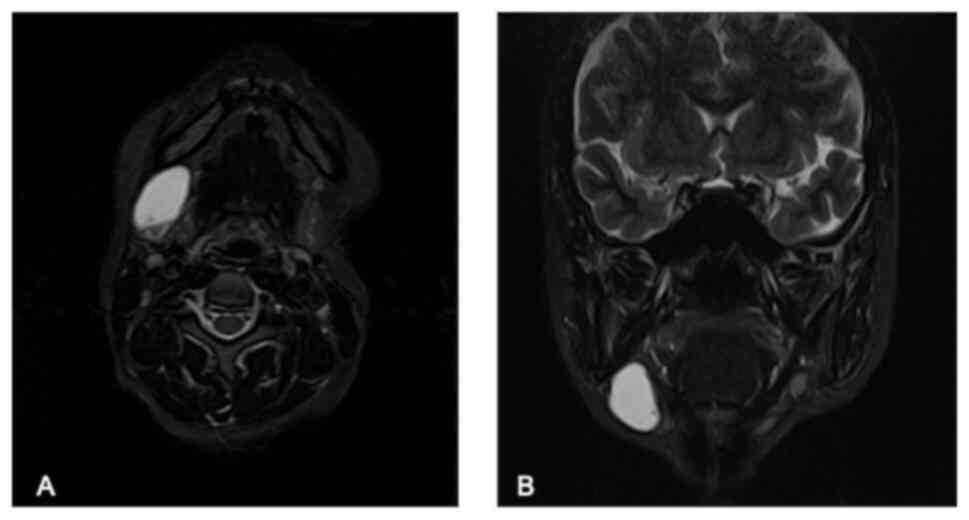
to have cholesterol crystals. On magnetic resonance imaging,
high-intensity lesions were visualized on both T2-weighted images
and short-τ inversion recovery images on the anterior margin of the
right sternocleidomastoid muscle just below the platysma muscle,
with a clear demarcation from the surroundings The submandibular
gland was compressed posteriorly and flattened (Fig. 4).
Cystectomy was performed under general anesthesia
and an incision was made approximately 20 mm below the lower edge
of the right lower jaw to reveal an encapsulated cystic lesion
located below the platysma muscle. The cystic lesion had no
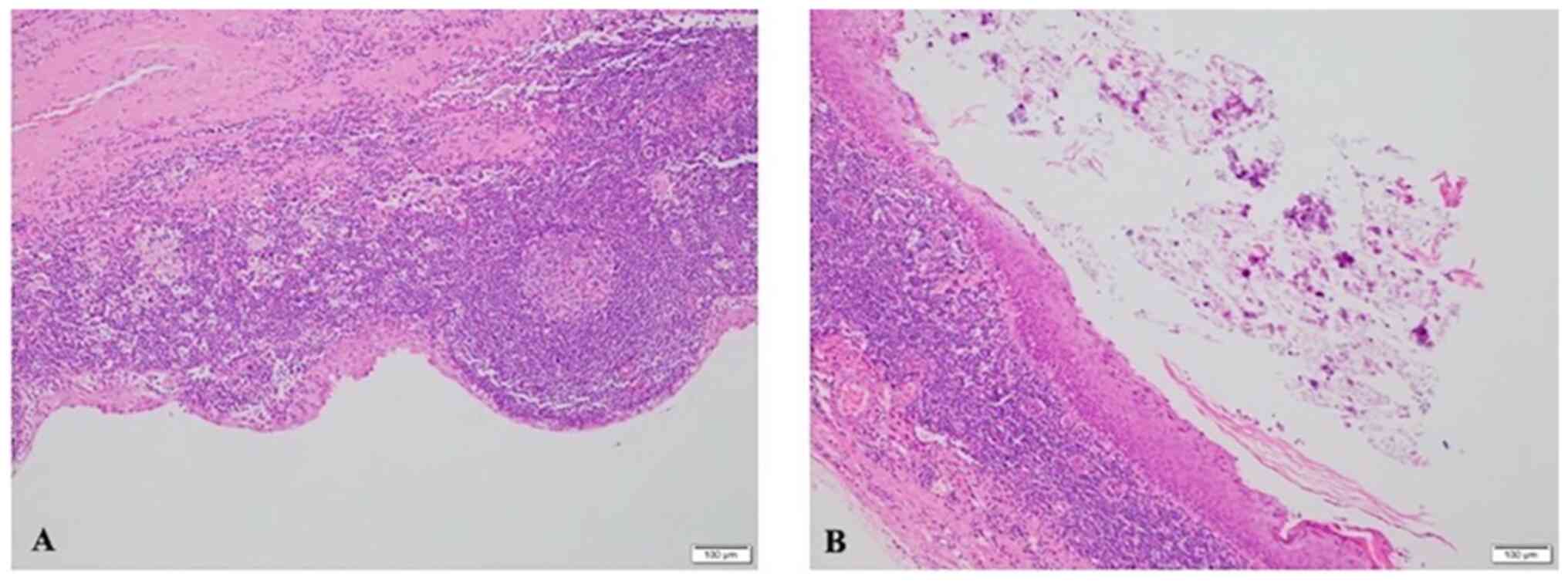
adhesions and was relatively easy to remove (Fig. 5). Histopathological examination
confirmed the diagnosis of branchial cyst. Some areas showed cysts
lined with stratified squamous epithelium and keratinization, while
lymphoid tissue containing lymphoid follicles was found just below
the epithelial lining. Additionally, keratinization and calcified
granules were observed inside the cyst cavity (Fig. 6). The patient has been under
observation for approximately 2 years since the operation through
follow-ups and has experienced no complications or recurrence. The
patient currently remains in good postoperative condition.
Discussion
From a histopathological standpoint, branchial cysts
are known by different names, such as lymph epithelial cysts or
lateral cervical cysts, depending on the site of occurrence. The
term branchial cyst has prevailed since the report by Ascherson,
which suggested its origin from branchiogenic organs (2). However, in 1949, King considered the
pathogenic basis of the etiology to be uncertain and reexamined the
cyst from a histopathological and anatomical perspective and
proposed the name lateral lymphoepithelial cyst (17). Since then, cases published in the
literature have referred to these cysts as branchial cyst,
lymphoepithelial cyst, or lateral cervical cyst, although they
essentially have the same pathology. Branchial cysts are also
observed in the oral cavity and the neck; however, their incidence
is rare (18). Gold first
described oral lymphoepithelial cysts as ‘branchial cleft cysts’ in
1962(19). Bhaskar described
branchial cysts in the oral cavity as ‘lymphoepithelial cysts’ in
1966(20).
Bailey classified the cysts into four types
according to site of occurrence (21). Type I is the most superficial, with
lesions along the anterior margin of the sternocleidomastoid
muscle. Type II is the most common, located along the anterior
margin of the sternocleidomastoid muscle, lateral to the carotid
space and posterior to the submandibular gland. Type III is a
lesion with an inward extension between the internal and external
carotid arteries toward the lateral pharyngeal wall. Lastly, type
IV is a lesion located inside the carotid artery gap and covered
with columnar epithelium. In the present case, the cyst was located
just below the platysma muscle and in front of the submandibular
gland at the anterior margin of the sternocleidomastoid muscle, and
it was classified as type I.
After the report of von Ascherson that branchial
cysts were caused by the remnants of the branchiogenic organs, the
pattern of cyst development has been roughly divided into the
theory that it is a remnant of the branchial organs during the
embryonic period (3) and that the
glandular epithelium that has invaded the lymphoid tissue has
become cystic (4).
The histopathological features of the branchial cyst
comprise a cyst wall covered with squamous epithelium, and lymphoid
tissue and lymphoid follicles with germinal centers under the
epithelium (4). Regauer et
al described this cystic epithelium as the respiratory
epithelium in childhood, transitional-type pseudostratified
epithelium in adolescence, and stratified squamous epithelium in
adulthood (22). They reported
changes in cytokeratin expression associated with such metaplasia.
Based on these findings, the origin of the development was defined
as the invasion of the residual epithelium of the second arch, and
the gradual transformation of the respiratory epithelium into
transitional-type pseudostratified epithelium, non-keratinized
stratified squamous epithelium, and keratinized stratified squamous
epithelium.
These cysts are said to be almost non-recurrent, if
completely removed. The recurrence rate is high at 20% when the
branchial cyst is removed after intervention, and low at 3% when
cystectomy is performed without any intervention (23). Olsen et al reported a case
of recurrence in which only the cyst was removed close to the
submandibular gland; in such cases, the cyst and the submandibular
gland should be removed at the same time (24). In our case, the cyst excluded the
posterior submandibular gland and was not exposed after cyst
removal; therefore, it was preserved. Currently, the postoperative
course provided good outcomes without recurrence; however, we
believe that sufficient follow-up is required in future.
Calcification in the cystic cavity can be
categorized as metastatic calcification when accompanied by
systemic electrolyte abnormalities, and dystrophic calcification
when there is no systemic electrolyte abnormalities (25). In the present case, the patient had
no history of any disease resulting in abnormal serum calcium
levels. Dystrophic calcification can be explained by a review of
biochemical events in cell death. Loss of control of intracellular
Ca2+ balance opens membrane calcium channels, leading to
an increase in intracellular calcium concentration. Calcium is
normally regulated in the cytosol, endoplasmic reticulum, and
mitochondria, each of which has a Ca2+-ATPase membrane
pump. Elevated intracellular calcium concentrations activate
calpain and cleave mitochondrial and other plasma membrane
Na+/Ca2+ exchangers, leading to reduced
Ca2+ efflux and reduced Ca2+ re-uptake by the
endoplasmic reticulum. Thus, calcium excess is an expected sequela
of cell death. Dystrophic calcification is most prominent in the
mitochondria and is initially visible histologically as basophilic
plaques of dead cells. As calcium salt deposition progresses,
entire cells and even extracellular tissues become calcified.
Dystrophic calcification occurs around necrotic and inflammatory
tissues at sites of local tissue damage and is caused by calcium
accumulation (25).
In the present case, chronic inflammation of the
cyst wall may have caused the cells of the cyst wall to peel off
into the cyst cavity or the cyst wall may have undergone
orthokeratotic hyperkeratosis, causing keratinocytes to peel off
into the cyst. Furthermore, tissue scattered as keratinized
material to form a nucleus that over time, deposited and calcified
calcium, resulting in dystrophic calcification. Yoon et al
described the concepts of metastatic calcification and dystrophic
calcification, as well as two other causes of calcification in
tumors: a component of the tumor, and calcification of the material
secreted by neoplastic cells
26). The possibility of calcification of the
material secreted by neoplastic cells was considered but ruled out
because the cyst wall comprised squamous epithelium on
histopathological examination. There have been no reports of
calcification of the material in branchial cysts, and it is
necessary to accumulate more cases in the future to investigate the
causes of calcification and to further examine the pathological
significance of calcification. In addition, in the case of a
disease with a non-novel name but with extremely rare clinical
manifestations, as in the case of the autopsy, pathological
investigations, such as additional immunostaining, would be
necessary to elucidate the etiology of the disease. Therefore, it
is important to collaborate closely with the pathology department
in such cases.
For the histopathological diagnosis of branchial
cysts, HE staining alone is sufficient. However, HE staining is not
sufficient to find the cause of calcification, necessitating an
immunohistological search; this is a limitation of this report. In
future, it will be necessary to establish a system that allows for
close collaboration with the pathology department such that
sufficient histopathological examination can be performed in cases
with rare clinical findings in addition to cases for which clinical
diagnosis is difficult.
In conclusion, we reported a rare case of branchial
cyst containing calcification in the cystic cavity and discussed
the factors contributing to the calcification in the literature.
The findings of this study are useful for enhancing the
understanding of the pathophysiology of branchial cyst with
calcification, and for facilitating accurate diagnosis and
effective treatment and management of such cases.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
All data generated or analyzed during this study are
included in this published article.
Authors' contributions
TK acquired patient clinical data, performed the
literature review and edited the manuscript. TK and MY
substantially contributed to the concept and design of the study.
KN and TW acquired the data and contributed clinical advice. TK
revised the manuscript. TW and KN evaluated the specimens and gave
histopathological advice. TK had a major role in writing the
manuscript. TK and MY confirm the authenticity of all the raw data.
All authors read and approved the final manuscript.
Ethics approval and consent to
participate
Not required.
Patient consent for publication
Written informed consent was obtained from the
patient for the publication of this case report and the
accompanying images.
Competing interests
The authors confirm that they have no competing
interests.
References
|
1
|
Skolnik EM, Loewy A and Ferrer J:
Swellings of the neck. Arch Otolaryng. 81:150–152. 1965.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Ascherson FM: De fistulis colli congenitis
adjectis fissurarum branchialium in mammalibus avibusque historia
succincta. Berolini. CH Jonas, pp1-22, 1832.
|
|
3
|
Simpson RA: Lateral cervical cysts and
fistulas. Laryngoscope. 79:30–59. 1969.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Bhaskar SN and Bernier JL: Histogenesis of
branchial cysts; a report of 468 cases. Am J Pathol. 35:407–443.
1959.PubMed/NCBI
|
|
5
|
Glosser JW, Pires CAS and Feinberg SE:
Branchial cleft or cervical lymphoepithelial cysts: Etiology and
management. J Am Dent Assoc. 134:81–86. 2003.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Yang X, Ow A, Zhang CP, Wang LZ, Yang WJ,
Hu YJ and Zhong LP: Clinical analysis of 120 cases of intraoral
lymphoepithelial cyst. Oral Surg Oral Med Oral Pathol Oral Radiol.
113:448–452. 2012.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Camilleri AC and Lloyd RE:
Lymphoepithelial cyst of the parotid gland. Br J Oral Maxillofac
Surg. 28:329–332. 1990.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Howie AJ and Proops DW: The definition of
branchial cysts, sinuses and fistulae. Clin Otolaryngol Allied Sci.
7:51–57. 1982.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Golledge J and Ellis H: . The aetiology of
lateral cervical (branchial) cysts: Past and present theories. J
Laryngol Otol. 108:653–659. 1994.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Daou FS: Branchial cyst: An often
forgotten diagnosis. Asian J Surg. 28:174–178. 2005.PubMed/NCBI
|
|
11
|
McPhail N and Mustard RA: Branchial cleft
anomalies: A review of 87 cases treated at the Toronto General
Hospital. Can Med Assoc J. 94:174–179. 1966.PubMed/NCBI
|
|
12
|
Agaton-Bonilla FC and Gay-Escoda C:
Diagnosis and treatment of branchial cleft cysts and fistulae. A
retrospective study of 183 patients. Int J Oral Maxillofac Surg.
25:449–452. 1996.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Rickles NH and Little JW: The histogenesis
of the branchial cyst. II. A study of the lining epithelium. Am J
Pathol. 50:765–777. 1967.PubMed/NCBI
|
|
14
|
Chen WL and Fang SL: Removal of second
branchial cleft cysts using a retroauricular approach. Head Neck.
31:695–698. 2009.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Bajaj Y, Ifeacho S, Tweedie D, Jephson CG,
Albert DM, Cochrane LA, Wyatt ME, Jonas N and Hartley BE: Branchial
anomalies in children. Int J Pediatr Otorhinolaryngol.
75:1020–1023. 2011.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Stefanicka P and Profant M: Branchial
cleft cyst and branchial cleft cyst carcinoma, or cystic lymph node
and cystic nodal metastasis? J Laryngol Otol. 137:31–36.
2023.PubMed/NCBI View Article : Google Scholar
|
|
17
|
King ESJ: The lateral lympho-epithelial
cyst of the neck; branchial cyst. Aust N Z J Surg. 19:109–121.
1949.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Nonaka CF, Henriques AC, de Matos FR, de
Souza LB and Pinto LP: Nonodontogenic cysts of the oral and
maxillofacial region: Demographic profile in a Brazilian population
over a 40-year period. Eur Arch Otorhinolaryngol. 268:917–922.
2011.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Gold C: Branchial cleft cyst located in
the floor of the mouth. Report of a case. Oral Surg Oral Med Oral
Pathol. 15:1118–1120. 1962.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Bhaskar SN: Lymphoepithelial cysts of the
oral cavity. Report of twenty-four cases. Oral Surg Oral Med Oral
Patho. 21:120–128. 1966.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Bailey H: The clinical aspects of
branchial cysts. Br J Surg. 10:565–572. 2005.
|
|
22
|
Regauer S, Gogg-Kamerer M, Braun H and
Beham A: Lateral neck cysts-the branchial theory revisited. A
critical review and clinicopathological study of 97 cases with
special emphasis on cytokeratin expression. APMIS. 105:623–630.
1997.PubMed/NCBI
|
|
23
|
Chandler JR and Mitchell B: Branchial
cleft cysts, sinuses, and fistulas. Otolaryngol Clin North Am.
14:175–186. 1981.PubMed/NCBI
|
|
24
|
Olsen KD, Maragos NE and Weiland LH: First
branchial cleft anomalies. Laryngoscope. 90:423–436.
1980.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Miller MA and Zachary JF: Mechanisms and
morphology of cellular injury, adaptation, and death. Pathologic
Basis Vet Dis. 2-43(e19)2017.
|
|
26
|
Yoon JH, Ahn SG, Kim SG and Kim J:
Calcifications in a clear cell mucoepidermoid carcinoma of the hard
palate. Int J Oral Maxillofac Surg. 34:927–929. 2005.PubMed/NCBI View Article : Google Scholar
|