Introduction
Thyroid disease with significant airway obstruction
is a rare occurrence, with an incidence rate of about 1-2% in
thyroid patients (1). Numerous
cases of the combination of thyroid disease and airway obstruction
occur along with thyroid cancer (1). However, a large benign goiter may
also be associated with severe acute airway obstruction (2). Significant airway obstruction can
induce severe respiratory distress and requires immediate action
for the prompt restoration of the airway passage (3). In severe respiratory distress, an
emergency thyroidectomy is required (3). However, an emergency thyroidectomy in
individuals with dyspnea can increase the risk of surgical
complications such as hemorrhage, recurrent laryngeal nerve injury
and hypoparathyroidism (3).
Therefore, an alternative effective therapeutic strategy is
necessary to avoid such complications.
In the present study, a rare case of acute airway
compression induced by a giant goiter was reported. Treatment of
this case involved placement of a self-expanding metal stent to
relieve dyspnea. Following stent placement, a thyroidectomy and
subsequent stent removal were performed.
Case presentation
A 62-year-old Chinese female presented to the
emergency department of Weifang Hospital of Traditional Chinese
Medicine in September 2018. The patient reported an abrupt onset of
dyspnea and stridor ~2 h prior. The patient did not exhibit other
symptoms such as appetite change, cough or palpitation. The patient
had no prior cardiopulmonary disease and reported a history of a
thyroid goiter for 40 years. The thyroid goiter was non-toxic and
exhibited a slow growth rate. The patient first experienced
intermittent dyspnea ~15 years prior and the frequency of dyspnea
had increased in recent years.
Clinical examination of the patient revealed a firm,
large, non-fluctuant thyroid swelling on the neck. SpO2
of the patient on admission to hospital was 82%. Thyroid hormone
concentrations were within the expected ranges: Triiodothyronine,
2.88 pmol/l; free thyroxine, 7.61 pmol/l; thyrotropin, 2.12 µIU/ml;
thyroglobulin autoantibody, 2.90 IU/ml; and thyroid peroxidase
autoantibody, 28.10 IU/ml. Serum potassium and sodium
concentrations were 2.95 mmol/l and 127.4 mmol/l, respectively.
Arterial blood gas analysis revealed a pH of 7.14, pCO2
of 59.5 mm Hg, pO2 of 71 mm Hg and an O2
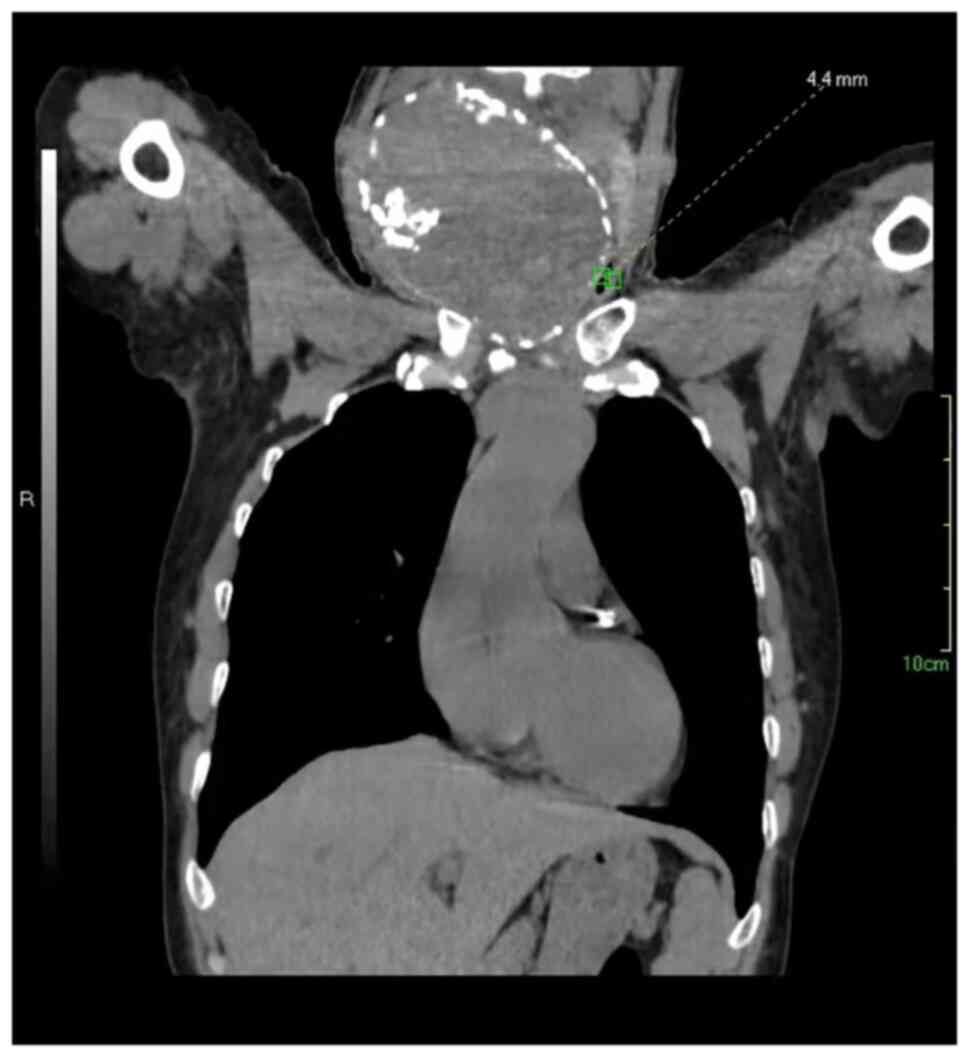
saturation of 83.2% without oxygen supplementation. Neck and chest
computed tomography scans obtained during the first admission to
hospital demonstrated a significant narrowing of the tracheal lumen
caused by enlargement of the bilateral thyroid glands. Diameter of
tracheal lumen measured at the narrowest point was 4.4 mm, with a
length of 20.0 mm (Fig. 1). Owing
to the complexity associated with emergency surgery, the surgical
team proposed treatment for severe hypopnea should take place
first. Thereafter, it was decided to place a self-expandable metal
stent to treat the compromised airway instead of an emergency
thyroidectomy.
Firstly, local anesthesia was induced using
lidocaine. Following anesthesia, an introductory guide wire was
inserted into the obstructed airway using a flexible bronchoscope.
The bronchoscope was then removed and a stainless self-expandable
metal stent (70x18 mm) was inserted into the trachea along the
guide wire until it was aligned with the previously placed skin
markers indicating the proximal and distal ends of the lesion.
Finally, the stent was deployed from the site of its delivery
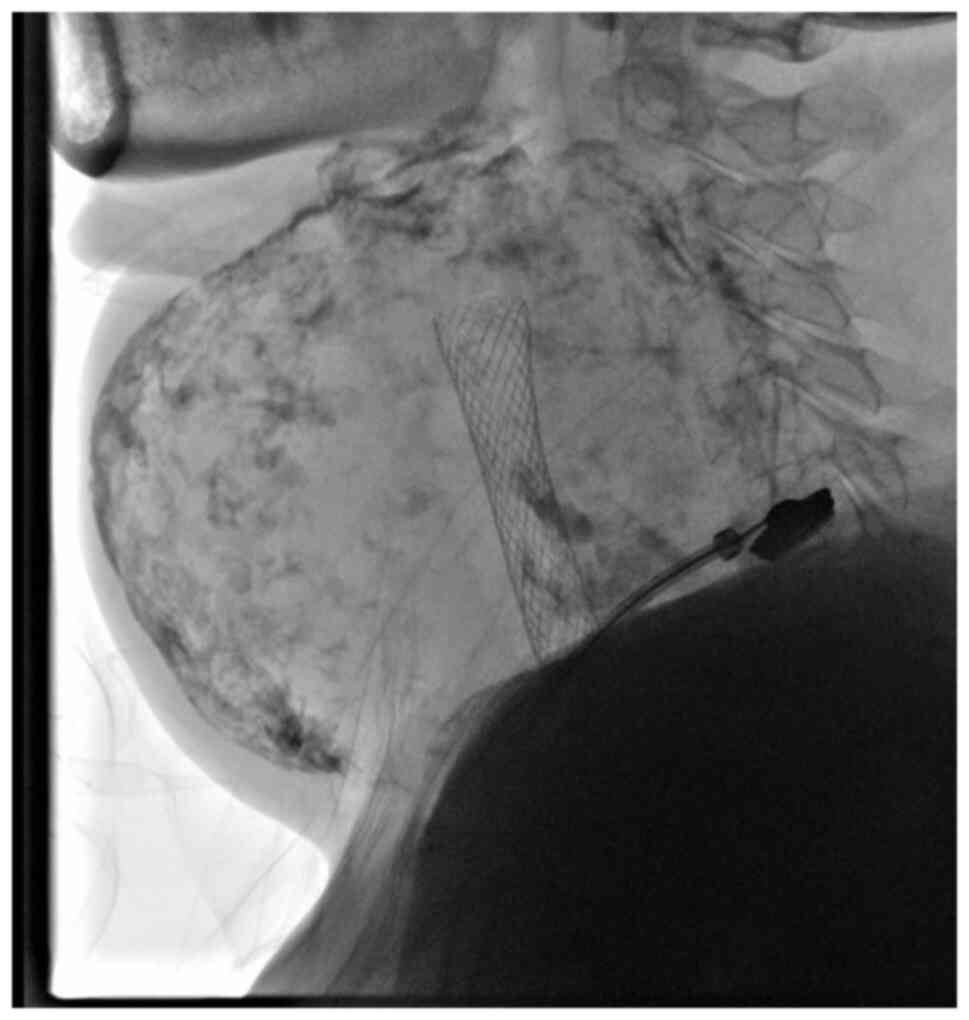
catheter. A chest radiography scan demonstrated that the stent had
successfully implanted in the trachea (Fig. 2). Patient respiratory function
improved and the SpO2 was immediately restored to 97%
upon stent placement.
Patient electrolyte balance was restored to expected
levels upon potassium and sodium supplementation. A week after
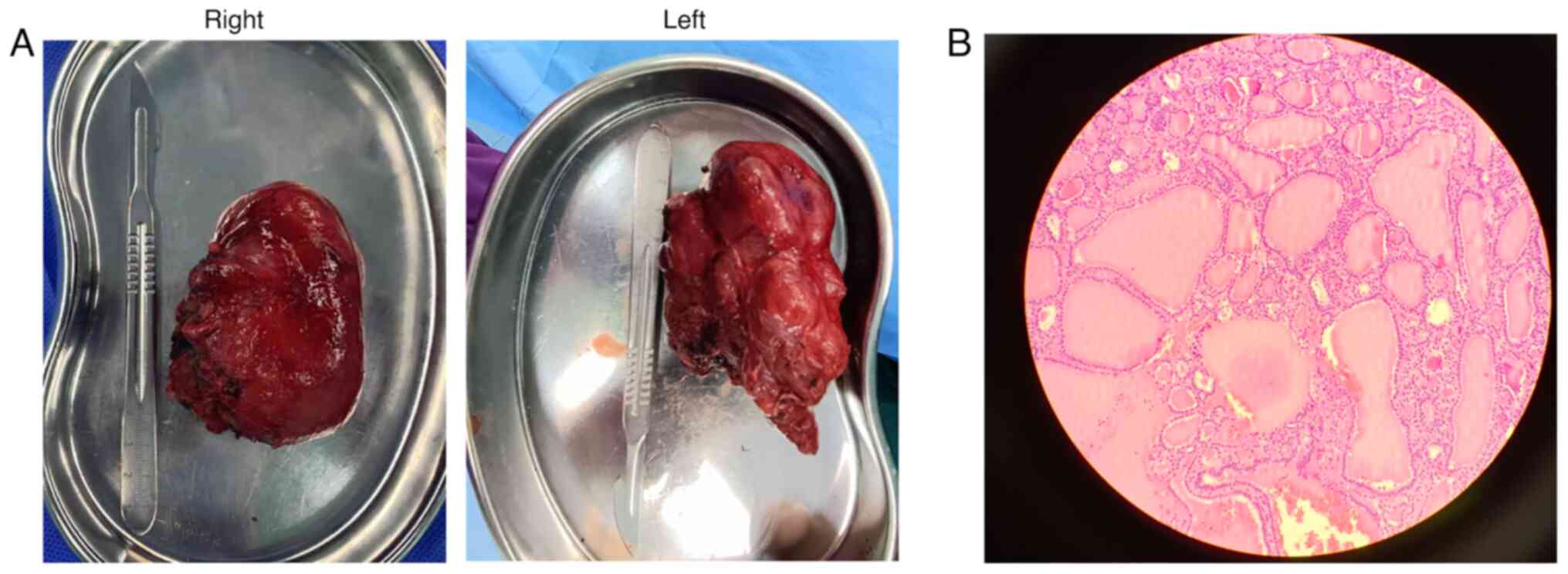
stent placement surgery, the patient underwent a thyroidectomy
under propofol-induced general anesthesia (Fig. 3A). Intratracheal intubation was
performed using a laryngoscope. Total thyroidectomy was performed
through a collar incision. The left lobe and isthmus were first
resected, followed by resection of the right lobe. Recurrent
laryngeal nerve (RLN) palsy and parathyroid glands were identified
and protected during the procedure. Specimens were fixed with 4%
formalin at room temperature for 12 h, embedded in paraffin, cut
into 4-µm sections, stained for 5 min at room temperature with
hematoxylin and eosin, and observed under a light microscope (Nikon
Corporation). As observed under the light microscope with x200
magnification, the thyroid demonstrated a benign multinodular
structure (Fig. 3B). The level of
parathyroid hormone was within the expected range and the voice of
the patient did not change after surgery.
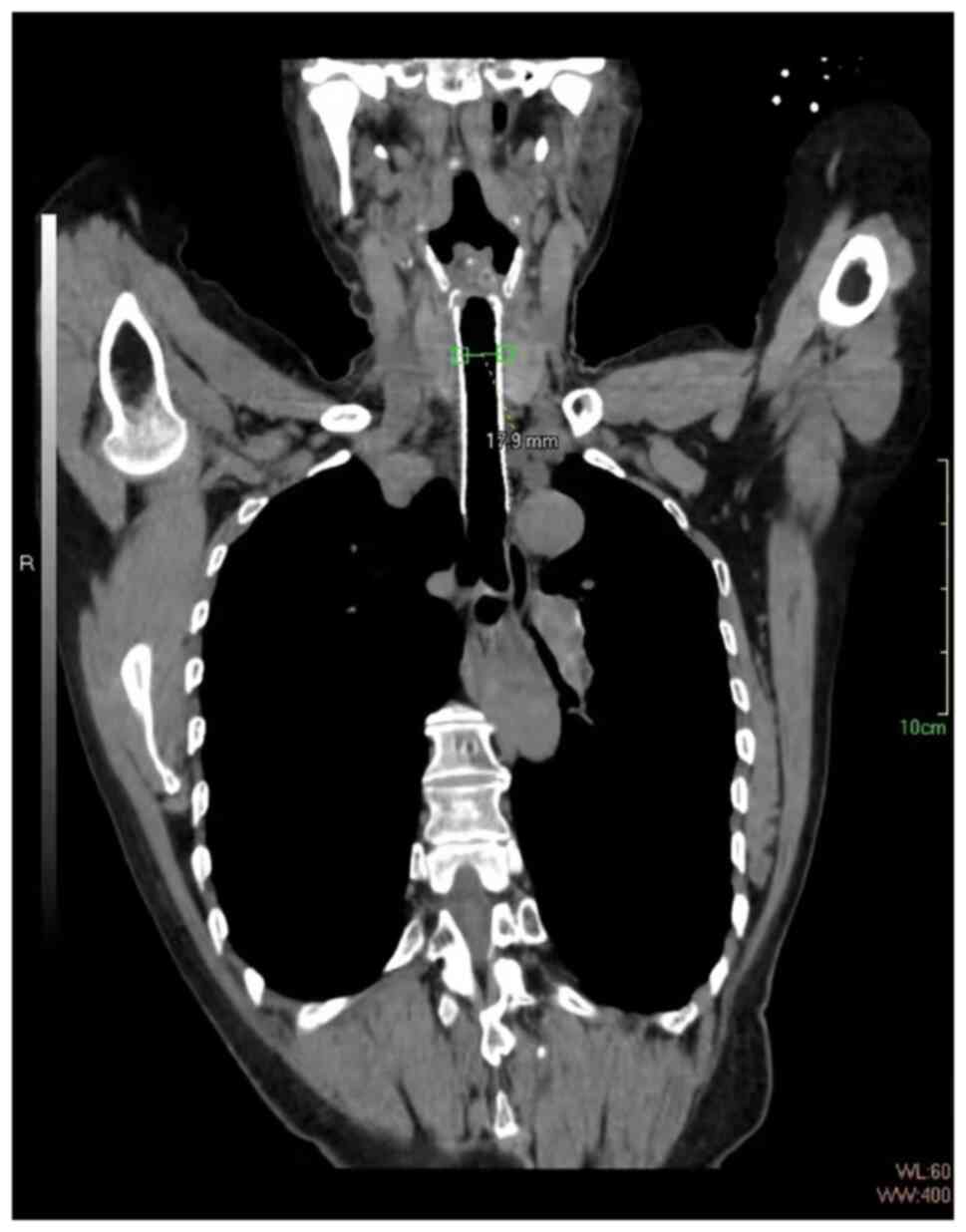
At 3 months after the thyroidectomy, the diameter of
the tracheal lumen was 17.9 mm (Fig.
4). Considering the potential complications that could arise
due to the stent, the surgical team recommended its removal.
However, the stent could not be removed using a bronchoscope
because of granulation tissue formation around stent. Therefore,
the patient underwent a second surgery for stent removal under
local anesthesia (Fig. 5).
At 6 months after stent removal, fiberoptic
bronchoscopy was performed on the patient. No structural change was
observed in the airway at the stent implantation site. A follow-up
2 years after the final surgery demonstrated that the patient had
no dyspnea relapse.
Discussion
With the development of improved diagnostic methods
including ultrasound and computed tomography and early treatment
modalities such as surgery and radiofrequency ablation, reports of
airway obstruction due to the presence of a goiter is very uncommon
though not completely unknown (2).
Airway stenosis may induce clinical symptoms of airway obstruction,
such as shortness of breath and severe suffocation (4). These symptoms may develop when the
diameter of the trachea is considerably narrowed. In the present
study, owing to the compression caused by the enlarged goiter, the
narrowest point of airway stenosis was 4.4 mm in diameter and led
to severe suffocation of the patient. Suffocation is an emergency
condition that can cause sudden asphyxia and mortality. Therefore,
patients who experience acute airway obstruction require urgent
treatment to prevent mortality.
According to a report from a previous study, the
most effective method for relieving suffocation is to surgically
remove the airway obstruction induced by the enlarged goiter
(5). However, this surgical
process presents a number of challenges. First, due to tracheal
stenosis, anesthesiologists may find it challenging to perform
tracheal intubation, and anesthetization could lead to tracheal
prolapse (3). Therefore, a
standard sequence of induction and intubation should be considered
at the risk of aspiration in patients with airway obstruction
(2,3). Secondly, in the present study,
emergency thyroidectomy was considered a challenge for the surgical
team because of the poor health of the patient, as indicated by
anoxia and electrolyte levels. To reduce the potential risk of
surgical complications, this emergency surgery should be considered
in limited cases.
In acute conditions, airway obstruction can be
temporarily ameliorated by tracheal stent implantation. The ideal
stent should exhibit an expansion force adequate to maintain airway
patency against compressive forces without exerting pressure on the
mucosa that could damage the airway, and should also be easy to
insert and remove (6). At present,
there are two types of tracheal stents made of different materials:
Metal and silicone stents, both of which have advantages and
disadvantages (7,8). Metal stents are radiopaque and can be
implanted in a radiological suite (7,8).
Meanwhile, silicone stents are radiolucent and are used in
operating rooms (7,8). A previous study has reported that
patients can be successfully intubated using a metal stent for
performing the chemotherapy and radiotherapy (9). Complications resulting from stent
implantation can occur with both types of stent. Granuloma
formation is the most common complication resulting from the use of
a metal stent (10). It is
particularly difficult to prevent the overgrowth of granulation
tissue when using non-membrane-coated metallic stents, which may
obstruct the lumen (4). Migration
of the stent and mucositis causing airway obstruction are more
common when silicon stents are used compared with using metal
stents (11). In addition, the
inner diameter of a silicon stent is too small for intubation and
can be easily obstructed by sputum (8). Once an airway obstruction has been
demonstrated, stent implantation should be performed as soon as
possible. Owing to the lower migration rate and longer inner
diameter of a metal stent, it is preferable to select a metal stent
for patient intubation (8). Due to
the easier removal process, it is more appropriate for the silicon
stent to be used to ameliorate an airway obstruction caused by
lymphoma or anaplastic thyroid cancer, which can be treated by
chemotherapy (8). Therefore, in
the present study, a self-expandable metallic stent was selected
for intubation and surgery.
An emergency tracheostomy is an alternative strategy
to resolve airway obstruction. However, an emergency tracheostomy
can be hindered by the presence of a large thyroid mass, preventing
access to the trachea and eradicating all anatomical landmarks
(3).
In the present study, once the airway obstruction
was removed, a thyroidectomy was selected as the appropriate
treatment method to eliminate the thyroid mass. However, when a
thyroidectomy is performed on a patient with an enlarged goiter, it
can lead to an increased risk of postoperative hypoparathyroidism,
RLN palsy and hemorrhage (12,13).
This risk can be decreased through the use of surgical loupes and
parathyroid autotransplantation during thyroid surgery, which can
decrease permanent and transient hypoparathyroidism (13,14).
In addition, the use of an RLN monitor could identify the RLN in a
safer and more rapid manner compared with no RLN monitor (15). Radiofrequency ablation may also be
a suitable alternative method for patients with a combination of
thyroid tumor and airway obstruction. Radiofrequency ablation has
been reported to be a valid and safe approach for the treatment of
benign thyroid nodules with airway obstruction (16). However, ablated thyroid nodules
demonstrate a gradual reduction in size over several months, and
edema and the resulting increase in tumor volume can occur
immediately following radiofrequency ablation (17,18).
Owing to the potential for multiple complications to
arise from the placement of a stent, its removal is necessary in
patients with a benign goiter. A silicon stent is easy and safe to
remove under endoscopy (8).
However, endotracheal intubation is challenging to perform due to
potential migration of the stent (8). Once a metallic stent is retained
inside the patient for a long period, it is difficult to remove due
to the migration of the stent and granulation tissue formation
(8). The stent can be removed
either by destruction and removal of the wires using an endoscopic
procedure or it can be removed using an open surgery. In the
present study, the metal stent could not be removed in a
radiological suite. There are two potential reasons for the initial
failure of stent removal. First, the shape of the stent may be
altered when the pressure induced by the large goiter decreases
after thyroidectomy (19,20). Second, epithelialization in
conjunction with granulation tissue formation around metal stents
can cause the stent removal to be challenging (19,20).
Stents are mucosalized within one month of placement (21). Therefore, stents require
deconstruction and gradual removal. However, an additional problem
that could be encountered is tracheomalacia, which may be induced
in response to compression by the enlarged goiter (22). The tracheomalacia could induce
collapse in the area of trachea. In this condition, the patient is
unable to breathe. To avoid this condition in the present study,
the trachea with malacia was sutured to the surrounding tissues,
such as platysma myoides. In addition to adhering to the
surrounding tissue, the trachea muscles exhibiting tracheomalacia
could maintain the tracheal diameter independent of the stent. The
duration required for the reduction of edema could be 3 months, and
the reoperation may have reduced the complications of thyroidectomy
(23). Therefore, 3 months after
the stent was placed, a second surgery was performed in which the
stent was removed.
In conclusion, airway obstruction induced by a
benign goiter is rare, and the prompt restoration of pulmonary
ventilation is a necessity in such cases. Stent placement for
airway stenosis could provide significant palliation to allow for
further intervention measures, such as thyroidectomy, which could
help to successfully manage this condition.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
QZ, YS, HZ, GR and YW performed the surgeries. GR
and YW collected and analyzed the data. GR and YW wrote the
manuscript. QZ and YS conceived the study, revised the manuscript
and confirmed the authenticity of all the raw data. All authors
have read and approved the final manuscript.
Ethics approval and consent to
participate
The present study was approved by the Ethics
Committee of Weifang Hospital of Traditional Chinese Medicine
(approval no. WF2023011302).
Patient consent for publication
Written informed consent was obtained from the
patient for publication.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Cady B: Management of tracheal obstruction
from thyroid diseases. World J Surg. 6:696–701. 1982.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Kadhim AL, Sheahan P and Timon C:
Management of life-threatening airway obstruction caused by benign
thyroid disease. J Laryngol Otol. 120:1038–1041. 2006.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Testini M, Logoluso F, Lissidini G,
Gurrado A, Campobasso G, Cortese R, De Luca GM, Franco IF, De Luca
A and Piccinni G: Emergency total thyroidectomy due to non
traumatic disease. Experience of a surgical unit and literature
review. World J Emerg Surg. 7(9)2012.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Schuster-Bruce J, Sargent P, Madden B, Ofo
E and Allin D: A systematic review of endotracheal stenting in
patients with locally advanced thyroid cancer. Clin Otolaryngol.
47:414–423. 2022.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Rohana A and Hisham AN: Emergency thyroid
surgery: A surgical challenge. Asian J Surg. 32:81–84.
2009.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Furman RH, Backer CL, Dunham ME, Donaldson
J, Mavroudis C and Holinger LD: The use of balloon-expandable
metallic stents in the treatment of pediatric tracheomalacia and
bronchomalacia. Arch Otolaryngol Head Neck Surg. 125:203–207.
1999.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Noppen M, Poppe K, D'Haese J, Meysman M,
Velkeniers B and Vincken W: Interventional bronchoscopy for
treatment of tracheal obstruction secondary to benign or malignant
thyroid disease. Chest. 25:723–730. 2004.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Tsutsui H, Kubota M, Yamada M, Suzuki A,
Usuda J, Shibuya H, Miyajima K, Sugino K, Ito K, Furukawa K and
Kato H: Airway stenting for the treatment of laryngotracheal
stenosis secondary to thyroid cancer. Respirology. 13:632–638.
2008.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Kim JH, Shin JH, Song HY, Ohm JY, Lee JM,
Lee DH and Kim SW: Palliative treatment of inoperable malignant
tracheobronchial obstruction: Temporary stenting combined with
radiation therapy and/or chemotherapy. AJR Am J Roentgenol.
193:W38–W42. 2009.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Stramiello JA, Mohammadzadeh A, Ryan J and
Brigger MT: The role of bioresorbable intraluminal airway stents in
pediatric tracheobronchial obstruction: A systematic review. Int J
Pediatr Otorhinolaryngol. 139(110405)2020.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Kim WK, Shin JH, Kim JH, Song JW and Song
HY: Management of tracheal obstruction caused by benign or
malignant thyroid disease using covered retrievable self-expandable
nitinol stents. Acta Radiol. 51:768–774. 2010.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Shen WT, Kebebew E, Duh QY and Clark OH:
Predictors of airway complications after thyroidectomy for
substernal goiter. Arch Surg. 139:656–659; discussion 659-660.
2004.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Ozdemir A, Hasbahceci M, Hamaloglu E and
Ozenc A: Surgical treatment of substernal goiter. Int Surg.
85:194–197. 2000.PubMed/NCBI
|
|
14
|
Testini M, Rosato L, Avenia N, Basile F,
Portincasa P, Piccinni G, Lissidini G, Biondi A, Gurrado A and
Nacchiero M: The impact of single parathyroid gland
autotransplantation during thyroid surgery on postoperative
hypoparathyroidism: A multicenter study. Transplant Proc.
39:225–230. 2007.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Ling Y, Zhao J, Zhao Y, Li K, Wang Y and
Kang H: Role of intraoperative neuromonitoring of recurrent
laryngeal nerve in thyroid and parathyroid surgery. J Int Med Res.
48(300060520952646)2020.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Na DG, Lee JH, Jung SL, Kim JH, Sung JY,
Shin JH, Kim EK, Lee JH, Kim DW, Park JS, et al: Radiofrequency
ablation of benign thyroid nodules and recurrent thyroid cancers:
Consensus statement and recommendations. Korean J Radiol.
13:117–125. 2012.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Ha EJ, Baek JH and Lee JH: The efficacy
and complications of radiofrequency ablation of thyroid nodules.
Curr Opin Endocrinol Diabetes Obes. 18:310–314. 2011.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Jeong WK, Baek JH, Rhim H, Kim YS, Kwak
MS, Jeong HJ and Lee D: Radiofrequency ablation of benign thyroid
nodules: Safety and imaging follow-up in 236 patients. Eur Radiol.
18:1244–1250. 2008.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Jacobs JP, Quintessenza JA, Botero LM, van
Gelder HM, Giroud JM, Elliott MJ and Herberhold C: The role of
airway stents in the management of pediatric tracheal, carinal, and
bronchial disease. Eur J Cardiothorac Surg. 18:505–512.
2000.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Rafanan AL and Mehta AC: Stenting of the
tracheobronchial tree. Radiol Clin North Am. 38:395–408.
2000.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Ruegemer JL, Perkins JA, Azarow KS,
O'Bryant LK, Nielsen RE and Thomas RW: Effect of the Palmaz
balloon-expandable metallic stent in the trachea of pigs.
Otolaryngol Head Neck Surg. 121:92–97. 1999.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Bhandari A, Wang YH, Lv SX, Xia EJ and
Wang OC: Novel strategy of stents in thyroid mass: A case series
report of managing severely dyspneic patients. Onco Targets Ther.
10:4997–5004. 2017.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Erbil Y, Bozbora A, Ademoglu E,
Salmaslioglu A and Ozarmagan S: Is timing important in thyroid
reoperation? J Otolaryngol Head Neck Surg. 37:56–64.
2008.PubMed/NCBI
|