Introduction
In 1895, the German surgeon, Hermann Kümmell,
described six patients with delayed compression fractures for the
first time (1). All of these
patients had a history of slight spinal trauma. After an
asymptomatic period lasting a few weeks or months, they experienced
progressive back pain, accompanied by a gradually worsening
kyphosis, and even neurological deficits. At first, Kümmell disease
was considered to be very rare; however, with the rapid development
of imaging technologies, particularly CT and MRI, the detection
rate of Kümmell disease increased significantly (2). The intravertebral vacuum cleft (IVC)
is a typical imaging manifestation (3). The exact pathogenesis of Kümmell
disease remains controversial and the majority of researchers
consider that it is caused by the ischemic necrosis of vertebral
bodies (4-8).
According to the clinical symptoms and the degree of
damage in the fractured vertebral body on a radiograph and MRI, Li
et al (9) divided Kümmell
disease into three stages as follows: Stage I, in which the loss of
vertebral body height is <20%, there is no degeneration of
adjacent intervertebral discs, no low back pain symptoms or mild
symptoms; stage II, in which the loss of vertebral body height is
<20%, the fractured vertebral body has dynamic instability and
there is adjacent intervertebral disc degeneration; stage III, in
which the posterior cortex breakage is accompanied by dynamic
instability and kyphosis of the vertebral body leads to spinal
canal stenosis with or without neurological deficits. According to
relevant literature reports (2,4,5,10,11),
percutaneous vertebroplasty (PVP) and percutaneous kyphoplasty
(PKP) have achieved good clinical outcomes in the treatment of
stage I and II Kümmell disease, and even stage III Kümmell disease
without neurological deficits can also be treated by PKP. Although
both Kümmell disease and common osteoporotic vertebral compression
fracture (OVCF) can be treated with PKP or PVP, there are still
significant differences in post-operative radiographs between them.
Polymethyl methacrylate (PMMA) in common OVCF surgery is evenly
distributed in the fractured vertebra and PMMA and bone trabeculae
are interlocked with each other. However, PMMA in Kümmell disease
is mainly concentrated in the IVC of the fractured vertebra to form
a bone cement mass, which has a clear boundary with the surrounding
bone. In this case, PMMA is very easy to loosen at the bone-cement
interface, which will lead to the recurrence of vertebral
instability, and the patient's low back pain will once again
worsen, even with neurological deficits (3,8,12-14).
Therefore, for patients with Kümmell disease, identifying a method
to firmly fix the PMMA in the IVC to prevent loosening is the key
to achieving good clinical outcomes.
The present study attempted to solve the problem of
PMMA loosening by using a modified PVP technique. The present study
aimed to evaluate the clinical efficacy of the bilateral pedicle
cement anchoring technique combined with the postural reduction in
PVP for Kümmell disease.
Patients and methods
Patients
Written informed consent was obtained from each
patient and the use of any relevant clinical images was authorized
by the patient for scientific research and online open-access
publication. The present study was approved by the Ethics Committee
of Yantaishan Hospital (Yantai, China; approval no. 20211005028).
The study protocol strictly adhered to the ethical guidelines of
The Declaration of Helsinki 1975(15).
Based on the sample size calculation formula
N=2[1+(K+1)ρ][(σ2(Z1-α+Z1-β)2/Kδ2)],
the hospital statistician suggested that the minimum sample size
(N) should be ≥16 cases to obtain meaningful statistical results
based on the incidence of Kümmell disease, based on confidence
intervals (α and β), the critical value of the normal distribution
(Z), the number of repeated measurements (K), smallest meaningful
difference to be detected (δ), measurement standard deviation (σ)
and internal correlation coefficient (ρ).
Between January 2018 and June 2021, a total of 26
patients diagnosed with Kümmell disease based on medical history,
radiograph (Multix Fusion; Siemens Healthineers), 128-detector
multislice CT scanner (Somatom Definition Flash; Siemens
Healthineers) and 1.5-T MRI (Magnetom Aera; Siemens Healthineers)
were visited at Yantaishan Hospital (Yantai, China; approval no.
20211005028) and retrospectively included in the present study.
However, the patients with ≥2 spinal vertebral fractures, tumors,
infections, pedicle fractures and neurological deficits were
excluded from the present study. All patients were initially
screened according to the exclusion criteria and a total of eight
patients were excluded from the study, including three with
multilevel involvements, one with pedicle fracture, and three with
neurological deficits. Finally, 18 patients were included in this
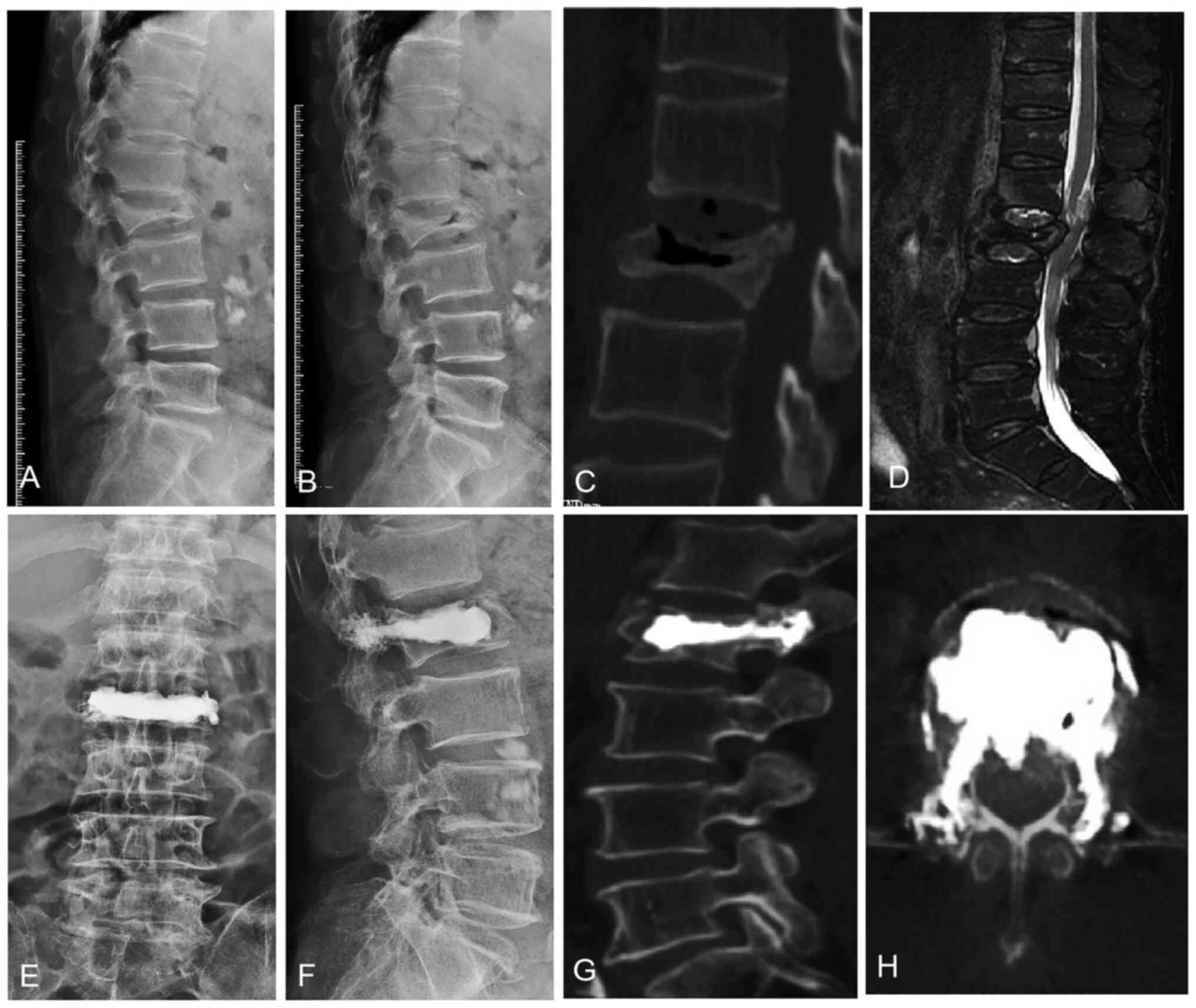
study (Fig 1A-D). All patients
were treated with PVP with the bilateral pedicle cement anchoring
technique and postural reduction. The surgeries were performed by
the same experienced surgeon at the Department of Spine Surgery,
Yantaishan Hospital. In terms of sex distribution, the study
involved five male and 13 female patients. The age of the patients
ranged from 69-82 years, with an average age of 76.5±3.8 years. In
total, 15 of the 18 patients had senile diseases, including six
cases of hypertension, three cases of diabetes, three cases of
coronary heart disease and three cases of diabetes with coronary
heart disease, which were well controlled during the peri-operative
period. The other demographic and clinical data, such as bone
mineral density (BMD), fractured level, injected cement volume,
etc., are presented in Table I.
BMD was measured using dual-energy X-ray absorptiometry and
osteoporosis was defined by a T-score ≤-2.5 standard deviations
(SD).
 | Table IDemographic and clinical data. |
Table I
Demographic and clinical data.
| | | | | | Visual analogue scale
score | Oswestry disability
index, % | Cobb angle, deg | Anterior vertebral
height, mm | | | |
|---|
| Case no. | Sex/age, years | Level | Bone mineral
density | Injected cement
volume, ml | Pre | Post | FFU | Pre | Post | FFU | Pre | Post | FFU | Pre | Post | FFU | FFU, months | Complication | Comorbidity |
|---|
| 1 | F/75 | L2 | -3.1 | 9.5 | 8 | 2 | 2 | 90 | 24 | 26 | 18 | 7 | 8 | 12 | 19 | 18 | 9 | - | HTN |
| 2 | F/78 | L1 | -3.5 | 8 | 8 | 2 | 3 | 86 | 30 | 30 | 12 | 8 | 8 | 13 | 15 | 15 | 6 | - | DM |
| 3 | M/80 | T12 | -4.2 | 8.5 | 9 | 3 | 4 | 92 | 36 | 42 | 22 | 12 | 16 | 10 | 15 | 13 | 8 | ACL, AVF | DM, CHD |
| 4 | F/76 | L1 | -2.8 | 9 | 8 | 1 | 1 | 86 | 24 | 26 | 20 | 9 | 10 | 13 | 17 | 17 | 10 | - | DM |
| 5 | M/75 | L1 | -3.6 | 8 | 7 | 1 | 2 | 82 | 20 | 20 | 16 | 8 | 9 | 14 | 18 | 17 | 8 | - | - |
| 6 | F/82 | T12 | -3.2 | 9.5 | 9 | 2 | 3 | 92 | 28 | 30 | 24 | 10 | 12 | 10 | 18 | 17 | 7 | - | HTN |
| 7 | F/73 | T10 | -2.8 | 8.5 | 9 | 1 | 1 | 88 | 16 | 20 | 15 | 7 | 7 | 11 | 16 | 16 | 10 | ACL | CHD |
| 8 | F/76 | T12 | -3 | 7 | 8 | 2 | 2 | 86 | 20 | 24 | 24 | 10 | 12 | 11 | 22 | 19 | 8 | - | HTN |
| 9 | M/82 | L1 | -3.4 | 10.5 | 9 | 2 | 3 | 94 | 40 | 44 | 22 | 12 | 17 | 13 | 20 | 16 | 7 | AVF | HTN |
| 10 | F/75 | L1 | -2.7 | 8 | 8 | 1 | 2 | 80 | 18 | 20 | 15 | 9 | 9 | 14 | 21 | 20 | 11 | - | DM, CHD |
| 11 | F/78 | L2 | -3 | 9.5 | 8 | 1 | 1 | 78 | 16 | 16 | 17 | 10 | 10 | 15 | 19 | 19 | 8 | ACL | HTN |
| 12 | M/69 | T12 | -2.8 | 7.5 | 9 | 1 | 1 | 90 | 20 | 22 | 20 | 14 | 15 | 14 | 20 | 19 | 10 | - | - |
| 13 | F/81 | L3 | -3.5 | 9 | 8 | 2 | 2 | 92 | 36 | 40 | 13 | 10 | 10 | 16 | 18 | 18 | 7 | - | DM, CHD |
| 14 | M/77 | L1 | -2.9 | 7 | 8 | 1 | 1 | 76 | 14 | 18 | 18 | 10 | 11 | 16 | 22 | 21 | 10 | - | - |
| 15 | F/74 | T12 | -3.5 | 7.5 | 7 | 1 | 2 | 86 | 22 | 24 | 20 | 12 | 16 | 13 | 19 | 18 | 6 | ACL | CHD |
| 16 | F/70 | L1 | -2.6 | 8 | 7 | 1 | 1 | 78 | 16 | 18 | 19 | 8 | 8 | 16 | 21 | 19 | 10 | - | HTN |
| 17 | M/81 | T12 | -3.8 | 9.5 | 9 | 2 | 3 | 92 | 32 | 38 | 22 | 10 | 13 | 14 | 20 | 16 | 9 | - | CHD |
| 18 | F/75 | L1 | -3.2 | 8.5 | 8 | 2 | 2 | 88 | 26 | 30 | 21 | 13 | 15 | 13 | 19 | 18 | 8 | ACL | DM |
Surgical procedure
All surgeries were performed under local anesthesia.
The patient was placed in a prone position on a Jackson operating
table, the chest and iliac region were elevated and the abdomen was
suspended, so that the fractured vertebra was opened and
repositioned as much as possible under the hyperextension position.
The bilateral transpedicular approach was performed under biplanar
fluoroscopic guidance. Unlike traditional PVP surgery, the puncture
point was located in the outer upper quadrant of the pedicle, and
the needle angle was more vertical to avoid injury to the inner and
lower walls of the pedicle as much as possible. First, under the
guidance of fluoroscopy, the trocar and cannula systems are placed
into the vertebral body through one side of the pedicle. The ideal
position was that the needle tip was located in the IVC. Second,
the drill was advanced to create a tunnel and then it was removed
and Polymethylmethacrylate (PMMA, Tecres, Spa.) was injected into
the vertebra. PMMA was divided into several 1-ml syringes in
advance; thus, it was easy to evaluate the injected cement volume
by counting the number of syringes used. Generally, the early
injected PMMA cement was located in the IVC. After the IVC was
filled, it was necessary to slowly inject PMMA cement while
retreating the working cannula. In particular, when the working
cannula was located in the pedicle, the injection speed of PMMA
cement needed to be slower. At the same time, it was necessary to
observe whether there was PMMA cement leakage under fluoroscopy and
to ask the patient whether there was nerve irritation. Similarly,
the same operation was performed on the opposite side to finally
complete the surgical procedure.
Clinical and radiological
assessment
Clinical and radiological assessments were performed
pre-operatively, 1 day after the surgery and at the final
follow-up. The visual analogue scale (VAS) was used to assess the
degree of lower back pain and the Oswestry disability index (ODI)
was used to assess the degree of dysfunction (16,17).
Radiological data were obtained and measured through the hospital's
image archiving and communication systems (PACS) under
authorization. The change in the anterior vertebral height (AVH)
was obtained by measuring lateral radiographs or sagittal CT
images. A straight line was drawn from the superior endplate one
level above the fractured vertebral body and a straight line was
then drawn from the inferior endplate of the one level below the
fractured vertebral body. The intersection of the two lines was
defined as the Cobb angle (Fig.
1A). The last follow-up time and postoperative complications
were also recorded and analyzed (Table
I). The criteria for judging the post-operative loosening of
PMMA cement were as follows: i) VAS or ODI scores of the patient
were significantly worse than those on the first day after surgery;
ii) instability of PMMA cement could be observed on a lateral
radiograph film of the flexion and extension position; iii) on
T2-weighted sagittal images of an MRI, there was an obvious annular
edema enhancement zone between the PMMA cement and the surrounding
bone (Fig. 1E-H).
Treatment of osteoporosis
Regular anti-osteoporosis treatment was performed
throughout the course of the treatment and during follow-up.
Patients were advised to take daily calcium and vitamin D
supplements, as well as bisphosphonates. Teriparatide is currently
recommended for patients as a first-line anti-osteoporosis
treatment option as well.
Statistical analysis
All statistical analyses were performed using SPSS
19.0 software (IBM Corp.). Each variable is presented as the mean ±
SD. Data were analyzed using repeated measures ANOVA and the
Bonferroni post hoc test. P<0.05 was considered to indicate a
statistically significant difference.
Results
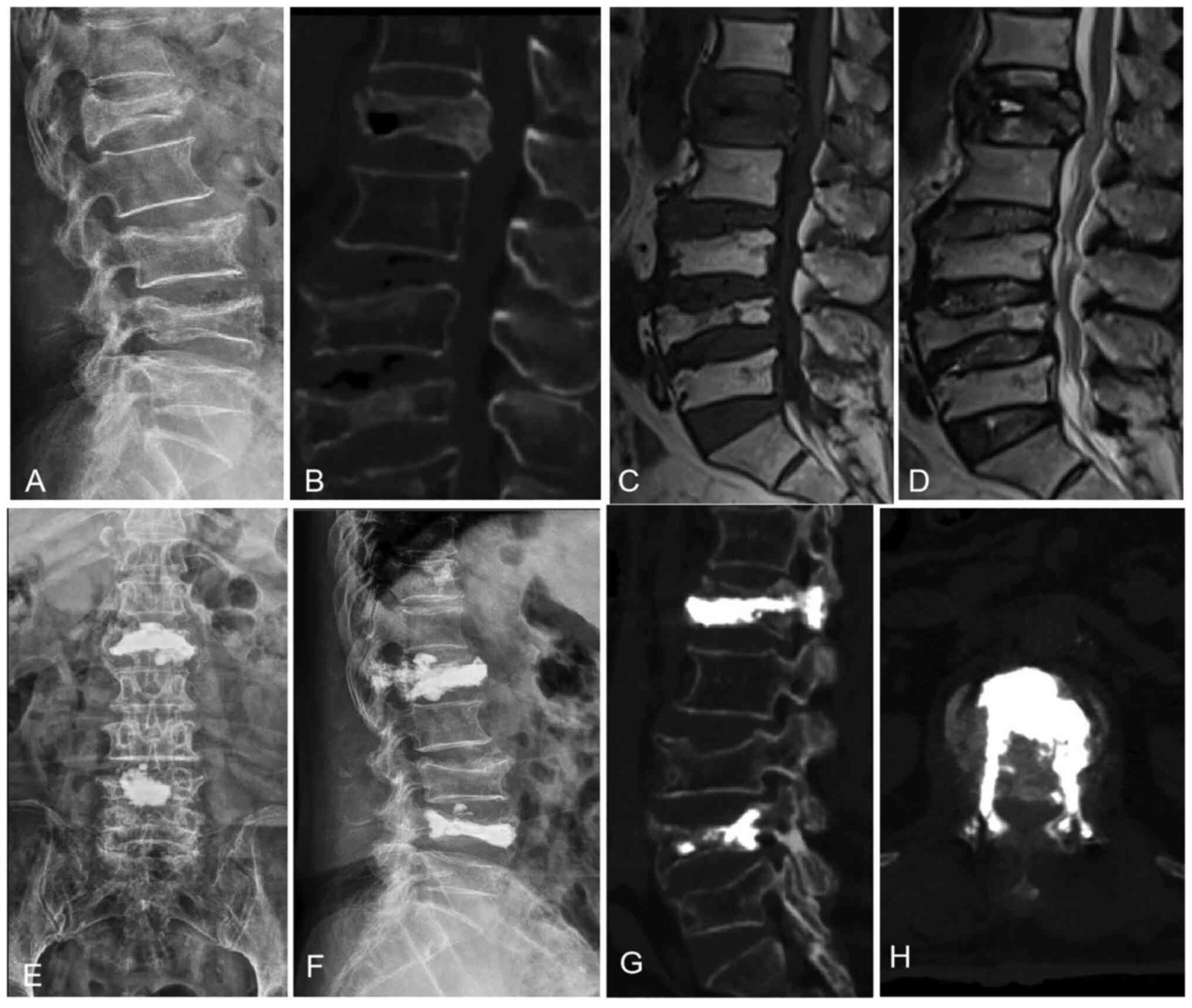
The modified PVP surgery used herein was
successfully performed in all patients (Figs. 2 and 3). The mean follow-up duration was
8.4±1.2 months (range, 6-11 months). The fractured vertebrae were
mainly located in the thoracolumbar region (T10-L2): One in T10;
three in T11; five in T12; six in L1; two in L2 and one in L3. The
mean T-score of BMD in the present study was -3.2±0.4 SD (range,
-2.6--4.2 SD). The mean injected cement volume was 8.5±1.0 ml
(range, 7-10.5 ml).
The back pain of the patients improved significantly
after the surgery, and their self-care ability and quality of life
also significantly improved (Table
II). The average pre-operative VAS score was 8.17±0.71 (range,
7-9) and the VAS score on the first day after surgery decreased to
1.56±0.62 (range, 1-3). The difference was statistically
significant between the two groups before and after surgery
(P<0.05). The pain relief continued to be maintained. Until the
final follow-up, the VAS score remained at 2.00±0.91 (range, 1-4),
with only a slight change compared with that on the first day after
surgery. The average pre-operative ODI was 86.44±5.5 (range,76-94)
and the ODI on the first day after surgery decreased to 24.33±7.82
(range, 14-40). Until the final follow-up, the ODI remained at
27.11±8.76 (range, 16-44).
 | Table IIComparisons of preoperative,
postoperative and final follow-up clinical parameters. |
Table II
Comparisons of preoperative,
postoperative and final follow-up clinical parameters.
| Parameters | Preoperative | Postoperative | Final
follow-up | Fa |
|---|
| Visual analogue
scale | 8.17±0.71 |
1.56±0.62b |
2.00±0.91b,c | 920.98 |
| Oswestry disability
index, % | 86.44±5.5 |
24.33±7.82b |
27.11±8.76b,c | 2,464.97 |
| Cobb angle,
deg | 18.77±3.55 |
9.94±2.01b |
11.83±3.96b,c | 122.45 |
| Anterior vertebral
height, mm | 13.22±1.90 |
18.83±2.12b |
17.56±1.91b,c | 101.87 |
The mean Cobb angles and anterior vertebral heights
were significantly improved compared with those before surgery. The
Cobb angles decreased from 18.77±3.55˚ (range, 12-24˚)
pre-operatively to 9.94±0.21˚ (range, 7-14˚) on the first day after
surgery. At the final follow-up, the Cobb angles remained at
11.83±3.96˚ (range, 7-20˚). The anterior vertebral heights
increased from 13.22±1.90 mm (range, 10-16 mm) pre-operatively to
18.83±2.12 mm (range, 15-22 mm) on the first day after surgery. At
the final follow-up, the anterior vertebral heights remained at
17.56±1.91 mm (raange, 13-21 mm). Statistically significant
differences were found in kyphosis correction and vertebral height
recovery between the pre-operative and post-operative time points
(P<0.05).
During the surgery and follow-up, no serious
complications were encountered, such as pulmonary embolism,
neurological deficits, cardiac arrest, etc. Similar to the
traditional PVP procedure, PMMA cement leakage continues to be the
most common complication. In the present study, five patients
exhibited an asymptomatic leakage of PMMA cement and did not
receive any specific treatment. In total, two patients with
adjacent vertebral fractures were treated with PVP and the symptoms
improved significantly. The loosening of cement was not observed in
any of the patients.
Discussion
Although the mechanism of Kümmell disease remains
controversial, delayed avascular osteonecrosis of the vertebral
body is widely accepted (1,4-7).
Kümmell disease can be regarded as a specific type of OVCF. The
anterior 1/3 of the vertebral body is supplied by the terminal
artery of the single segmental artery (6,14).
For elderly patients with osteoporosis, the blood supply of the
vertebral terminal artery is weakened due to arteriosclerosis. At
this time, a minor vertebral fracture will cause the interruption
of the blood supply, leading to avascular necrosis of the vertebral
body and a nonunion fracture. With the increase in avascular
osteonecrosis, IVC may occur and, eventually, the vertebral body
collapses. At the same time, the patient's back pain becomes more
severe, even with neurological deficits (8,18,19).
According to the patient's medical history,
photograph, CT and MRI examinations, the diagnosis of Kümmell
disease is not difficult at present (4). The appearance of IVC is a typical
manifestation in an imaging examination. On MRI images, it can be
observed that IVC is filled with gas or liquid which undergo a
dynamic change according to the patient's position and bed rest
time (20,21). On T2-weighted images, a double-line
sign can be observed: The periphery of IVC is surrounded by a
hyperintensity zone and the outer layer is surrounded by
hypointense sclerotic bone (3).
Hasegawa et al (22)
through the IVC histological examination of five patients found
that the hyperintensity zone consisted of fibrocartilage tissue.
Therefore, due to these characteristics, traditional conservative
treatments such as a brace, bed rest and analgesics may not be
suitable for the treatment of Kümmell disease (8,23-25).
At present, similar to the treatment of common OVCF, PVP or PKP
remains the first choice for Kümmell disease without neurological
deficits. However, for patients with common OVCF, bone cement and
trabecular bone are fully interdigitated in the vertebral body,
while for patients with Kümmell disease, bone cement is mainly
concentrated in IVC, which has a clear boundary with the
surrounding vertebral body and there is no sufficient mechanical
interlock between them (14). In
this case, the bone cement mass in IVC gradually loosens, the scope
of ischemic osteonecrosis is further expanded under repeated stress
and, finally, kyphosis is aggravated due to the re-collapse of the
vertebral body. Heo et al (14) reported that among 21 patients with
Kümmell disease treated with PVP, six patients had vertebral body
re-collapse during follow-up and the incidence of re-collapse was
28.57%. Their study suggested that PVP may be a relative
contraindication of Kümmell disease (14). Kim and Kim (3) also reported that the corrected
kyphotic angles may be reaggravated over time after PKP, suggesting
that PKP is not suitable for Kümmell disease. On the contrary,
through a prospective cohort study, Chang et al (5) found that PVP and PKP could achieve
good clinical outcomes in the treatment of Kümmell disease and
there was no significant difference between the two surgical
methods during long-term follow-up.
In the present study, the PMMA cement mass was
firmly fixed in the IVC in the vertebral body through the bilateral
pedicle cement anchoring technology under postural reduction. The
bilateral pedicle and the PMMA cement mass formed a
three-dimensional stable structure, which prevented as much as
possible the loosening of PMMA cement in the IVC. The VAS and ODI
scores of the patients after surgery were significantly improved
compared with those before surgery. Pain and quality of life
improved and were maintained well during follow-up. The Cobb angles
of the patients after surgery also significantly improved. Although
a slight correction loss occurred during follow-up, the difference
was not statistically significant. In the present study, PVP was
selected as the surgical method for Kümmell disease rather than
PKP. It was considered that PKP has no obvious advantage over PVP
in the treatment of Kümmell disease (5). Due to the existence of IVC, the
natural opening of the vertebral body can be achieved through
postural reduction under the prone position, and kyphosis can be
corrected to a certain extent. Although PKP balloon dilation can
achieve a greater kyphosis correction, relevant research has shown
that excessive kyphosis correction cannot achieve good clinical
outcomes. Kim and Kim (3)
indicated that excessive kyphosis correction could cause
instability of the fractured vertebra, leading to the injury of
paravertebral soft tissues and ligaments. PKP appears to be
unnecessary for Kümmell disease.
As with the traditional PVP procedure, PMMA cement
leakage remains the most common complication. In the present study,
the leakage rate of bone cement was 27.8%. Chang et al
(5) reported that the bone leakage
rates for Kümmell disease were 17.9 and 10.7% in the PVP and PKP
groups, respectively. As bone cement is mainly concentrated in the
IVC and is surrounded by sclerotic bone, the leakage rate of bone
cement may be lower than PVP for common OVCF (26). Another common complication is an
adjacent vertebral fracture and the incidence rate (11.1%) of the
present study was similar to that in a previous study (27).
However, the present study still had the following
limitations. First of all, the present study was a retrospective
study with small sample size. Although good clinical outcomes were
achieved, a prospective, randomized controlled study with a larger
sample size is required to further verify its clinical efficacy.
Secondly, the follow-up time in the present study did not exceed 12
months. Whether vertebral re-collapse will occur, causing further
aggravation remains unclear. Thus, the present authors aim to
continue the long-term follow-up. In the future, the present
authors aim to conduct a multicenter, prospective, randomized
controlled study to compare the differences between the bilateral
pedicle cement anchoring technique and traditional PVP technology
in the treatment of Kümmell disease. The research protocol has been
submitted to the hospital ethics committee for approval.
In conclusion, as demonstrated in the present study,
during the treatment of Kümmell disease with PVP, the bilateral
pedicle cement anchoring technique combined with postural reduction
can effectively be used to prevent the loosening of PMMA cement in
IVC, the aggravation of vertebral re-collapse and kyphosis. As a
modified PVP technology, it can achieve good clinical outcomes.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
WD designed the research plan and wrote the
manuscript. DZ performed the statistical analysis of the research
data and assisted WD in the writing of the manuscript. HW, XS and
YZ were responsible for data collection. All authors read and
approved the final version of the manuscript. DZ and WD confirm the
authenticity of all the raw data.
Ethics approval and consent to
participate
Written informed consent was obtained from each
patient and the present study was approved by the Ethics Committee
of Yantaishan Hospital (approval no. 20211005028). The authors
declare that the methods carried out in this study were following
The Declaration of Helsinki.
Patient consent for publication
The use of any relevant clinical images was
authorized by the patient for scientific research and online
open-access publication.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Zhang X, Hu W, Yu J, Wang Z and Wang Y: An
effective treatment option for Kümmell disease with neurological
deficits: Modified transpedicular subtraction and disc osteotomy
combined with long-segment fixation. Spine (Phila Pa 1976).
41:e923–e930. 2016.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Chen GD, Lu Q, Wang GL, Zou J, Yang HL,
Yang Y and Luo ZP: Percutaneous kyphoplasty for kummell disease
with severe spinal canal stenosis. Pain Physician. 18:E1021–E1028.
2015.PubMed/NCBI
|
|
3
|
Kim P and Kim SW: Balloon kyphoplasty: An
effective treatment for kümmell disease? Korean J Spine.
13:102–106. 2016.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Huang Y, Peng M, He S, Tang X, Dai M and
Tang C: Clinical efficacy of percutaneous kyphoplasty at the
hyperextension position for the treatment of osteoporotic Kümmell
disease. Clin Spine Surg. 29:161–166. 2016.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Chang JZ, Bei MJ, Shu DP, Sun CJ, Chen JB
and Xiao YP: Comparison of the clinical outcomes of percutaneous
vertebroplasty vs. kyphoplasty for the treatment of osteoporotic
Kümmell's disease:A prospective cohort study. BMC Musculoskelet
Disord. 21(238)2020.PubMed/NCBI View Article : Google Scholar
|
|
6
|
He D, Yu W, Chen Z, Li L, Zhu K and Fan S:
Pathogenesis of the intravertebral vacuum of Kümmell's disease. Exp
Ther Med. 12:879–882. 2016.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Kim YC, Kim YH and Ha KY: Pathomechanism
of intravertebral clefts in osteoporotic compression fractures of
the spine. Spine J. 14:659–666. 2014.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Yu W, Liang D, Yao Z, Qiu T, Ye L, Huang X
and Jiang X: Risk factors for recollapse of the augmented vertebrae
after percutaneous vertebroplasty for osteoporotic vertebral
fractures with intravertebral vacuum cleft. Medicine (Baltimore).
96(e5675)2017.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Li KC, Li AF, Hsieh CH, Liao TH and Chen
CH: Another option to treat Kümmell's disease with cord
compression. Eur Spine J. 16:1479–1487. 2007.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Chen LH, Lai PL and Chen WJ: Unipedicle
percutaneous vertebroplasty for spinal intraosseous vacuum cleft.
Clin Orthop Relat Res. 435:148–153. 2005.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Dai SQ, Qin RQ, Shi X and Yang HL:
Percutaneous vertebroplasty versus kyphoplasty for the treatment of
neurologically intact osteoporotic Kümmell's disease. BMC Surg.
21(65)2021.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Wang HS, Kim HS, Ju CI and Kim SW: Delayed
bone cement displacement following balloon kyphoplasty. J Korean
Neurosurg Soc. 43:212–214. 2008.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Nakamae T, Yamada K, Tsuchida Y, Osti OL,
Adachi N and Fujimoto Y: Risk factors for cement loosening after
vertebroplasty for osteoporotic vertebral fracture with
intravertebral cleft: A retrospective analysis. Asian Spine J.
12:935–942. 2018.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Heo DH, Chin DK, Yoon YS and Kuh SU:
Recollapse of previous vertebral compression fracture after
percutaneous vertebroplasty. Osteoporos Int. 20:473–480.
2009.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Shephard DA: The 1975 declaration of
helsinki and consent. Can Med Assoc J. 115:1191–1192.
1976.PubMed/NCBI
|
|
16
|
Heller GZ, Manuguerra M and Chow R: How to
analyze the visual analogue scale: Myths, truths and clinical
relevance. Scand J Pain. 13:67–75. 2016.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Fairbank JC and Pynsent PB: The oswestry
disability index. Spine (Phila Pa 1976). 25:2940–2952.
2000.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Libicher M, Appelt A, Berger I, Baier M,
Meeder PJ, Grafe I, Dafonseca K, Nöldge G and Kasperk C: The
intravertebral vacuum phenomen as specific sign of osteonecrosis in
vertebral compression fractures: Results from a radiological and
histological study. Eur Radiol. 17:2248–2252. 2007.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Chongyan W, Zhang X, Li S, Liu J, Shan Z,
Wang J, Chen J, Fan S and Zhao F: Mechanism of formation of
intravertebral clefts in osteoporotic vertebral compression
fractures: An in vitro biomechanical study. Spine J. 18:2297–2301.
2018.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Linn J, Birkenmaier C, Hoffmann RT, Reiser
M and Baur-Melnyk A: The intravertebral cleft in acute osteoporotic
fractures: Fluid in magnetic resonance imaging-vacuum in computed
tomography? Spine (Phila Pa 1976). 34:e88–e93. 2009.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Lane JI, Maus TP, Wald JT, Thielen KR,
Bobra S and Luetmer PH: Intravertebral clefts opacified during
vertebroplasty: Pathogenesis, technical implications, and
prognostic significance. AJNR Am J Neuroradiol. 23:1642–1646.
2002.PubMed/NCBI
|
|
22
|
Hasegawa K, Homma T, Uchiyama S and
Takahashi H: Vertebral pseudarthrosis in the osteoporotic spine.
Spine (Phila Pa 1976). 23:2201–2206. 1998.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Qin R, Zhang X, Liu H, Zhou B, Zhou P and
Hu C: Application of anchoring technique in unilateral percutaneous
vertebroplasty for neurologically intact Kümmell's disease. Pain
Res Manag. 24(4145096)2020.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Wang W, Liu Q, Liu WJ, Li QB, Cai L and
Wang ZK: Different performance of intravertebral vacuum clefts in
Kümmell's disease and relevant treatment strategies. Orthop Surg.
12:199–209. 2020.PubMed/NCBI View
Article : Google Scholar
|
|
25
|
Wang Y, Liu B, Sun Z, Zhang Y and Su J:
Comparative efficacy of three minimally invasive procedures for
kümmell's disease: A systematic review and network meta-analysis.
Front Surg. 9(893404)2022.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Krauss M, Hirschfelder H, Tomandl B,
Lichti G and Bär I: Kyphosis reduction and the rate of cement leaks
after vertebroplasty of intravertebral clefts. Eur Radiol.
16:1015–1021. 2006.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Park JW, Park JH, Jeon HJ, Lee JY, Cho BM
and Park SH: Kümmell's disease treated with percutaneous
vertebroplasty: Minimum 1 year follow-up. Korean J Neurotrauma.
13:119–123. 2017.PubMed/NCBI View Article : Google Scholar
|