Introduction
IgG4-related disease (IgG4-RD) is a chronic
inflammatory disease related to fibrosis that is mediated by the
immune system. The characteristic features of IgG4-RD include
elevated serum IgG4 levels, infiltration of abundant IgG4+ plasma
cells and lymphocytes and fibrosis in affected organs (1). This disease may occur in various
parts of the body, with the pancreas being the most commonly
involved organ, followed by the hepatobiliary system, salivary
glands, lacrimal glands, lungs, posterior peritoneum, kidneys and
prostate (1,2). Furthermore, IgG4-RD is a disease
characterized by involvement of multiple organs and systems. Due to
the limited knowledge and understanding of IgG4-RD, it is common
for doctors to misdiagnose IgG4-RD as malignant or infectious
lesions, resulting in certain patients undergoing unnecessary
surgical interventions. However, as an immune-mediated systemic
disease, IgG4-RD was indicated to show excellent responses to
glucocorticoid therapy (2,3). Thus, early diagnosis and accurate
treatment are crucial for patients to acquire more benefits.
Imaging examinations are effective methods to find the lesions of
IgG4-RD. Furthermore, they may be used to describe the scope of
lesions and evaluate the efficiency of hormone therapy (2,4). The
present study reported a case of IgG4-RD of the bilateral distal
ureters, which are rarely involved in IgG4-RD, and the magnetic
resonance imaging (MRI) features were analyzed to improve the
understanding and diagnosis of the disease.
Case report
In September 2021, a 55-year-old male patient sought
medical attention at Xiangyang No. 1 People's Hospital (Xiangyang,
China) due to complaints of ‘lower back pain for one week’, without
any symptoms such as painful urination, gross hematuria, frequent
urination and urgency of urination. The medical record indicated a
history of oral medication therapy for hypertension and
hypothyroidism. Physical examination on admission found no obvious
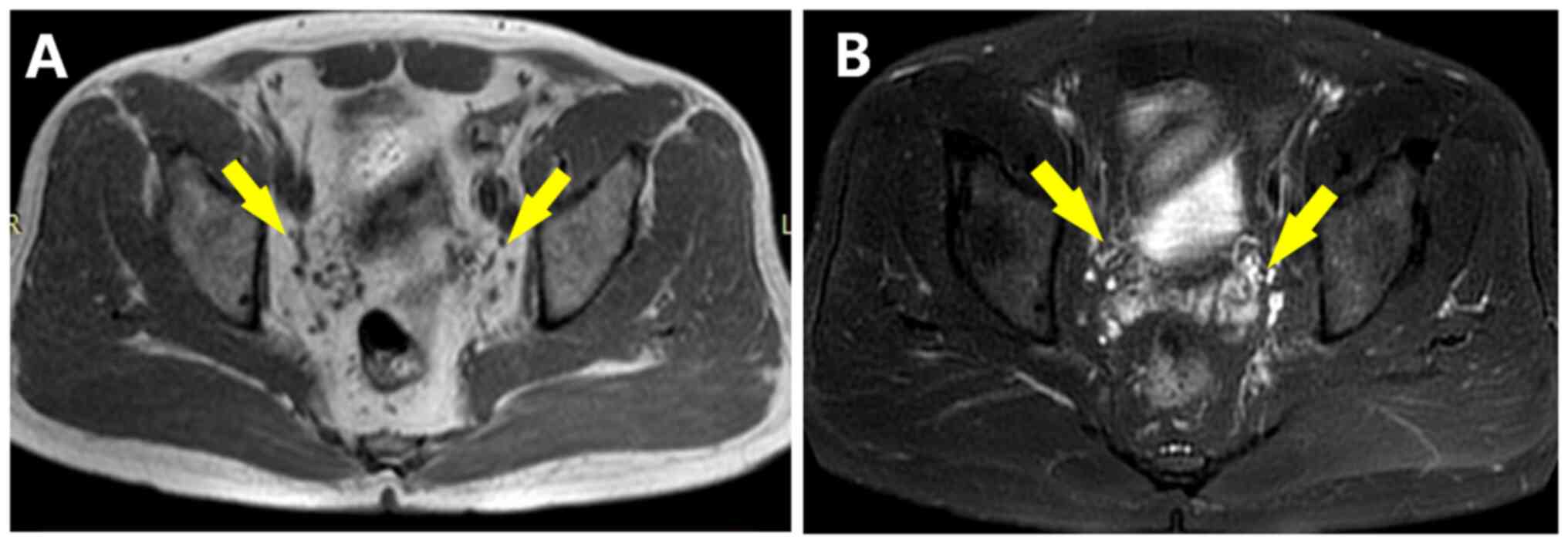
abnormality. MRI showed symmetrical soft tissue masses around the
bilateral distal ureters, with equal signal on T1-weighted imaging
(T1WI) (Fig. 1A), slightly higher
signal on T2WI (Fig. 1B) and
significant enhancement (Fig. 1C
and D). In the diffusion-weighted
imaging sequence (DWI), the lesions had a high signal (Fig. 1E), while they had a low signal in
the apparent diffusion coefficient (ADC) image (Fig. 1F). The size of the larger mass was
25x23x35 mm and the smaller one was 18x21x23 mm(right). Magnetic
resonance urography indicated stenoses of bilateral distal ureters
and proximal hydronephrosis (Fig.
2). The serological results revealed that the IgG4 level was
8.690 g/l (0.03-2.01, for IgG4-RD cutoff, >1.35 g/l), IL-6 level
was 7.1 pg/ml (normal range: 0.1-2.9 pg/ml)and IgE level was 255.10
IU/ml (normal, ≤100 IU/ml). Due to consideration of IgG4-RD,
prednisone acetate tablets (40 mg/day) and mycophenolate mofetil
dispersible tablets (1 g/day) were administered. After 30 days, the
IgG4 level had dropped to 4.610 g/l and the IgE level had decreased
to 130.60 IU/ml. After 6 months, the masses had disappeared
completely in the follow-up MRI (Fig.
3A and B). In May 2022,
laboratory examination at another hospital indicated that IgE and
IL-6 had dropped to normal. The patient continued to take
mesalazine dispersible tablets (0.5 g/day) to prevent relapse.
According to an MRI scan conducted in April 2023, there was no
significant recurrence of the lesions observed at the distal ends
of both ureters.
Discussion
Patients with IgG4-RD usually undergo a two-stage
progression, including an inflammatory phase and a fibrotic phase.
The inflammatory lesions of IgG4-RD may be related to immune
disorders, environmental pollution or drug abuse (5). According to a study conducted in
Japan, there has been an increase in the incidence rate of IgG4-RD
over a period of 10 years, from 0.8 cases per 100,000 individuals
to 3.1 cases per 100,000 individuals. This may be attributed to the
improvement in the diagnosis of IgG4-RD (6). Of note, IgG4-RDs more commonly occur
in middle-aged and elderly individuals (with an average age of 56
years) and males (7). An important
characteristic of IgG4-RD is its ability to affect multiple organs.
Several previous studies have provided insight into the prevalence
of multi organ involvement, reporting that it ranges from 51 to 92%
(7-10).
Furthermore, the symptoms of IgG4-RD are usually nonspecific and
vary according to the organs involved. For patients with
retroperitoneal IgG4-RD, the initial symptoms are milder and more
undetectable than those with other organs involved. As a result,
the diagnosis of retroperitoneal IgG4-RD may be delayed (11). Ureteral IgG4-RD is a fairly
uncommon condition that is predominantly reported as an individual
case with symptoms including lower back pain, loss of appetite and
renal dysfunction (12,13). In the case of the present study,
the patient only had lower back pain.
Thus far, there are no unified diagnostic criteria
for IgG4-RD. Elevated serum IgG4 is an important indicator for the
diagnosis and evaluation of IgG4-RD. It can be found in 55-97% of
cases, particularly in Asian patients, and it is correlated with
the number of organs involved (14). Serum IgG4 levels of >1.35 g/l
are considered strong evidence for the diagnosis of IgG4-RD
(15). However, elevated serum
IgG4 is not a specific biomarker for IgG4-RD, as it may be found in
numerous other diseases, such as tumors, infections, connective
tissue diseases, hematological diseases and allergic conditions. In
addition, not all patients with IgG4-RD have elevated serum IgG4
levels. Thus, higher serum IgG4 is neither sufficient nor necessary
for the diagnosis of IgG4-RD. Higher serum IL-6 is a marker to
reflect acute phase response (16). The IgG4 and IL-6 levels in the
present case were significantly elevated, which may support the
diagnosis and suggest that the disease is in an active phase.
The pathogenesis of IgG4-RD has remained to be
elucidated; however, it is thought to be mainly mediated by
immunological imbalance. Its main pathological features are
lymphocyte and plasma cell infiltration and fibrosis within the
affected tissues or organs, and the histopathological presentation
remains the gold standard for diagnosis (17). The pathological changes of IgG4-RD
provide an important basis for characteristic radiological
manifestations, particularly MRI signal changes and enhancement
patterns (7). Although the
international diagnostic criteria for IgG4-RD are different, they
all emphasize that imaging findings are the main basis for the
diagnosis of IgG4-RD (2),
particularly CT and MRI (18),
which may display the location, scope and shape and size of the
lesion. MRI is slightly superior to CT in determining the nature of
the lesion involving retroperitoneal organs. MRI may show a patchy
soft tissue signal shadow surrounding the anterolateral abdominal
aorta and the common iliac artery, which is similar to the psoas
major muscle signal, frequently causing medial displacement or
obstruction of the lower ureter (11). The imaging findings of
retroperitoneal IgG4-RD are mostly isodense on plain CT scan. MRI
shows an equal or slightly lower signal on T1WI and T2WI, and mild
to moderate delayed enhancement after enhancement (19). The characteristic imaging features
may be related to intrafocal fibrosis and more infiltration of
lymphocytes and plasma cells. When the lesion stays in the active
phase, T2WI shows high signal intensity (19). DWI is conducive to identifying
whether IgG4-RD is in the active phase and presenting similar
retroperitoneal malignancies (20). The ADC value of nonactive lesions
is higher than that of active lesions and retroperitoneal malignant
tumors. When a patient is clinically suspected to have IgG4-RD with
a retroperitoneal mass, a puncture biopsy of the retroperitoneal
lesion is often necessary. However, Raglianti et al
(19) suggested that when clinical
suspicion of retroperitoneal mass associated with IgG4-RD is
confirmed by serological examinations, and there are typical
imaging manifestations as described above, hormone treatment may be
directly initiated to avoid the potential risk of retroperitoneal
vascular injury caused by biopsy. IgG4-RD occurring in the ureter
is relatively rare and the imaging manifestation is often segmental
thickening of the ureter wall or the formation of local masses,
accompanied by mild to moderate hydronephrosis (13,21).
It may affect any part of the ureter, but unilateral involvement is
more common, with the left side being more frequently affected than
the right side (13). When the
ureter is affected unilaterally, it is difficult to differentiate
from ureteral malignancy. According to previous reports, it has
been frequently misdiagnosed as an ureteral malignancy prior to
surgery and surgical resection was performed (12,13,21).
However, in patients with ureteral IgG4-RD, the degree of
hydronephrosis is relatively mild compared to that with malignant
tumors (21). This may be because
the ureteral stenosis in this disease is mostly due to compression
by wall or peripheral inflammatory lesions, rather than direct
obstruction by intraluminal soft tissue masses (21). In cases where no malignant tumor
cells are found in cytological and ureteroscopic brush specimens,
particularly when the mass involves the bilateral ureters,
consideration should be given to the possibility of ureteral
IgG4-RD and further related serological immunological tests may be
performed to assist in the diagnosis. The imaging manifestation of
the case of the present study is relatively special, with the main
features being symmetrical, round, soft tissue signal masses at the
bilateral distal ureters, accompanied by limited lesions and
irregular morphology. The T2WI signal is higher than that of the
surrounding muscle and soft tissue, with significant enhancement,
diffusion limitation and a significant decrease in ADC value,
suggesting that the patient may be in the active stage, which is
prone to be misdiagnosed as a neoplastic lesion. The reasons for
the relatively accurate imaging diagnosis at initial MRI may
include the following: i) The lesion simultaneously involves the
bilateral ureters and symmetry development may be an important
basis for excluding other malignant tumors; ii) the signal of the
lesion is relatively uniform, without obvious cystic changes,
necrosis and bleeding; iii) the boundary of the lesion is
relatively vague with surrounding adipose tissue, while other
tumors at this site generally have clear boundaries or exhibit
aggressive growth patterns and peripheral tissue traction; iv)
bilateral hydronephrocalyces are not serious. Most malignant tumors
feature severe hydronephrosis, frequently accompanied by hematuria
(21).
IgG4-RD retroperitoneal lesions may be divided into
three subtypes based on the anatomical location and their
involvement (22): i) Surrounding
the abdominal aorta or iliac artery; ii) surrounding the renal
pelvis and ureter; iii) no clear correlation with any pelvic cavity
organ and only distributed behind the pelvic peritoneum. The first
subtype is the most common. When the lesion is localized around the
bilateral ureters, it is mainly differentiated from the following
malignant tumors in the ureter: A) Primary tumors of the ureter:
Clinically rare, most are transitional cell carcinoma. The major
clinical manifestation is recurrent gross hematuria. MRI often
shows a mass in the ureter or invade its surroundings, with T1WI
and T2WI signals higher and lower than those in urine,
respectively, and frequently uneven signals involving the outside
of the lumen. Symmetrical involvement of bilateral ureters is rare
and it is difficult to differentiate from unilateral ureteral
involvement of IgG4-RD. However, when urinary cytology examination
and ureteroscopic biopsy are inconclusive regarding malignant
tumors, IgG4-RD should be considered and further relevant serum
immunological tests should be performed (13,23).
B) Lymphoma: Lymphoma has a wide range, with common retroperitoneal
enlarged lymph nodes appearing from the peripancreatic level, and
some of them can be fused; ‘when the lymph nodes behind the
abdominal aorta are gradually enlarged, the abdominal aorta can be
pushed forward and obscure display, resulting in an aortic
submersion sign. However, the lymphoma is soft and rarely causes
bilateral ureteral stenosis’ (24). C) Periureteral metastatic tumor: It
can appear as a parenchymal mass or enlarged lymph nodes adjacent
to the ureter, the former having no obvious characteristics, while
the latter often presents as a single or multiple discontinuous
nodular lesions with a clear boundary. Most patients have a history
of primary malignant tumors.
Glucocorticoids are generally effective for IgG4-RD
and immunosuppressants are also necessary as drugs to induce
remission. The responsiveness of glucocorticoids to treatment is
also one of the diagnostic inclusion criteria for IgG4-RD (25). When IgG4-RD is suspected, timely
serum immunologic testing and hormone impact treatment may spare
patients from having to undergo surgery, radiotherapy and
chemotherapy. Biological targeted therapy, particularly the
anti-CD20 monoclonal antibody rituximab, has achieved good results
in the treatment of IgG4-RD (26).
Rituximab may be considered for patients who have failed
traditional treatment, experienced relapse during steroid tapering,
or have steroid resistance or intolerance. However, precautions
should be taken to prevent infection after using this medication.
In urgent situations where specific sites affected by IgG4-RD cause
organ dysfunction due to compression, if medication fails to
rapidly control the condition, surgical or interventional
treatments may be considered. IgG4-RD is a disease prone to
relapse. Different studies have reported risk factors for relapse,
including male gender, younger age, history of allergies, elevated
baseline serum IgG4 levels, low maintenance steroid dosage and
previous relapse history (27,28).
Furthermore, a subsequent increase in serum IgG4 levels during
follow-up is also a risk factor for disease relapse (29). In this case, the patient's IgG4 and
IgE levels significantly decreased after one month of combined
treatment with glucocorticoids and immunosuppressive agents. Six
months later, a follow-up MRI showed the disappearance of the
retroperitoneal mass, and thus, no further treatment with targeted
biological drugs or surgery was considered. The patient continued
to take mesalazine dispersible tablets (0.5 g/day) to prevent
relapse. In April 2023, the patient came to our hospital for
re-examination and pelvic MRI showed no obvious recurrence of
bilateral ureteral terminal masses. The prognosis has been good so
far. The patient has shown sensitivity and effectiveness to hormone
and immunosuppressive therapy, which provides strong evidence for
the diagnosis of IgG4-RD in this case.
Therefore, when clinically encountering patients
with subacute onset, only presenting with lower back pain and
retroperitoneal soft tissue masses surrounding the bilateral
ureters, the possibility of IgG4-RD should be considered and a
comprehensive diagnosis should be made in combination with
serological examination, imaging characteristics and treatment
response to avoid misdiagnosis.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
All data generated or analyzed during this study are
included in this published article.
Authors' contributions
JC, YW and PG contributed to the conceptualization
and design of the study and drafting of the manuscript. AG, PA, HC
and RC collected the patient's clinical information and images and
assisted with the drafting of the manuscript. YW and PG contributed
to critical revisions of the intellectual content and confirmed the
authenticity of all the raw data. All authors have read and
approved the final manuscript.
Ethics approval and consent to
participate
The present study was approved by the Institutional
Review Board of Xiangyang No.1 People's Hospital, Hubei University
of Medicine (approval no. 2023KY037), complied with the Health
Insurance Portability and Accountability Act, and followed the
guidelines of the Declaration of Helsinki.
Patient consent for publication
Written informed consent was provided by the patient
for publication of data and images.
Competing interests
The authors have no competing interests to
declare.
References
|
1
|
Kamisawa T, Zen Y, Pillai S and Stone JH:
IgG4-related disease. Lancet. 385:1460–1471. 2015.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Wallace ZS, Naden RP, Chari S, Choi H,
Della-Torre E, Dicaire JF, Hart PA, Inoue D, Kawano M, Khosroshahi
A, et al: The 2019 American college of rheumatology/european league
against rheumatism classification criteria for IgG4-related
disease. Ann Rheum Dis. 79:77–87. 2020.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Kamisawa T, Funata N, Hayashi Y, Eishi Y,
Koike M, Tsuruta K, Okamoto A, Egawa N and Nakajima H: A new
clinicopathological entity of IgG4-related autoimmune disease. J
Gastroenterol. 38:982–984. 2003.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Okazaki K, Uchida K, Koyabu M, Miyoshi H,
Ikeura T and Takaoka M: IgG4 cholangiopathy: Current concept,
diagnosis, and pathogenesis. J Hepatol. 61:690–695. 2014.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Masamune A, Kikuta K, Hamada S, Tsuji I,
Takeyama Y, Shimosegawa T and Okazaki K: Collaborators. Nationwide
epidemiological survey of autoimmune pancreatitis in Japan in 2016.
J Gastroenterol. 55:462–470. 2020.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Lanzillotta M, Mancuso G and Della-Torre
E: Advances in the diagnosis and management of IgG4 related
disease. BMJ. 369(m1067)2020.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Pan YY, Zhou SC, Wang YJ, Zhu TT, Peng D
and Guan HX: IgG4-related disease: A retrospective Chinese study of
features and treatment response of 98 patients including 4 rare
cases. Curr Med Sci. 41:390–397. 2021.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Ebbo M, Daniel L, Pavic M, Sève P, Hamidou
M, Andres E, Burtey S, Chiche L, Serratrice J, Longy-Boursier M, et
al: IgG4-related systemic disease: Features and treatment response
in a French cohort: Results of a multicenter registry. Medicine
(Baltimore). 91:49–56. 2012.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Inoue D, Yoshida K, Yoneda N, Ozaki K,
Matsubara T, Nagai K, Okumura K, Toshima F, Toyama J, Minami T, et
al: IgG4-related disease: Dataset of 235 consecutive patients.
Medicine (Baltimore). 94(e680)2015.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Yamada K, Yamamoto M, Saeki T, Mizushima
I, Matsui S, Fujisawa Y, Hara S, Takahashi H, Nomura H, Kawa S and
Kawano M: New clues to the nature of immunoglobulin G4-related
disease: A retrospective Japanese multicenter study of baseline
clinical features of 334 cases. Arthritis Res Ther.
19(262)2017.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Liu Y, Zhu L, Wang Z, Zeng Q, Yang F, Gao
J, Wang Z, Wang K, Ren L, Zhang Y, et al: Clinical features of
IgG4-related retroperitoneal fibrosis among 407 patients with
IgG4-related disease: A retrospective study. Rheumatology (Oxford).
60:767–772. 2021.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Moriarty MA, Dahmoush L and Nepple KG:
IgG4 related disease of the ureter (inflammatory pseudotumor). J
Urol. 191:1126–1127. 2014.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Marando A, D'Ambrosio G, Catanzaro F, La
Rosa S and Sessa F: IgG4-related disease of the ureter: Report of
two cases and review of the literature. Virchows Arch. 462:673–678.
2013.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Fernández-Codina A, Pinilla B,
Pinal-Fernández I, López C, Fraile-Rodríguez G, Fonseca-Aizpuru E,
Carballo I, Brito-Zerón P, Feijóo-Massó C, López-Dupla M, et al:
Treatment and outcomes in patients with IgG4-related disease using
the IgG4 responder index. Joint Bone Spine. 85:721–726.
2018.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Dai T and He YQ: CT and MRI features of
multi-organ involvement in IgG4-related disease. Diagn Interv
Imaging. 104:261–262. 2023.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Vaglio A, Catanoso MG, Spaggiari L,
Magnani L, Pipitone N, Macchioni P, Pulsatelli L, Nicastro M,
Becchi G, Corradi D, et al: Interleukin-6 as an inflammatory
mediator and target of therapy in chronic periaortitis. Arthritis
Rheum. 65:2469–2475. 2013.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Adding Ref, Arora K, Rivera M, Ting DT and
Deshpande V: The histological diagnosis of IgG4-related disease on
small biopsies: challenges and pitfalls. Histopathology.
74:688–698. 2019.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Lecler A and Sene T: MRI and
ultrasonography are useful tools for a non-invasive diagnosis of
IgG4-related disease. Ann Rheum Dis. 81(e51)2022.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Raglianti V, Rossi GM and Vaglio A:
Idiopathic retroperitoneal fibrosis: An update for nephrologists.
Nephrol Dial Transplant. 36:1773–1781. 2021.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Bakir B, Yilmaz F, Turkay R, Ozel S,
Bilgiç B, Velioglu A, Saka B and Salmaslioglu A: Role of
diffusion-weighted MR imaging in the differentiation of benign
retroperitoneal fibrosis from malignant neoplasm: Preliminary
study. Radiology. 272:438–445. 2014.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Abe H, Morikawa T, Araki A, Shima T,
Nakatsu H, Fukayama M and Suzuki Y: IgG4-related periureteral
fibrosis presenting as a unilateral ureteral mass. Pathol Res
Pract. 207:712–714. 2011.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Kawano M, Saeki T and Nakashima H:
IgG4-related kidney disease and retroperitoneal fibrosis: An
update. Mod Rheumatol. 29:231–239. 2019.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Lei WH, Xin J, Shao CX, Mao MF, Zhu CY, Wu
CF and Jin L: IgG4-related kidney disease mimicking malignant
ureter tumor: Case report and literature review. Medicine
(Baltimore). 95(e2550)2016.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Improta L, Tzanis D, Bouhadiba T,
Abdelhafidh K and Bonvalot S: Overview of primary adult
retroperitoneal tumours. Eur J Surg Oncol. 46:1573–1579.
2020.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Katz G and Stone JH: Clinical perspectives
on IgG4-related disease and its classification. Annu Rev Med.
73:545–562. 2022.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Carruthers MN, Topazian MD, Khosroshahi A,
Witzig TE, Wallace ZS, Hart PA, Deshpande V, Smyrk TC, Chari S and
Stone JH: Rituximab for IgG4-related disease: A prospective,
open-label trial. Ann Rheum Dis. 74:1171–1177. 2015.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Miki M, Fujimori N, Oono T, Kawabe K, Ohno
A, Matsumoto K, Teramatsu K, Tachibana Y and Ogawa Y: Relapse
patterns and predictors of IgG4-related diseases involved with
autoimmune pancreatitis: A single-center retrospective study of 115
patients. J Dig Dis. 20:152–158. 2019.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Liu Y, Zeng Q, Zhu L, Gao J, Wang Z, Wang
Z, Yang F, Wang K, Chen D, Xia C, et al: Relapse predictors and
serologically unstable condition of IgG4-related disease: A large
Chinese cohort. Rheumatology (Oxford). 59:2115–2123.
2020.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Peng Y, Li JQ, Zhang PP, Zhang X, Peng LY,
Chen H, Zhou JX, Zhang SZ, Yang HX, Liu JJ, et al: Clinical
outcomes and predictive relapse factors of IgG4-related disease
following treatment: A long-term cohort study. J Intern Med.
286:542–552. 2019.PubMed/NCBI View Article : Google Scholar
|