Introduction
Chemical pneumonitis is a lung injury caused by the
inhalation of noxious liquids or fumes. The most common causes are
microaspiration of gastrointestinal contents, drowning and
inhalation of chemical substances such as acid or gasoline. It is
an inflammatory reaction to inhaled noninfectious substances that
can cause acute pulmonary edema, a life-threatening acute
respiratory distress syndrome (ARDS) (1). ARDS occurs due to local corrosion,
toxic absorption, or allergies. Acid fumes, drowning and aspiration
are the leading causes of chemical pneumonitis (2-4).
However, as chemical pneumonitis has only occasionally been
reported owing to its accidental occurrence (5), it is frequently misdiagnosed and
poorly treated.
Currently, no uniform standards for treating
chemical pneumonitis are available and treatment typically involves
the use of glucocorticoids, antibiotics and mechanical ventilation
programs (6). Sivelestat sodium, a
neutrophil elastase inhibitor, has been identified as a novel drug
for ARDS treatment (7).
The present case report aimed to describe three
classic cases of chemical pneumonitis induced by different
pathological factors that were successfully treated with sivelestat
sodium in the early stages of disease progression, thus providing
valuable experience in treating ARDS caused by chemical
pneumonitis.
Case report
Case 1
A 67-year-old man accidentally inhaled acid fumes
for 1 min before leaving the scene. The patient experienced mild
dizziness without any other symptoms one afternoon in April 2021.
During approximately 6 h, the patient developed chest tightness and
dyspnea. The next day, the patient presented to the Emergency
Department of Wuxue People's Hospital (Wuxue, China) complaining of
dyspnea after cleaning metal appliances using a nitric-hydrofluoric
acid mixture without any protective tools. The patient reported no
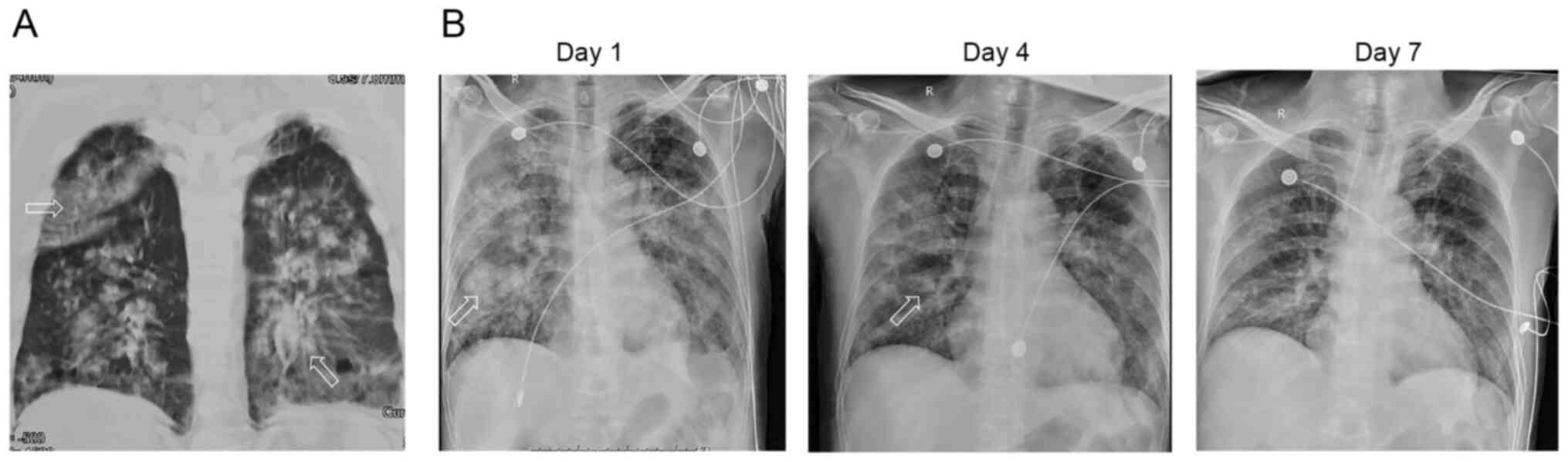
history of fever or hemoptysis. A chest CT scan showed bilateral
diffuse exudative shadows suggestive of pulmonary edema (Fig. 1A). However, the medical
capabilities of the hospital were limited and the patient was
immediately transferred to the intensive care unit (ICU) of Tongji
Hospital (Wuhan, China) for subsequent treatment. The patient
experienced tachypnea with the following clinical manifestations:
Respiratory rate (RR), 32 breaths/min; body temperature, 36.1˚C;
pulse, 105/min; blood pressure (BP), 148/63 mmHg; percutaneous
oxygen saturation (SpO2), 90% with consciousness; and
inspired oxygen [PaO2(P)/FiO2(F)] ratio, 126.
The patient was given oxygen through a facial mask. Dry rales were
heard in both lungs. No neck rigidity, arrhythmia or bellyaches
were observed. The results of laboratory examinations were as
follows: White blood cell (WBC) count, 16.88x109/l;
albumin, 25.6 g/l; creatine kinase, 356 U/l; myoglobin, 349.9
ng/ml; calcium, 1.86 mmol/l; phosphorus, 0.66 mmol/l; urea, 10.30
mmol/l; glucose, 11.18 mmol/l; and IL-6, 28.96 pg/ml. Arterial
blood gas (ABG) test results showed pH=7.421; oxygen pressure
(PaO2), 67 mmHg; carbon dioxide (PaCO2), 35.7
mmHg; arterial oxygen saturations (SaO2), 93%; and P/F,
230 (Table I).
 | Table ILaboratory data of three cases. |
Table I
Laboratory data of three cases.
| | Case 1 | Case 2 | Case 3 | |
|---|
| Characteristics | Before | After | Before | After | Before | After | Reference range |
|---|
| Age, years | 67 | 67 | 60 | 60 | 33 | 33 | - |
| Sex | Male | | Female | | Male | | |
| Blood pressure,
mmHg | 148/63 | 102/60 | 130/80 | 108/62 | 132/65 | 122/61 | - |
| Respiratory rate,
breaths/min | 32 | 21 | 26 | 19 | 26 | 22 | - |
| Body temperature,
˚C | 36.1 | 36.7 | 36.6 | 36.2 | 36.8 | 36.8 | - |
| Hematological
test | | | | | | | |
|
White blood
cells, x109/l | 16.88 | 6.57 | 11.67 | 11.71 | 6.46 | 6.46 | 3.5-9.5 |
|
Neutrophils,
% | 95.7 | 73.5 | 91.8 | 89.8 | 66.5 | 62.6 | 40-75 |
|
Lymphocytes,
% | 2.3 | 16.9 | 3.2 | 3.6 | 23.1 | 25.4 | 20-50 |
|
Monocytes,
% | 2 | 7.3 | 4.9 | 6.6 | 7.9 | 8 | 3-10 |
| Red blood cells,
x1012/l | 3.73 | 3.8 | 3.92 | 3.45 | 5.24 | 5.31 | 4.3-5.8 |
| Hemoglobin g/l | 125 | 127 | 124 | 108 | 161 | 159 | 130-175 |
|
Platelet
count, x109/l | 138 | 132 | 169 | 186 | 215 | 235 | 125-350 |
|
Prothrombin
time, sec | 14.7 | 12.9 | 14.2 | 12.7 | 12.7 | 13 | 9.4-12.5 |
|
Activated
partial thromboplastin time, % | 82 | 107 | 84 | 111 | 113 | 102 | 80-130 |
|
D-dimer,
ug/ml | 5.42 | 1.53 | 0.92 | 0.72 | 0.22 | 0.27 | <0.5 |
|
Total
protein, g/l | 57 | 52.8 | - | 63.5 | 60.2 | - | 64-83 |
|
White
albumin, g/l | 25.6 | 30.1 | 34 | 40.6 | 38.3 | - | 35-52 |
|
Total
bilirubin, umol/l | 12 | 7.8 | - | 14.6 | 7.8 | - | <26 |
|
Alanine
transaminase, U/l | 9 | 30 | 14 | 45 | 39 | 97 | <41 |
|
Aspartate
transaminase, U/l | 20 | 26 | 21 | 25 | 24 | 42 | <40 |
|
Urea,
mmol/l | 10.3 | 4.5 | 6.1 | 5.9 | 3.4 | 4.9 | 3.1-8 |
|
Creatinine,
umol/l | 80 | 73 | 55 | 58 | 70 | 75 | 59-104 |
|
Sodium,
mmol/l | 137.7 | 140.1 | 135.3 | 137.4 | 140.1 | 139.4 | 136-145 |
|
Potassium,
mmol/l | 3.92 | 4.56 | 4.33 | 4.02 | 4.41 | 4.46 | 3.5-5.1 |
|
Calcium,
mmol/l | 1.86 | 2.14 | 2 | 2.23 | 2.23 | 2.29 | 2.15-2.5 |
|
Procalcitonin,
ng/ml | 0.1 | 0.05 | 20.3 | 2 | 0.06 | 0.06 | <0.5 |
|
N-terminal
pro-B-type natriuretic peptide, pg/ml | 413 | 109 | 890 | - | 607 | <10 | <89.3 |
| Arterial blood
gas | | | | | | | |
|
Ph | 7.421 | 7.62 | 7.359 | 7.422 | 7.335 | 7.435 | 7.35-7.45 |
|
Pressure of
oxygen, mmHg | 67 | 283 | 60 | 90 | 59 | 157 | 80-105 |
|
Carbon
dioxide, mmHg | 35.7 | 22.6 | 33.5 | 44.8 | 50.8 | 30.7 | 35-45 |
|
Arterial
oxygen saturations, % | 93 | 100 | 90 | 97 | 93 | 100 | 95-98 |
Based on the examination data, the patient was
diagnosed with chemical pneumonitis, pulmonary infection and ARDS
according to the 2013 Berlin Definition (8). As the patient developed respiratory
failure, nasal high-flow oxygen (oxygen flow 55 l/min; oxygen
concentration, 60%) was given 4 h later. A new ABG test was
performed and the results were as follows: pH, 7.506;
PaO2, 138 mm Hg; PaCO2, 31.2 mmHg; and
SaO2, 99%. The doctors decided to administer 40 mg of
intravenous methylprednisolone and broad-spectrum antibiotics
(biapenem and levofloxacin), as referred to in the instructions of
the acid cleaning agent, which main components were nitric acid,
hydrofluoric acid and surfactants (detailed proportions and
concentrations were not described). For ARDS, due to the patient's
current nitric acid/hydrofluoric acid inhalation, the drug
recommendation was unclear. The patient was treated for 7 days with
0.3 g/day intravenous sivelestat sodium according to the drug
indications. The patient presented with severe exudation in both
lungs (Fig. 1A) and mild ARDS
(nasal high-flow oxygen, P/F 230) without multiple organ
dysfunction and met the following criteria for the use of
sivelestat sodium: Occurred systemic inflammatory response syndrome
(elevated white blood cells and rapid respiratory rate); acute lung
injury (P/F >300 mmHg, double lung infiltration shadow on
X-ray); and no multiple organ damage of four or more organs. The
patient did not have underlying chronic obstructive pulmonary
disease (COPD) and other diseases, and high-flow oxygen merely
served as a means of respiratory support, rather than as a
therapeutic measure. The patients lacked typical infection-related
symptoms and was less responsive to antibiotic treatment. At 1 week
post-admission to the hospital, the patient's oxygenation had
improved and ABG results were pH, 7.662; PaO2, 283 mmHg;
PaCO2, 22.6 mmHg; SaO2, 100%; and P/F, 514.
Nasal high-flow oxygen was replaced with a nasal catheter.
Methylprednisolone and sivelestat sodium were simultaneously
discontinued. Radiography revealed significant improvement, as
shown in Fig. 1B. The patient was
observed in the respiratory department and discharged at 2 weeks
post-admission. After 1 month, chest CT and pulmonary function test
results were normal.
Case 2
A 60-year-old woman was brought to the emergency
department of Tongji Hospital (Wuhan, China) in January 2022 after
nearly drowning in a pool. Witnesses reported that she had been
underwater for ~10 min. After vomiting a lot of sewage, the patient
gradually recovered and developed dyspnea and limb weakness over
the next 3 h. Upon arrival at the emergency department, the patient
presented SpO2, 88%; P/F, 100; BP, 130/80 mmHg; pulse
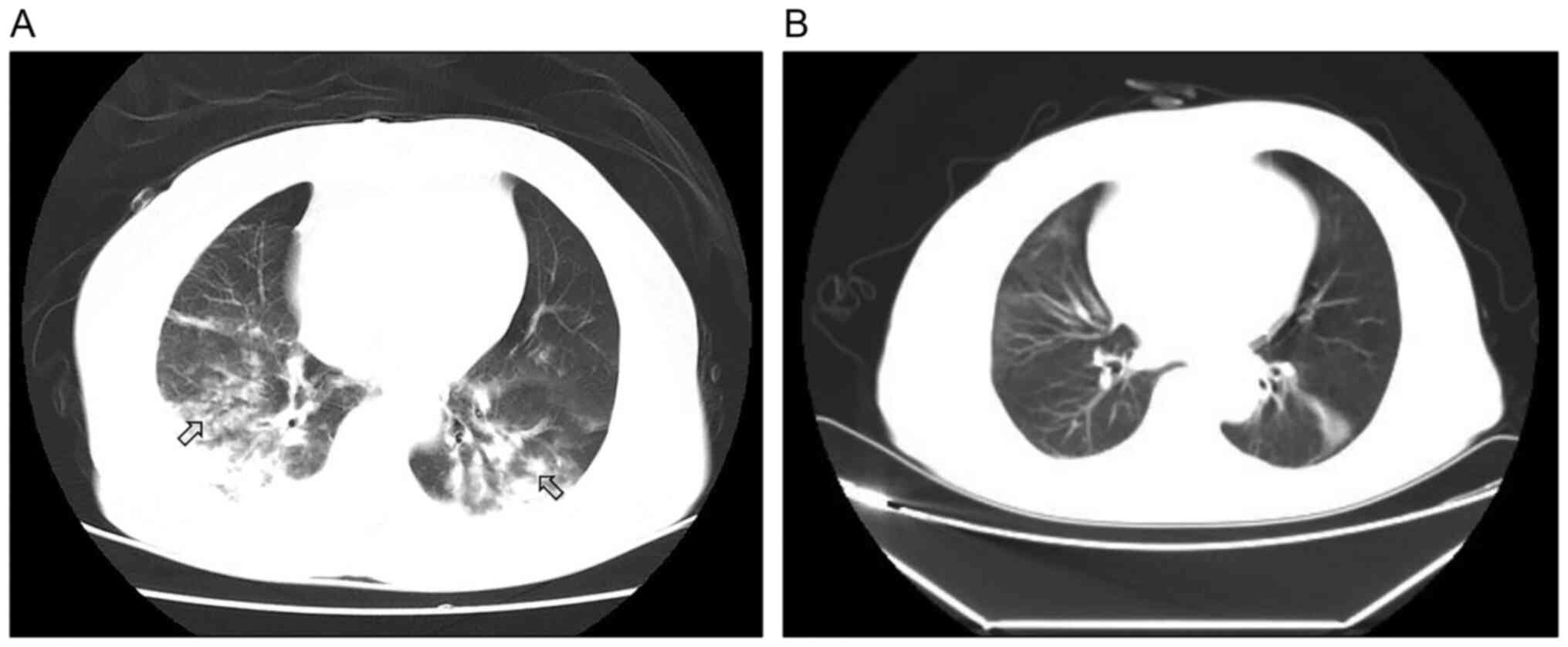
98/min; and RR, 26 breaths/min, without fever or rales. Chest CT
revealed bilateral alveolar opacity (Fig. 2A).
The patient was administered nasal high-flow oxygen
(oxygen flow 60 l/min; oxygen concentration, 60%) when admitted to
the ICU. The results of laboratory examinations were as follows:
WBC count, 11.67x109/l; NT-proBNP, 890 pg/ml; and
procalcitonin, 20.30 ng/ml. ABG test results were pH, 7.359;
PaO2, 60 mmHg; PaCO2, 33.5 mmHg;
SaO2, 90%; and P/F, 284. Considering the clinical
manifestations of dyspnea and the experimental results of the
pulmonary infection, the patient was diagnosed with chemical
pneumonitis, pulmonary infection and ARDS according to the 2013
Berlin Definition (8).
Based on the successful treatment protocol presented
in case 1, the patient was prescribed for 7 days: 40 mg/day
methylprednisolone; 0.1 g sivelestat sodium three times a day using
an intravenous pump under mild ARDS diagnosis (nasal high-flow
oxygen, P/F284) performed within 24 h, according to the
aforementioned drug indications, with 0.3 g biapenem every 8 h and
0.6 g levofloxacin. The patient did not have underlying COPD or
other diseases, and high-flow oxygen was solely used as a means of
respiratory support, providing no therapeutic role. Following 7
days of treatment, the patient showed significant clinical and
radiological improvement, including ABG test results as pH, 7.422;
PaO2, 92 mmHg; PaCO2, 44.8 mmHg;
SaO2, 97%; and P/F, 284. Laboratory examination showed:
WBC count, 11.71x109/l; and PCT, 0.22 ng/ml. A chest CT
showed the resolution of most of the interstitial opacities
(Fig. 2B). Microbiological
analysis of the sputum and serum showed negative results. The nasal
high-flow oxygen was discontinued and the patient was discharged
after 3 days.
Case 3
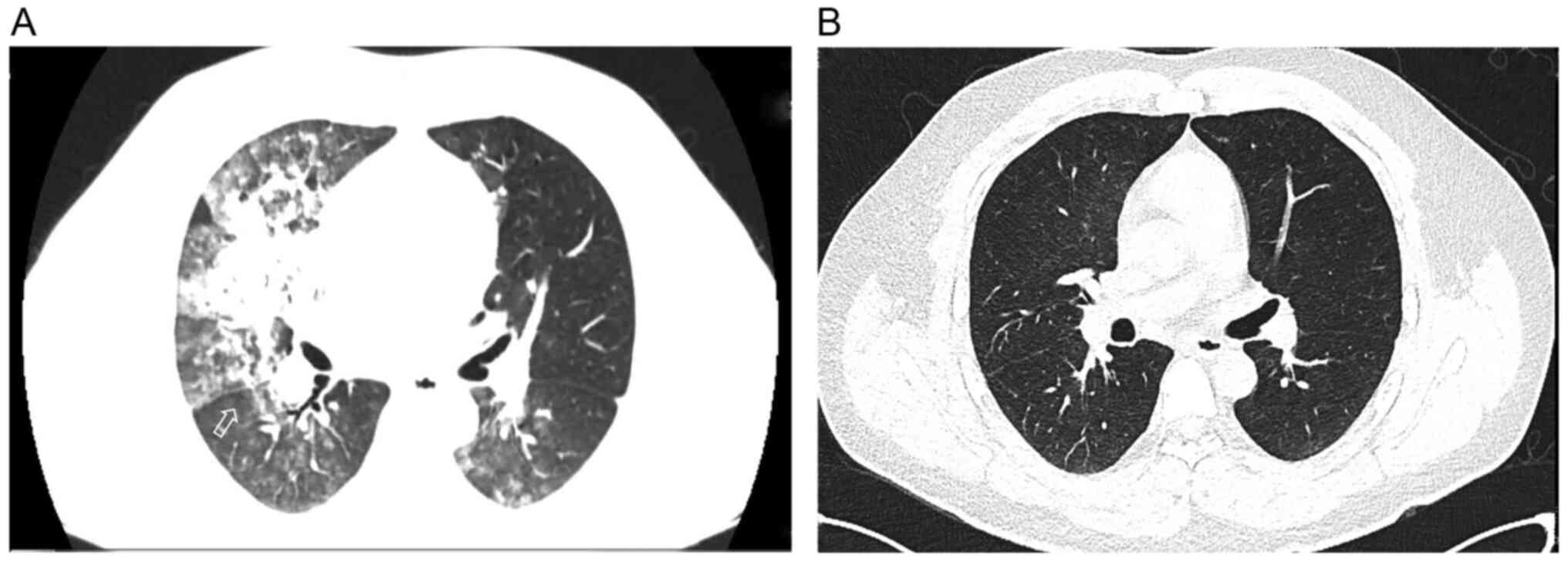
In January 2022, a 33-year-old man fell into a pool.
First-aid paramedics arrived soon after and transferred him to the
Tongji Hospital (Wuhan, China) for further treatment. The paramedic
crew observed that he had aspirated gastrointestinal contents and
provided suction care. Upon arrival at the emergency department,
the patient had fully revived but developed mild dyspnea with RR,
26 breaths/min and SpO2, 92%. ABG test results were as
follows: pH 7.335; PaO2, 59 mm Hg; PaCO2, 508
mmHg; SaO2, 93%; and P/F, 169. Although no remarkable
abnormalities were found upon physical examination, the patient was
admitted to the ICU owing to severe bilateral alveolar exudation
(Fig. 3A) and manifestations of
dyspnea. The patient was diagnosed with chemical pneumonitis,
pulmonary infection and ARDS according to the 2013 Berlin
Definition (8).
Considering the experience with the treatment
protocol presented in the two prior cases, nasal high-flow oxygen
(oxygen flow 40 l/min; oxygen concentration 50%), ceftazidime 2 g
every 12 h and sivelestat sodium (0.1 g three times/day using an
intravenous pump for 7 days) were administered to the patient under
significant pulmonary exudation early in the onset of the disease
(within 24 h) and mild ARDS diagnosis (although the P/F of the
patient was 314 mmHg under high-flow nasal cannula oxygen
administration, the P/F of the patient was only 169 mmHg under
nasal cannula oxygen administration), according to the
aforementioned drug indications. Methylprednisolone was not used
because of mild dyspnea and the presence of inhaled gastric
contents. The patient had no pre-existing COPD or other illnesses,
and high-flow oxygen was used solely for respiratory support and
not for any therapeutic role. After 5 days, the ABG results had
improved, showing PaO2, 157 mmHg; PaCO2, 30.7
mmHg; SaO2, 100%; and P/F, 314. Additionally, chest CT
showed a significant improvement (Fig.
3B). The symptoms improved in the course of 7 days and the
patient was subsequently discharged.
CT protocol
All images of the three patients were obtained with
one of three CT systems [Aquilion TSX-101A (Toshiba Medical
Systems; Canon Medical Systems Corporation), Optima 660 (GE
Healthcare) or Somatom force (Siemens Healthineers)] with patients
in the supine position. The imaging parameters were as follows:
Tube voltage, 120 kVp; automatic tube current modulation; tube
current, 30-70 mAs; pitch, 0.99-1.22 mm; matrix, 512x512; slice
thickness, 10 mm; and field of view, 350x350 mm. All images were
then reconstructed with a slice thickness of 0.625-1.250 mm with
the same increment.
Discussion
The present report presents three cases of ARDS
induced by acid inhalation, drowning and aspiration that resulted
in chemical pneumonitis and pulmonary infection. Treatment with
nasal high-flow oxygen and sivelestat sodium resulted in a good
prognosis. Various causes of chemical pneumonitis can lead to
overlapping clinical syndromes such as a cough, asthma and
expectoration (9). In the three
cases presented here, dyspnea and obvious exudative imaging changes
appeared several hours after the accidents. Clinical manifestations
are mainly determined by the nature of the substances and the
amounts inhaled (10). Thus, a
severity increase in the transition from transient hypoxemia to
severe ARDS was apparent. To guide treatment and predict outcomes,
it is helpful to clarify the specific clinical characteristics of
each patient.
Commercial nitric acid (concentration, 52-68%) is
generally mixed with a variety of nitrogen oxides (e.g., NO and
NO2). In high-concentration environments, the corrosive
effect of acids on the airways can lead to immediate death
(11,12). In other cases, the acidity and
corrosiveness of nitric and hydrofluoric acids may induce Acute
lung injury/ARDS due to inflammatory and allergic reactions
(13,14). In the physiological state, these
acids are oxidized to nitrate or hydrofluoride, which is excreted
by the kidneys (15). Hydrofluoric
acid can cause fatal hypocalcemia and hypomagnesemia by
specifically binding to calcium and magnesium ions (16). These symptoms were not observed in
Case 1, which may be due to the low concentration of hydrofluoric
acid in the mixture.
Although drowning can be prevented, it is the cause
of approximately 63,000 deaths/year in China (17). Because of the large amount of
liquid aspired, drowning patients initially develop
pathophysiological manifestations of chemical pneumonitis, such as
alterations in gas exchange, hypoxemia and decreased pulmonary
compliance (18). The symptoms
gradually worsen over time. Unlike acid inhalation, the clinical
manifestations depend highly on the sanitary conditions of the
drowning environment. A polluted environment is likely to induce
polymicrobial infections. In Case 2, laboratory examination showed
a significant increase in procalcitonin levels, which indicated a
serious infection. Broad-spectrum antibiotics were prescribed and
the patient eventually achieved good clinical outcomes.
In most cases, a microaspirated bacterial inoculum
is cleared by the airways. Based on animal experiments, a pH<2.4
and a large amount (>120 ml) of gastric contents are needed to
induce aspiration pneumonitis (4).
Therefore, the use of glucocorticoids to alleviate the symptoms of
aspiration pneumonitis remains controversial.
Inhalation of an infectious inoculum or secondary
dysbacteriosis may lead to aspiration pneumonia (19). Although aspiration pneumonia is
occasionally difficult to distinguish from aspiration pneumonitis,
the latter is a distinct clinical condition. Aspiration pneumonia
is a subset of bacterial pneumonia caused by inoculum aspiration.
Aspiration pneumonitis refers to a pathophysiological disease
characterized by ARDS. Aerobic and nosocomial bacteria (especially
enteric Gram-negative bacteria) that can be treated with empirical
antibiotics have been reported to be involved in the onset of
aspiration pneumonia (20,21). Moreover, mild antibiotic treatment
is appropriate to prevent secondary pneumonia caused by
multidrug-resistant (MDR) pathogens. In Case 3, owing to the lack
of signs of severe pneumonia, ceftazidime and sivelestat sodium
were prescribed instead of glucocorticoids. Finally, the patient
recovered within a short period.
The pathological progression of ARDS includes an
inflammatory response (<6 h), alveolar edema (6-48 h) and
pulmonary fibrosis (>48 h) (22). During the inflammatory response
phase, damaged capillary endothelial cells induce the recruitment
and activation of neutrophils, which can release a series of
inflammatory factors, such as leukotrienes, peroxides and elastase.
Elastase has the greatest hydrolytic effect on the alveolar
basement membrane and extracellular matrix, resulting in the
degradation of alveolar surfactants and, eventually, irreversible
pulmonary fibrosis (23).
Therefore, early intervention of inflammatory factors in the
alveolar edema stage would be the ‘time window’ for ARDS
treatment.
Glucocorticoids are widely used in the treatment of
chemical pneumonitis because of their inhibitory effects on
inflammatory responses (12,24).
However, the use and dosage of glucocorticoids remain
controversial. In the treatment guidelines for ARDS,
glucocorticoids are not routinely recommended. To the best of our
knowledge, only a few studies reported their ability to improve
pulmonary compliance over a short-term course (25,26).
Long-term use or an overdose of glucocorticoids can lead to airway
necrosis and secondary MDR infections. The dose of glucocorticoids
prescribed for ARDS induced by strong acid inhalation has become
more conservative (27), aiming to
balance therapeutic effects and the occurrence of complications.
Clinicians are trying to use novel drugs to treat chemical
pneumonitis, such as pirfenidone and acetylcysteine, and some
studies reported positive therapeutic effects (28,29).
Sivelestat sodium is a competitive inhibitor of
neutrophil elastase and was proven to be effective in treating
acute lung injury. Sivelestat sodium can reduce the serum levels of
inflammatory factors such as neutrophil elastase, IL-8, NO, and
NO2. A study involving 110 patients with acute lung
injury reported that sivelestat sodium markedly reduced mortality
(30) in critically ill patients
(31). Notably, sivelestat sodium
inhibits neutrophil migration and the release of inflammatory
factors, but does not affect other pathophysiological mechanisms of
ARDS, such as chymotrypsin or plasminase (32). In the study, we hypothesise that
sivelestat sodium is not applicable in patients with moderate or
severe ARDS for whom a protective ventilation strategy is more
effective. Therefore, we speculated that sivelestat sodium would be
suitable for treating mild ARDS induced by chemical pneumonitis in
its early stages (24-36 h). In the present study, all patients were
treated with 4.8 mg/kg/day intravenous sivelestat sodium and
experienced an effective relief of symptoms within the 7-day
treatment period.
The current study had some limitations. Nasal
high-flow oxygen, methylprednisolone and antibiotics were
administered to all patients, making it difficult to determine
which approach had the greatest impact on recovery. Nonetheless, in
the present study, treatment with sivelestat sodium significantly
contributed to the recovery of all patients. The shared
characteristics among the patients were early disease onset (within
24 h), mild ARDS and the absence of underlying conditions such as
COPD. Consequently, oxygen was administered only for respiratory
support and not for therapeutic purposes. Antibiotics were
prescribed solely to Cases 2 and 3 as preventive measures against
pulmonary infections resulting from exposure to unclean water.
However, the anti-infective properties of these antibiotics cannot
be compared to those of sivelestat sodium. In Case 1,
methylprednisolone played an effect similar role in the emergency
relief of acute exacerbation symptoms at a minimal dose. In Case 2,
methylprednisolone was administered owing to breathing
difficulties, leading to an improved clinical outcome. In Case 3,
anti-infective therapy with ceftazidime was administered due to
unclean water inhalation. This treatment is weaker than silvelestat
sodium in the rehabilitation of patients, which but is only a
secondary effect to its anti-infective role. Nonetheless, the
therapeutic application of sivelestat sodium provides valuable
information for the clinical treatment of patients with a similar
presentation. Additionally, clinical studies have shown that
hormone use is controversial (33); therefore, silverestat sodium may be
an effective combination or complementary therapy. The present
authors expect that the successful strategies reported in the
present study will stimulate further research to improve the
understanding of the mechanisms underlying this treatment approach,
thereby enabling patients with similar presentations to benefit
from it.
Currently, few complications associated with
sivelestat sodium have been reported. The drug indications only
mention allergic reactions. The present study did not observe any
abnormal liver function. The present cases indicated that
sivelestat sodium is an effective supplement for treating chemical
pneumonitis. However, the efficacy of sivelestat sodium in the
treatment of ARDS with multiple organ dysfunction or chronic
respiratory diseases remains unclear; therefore, future large-scale
clinical studies are needed.
Acknowledgements
Not applicable.
Funding
Funding: This work was supported by the Scientific Research
Project of Hubei Provincial Health and Family Planning Commission
(grant no. WJ2019M123).
Availability of data and materials
All data generated or analyzed during this study are
included in this published article.
Authors' contributions
LJ and WZ designed the study, searched the
literature and wrote the first draft of the manuscript. XP, DL, YQ
and YS collected and interpreted the relevant data. WZ and XP
supervised the literature review and revised the manuscript for
important intellectual content. LJ and WZ confirm the authenticity
of all the raw data. All the authors read and approved the final
version of the manuscript.
Ethics approval and consent to
participate
This study was approved by the Institutional Review
Board of Tongji Hospital and the requirement for informed consent
was waived (approval no. TJ-IRB20220436).
Patient consent for publication
Consent for publication was signed by all
patients.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Matthay MA, Zemans RL, Zimmerman GA, Arabi
YM, Beitler JR, Mercat A, Herridge M, Randolph AG and Calfee CS:
Acute respiratory distress syndrome. Nat Rev Dis Primers.
5(18)2019.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Jang JH, Hwang SY, Chung CR, Suh GY and Ko
RE: Acute lung injury following occupational exposure to nitric
acid. Acute Crit Care. 36:395–396. 2021.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Cerland L, Mégarbane B, Kallel H, Brouste
Y, Mehdaoui H and Resiere D: Incidence and consequences of
near-drowning-related pneumonia-a descriptive series from
Martinique, French West Indies. Int J Environ Res Public Health.
14(1402)2017.PubMed/NCBI View Article : Google Scholar
|
|
4
|
DiBardino DM and Wunderink RG: Aspiration
pneumonia: A review of modern trends. J Crit Care. 30:40–48.
2015.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Jegan NK, Vithyatharan KS, Sakunthala SR
and Rajasekaran D: Chemical pneumonitis. J Assoc Physicians India.
59(314)2011.PubMed/NCBI
|
|
6
|
Neill S and Dean N: Aspiration pneumonia
and pneumonitis: A spectrum of infectious/noninfectious diseases
affecting the lung. Curr Opin Infect Dis. 32:152–157.
2019.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Miyoshi S, Hamada H, Ito R, Katayama H,
Irifune K, Suwaki T, Nakanishi N, Kanematsu T, Dote K, Aibiki M, et
al: Usefulness of a selective neutrophil elastase inhibitor,
sivelestat, in acute lung injury patients with sepsis. Drug Des
Devel Ther. 7:305–316. 2013.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Ferguson ND, Fan E, Camporota L, Antonelli
M, Anzueto A, Beale R, Brochard L, Brower R, Esteban A, Gattinoni
L, et al: The Berlin definition of ARDS: An expanded rationale,
justification, and supplementary material. Intensive Care Med.
38:1573–1582. 2012.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Marik PE: Aspiration pneumonitis and
aspiration pneumonia. N Engl J Med. 344:665–671. 2001.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Mandell LA and Niederman MS: Aspiration
pneumonia. N Engl J Med. 380:651–663. 2019.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Murphy CM, Akbarnia H and Rose SR: Fatal
pulmonary edema after acute occupational exposure to nitric acid. J
Emerg Med. 39:39–43. 2010.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Kao SL, Yap ES, Khoo SM, Lim TK,
Mukhopadhyay A and Teo ST: Acute lung injury after inhalation of
nitric acid. Eur J Emerg Med. 15:348–350. 2008.PubMed/NCBI View Article : Google Scholar
|
|
13
|
de Lange DW, Sikma MA and Meulenbelt J:
Extracorporeal membrane oxygenation in the treatment of poisoned
patients. Clin Toxicol (Phila). 51:385–393. 2013.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Purva SB and More KD: Acute lung injury
after exposure to fumes of pickling paste in a fabrication worker.
Indian J Occup Environ Med. 22:54–56. 2018.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Jayalakshmi TK, Shah S, Lobo I, Uppe A and
Mehta A: Acute lung injury following exposure to nitric acid. Lung
India. 26:149–151. 2009.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Sanz-Gallén P, Nogué S, Munné P and
Faraldo A: Hypocalcaemia and hypomagnesaemia due to hydrofluoric
acid. Occup Med (Lond). 51:294–295. 2001.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Wang L, Cheng X, Yin P, Cheng P, Liu Y,
Schwebel DC, Liu J, Qi J, Zhou M and Hu G: Unintentional drowning
mortality in China, 2006-2013. Inj Prev. 25:47–51. 2019.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Estella AA and Bello Fontaiña LP: Sea
drowning: A case report and review of the literature. Monaldi Arch
Chest Dis. 75:135–137. 2011.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Sanivarapu RR and Gibson J: Aspiration
Pneumonia. In: StatPearls (Internet). Treasure Island (FL):
StatPearls Publishing, 2023.
|
|
20
|
Tokuyasu H, Harada T, Watanabe E, Okazaki
R, Touge H, Kawasaki Y and Shimizu E: Effectiveness of meropenem
for the treatment of aspiration pneumonia in elderly patients.
Intern Med. 48:129–135. 2009.PubMed/NCBI View Article : Google Scholar
|
|
21
|
El-Solh AA, Pietrantoni C, Bhat A,
Aquilina AT, Okada M, Grover V and Gifford N: Microbiology of
severe aspiration pneumonia in institutionalized elderly. Am J
Respir Crit Care Med. 167:1650–1654. 2003.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Yadav H, Thompson BT and Gajic O: Fifty
years of research in ARDS. Is acute respiratory distress syndrome a
preventable disease? Am J Respir Crit Care Med. 195:725–736.
2017.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Voynow JA and Shinbashi M: Neutrophil
elastase and chronic lung disease. Biomolecules.
11(1065)2021.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Britto J and Demling RH: Aspiration lung
injury. New Horiz. 1:435–439. 1993.PubMed/NCBI
|
|
25
|
Cho YJ, Moon JY, Shin ES, Kim JH, Jung H,
Park SY, Kim HC, Sim YS, Rhee CK, Lim J, et al: Clinical practice
guideline of acute respiratory distress syndrome. Tuberc Respir Dis
(Seoul). 79:214–233. 2016.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Steinberg KP, Hudson LD, Goodman RB, Hough
CL, Lanken PN, Hyzy R, Thompson BT and Ancukiewicz M: Efficacy and
safety of corticosteroids for persistent acute respiratory distress
syndrome. N Engl J Med. 354:1671–1684. 2006.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Bansal DP, Ambegaonkar R, Radhika P and
Sharma M: ARDS following inhalation of hydrochloric acid. J Assoc
Physicians India. 59:115–117. 2011.PubMed/NCBI
|
|
28
|
Seifirad S: Pirfenidone: A novel
hypothetical treatment for COVID-19. Med Hypotheses.
144(110005)2020.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Soltan-Sharifi MS, Mojtahedzadeh M, Najafi
A, Reza Khajavi M, Reza Rouini M, Moradi M, Mohammadirad A and
Abdollahi M: Improvement by N-acetylcysteine of acute respiratory
distress syndrome through increasing intracellular glutathione, and
extracellular thiol molecules and anti-oxidant power: Evidence for
underlying toxicological mechanisms. Hum Exp Toxicol. 26:697–703.
2007.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Aikawa N and Kawasaki Y: Clinical utility
of the neutrophil elastase inhibitor sivelestat for the treatment
of acute respiratory distress syndrome. Ther Clin Risk Manag.
10:621–629. 2014.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Li H, Zhou X, Tan H, Hu Y, Zhang L, Liu S,
Dai M, Li Y, Li Q, Mao Z, et al: Neutrophil extracellular traps
contribute to the pathogenesis of acid-aspiration-induced ALI/ARDS.
Oncotarget. 9:1772–1784. 2018.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Pu S, Wang D, Liu D, Zhao Y, Qi D, He J
and Zhou G: Effect of sivelestat sodium in patients with acute lung
injury or acute respiratory distress syndrome: A meta-analysis of
randomized controlled trials. BMC Pulm Med. 17(148)2017.PubMed/NCBI View Article : Google Scholar
|
|
33
|
Wiedemann HP and Tai DY: Adult respiratory
distress syndrome (ARDS): Current management, future directions.
Cleve Clin J Med. 64:365–372. 1997.PubMed/NCBI View Article : Google Scholar
|