Introduction
In recent years, with the aggravation of global
aging, the incidence of hip fractures in the elderly is increasing
year by year, and femoral neck fractures account for >50% of hip
fractures (1,2). Conservative treatment of femoral neck
fractures in the elderly has increased risk of complications and
high mortality, which seriously affects the quality of life of
patients. Although researchers all around the world have
investigated femoral neck fractures in the elderly, the best
surgical treatment is still a controversial topic in clinical
practice (3-5).
At present, the treatment of femoral neck fractures in the elderly
is mainly divided into two categories: Internal fixation and
artificial joint replacement (6-12).
Most of the severely displaced Garden III-IV femoral neck fractures
in the elderly are treated with hip replacement (6-8),
but for nondisplaced Garden I-II and less displaced Garden III
femoral neck fractures, internal fixation operation is still an
important treatment, especially for elderly patients with a variety
of medical diseases who cannot tolerate joint replacement (9,10).
Although there are numerous types of internal fixation devices for
internal fixation of femoral neck fractures, such as cannulated
screw, dynamic hip screw (DHS) and femoral neck system (FNS),
proximal femoral nail, and proximal femoral locking plate (11), cannulated screw internal fixation
remains the most important surgical method in the certain areas of
China, where economic development is limited. Three cannulated
screws with inverted triangular distribution have become the ‘gold
standard’ for cannulated screw treatment due to high biomechanical
stability (12). However, there
are drawbacks to this method, such as the inability to place the
screws due to anatomically slender femoral necks, or the
destruction of bone quality and blood supply, and longer operation
time caused by repeated needle insertion during surgery in order to
achieve three-point fixation of screws. Over the years, the First
Affiliated Hospital of Nanjing Medical University (Jiangsu Province
Hospital) (Nanjing, China), has used three cannulated screws with
parallel distribution to treat femoral neck fractures in the
elderly, and the clinical efficacy, as reported in the present
study, is remarkable. The aim of the present study was to
investigate the clinical efficacy of three cannulated screws with
parallel distribution compared with the ‘gold standard’ of
inverting three cannulated screws with triangular distribution in
the treatment of femoral neck fractures in the elderly.
Materials and methods
Clinical data
Retrospective analysis was performed on patients
with femoral neck fractures who visited the Orthopedic Arthropathy
ward and Trauma ward of the First Affiliated Hospital of Nanjing
Medical University (Jiangsu Provincial Hospital; Nanjing, China)
from October 2018 to March 2020, and a total of 106 patients,
including 38 male patients and 68 female patients with a mean age
of 73.9±7.1 years, met the inclusion and exclusion criteria for
this study. All patients were admitted to the Emergency Department
of First Affiliated Hospital of Nanjing Medical University (Jiangsu
Provincial Hospital) and were routinely included in the fast track
for hip fractures in the elderly, with preoperative waiting times
of <48 h. According to the distribution pattern of screws during
surgery, the patients were divided into group A (control group,
three cannulated screws with inverted triangular distribution) and
group B (experimental group, three cannulated screws with parallel
distribution). There were 51 patients in group A and 55 patients in
group B. The medical complications of the 106 patients were as
follows: 78 cases of cardiovascular diseases such as hypertension,
coronary heart disease, PCI stent implantation for myocardial
infarction, and mild to moderate heart failure; 63 cases of nervous
system disorders such as lacunar infarction, mild cerebral
infarction, and cerebral infarction sequelae; 48 cases of
respiratory diseases such as chronic bronchitis, emphysema, and
pulmonary heart disease; 56 cases of type 2 diabetes mellitus; 38
cases of digestive system diseases such as atrophic gastritis and
gastrointestinal ulcers; and 19 cases of tumors. An in-depth
inquiry into the medical history of the patients was performed,
patients underwent an X-ray and hip CT examination and signed the
operation consent form before surgery. There were no significant
differences in general demographic data [sex, age, injured side,
American Society of Anesthesiologists (ASA) grade, Garden type,
fracture site, cause of injury, and Pauwels type] between groups A
and B (P>0.05; Table I).
 | Table IComparison of baseline data between
the two groups of patients with femoral neck fractures. |
Table I
Comparison of baseline data between
the two groups of patients with femoral neck fractures.
| | Sex | Side | | ASA grade | Garden type | Classification of
fracture site | Causes of injury | Pauwels type |
|---|
| Group | No. of subjects | Male | Female | Left | Right | Age (± s, years) | II | III | IV | Grade I | Grade II | Grade III | Subcapital | Transcervical | Falls | Automobile
accident | I | II | III |
|---|
| Group A | 51 | 20 | 31 | 25 | 26 | 73.3±6.8 | 14 | 31 | 6 | 15 | 24 | 12 | 20 | 31 | 41 | 10 | 17 | 28 | 6 |
| Group B | 55 | 18 | 37 | 26 | 29 | 74.5±7.3 | 16 | 34 | 5 | 16 | 29 | 10 | 19 | 36 | 43 | 12 | 21 | 30 | 4 |
| T-value | | 0.4844 | | 0.0323 | | -0.8739 | 0.7431 | | | 0.5356 | | | 0.2482 | | 0.0786 | | 0.7401 | | |
| P-value | | 0.486 | | 0.857 | | 0.384 | 0.690 | | | 0.765 | | | 0.618 | | 0.779 | | 0.691 | | |
Inclusion and exclusion criteria
The inclusion criteria were as follows: i) Patients
diagnosed with unilateral subcapital or transcervical fresh femoral
neck fracture; ii) aged >65 years; iii) nondisplaced Garden I-II
or Garden III femoral neck fracture displaced within 5 mm; iv)
admitted to the Emergency Department within 24 h after injury; v)
underwent intraoperative closed reduction + three cannulated screws
with inverted triangular distribution or parallel distribution; and
vi) patients and their families were highly compliant and
cooperated with treatment and follow-up. The exclusion criteria
were as follows: i) Patients also diagnosed with severe
cardiovascular and cerebrovascular diseases and other medical
conditions or mental illness; ASA grade IV or above; with severe
surgical contraindications, and unable to tolerate surgery; ii)
patients also diagnosed with ipsilateral hip joint infection,
tumors, rheumatic immune diseases, etc.; iii) patients with old,
open or pathological fractures; iv) patients who had undergone
previous ipsilateral hip operations; v) patients treated with other
methods of internal fixation such as with DHS or FNS; and vi)
patients and their families who did not cooperate with
follow-up.
Treatment methods
Skin traction immobilization of the affected limb
was applied and low molecular weight heparin anticoagulation was
administered after admission. Complete preoperative relevant
examinations were performed to regulate blood glucose and blood
pressure and fast-track anesthesiology consultation for hip
fracture was performed. Routine preoperative blood tests were
performed and intensive care unit (ICU) beds were prepared for
future use.
Surgery was completed within 48 h for patients in
both groups. According to the ASA grade and the pre-existing
diseases of the patients, different anesthesia methods such as
general anesthesia, unilateral spinal anesthesia + fascia iliaca
nerve block, fascia iliaca nerve block + local anesthesia were
adopted. The patient was placed in supine position with the
affected limb fixed on an orthopedic traction operating bed, and
after the fracture end was unlocked, longitudinal traction,
moderate adduction, and closed reduction with internal rotation
were performed. The fracture reduction was monitored under C-arm
fluoroscopy, with referral to the Garden reduction index. The bone
was fixed in the corresponding position when both anteroposterior
and lateral reductions were satisfactory. In order to reduce the
times of subsequent intraoperative fluoroscopy, a 2.0-mm Kirschner
wire (DePuy Synthes; Johnson & Johnson) was placed in front of
the hip joint after successful reduction, parallel to the femoral
neck and close to the femoral calcar, and after fluoroscopic
localization, the placement of the Kirschner wire was adjusted to
scribing for future use. In group A, the first guide wire
(anteroposterior parallel femoral neck and close to the femoral
calcar; lateral position pointing to the direction of the femoral
head along the longitudinal axis of the femoral neck and located in
the center of the femur) was placed first along the positioning
line before disinfection under fluoroscopic localization. The
second and third guide wires were placed anteroposteriorly and
posteriorly of the lateral femoral wall, respectively, with three
guide wires distributed in an inverted triangle, with wires of the
second and third guide placed as close as possible to the anterior
and posterior cortex of the femoral neck within a distance of 2-3
mm, making the cross-sectional area of the inverted triangle as
large as possible. In group B, the first guide wire was placed in
the same way, and then the second and third guide wires were placed
in parallel at the ½ and upper 1/3 of the femoral neck,
respectively. The second and third guide wires were parallel to the
first guide wire in the anteroposterior position and were centered
on the lateral femoral wall in the lateral position. A hole was
then opened with a drill bit (DePuy Synthes; Johnson &
Johnson), and the 7.3 mm diameter cannulated screws were placed,
with the end of the cannulated screws reaching 5 mm below the
subchondral bone of the femoral head to ensure that all threads
passed the fracture line, adding additional spacers for some
patients with severe osteoporosis. Three cannulated screws were
gradually compressed separately to avoid fracture displacement
during screw compression. Finally, fluoroscopy was performed again
to confirm good fracture reduction and acceptable screw position
and length. The hip was punctured aseptically to extract
hemarthrosis, the wound was irrigated and then sutured. Patients in
group A were operated on by senior directors including surgeons Dr
Fang Jiahu and Dr Qin Xiaodong of the Department of Trauma and
Orthopedics [the First Affiliated Hospital of Nanjing Medical
University (Jiangsu Province Hospital)] and patients in group B
were operated on by senior directors including surgeons Dr Liu
Feng, Dr Cui Weiding and Dr Wan Bin of the Department of Joint
Surgery [(the First Affiliated Hospital of Nanjing Medical
University (Jiangsu Province Hospital)]. The present study was
approved (approval no. 2019-SRFA-453) by the Ethics Committee of
the First Affiliated Hospital of Nanjing Medical University.
Informed consent was obtained from all patients or their families
for participation in the present study. Consent for publication was
also obtained from all the patients.
After surgery, the patients were treated with pain
relief, anti-infection and anticoagulation therapies. On the second
day after surgery, the patients could perform lower limb functional
exercises in a sitting position. Full weight-bearing of the
affected limb was avoided for three months, and gradual
weight-bearing to full weight-bearing was performed with the help
of a walking aid according to fracture healing during follow-up
examinations. Patients in groups A and B visited the First
Affiliated Hospital of Nanjing Medical University (Jiangsu Province
Hospital) for regular follow-up examinations at 1, 2, 3, 6 and 12
months after surgery. At these follow-ups, anteroposterior and
lateral hip radiographs (digital radiography equipment; Ysio Max
Smart Speed MAX Platform; Siemens Healthineers) were performed and
used to assess fracture healing, and a functional assessment of the
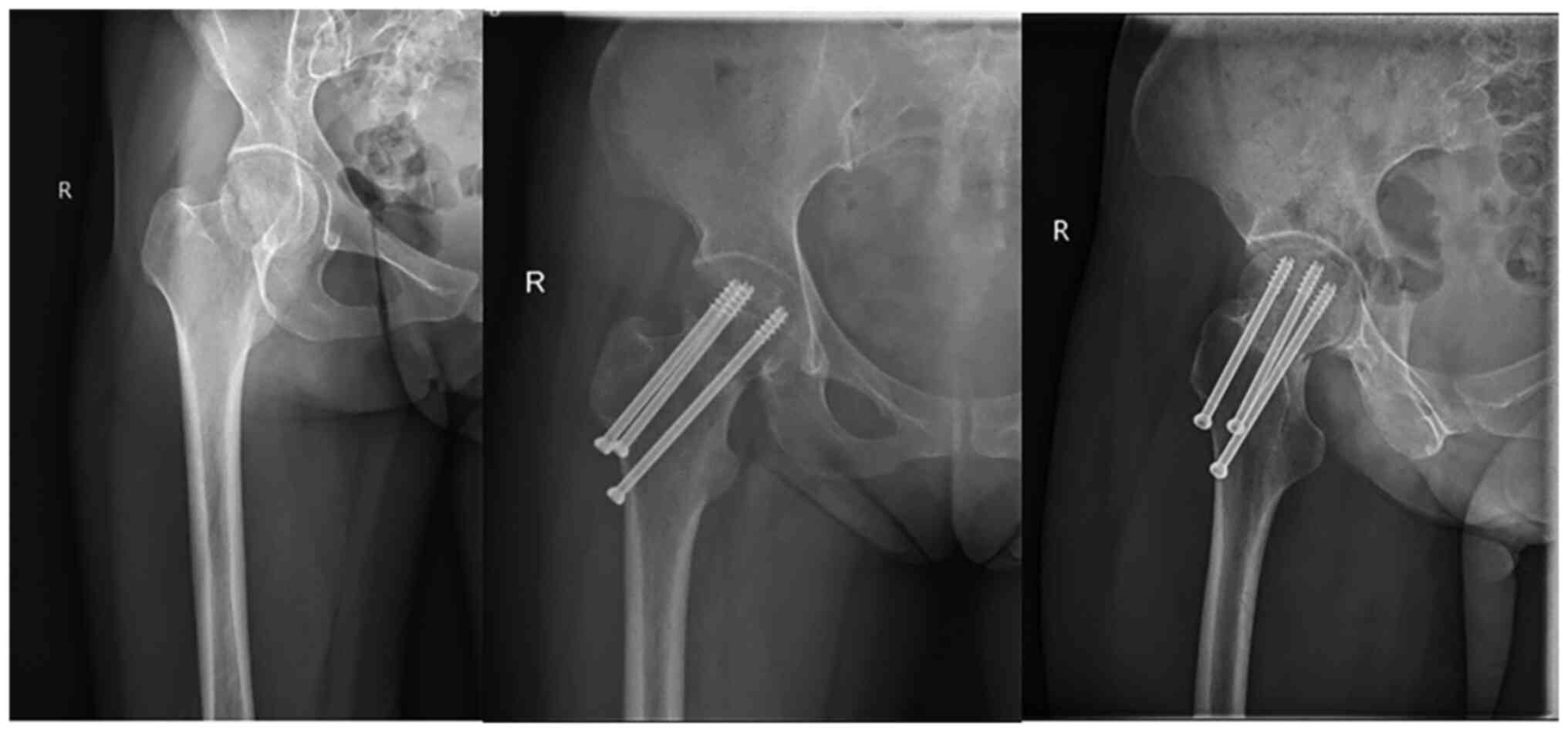
hip joint was performed. Typical cases in both groups are shown in
Figs. 1 and 2.
Clinical efficacy assessments
The general surgical conditions including the
anesthesia method, the preoperative waiting time, the operation
time, intraoperative bleeding, the number of times intraoperative
fluoroscopy was performed, the number of intraoperative guide wire
adjustments, the proportion of postoperative referrals to the ICU,
and complications (wound infection, hypostatic pneumonia, bed
sores, deep venous thrombosis, internal fixation failure, etc.)
were recorded in groups A and B.
For fracture reduction and healing, the Garden
alignment index (13) was used to
evaluate the reduction of the femoral neck fracture in groups A and
B. The fracture healing time, incidence of avascular necrosis of
the femoral head and incidence of fracture nonunion were recorded
according to the follow-up results.
For hip function assessment, the daily activity
function of the hip joint was recorded during follow-up in groups A
and B and the functional recovery scale (FRS) (14) for elderly patients with hip
fractures was used.
Statistical analysis
The statistical software Stata 15.0 (StataCorp LLC)
was used for analysis, and numerical variables were expressed as
mean ± SD. Independent sample t-tests were performed for two
groups of continuous numerical variables satisfying normal
distribution. FRS scores were compared between patients in the same
group Before injury and at the last follow-up after fracture
treatment. Paired t-tests were performed. Categorical
variables were analyzed using χ2 test or Fisher's exact
test at a test level of α=0.05. P<0.05 was considered to
indicate a statistically significant difference.
Results
Patients in both groups A and B were followed up for
12-25 months, with an average of 14.8 months, and there were no
cases of loss to follow-up. During follow-up, one patient in group
A succumbed to myocardial infarction 15 months after surgery.
The results revealed that there were no significant
differences with regard to anesthesia, preoperative waiting times,
and intraoperative bleeding between groups A and B (P>0.05;
Table II). However, when the
number of times of intraoperative fluoroscopy, the number of
intraoperative guide wire adjustments, the proportion of
postoperative referrals to the ICU, which were performed during
surgery, were compared, it was found that group B exhibited
significant advantages compared with group A, and the differences
were statistically significant (P<0.05; Table II).
 | Table IIComparison of general surgical
conditions between the two groups of patients with femoral neck
fractures. |
Table II
Comparison of general surgical
conditions between the two groups of patients with femoral neck
fractures.
| | Anesthesia | |
|---|
| Group | No. of
subjects | General
anesthesia | Spinal anesthesia +
nerve block | Nerve block + local
anesthesia | Preoperative
waiting time from injury to operation (h) | Operation time
(min) | Intraoperative
bleeding (ml) | Intraoperative
fluoroscopy (no. of times) | Intraoperative
guide wire adjustments (no. of times) | Postoperative
transfer to the ICU |
|---|
| Group A | 51 | 42 | 6 | 3 | 31.7±5.9 | 46.7±9.1 | 35.6±8.3 | 45.1±6.5 | 28.2±7.6 | 7 |
| Group B | 55 | 44 | 7 | 4 | 30.6±7.5 | 28.8±6.9 | 34.8±7.5 | 28.3±5.8 | 15.5±4.3 | 1 |
| T-value | | 0.1155 | | | 0.8348 | 11.4624 | 0.5213 | 14.0603 | 10.6870 | Fisher |
| P-value | | 0.944 | | | 0.406 | <0.001 | 0.603 | <0.001 | <0.001 | 0.027 |
In addition, there were no significant differences,
as regards fracture reduction quality, rate of fracture healing,
incidence of femoral neck fracture nonunion, incidence of avascular
necrosis of the femoral head and other complications between groups
A and B (P>0.05; Table III).
In group A, there were 2 cases of lower extremity deep venous
thrombosis and 2 cases of superficial wound infection, while in
group B, there were 1 case of lower extremity deep venous
thrombosis, 1 case of mild lung infection, and 1 case of
superficial wound infection. In both groups, the femoral neck was
shortened in all patients after surgery, ranging from 1 to 4 mm. No
other complications such as screw cutting and bed sores occurred in
either group (data not shown).
 | Table IIIComparison of fracture reduction,
fracture healing and postoperative complications between the two
groups of patients with femoral neck fractures. |
Table III
Comparison of fracture reduction,
fracture healing and postoperative complications between the two
groups of patients with femoral neck fractures.
| | Garden alignment
index | Fracture
healing | |
|---|
| Group | No. of
subjects | I | II | III | IV | <16 weeks | >16 weeks | Fracture
nonunion | Femoral head
necrosis | Other
complications |
|---|
| Group A | 51 | 42 | 8 | 1 | 0 | 46 | 5 | 1 | 2 | 4 |
| Group B | 55 | 45 | 10 | 0 | 0 | 52 | 3 | 0 | 1 | 3 |
| T-value | | Fisher | | | | Fisher | | Fisher | Fisher | Fisher |
| P-value | | 0.701 | | | | 0.316 | | 0.481 | 0.471 | 0.709 |
With regard to hip joint function assessment, there
were no significant differences in FRS scores before injury, before
surgery and at 1, 3 and 12 months following surgery between groups
A and B (P>0.05; Table IV).
There were also no significant statistical differences in FRS
scores at the last follow-up in each group compared with those
before injury, indicating that the two groups of patients basically
restored their hip function, as before injury, at 12 months after
surgery (P>0.05; Table
IV).
 | Table IVComparison of hip FRS functional
scores between the two groups of patients with femoral neck
fractures. |
Table IV
Comparison of hip FRS functional
scores between the two groups of patients with femoral neck
fractures.
| Parameter | Time-point | Group A (n=51) | Group B (n=55) | T-value | P-value |
|---|
| Hip function FRS
score | Before injury | 83.8±6.9 | 84.3±6.2 | -0.3929 | 0.6952 |
| | Before surgery | 27.5±3.9 | 28.2±4.8 | -0.8202 | 0.4140 |
| | 1 month after
surgery | 52.1±2.5 | 52.3±3.1 | -0.3639 | 0.7167 |
| | 3 months after
surgery | 55.3±3.5 | 56.2±2.9 | -1.4457 | 0.1513 |
| | 12 months after
surgery | 83.3±7.5 | 84.1±6.9 | -0.5720 | 0.5686 |
|
F-valuea | | 0.3504 | 0.1599 | | |
|
P-valuea | | 0.7268 | 0.8733 | | |
Discussion
Femoral neck fractures are common hip fractures in
the elderly, with an incidence of ~3%. Femoral neck fractures are a
serious threat to the life safety of elderly patients. If
conservatively treated, patients often succumb from complications
such as hypostatic pneumonia, deep venous thrombosis, bed sores,
and urinary system infections. Therefore, surgical treatment to
quickly restore hip function and avoid bedridden complications, has
been unanimously recognized by the academic community. At present,
hip replacement is often performed for severely displaced Garden
III and IV femoral neck fractures in the elderly; at the same time,
internal fixation is recommended for nondisplaced Garden I-II and
less displaced Garden type III femoral neck fractures. In addition,
internal fixation is also the preferred alternative for elderly
patients who cannot tolerate joint replacement surgery (12,15).
Since Dr Smith-Petersen, an American physician,
invented trifin screws for treating femoral neck fractures in 1931,
femoral neck internal fixation surgical devices have been rapidly
developed over the decades, and various internal fixation devices
such as cannulated screws, DHS, proximal femoral locking plate,
percutaneous compression plate, medial buttress plate, and FNS have
been invented are used in clinical practice to this day. Among
them, the novel FNS has obvious biomechanical advantages and can
support the fracture in multi-axial direction, with excellent
anti-rotation and anti-shortening properties, with significant
clinical efficacy (15-19).
However, in China, limited by unbalanced economic development,
cannulated screw internal fixation is still the most important
surgical method, especially in the vast Central and Western regions
and primary hospitals. After closed reduction of femoral neck
fracture, internal fixation of three cannulated screws has obvious
economic and safety advantages, significantly reducing surgical
trauma and retaining better joint function. Therefore, this
surgical intervention is widely used in primary hospitals in China.
The arrangement of three half-threaded cannulated screws has always
been the focus of the attention of clinicians, and a number of
previous biomechanical experiments have shown that inverted
triangular distribution has theoretically strong biomechanical
properties and is the ‘gold standard’ for treatment with three
cannulated screws (12,18,20,21).
However, it must be emphasized that inverted
triangular distribution has numerous shortcomings and limitations
as well (15,16,22-24).
First of all, osteoporosis is common in elderly patients. During
injury, due to the traction of hip muscles and ligaments, femoral
neck fractures are often angulated anteriorly, and the
posterolateral cortex is often compressed and comminuted. However,
in biomechanical experiments, the fracture line of the femoral neck
fracture model is commonly neatly cut artificially. Therefore,
during inverted triangular fixation, posterolateral screws often
have shortcomings such as difficult guide wire placement, poor
screw holding force, and even increased screws on the lateral and
posterior sides to improve biomechanical stability. Secondly, the
Chinese population, especially the female population, often has
small bones, anatomically slender femoral necks and narrow screw
placement spaces, making it difficult to place two 7.3 mm or even
6.5 mm diameter cannulated screws in the same plane of the lateral
femoral wall. The core of inverted triangular distribution is to
maximize the biomechanical efficacy through the ‘cortical support’
effect of three screws. The key point of cortical support is to
arrange each screw to be as close as possible to the anterior,
posterior, and inferior cortex of the femoral neck so that the
distance between the screw and the cortex is within 3 mm, thereby
maximizing screw holding force. However, in the sagittal position,
the proximal femur is wider at the top and narrower at the bottom.
As a result, the screw can only be guided by fluoroscopy after
closed reduction. In order to achieve the inverted triangular
distribution of the three screws and provide enough support,
multiple fluoroscopies are often required during the operation to
repeatedly adjust the direction of the guide wire, and repeated
adjustment of the guide wire in elderly patients easily causes
severe destruction of the residual bone due to severe osteoporosis,
resulting in decreased screw holding force after screw placement,
and repeated operations can cause more soft tissue injuries.
Therefore, in recent years, some scholars have continuously
proposed the use of novel guidance devices (25), such as a 3D printing navigation
module, and even the placement of guide wires and screws under
robotic navigation (20), but
these devices are all costly and not suitable for the national
economic conditions of China. In addition, such surgical methods
have a long learning cycle for doctors in primary care institutions
and young doctors in China, and are difficult to operate. Because
the blood supply of the femoral head is mainly supplied by the
vascular network around the femoral neck (especially the
retinacular artery and supraepiphyseal artery network) (26,27),
repeated adjustment of the guide wire during operation is also
likely to cause new iatrogenic vascular injury, resulting in an
increased incidence of avascular necrosis of the femoral head.
Therefore, the Department of Joint Surgery of the
First Affiliated Hospital of Nanjing Medical University (Jiangsu
Province Hospital), has been working on the treatment of femoral
neck fractures in the elderly with three cannulated screws with
parallel distribution for numerous years, and have achieved
satisfactory clinical results. Compared with traditional inverted
triangular distribution, the operation steps of parallel
distribution are significantly simplified, with significant
advantages in the operation time, number of times intraoperative
fluoroscopy is performed and number of intraoperative guide wire
adjustments, and without the need for various complex navigation
devices. The learning period required for this surgical technique
is short, making it particularly suitable for young doctors and
inexperienced orthopedic surgeons. The main reason is that parallel
distribution only requires locating the spatial position of the
guide wire on the anteroposterior view, and the lateral view can
only be in the direction of the femoral neck axis, without
considering the needle insertion direction of the two planes in the
anteroposterior and lateral views to pursue the cortical support
effect which is required for inverted triangular distribution.
Central screw placement in the lateral femoral neck axis can also
reduce injury to the anterolateral and posterolateral cortex, which
instead increases system stability. Moreover, parallel distribution
theoretically reduces the incidence of femoral head necrosis due to
the simple operation which reduces the interference with the
vascular network around the femoral neck. For elderly patients,
parallel distribution accelerates the speed of surgery,
significantly shortens the anesthesia time, significantly reduces
the surgical stress and surgical injury to patients, significantly
increases the incidence of extubation in patients after surgery,
and significantly decreases the proportion of patients transferred
to the ICU. Therefore, it is more conducive to the rehabilitation
of patients, and is more in line with the ERAS concept of
orthopedics (28). In addition, in
terms of fracture healing and fracture reduction, cannulated screws
with parallel distribution achieve similar clinical efficacy to the
‘gold standard’ inverted triangular distribution and do not
increase the probability of femoral neck nonunion and avascular
necrosis of the femoral head. Although postoperative functional
recovery is emphasized, there is still a significant gap between
Chinese patients and Western patients with regard to functional
rehabilitation. The majority of patients continue bed rest at home
for 6-8 weeks after discharge, resulting in a low incidence of
complications such as back-off of the screws and failure of
fixation. At the beginning of 2022, Chinese scholars reported the
clinical efficacy of cannulated screws with parallel distribution
and cannulated screws with inverted triangular distribution in the
treatment of young and middle-aged femoral neck fractures. The
final results showed that the parallel distribution of three
cannulated screws in the screw placement group had achieved
satisfactory clinical efficacy, which is worthy of clinical
promotion (29). At present, to
the best of the authors' knowledge there is no clinical report on
the treatment of femoral neck fractures in the elderly with three
cannulated screws with parallel distribution in China. In
biomechanical studies, the biomechanical stability of various
femoral neck fixation devices varied due to their own structure and
indications (17,18,30,31).
At present, the mainstream view is that FNS exhibits good stability
(17,18). However, there is a lack of
biomechanical stability studies on three cannulated screws with
parallel distribution and inverted triangular distribution, thus
requiring further elucidation in future studies. The next research
plan of the authors will be to develop related biomechanical
studies.
In conclusion, the elderly patients with femoral
neck fractures that underwent surgery with the parallel
distribution of three cannulated screws after closed reduction
achieved similar clinical efficacy to the ‘gold standard’ of
inverted triangular distribution, and had obvious advantages in
terms of operation time, number of times intraoperative fluoroscopy
was performed and number of intraoperative guide wire adjustments,
with significantly reduced surgical difficulty. In summary, this
procedure is worthy of promotion and clinical application in the
majority of primary hospitals in China.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
All data generated or analyzed during this study are
included in this published article.
Authors' contributions
XH designed the whole study, collected the data
regarding hospitalization and follow-up of all patients, and agreed
to be accountable for all aspects of the study. JL analyzed and
interpreted the data, and drafted the initial manuscript. QZ and HZ
analyzed and interpreted the data. XH and JL confirm the
authenticity of all the raw data. All authors read and approved the
final manuscript.
Ethics approval and consent to
participate
The present study was approved (approval no.
2019-SRFA-453) by the Ethics Committee of the First Affiliated
Hospital of Nanjing Medical University (Nanjing, China). All
patients signed the operation consent form before surgery, and
informed consent for participation was obtained from the patients
or their families.
Patient consent for publication
Patient consent for publication was obtained from
all the patients.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Walter N, Szymski D, Kurtz SM, Lowenberg
DW, Alt V, Lau EC and Rupp M: Epidemiology and treatment of
proximal femoral fractures in the elderly U.S. population. Sci Rep.
13(12734)2023.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Veronese N and Maggi S: Epidemiology and
social costs of hip fracture. Injury. 49:1458–1460. 2018.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Parker MJ and Cawley S: A long term
follow-up for a randomised trial of total hip arthroplasty versus
hemiarthroplasty for displaced intracapsular fractures. Injury.
54(110925)2023.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Zhang J, Chang X, Sun Z and Tang X:
Comparison of femoral neck system versus cannulated compression
screws in treating femoral neck fractures: A systematic review and
meta-analysis. Asian J Surg. 46:3259–3260. 2023.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Li L, Bennett-Brown K, Morgan C and
Dattani R: Hip fractures. Br J Hosp Med (Lond). 81:1–10.
2020.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Bartels S, Kristensen TB, Gjertsen JE,
Frihagen F, Rogmark C, Dolatowski FC, Figved W, Benth JŠ and Utvåg
SE: Total Hip arthroplasty leads to better results after low-energy
displaced femoral neck fracture in patients aged 55 to 70 years: A
randomized controlled multicenter trial comparing internal fixation
and total hip arthroplasty. J Bone Joint Surg Am. 104:1341–1351.
2022.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Ekhtiari S, Gormley J, Axelrod DE, Devji
T, Bhandari M and Guyatt GH: Total hip arthroplasty versus
hemiarthroplasty for displaced femoral neck fracture: A systematic
review and meta-analysis of randomized controlled trials. J Bone
Joint Surg Am. 102:1638–1645. 2020.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Guyen O: Hemiarthroplasty or total hip
arthroplasty in recent femoral neck fractures? Orthop Traumatol
Surg Res. 105(1S):S95–S101. 2019.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Dekhne MS, Thomas HM, Haider T, Mortensen
S, Rodriguez EK, Weaver MJ and Keudell AV: Treatment and outcomes
of basicervical femoral neck fractures: A systematic review. J
Orthop Surg (Hong Kong). 29(23094990211003344)2021.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Tang Y, Zhang Z, Wang L, Xiong W, Fang Q
and Wang G: Femoral neck system versus inverted cannulated
cancellous screw for the treatment of femoral neck fractures in
adults: A preliminary comparative study. J Orthop Surg Res.
16(504)2021.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Augat P, Bliven E and Hackl S:
Biomechanics of femoral neck fractures and implications for
fixation. J Orthop Trauma. 33 (Suppl 1):S27–S32. 2019.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Zelle BA, Salazar LM, Howard SL, Parikh K
and Pape HC: Surgical treatment options for femoral neck fractures
in the elderly. Int Orthop. 46:1111–1122. 2022.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Garden RS: Malreduction and avascular
necrosis in subcapital fractures of the femur. J Bone Joint Surg
Br. 53:183–197. 1971.PubMed/NCBI
|
|
14
|
Zuckerman JD, Koval KJ, Aharonoff GB and
Skovron ML: A functional recovery score for elderly hip fracture
patients: II. Validity and reliability. J Orthop Trauma. 14:26–30.
2000.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Davidson A, Blum S, Harats E, Kachko E,
Essa A, Efraty R, Peyser A and Giannoudis PV: Neck of femur
fractures treated with the femoral neck system: outcomes of one
hundred and two patients and literature review. Int Orthop.
46:2105–2115. 2022.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Tian P, Kuang L, Li ZJ, Xu GJ and Fu X:
Comparison between femoral neck systems and cannulated cancellous
screws in treating femoral neck fractures: A meta-analysis. Geriatr
Orthop Surg Rehabil. 13(21514593221113533)2022.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Teng Y, Zhang Y and Guo C: Finite element
analysis of femoral neck system in the treatment of Pauwels type
III femoral neck fracture. Medicine (Baltimore).
101(e29450)2022.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Wang F, Liu Y, Cheng L and Zhao D:
Research progress in biomechanics of common internal fixation for
femoral neck fracture. ZhongguoXiu Fu Chong Jian Wai Ke Za Zhi.
36:896–901. 2022.PubMed/NCBI View Article : Google Scholar : (In Chinese).
|
|
19
|
Wu ZF, Luo ZH, Hu LC and Luo YW: Efficacy
of the femoral neck system in femoral neck fracture treatment in
adults: A systematic review and meta-analysis. World J Clin Cases.
10:11454–11465. 2022.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Cheng QH, Li PB, Lu TT, Guo SF, Di WF,
Yang KH and Qian YW: Computer-assisted cannulated screw internal
fixation versus conventional cannulated screw internal fixation for
femoral neck fractures: A systematic review and meta-analysis. J
Orthop Surg Res. 16(687)2021.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Long Y, Zhang S, Wang K, Liu C, Zhou M,
Wang X, Zhang W and Qiao L: Strategies of closed reduction in
treatment of femoral neck fracture using cannulated screw fixation.
ZhongguoXiu Fu Chong Jian Wai Ke Za Zhi. 30:809–814.
2016.PubMed/NCBI View Article : Google Scholar : (In Chinese).
|
|
22
|
Yuan KX, Yang F, Fu K, Zhu DY, Jiang CY,
Jin DX, Wang ZH, Peng XY, Gao YS and Luo PB: Internal fixation
using fully threaded cannulated compression screws for fresh
femoral neck fractures in adults. J Orthop Surg Res.
17(108)2022.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Cuellar DO III, Garcia Velez DA, Bledsoe G
and Tracy Watson J: Hybrid screw fixation for femoral neck
fractures: Does it prevent mechanical failure? Injury.
53:2839–2845. 2022.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Jin ZY, Gu C, Yang HL and Xu M: Outcome of
percutaneous compression plate for treatment of femoral neck
fractures: mean follow-up of 4.4 years. Int Orthop. 46:1891–1898.
2022.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Ren BF, Li G, Ma QP, Lv X and Sun J: Quick
and accurate placement of cannulated screws to internal fixation of
femoral neck fractures using a novel guide device. Adv Ther Nov.
40:844–852. 2022.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Wu SH, Miao Y, Zhu XZ and Li GY:
Assessment of the local blood supply when femoral neck fracture
occurs: Advances in the anatomy research and its clinical
application. Zhongguo Gu Shang. 36:294–298. 2023.PubMed/NCBI View Article : Google Scholar : (In Chinese).
|
|
27
|
Seijas R, Sallent A, Rivera E and Ares O:
Avascular necrosis of the femoral head. J Invest Surg. 32:218–219.
2019.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Liu SY, Li C and Zhang PX: Enhanced
recovery after surgery for hip fractures: A systematic review and
meta-analysis. Perioper Med (Lond). 10(31)2021.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Ma Z, Zhang S, Zhang Z, et al: Comparison
of therapeutic effects between parallel and inverted triangular
nail placement in the treatment of femoral neck fractures in
middle-aged and young adults. J North Sichuan Med College.
37:509–512. 2022.
|
|
30
|
Wang J, Gao Y, Song D and Ni J:
Biomechanical study on parallel cannulated compression screw
combined with medial buttress plate fixation and F-type cannulated
compression screw fixation in Pauwels III femoral neck fracture: A
finite element analysis. Zhong Nan Da XueXue Bao Yi Xue Ban.
47:1143–1153. 2022.PubMed/NCBI View Article : Google Scholar : (In Chinese).
|
|
31
|
Zhang RY, Li JT, Zhao JX, Zhao Z, Zhang
LC, Yun C, Su XY and Tang PF: The oblique triangle configuration of
three parallel screws for femoral neck fracture fixation using
computer-aided design modules. Sci Rep. 12(325)2022.PubMed/NCBI View Article : Google Scholar
|