Introduction
The chest is a vulnerable site for injury, but
rupture of the main airway after chest trauma is a rare and
potentially fatal occurrence (1).
The incidence of tracheal injury after trauma is 0.5-2% and the
mortality rate is ~9% (2). Often,
physical airway obstruction is caused by a collapse of the main
airway due to tremendous kinetic energy caused by the injury. This
high-energy trauma is combined with fractures of the ribs and
sternum, which alter the intrathoracic pressure state through
paradoxical breathing, thereby affecting the stability of the
thorax. The combination of massive pneumothorax and extensive lung
contusion can potentially result in death from respiratory failure
(3). In order to alleviate airway
obstruction and restore thoracic stability, such patients often
require active surgical procedures (4).
Extracorporeal membrane oxygenation (ECMO), also
known as artificial lung, is a modified extracorporeal circulation
technique that can effectively replace the heart and pulmonary
function to maintain the body's circulation and gas exchange, which
allows time for the recovery of cardiopulmonary function (5). For decades, ECMO has been a useful
supportive therapy for severe cardiopulmonary disease (6). Cardiopulmonary support for traumatic
tracheo-bronchial injury in adults was first described in
2012(7). The present case report
provides details on the diagnosis and treatment process of a
39-year-old male patient who underwent airway reconstruction in
order to relieve airway obstruction under ECMO support.
Case Report
A 39-year-old man was crushed by an excavator during
the course of his work in July 2022. The patient experienced severe
chest pain immediately after the injury, as well as chest tightness
and shortness of breath, dyspnea and continuous hemoptysis, without
hematemesis. The patient presented to the emergency room of Jiashan
First People's Hospital (Jiaxing, China) 30 min after the injury
occurred, where they were admitted with clear consciousness and
dysphoria, a body temperature of 36.2˚C, heart rate of 112
beats/min (bpm), respiration rate of 38 breaths/min, blood pressure
of 107/72 mmHg and oxygen saturation (SPO2) of 92%. Upon
examination of the patient, there was swelling and bruising in the
neck, massive subcutaneous emphysema on both sides of the chest
wall and beneath the abdominal wall, drum sounds on percussion of
both lungs and a loss of breath sounds on auscultation. On physical
examination, the patient's oxygen saturation had declined to
<80%, tracheal intubation was performed immediately and CT was
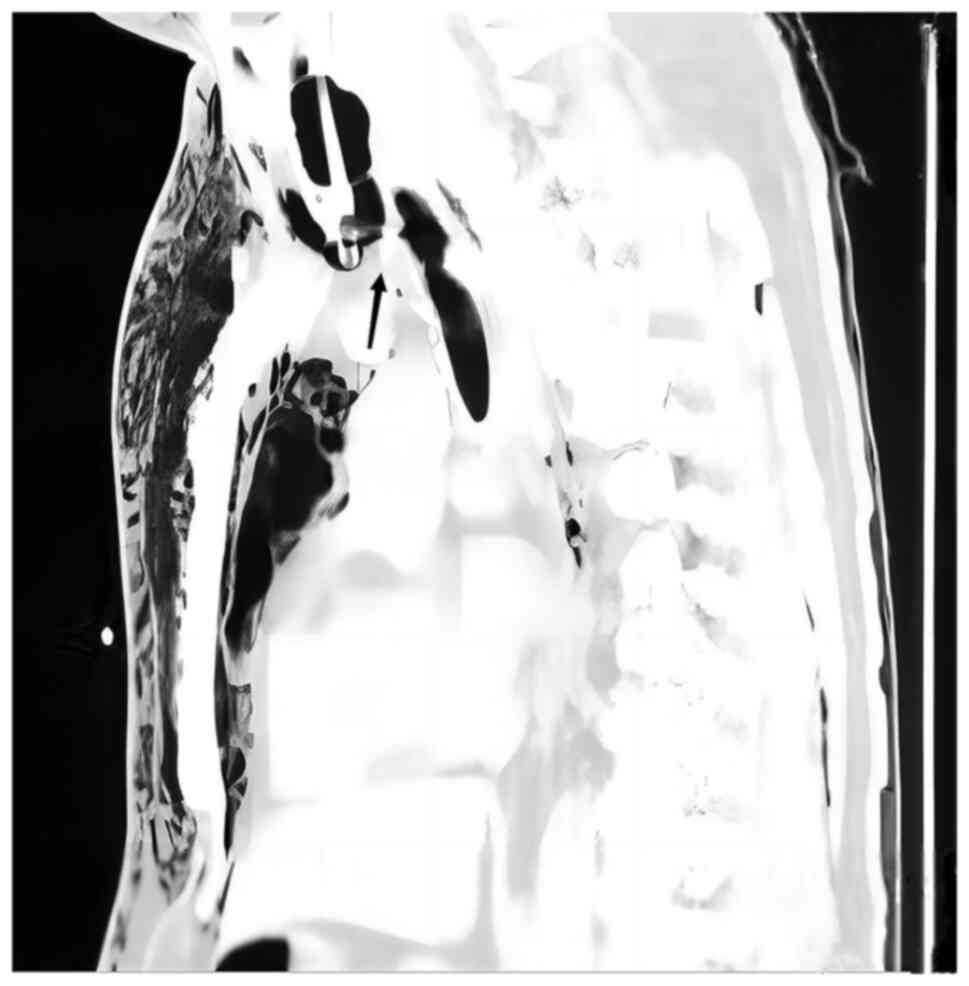
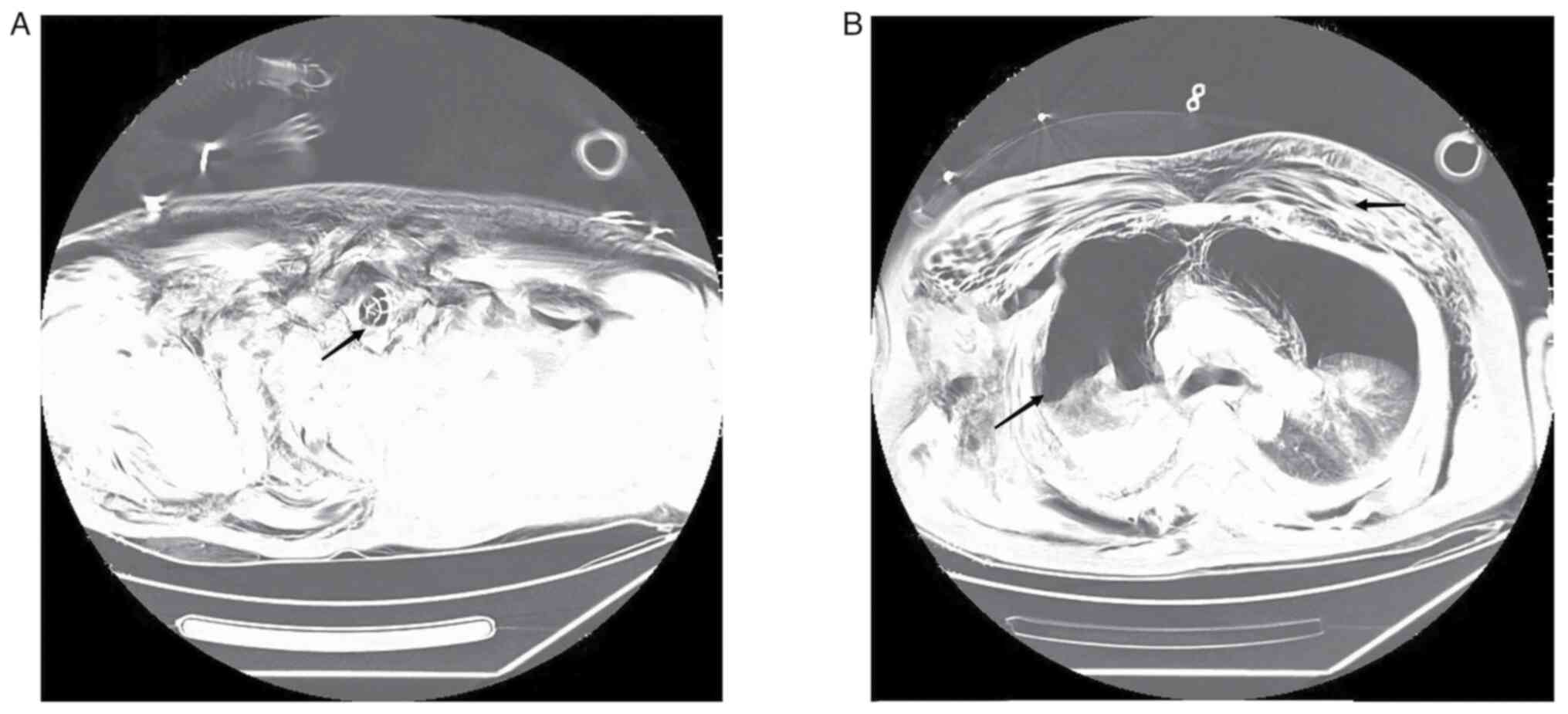
performed. CT examination demonstrated multiple air accumulations
in the cerebral sulcus, cerebral fissure and ventricles, collapse
of the main bronchus, bronchial occlusion on both sides,
pneumothorax on both sides with partial lung tissue inflation, 70%
lung compression, multiple rib fractures on both sides, massive
subcutaneous emphysema on both sides of the chest wall, fracture of
the right scapula and fracture of the right clavicle (Figs. 1 and 2). The results of the blood gas analysis
were as follows: Partial pressure of oxygen (PaO2), 51.3
mmHg (normal range: 80-100 mmHg); partial pressure of carbon
dioxide, 67.2 mmHg (normal range: 35-45 mmHg); base excess, -8.4
mmol/l (normal range: -3-+3 mmol/l); pH, 7.15 (normal range:
7.35-7.45); lactate level, 4.5 mmol/l (normal range: 0.5-2.2
mmol/l); and hemoglobin level, 104 g/l (normal range: 130-175
g/l).
The preliminary diagnosis was as follows: Main
bronchial rupture, bilateral hemopneumothorax, pulmonary contusion,
multiple rib fractures and respiratory failure. After the course of
CT examination, the patient became unconscious and ceased to
respond to calls, SPO2 gradually decreased to 65% and
the heart rate slowed to 23 bpm. The monitor indicated ventricular
escape rhythm; therefore, the patient was immediately administered
cardiothoracic compressions, bilateral closed chest drainage and
epinephrine 1 mg was administered intravenously for cardiac
stimulation. Tranexamic acid 1 g was administered by intravenous
drip to stop bleeding and pethidine 50 mg was injected
intramuscularly for pain relief. The patient also received lactate
Ringer's solution 2,000 ml intravenous infusion to replenish the
blood volume and Propofol 0.5 g micropump injection for sedation.
The patient achieved return of spontaneous circulation 10 min after
resuscitation. Combined with the previous CT report, respiratory
arrest due to acute respiratory failure caused by collapse of the
main airway was considered. After the multidisciplinary team (MDT)
of the regional trauma center (Jiaxing First Hospital Trauma
Center; Jiaxing China), was invited for remote consultation, it was
decided to perform main airway repair to improve the patient's
ventilation and oxygen supply.
The operation could not be performed immediately, as
the emergency operating room of Jiashan First People's Hospital's
(Jiaxing, China) was occupied at the time due to an ongoing
surgery. The second hour after the injury, no improvement in the
patient's condition was observed after endotracheal intubation.
Subcutaneous emphysema developed and SPO2 continued to
decline after endotracheal intubation. Under volume control mode
(tidal volume, 8 ml/kg; respiratory rate, 42 breaths/min; positive
end-expiratory pressure, 10 mmHg; oxygen concentration, 100%), the
patient's oxygenation index (PaO2/fraction of inspired
oxygen) continued to fall <50 mmHg and blood lactate rose to 8.2
mmol/l; therefore, the patient's condition had reached the level
where ECMO support was required (5).
The operating room was occupied; therefore, the
operation could not be carried out after the arrival of the MDT
specialist cardiothoracic surgeon. The cardiothoracic surgeon
performed a tracheoscopy. Immediate tracheoscopy showed no tracheal
prominences and indicated that the main airway was broken.
Veno-venous-ECMO (VV-ECMO) was performed on the right femoral vein
and the right internal jugular vein. Under ultrasound guidance, a
20Fr introducer catheter was placed through the right femoral vein
and a 19Fr return catheter through the right internal jugular vein
at the puncture point using the Seldinger technique (8). The initial catheter position was
adjusted through transepigastric ultrasound. Upon completion of the
procedure, a bedside X-ray confirmed the placement of the head of
the femoral vein at the opening between the inferior vena cava and
right atrium (data not shown). A ROTAFLOW centrifugal pump (Maquet
Cardiopulmonary GmbH) and a QUADROX PLS oxygenator (Maquet
Cardiopulmonary GmbH) were used to pre-flush the ECMO line with
5,000 units heparin. After flushing, the catheter was connected to
the patient. Treatment parameters were set as follows: Speed, 685 x
g; blood flow, 4 l/min; and oxygen flow, 4 l/min. Patient
SPO2 was maintained at ~90%.
Five hours after the injury, the patient was
escorted in an ambulance to Jiaxing First Hospital Trauma Center
(Jiaxing, China) with support for ECMO and ventilator. After
arrival, the patient underwent emergency tracheal repair at the
cardiothoracic surgery department, while maintaining an
SPO2 of ~93% with ECMO support. A median cervical
incision was made, and a complete dissection of the tracheal
membrane was observed intraoperatively between the first and second
tracheal cartilages. ECMO was used in place of intraoperative
ventilator support and pulmonary ventilation was terminated. As
part of the tracheal reconstruction procedure, the upper and lower
severed ends were explored, and the broken membrane was sutured to
the anterior tracheal cartilage. Following the ECMO procedure, the
patient was transported to the Emergency Intensive Care Unit, where
heparin anticoagulation was administered. Heparin speed was
maintained at 125-375 U/h, activated clotting time at 100-140 sec
and hemoglobin at 85-101 g/l. On the second day after surgery, the
ECMO parameters were as follows: Rotational speed, 3,200 r/min;
blood flow, 3.1 l/min; oxygen flow, 2.3 l/min; and SPO2,
~93%. The mean arterial pressure was ~60 mmhg before norepinephrine
administration and increased to 80-90 mmHg with norepinephrine
norepinephrine (0.1-0.2 µg/kg/min), SPO2 was >93%.
ECMO flow was adjusted according to blood gas analysis; the
rotational speed was reduced by ~5 x g per day. PaO2
fluctuated between 95 and 234 mmHg, and the partial pressure of
carbon dioxide was within the 35-45 mmHg (normal range: 35-45
mmHg). After 5 days, ECMO parameters were as follows: Rotational
speed, 224 x g; blood flow, 2.2 l/min; oxygen flow, 1.2 l/min; and
SPO2, >95%. The patient's condition improved with
stable blood circulation and ECMO was terminated. No further
surgery was performed for rib, scapula and clavicle.
After ECMO decannulation, ventilator therapy was
used under volume control mode (tidal volume, 8 ml/kg; respiratory
rate, 25 breaths/min; positive end-expiratory pressure, 5 mmHg;
oxygen concentration, 50%). Following the withdrawal of the ECMO
machine, a chest CT was performed. Bilateral lung effusion and
pleural effusion were reduced, and pneumothorax and subcutaneous
emphysema was partially absorbed in the chest wall compared with
the patient's condition at the time of admission. At 7 days after
the injury, the patient's consciousness was similar to that on
arrival at the trauma center, which may be related to
craniocerebral injury or cerebral anoxia due to ventricular escape
rhythm, and expectoration was poor. When the tracheal catheter was
used for sputum aspiration, only ~20 cm of the sputum aspiration
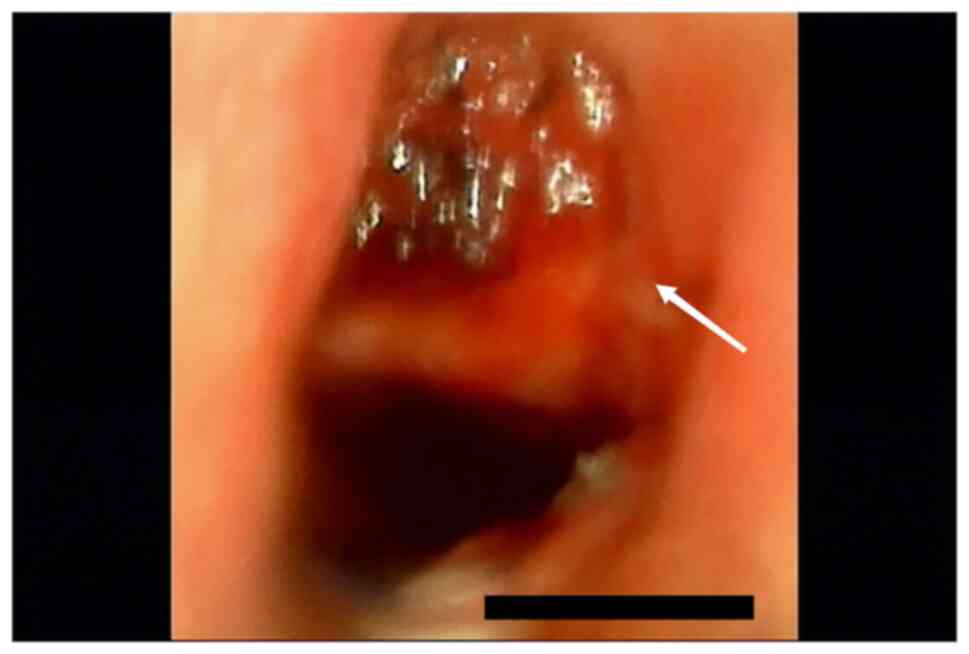
tube could be inserted. A fiberoptic bronchoscopy was performed and
when the fiberoptic tracheoscope probe was inserted into the
tracheal repair site, it was found that the tracheal cartilage had
collapsed, resulting in airway stenosis (Fig. 3). In consultation with the
Department of Otolaryngology, Jiaxing First Hospital, a tracheotomy
was recommended. A tracheal tube was placed under the inferior
tracheal cartilage through a median cervical incision. The patient
was treated with high-flow oxygen therapy after tracheotomy and was
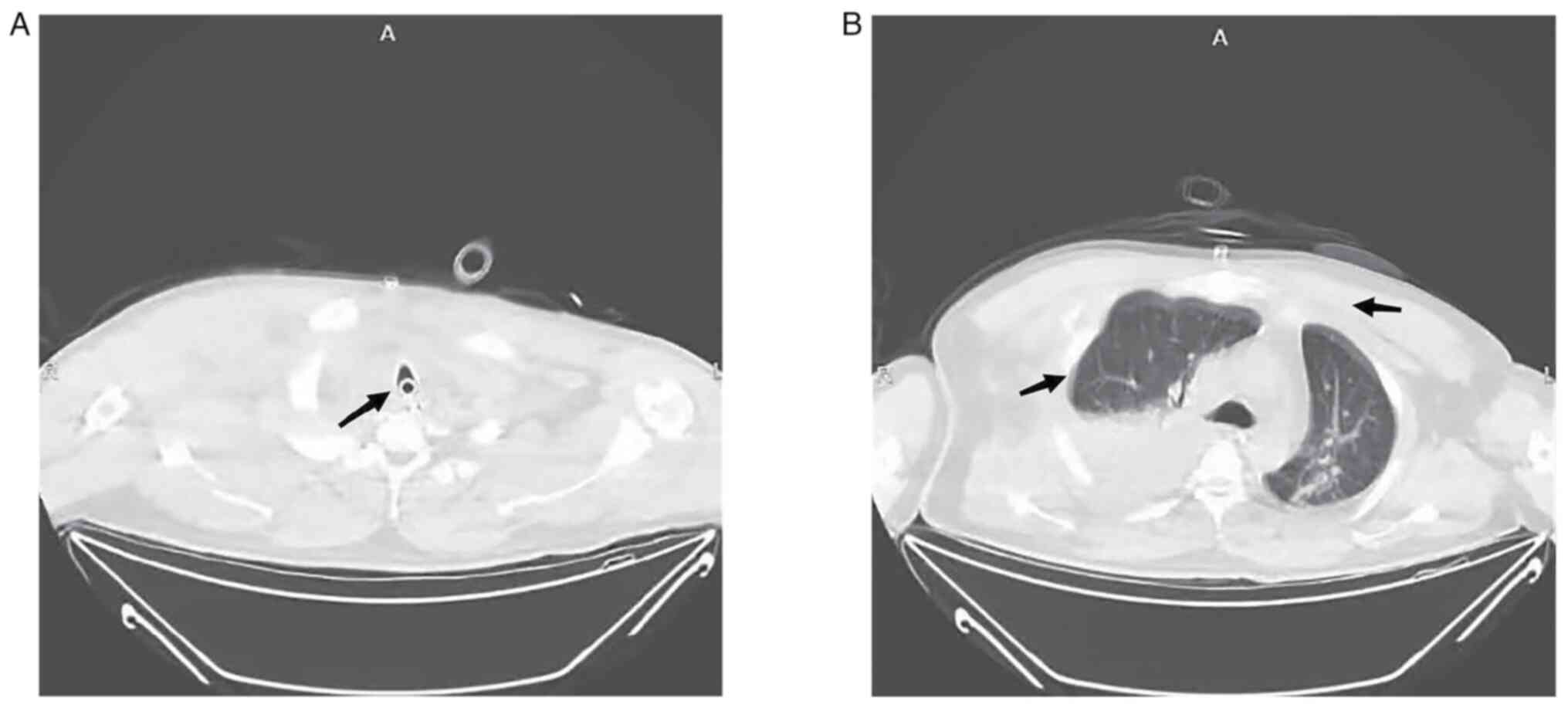
then transferred to a general ward for rehabilitation. On the 10th
day after injury, chest CT indicated that lungs were not
compressed, and the pneumothorax and subcutaneous emphysema had
been absorbed (Fig. 4). After 24
days of hospitalization, the patient's consciousness had improved;
however, they could not take care of themselves. The patient was
transferred back to the hospital of the first presentation, Jiashan
First People's Hospital (Jiaxing, China), for rehabilitation
treatment. The patient was discharged after 58 days of
rehabilitation. In January 2023, the patient is off the ventilator,
but is unconscious, bedridden and unable to care for
themselves.
Discussion
ECMO is a valuable clinical tool used for
cardiopulmonary support, allowing effective gas exchange when
ventilation is not possible in certain situations, such as heart or
respiratory failure. According to the blood flow pathway, there are
two types of ECMO: VV- and veno-arterial (VA)-ECMO. As VA-ECMO
improves oxygenation and provides cardiac support, it is primarily
used in cases of severe heart failure or heart transplantation.
However, VV-ECMO has a relatively low impact on circulation since
the patient's own cardiac function maintains the blood flow
(5). Therefore, VV-ECMO is
primarily used in patients with non-cardiac acute respiratory
failure in order to improve oxygenation by adjusting oxygenation
parameters (9). Although the use
of ECMO in patients with severe chest trauma has been controversial
due to trauma-induced coagulopathy and higher bleeding risk
(10), there is increasing
evidence that ECMO can serve a crucial role in the case of
ineffective conventional treatment of patients with severe chest
trauma (11-13).
In order to improve the chance of survival of the patient presented
in the current case report during surgery, the multidisciplinary
trauma team decided to apply the VV-ECMO treatment model.
The repair of the trachea is a demanding and
difficult procedure, which requires optimal exposure of the
surgical field and adequate oxygenation of the tissues during the
reconstruction of the airway. In order to maintain oxygen supply
during bronchial repair, a catheter is often used to ventilate the
distal airway, or high-frequency jet ventilation or high-flow
oxygen is instilled into the tracheal intubation catheter (14,15).
Alternatively, a double-lumen tracheal intubation catheter can be
used, where the lung tissue on the affected side is prevented from
being ventilated, while the lung tissue on the healthy side is
ventilated (16). In the present
case report, the lung ventilation-blood flow ratio was imbalanced
due to the dissection of the main airway and incomplete expansion
of both lungs; therefore, intraoperative oxygenation could not
provide adequate oxygen if administered exclusively through
tracheal intubation. When effective ventilation cannot be assured,
ECMO support is considered to be essential in ensuring effective
gas exchange. The purpose of this procedure is to prevent hypoxia
in the patient caused by inadequate intrapulmonary ventilation
during surgery (17).
In order to prevent the development of thrombosis in
the membrane oxygenator during ECMO therapy, appropriate
anticoagulation measures should be taken (5). However, in trauma and surgical
patients, anticoagulation therapy may lead to severe bleeding, and
heparinization management during ECMO therapy in post-trauma
patients has been a focus of current research (18). The high speed of the ECMO
centrifugal pump, the high blood flow generated during surgery and
the biological layer used on the inner surface of the line (Bioline
coating), the main components of which are macromolecule heparin
and therapeutic peptide molecules, have resulted in a reduction of
the risk of blood clotting in the device (19,20).
A previous study reported that there was no heparinization
management prescribed for 5 days following the membrane oxygenator
therapy, which may result in apparent clotting spots and
thrombosis-related complications (20). In this case, ECMO coagulation was
not observed and organ bleeding due to anticoagulation therapy was
avoided by closely monitoring changes in hemoglobin, lactate and
vital signs, and administering low-dose heparin anticoagulation
postoperatively.
In the present study, despite the patient undergoing
an airway reconstruction in order to relieve airway obstruction
under ECMO support, the recovery of brain function was slow as a
result of cerebral ischemia and hypoxia. In addition, the narrowing
of the trachea for subsidence of the tracheal reconstruction
prevented the discharge of airway secretions, which can cause
pulmonary atelectasis and lung infection (21). However, although tracheotomy is a
mandatory procedure, the location of tracheal rupture overlapped
with the location of airway reconstruction. Tracheotomy was
performed between the tracheal cartilage rings below the airway
reconstruction following consultation with an
otorhinolaryngologist. To date, previous studies examining the
timing of tracheotomies in trauma patients have focused on
subgroups of patients, such as those suffering from traumatic brain
injuries and burns (22,23). A previous study by Zhang et
al (24) concluded that early
tracheotomy may improve the 28-day survival in patients with
multiple rib fractures. However, a better predictive model is
required to assess the timing of tracheotomy in patients with
post-traumatic tracheal rupture.
The procedures presented in the current study may
provide guidance for the diagnosis and treatment of future patients
with traumatic tracheal rupture and respiratory failure. The use of
ECMO during tracheal repair surgery has a major advantage of
maintaining adequate gas exchange during the procedure to avoid the
poor prognosis commonly associated with inadequate ventilation
during conventional surgery. Due to the working characteristics of
ECMO and the lines with Bioline coating, combined with close
bleeding risk monitoring and a highly specialized disciplinary
team, the risk of bleeding during ECMO support in trauma patients
is significantly reduced with low anticoagulation intensity
compared with standard anticoagulation therapy regimens. In these
patients, timing of the tracheotomy needs to be further discussed,
and performing the tracheotomy earlier to be completed during
airway reconstruction is an additional option to improve the
treatment of such patients.
The present case report demonstrated that ECMO could
replace lung function in a patient with chest trauma during an
emergency condition to save time for surgery and reduce the
potential adverse outcomes of the patient. In summary, to improve
oxygenation and assist in airway reconstruction surgery, ECMO
therapy in patients with traumatic tracheal ruptures is a potential
successful treatment method, and could be considered during the
diagnosis and management of related conditions.
Acknowledgements
Not applicable.
Funding
Funding: This study was supported by a project from the
Scientific Research Fund of Zhejiang Provincial Education
Department (grant no. Y202249584).
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
LC and XX designed and supervised the study. LC, JX
and LT performed data collection and analysis. LC and YZ performed
data analysis and interpretation. All authors confirm the
authenticity of all the raw data. All authors have read and
approved the final version of the manuscript.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
The patient provided written informed consent for
publication of this case report and the accompanying images.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Lafferty PM, Anavian J, Will RE and Cole
PA: Operative treatment of chest wall injuries: Indications,
technique, and outcomes. J Bone Joint Surg Am. 93:97–110.
2011.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Prokakis C, Koletsis EN, Dedeilias P,
Fligou F, Filos K and Dougenis D: Airway trauma: A review on
epidemiology, mechanisms of injury, diagnosis and treatment. J
Cardiothorac Surg. 9(117)2014.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Gao JM, Li H, Du DY, Yang J, Kong LW, Wang
JB, He P and Wei GB: Management and outcome of bronchial trauma due
to blunt versus penetrating injuries. World J Clin Cases.
10:5185–5195. 2022.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Lin WT, Su SY, Hsieh CF, Lai CC and Chao
CM: Traumatic thoracic burst fracture associated with bronchial
rupture. J Emerg Med. 53:260–261. 2017.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Wrisinger WC and Thompson SL: Basics of
extracorporeal membrane oxygenation. Surg Clin North Am. 102:23–35.
2022.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Abrams D and Brodie D: Novel uses of
extracorporeal membrane oxygenation in adults. Clin Chest Med.
36:373–384. 2015.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Walker JL, Wiersch J, Benson C, Young HA,
Dearmond DT and Johnson SB: The successful use of cardiopulmonary
support for a transected bronchus. Perfusion. 27:34–38.
2012.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Patel AR, Patel AR, Singh S, Singh S and
Munn NJ: Venovenous extracorporeal membrane oxygenation therapy in
adults. Cureus. 11(e5365)2019.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Squiers JJ, Lima B and Dimaio JM:
Contemporary extracorporeal membrane oxygenation therapy in adults:
Fundamental principles and systematic review of the evidence. J
Thorac Cardiovasc Surg. 152:20–32. 2016.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Lee OJ, Cho YH, Hwang J, Yoon I, Kim YH
and Cho J: Long-term extracorporeal membrane oxygenation after
severe blunt traumatic lung injury in a child. Acute Crit Care.
34:223–227. 2019.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Bosarge PL, Raff LA, McGwin G Jr, Carroll
SL, Bellot SC, Diaz-Guzman E and Kerby JD: Early initiation of
extracorporeal membrane oxygenation improves survival in adult
trauma patients with severe adult respiratory distress syndrome. J
Trauma Acute Care Surg. 81:236–243. 2016.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Zhang LY, Qin CN, Zhang Q, Liu XD, Tian RB
and Hei FL: The Application of Extracorporeal Membrane Oxygenation
in the Treatment of Lung Injury. J Chin Extracorpor Cardiocirc.
18:328–332. 2020.(In Chinese).
|
|
13
|
Aprile V, Korasidis S, Ambrogi MC and
Lucchi M: Extracorporeal membrane oxygenation in traumatic tracheal
injuries: A bold life-saving option. J Thorac Dis. 11:2660–2663.
2019.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Abouarab AA, Elsayed HH, Elkhayat H,
Mostafa A, Cleveland DC and Nori AE: Current solutions for
long-segment tracheal reconstruction. Ann Thorac Cardiovasc Surg.
23:66–75. 2017.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Ahmed N, Naseem K and Rafiq M: Anesthetic
challenges in tracheal resection and reconstruction surgery.
Anaesth Pain Intensi. 22:323–329. 2018.
|
|
16
|
Wanat-Hawthorne A, Stubblefield J, Lynch
I, Dellaria S and Kernstine K: Successful use of a double lumen
endotracheal tube and bronchial blocker for lung isolation in
pulmonary mucormycosis. J Cardiothorac Vasc Anesth. 33:776–780.
2019.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Carretta A, Ciriaco P, Bandiera A, Muriana
P, Pappalardo F, Broman LM, Montisci A and Negri G: Veno-venous
extracorporeal membrane oxygenation in the surgical management of
post-traumatic intrathoracic tracheal transection. J Thorac Dis.
10:7045–7051. 2018.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Wu MY, Chou PL, Wu TI and Lin PJ:
Predictors of hospital mortality in adult trauma patients receiving
extracorporeal membrane oxygenation for advanced life support: A
retrospective cohort study. Scand J Trauma Resusc Emerg Med.
26(14)2018.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Zhang Y, Deng L, Feng XL, Li Y, Song ML,
Wang Y, Chang L and Zhou P: Analysis of different anticoagulation
strategies and complications in extracorporeal membrane oxygenation
therapy. Chin J Critical Care Med. 41:630–634. 2021.(In
Chinese).
|
|
20
|
Yu HJ, Zhu XY, Xu XQ and Cao WZ:
Resuscitation of Severe Pulmonary Contusion with Hemoptysis by
Heparin-free Anticoagulation Extracorporeal Membrane Oxygenation.
Chin J Emerg Med. 29:1480–1482. 2020.(In Chinese).
|
|
21
|
Cheng J, Shi JY, Sun P, Zhu H, Li XO and
Liu D: Application of extracorporeal membrane oxygenation in
bronchoscopic interventional surgery for patients with severe
airway stenosis and literature review. Chin J Respir Crit Care Med.
21:498–504. 2022.(In Chinese).
|
|
22
|
Robba C, Galimberti S, Graziano F, Wiegers
EJA, Lingsma HF, Iaquaniello C, Stocchetti N, Menon D and Citerio
G: CENTER-TBI ICU Participants and Investigators. Tracheostomy
practice and timing in traumatic brain-injured patients: A
CENTER-TBI study. Intensive Care Med. 46:983–994. 2020.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Tsuchiya A, Yamana H, Kawahara T, Tsutsumi
Y, Matsui H, Fushimi K and Yasunaga H: Tracheostomy and mortality
in patients with severe burns: A nationwide observational study.
Burns. 44:1954–1961. 2018.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Zhang B, Li GK, Wang YR, Wu F, Shi SQ,
Feng QL, Hang X, Miao RF, Xia L, Duan C, et al: Analysis of timing
and prognostic factors of early tracheotomy in patients with
multiple rib fractures. Chin J Trauma. 37:646–652. 2021.(In
Chinese).
|