Introduction
It is well known and proven by a number of studies
over the last 60 years, that the primary etiologic factor in
periodontal disease is the oral bacterial plaque (1-4).
Other factors such as smoking, diabetes, vicious habits (bruxism
and occlusal trauma), dentoalveolar incongruity, including some
drugs such as antiepileptic and some antihypertensive (as calcium
channel blockers) medication are considered as additional risk
factors, some with higher pathological influence than others.
The physio-pathological mechanism of calcium channel
blockers-influenced gingival overgrowth involves an association
between the decrease in the catabolic events (derived from
decreasing of cation influx and folic acid transport within the
fibroblasts in the gingiva) and the increase in the anabolic events
in the gingiva (triggered by increased synthesis of keratinocyte
growth factor by fibroblasts and decreased aldosterone), which end
up in the accumulation of collagen and ground substance (4,5).
However, no matter which one of these proposed mechanisms is
considered, all studies show direct involvement of the dental
plaque, as a sine qua non factor, in the process (4,5). The
inflammatory and non-inflammatory mechanisms underlying this type
of drug-influenced gingival growth impede different stages of the
disease.
In these patients, there is also a vicious circle
effect: The gingival overgrowth promotes dental plaque retention on
increased gingival surfaces, and concurrently, the development of
false periodontal pockets provide favorable conditions for the
formation of the higher pathogenic anaerobic flora (6). Of course, the poorly marginally
adapted prosthodontics play also an important role in excessive
plaque retention and act as irritating spikes for the already
inflamed gingiva.
In the great majority of these patients, other
favoring factors coexist, thus creating the full picture of a true
periodontal disease: Smoking, diabetes, and, most important and
most often, the poor home management of dental hygiene.
Consequently, the treatment of these patients should
begin with the thorough removal of the bacterial plaque and the
favorable factors that can be removed (re-education of the patient
about oral hygiene and removal of fixed prosthetic works or
marginally unsuited restorations).
At present, there are new generation methods, more
efficient and less invasive, available both for bacterial
decontamination and surgical excision part: For decontamination
there is mechanical decontamination according to the guided biofilm
therapy (GBT) protocol (7,8) (including patient
re-education/motivation) and laser decontamination; laser-assisted
nonsurgical periodontal pocket therapy at 980 nm (9-14).
For the surgical excision of the overgrown gingiva, the use of a
450-nm laser is the most efficient and least invasive method
(minimum tissue necrosis in depth) (15-17),
with the fastest and most comfortable healing for the patient and
with the lowest recurrence rate (18-25).
Case report
Patient
Regarding the clinical case presented below, a
patient was chosen with gingival hyperplasia influenced by calcium
channel blockers, with no other risk factors except higher plaque
retention caused by fixed prosthodontics with poor marginal
adaptation and the inconsistent oral hygiene technique of the
patient.
A 71-year-old male, non-smoking, non-alcoholic, with
a medical history of atrial fibrillation, angina pectoralis and
high blood pressure, under treatment with nifedipine 40 mg per day,
for the last 6 months, attended the dental office complaining of
pain, bleeding when touched and during mastication, and
aesthetically disturbing overgrowth gingiva.
Prior to enrollment, the patient signed the written
informed consent and the study was conducted in accordance with the
principles of the Declaration of Helsinki. The ethical committee of
the Titu Maiorescu University of Bucharest approved the research
(approval no. 23/2023).
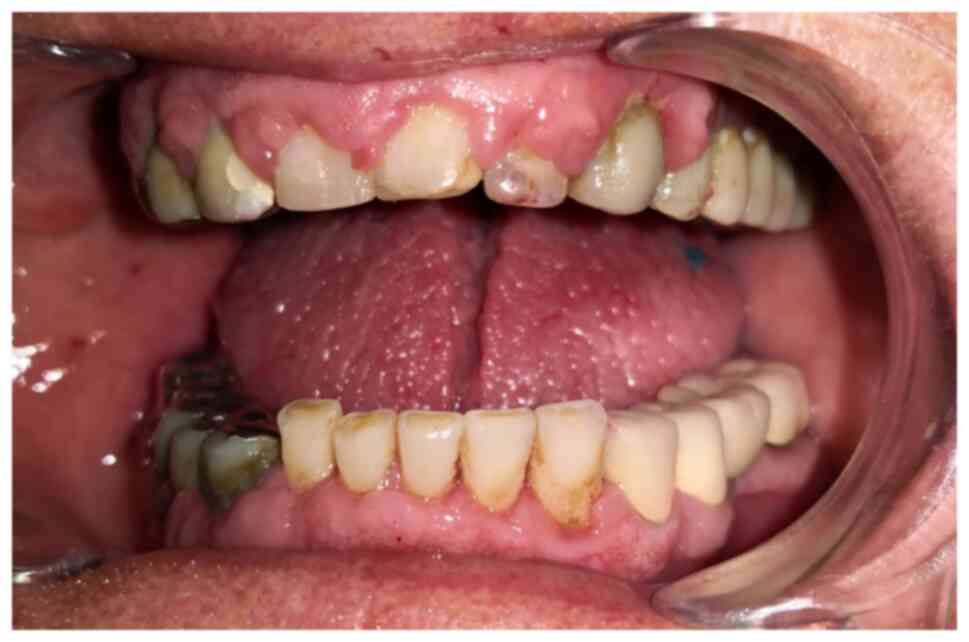
At the initial intraoral examination (Fig. 1), gingival overgrowth,
inflammation, and bleeding lesions were present, surrounding all
teeth, accentuated on the buccal side and in the gingiva in contact
with old prosthodontics.
Prior to beginning of any treatment, anamnesis,
clinical and para-clinical examinations (blood tests, radiological
examination and histopathological examination) any tumoral etiology
of the gingival growth, as well as other diseases in patient
personal medical history that might lead to or represent other risk
factors for the periodontal disease were excluded.
Following discussion with the attending
cardiologist, the calcium channel blockers medication was
substituted with another class of antihypertensive drugs. The
treatment involved the thorough removal of the bacterial plaque, as
described below, and the removal of risk factors that could be
removed: Re-education of the patient concerning oral hygiene (also
as a part of the GBT protocol) and removal of fixed prosthetic
works and marginally unsuitable restorations.
Periodontal treatment
The treatment itself was multimodal and involved two
stages.
First stage: The thorough mechanical
removal of bacterial plaque using the GBT protocol (7,8)
The procedure involved the following in-clinic
procedures: Air-flow, deep scaling and root decontamination in four
quadrants according to GBT, associated with 980-nm diode laser
decontamination and laser-assisted nonsurgical periodontal pocket
therapy, following the recommendations of several authors (11-14)
(Figs. 2 and 3) followed by the at-home correction of
oral hygiene and a two weeks period of use of chlorhexidine
gluconate (0.12%) mouthwash
In this case, the protocol for laser decontamination
included the use of a 980-nm continuous wave (CW) 0.9 watts power
laser. The device used was a medical diode laser (PIOON S3)
manufactured by Wuhan Pioon Technology Co, Ltd. The procedure
involved inserting a 300 um diameter fiber with a non-activated tip
1 mm coronary from the gingival insertion and performing sweeping,
inward-outward movements parallel to the tooth axis in contact with
the sulcular epithelium and the root for no longer than 20 sec per
site (periodontal pocket). This protocol involved all gingival
sulcus and periodontal pockets and was performed three times in one
month (day 1, 1 week later and 3 weeks from day 1).
Second stage. The second stage was the
surgical one to remove gingival hyperplasia. In the case of
patients with gingival overgrowth influenced by calcium channel
blockers, the hyperplasia is always associated with inflammation,
vasculopathy and coagulation problems (some induced even by the
associated medication) which leads to significant gingival
bleeding, especially when an attempt is made to excise hyperplasia
through a classic surgical technique with the bistoury (19,24).
This is why an excision was needed that involved, at the same time,
hemostasis. Between a classic excision technique with
electrocautery hemostasis and the laser excision technique, the
latter was chosen due to the effects of laser excision: A smaller
area of intra-tissue necrosis, less pain and inflammation
post-excision and lower risk of recurrence. Among the wavelengths
generally used for surgery, the 450-nm laser was chosen, rather
than the 980-nm laser, due to the smaller area of carbonization of
the cut tissues, as well as the speed of the technique, as
recommended by other authors (15-17,24).
For the working protocol, surgical excision of
gingival hyperplasia was performed under local anesthesia, using
the 450-nm diode laser, with 400 um fiber diameter with the
following protocol: 1.5 W CW, activated fiber tip with contact or
without contact, non-activated fiber tip at 1 mm distance from
tissue; metronidazole 5 g/l solution wash,
tetracycline-metronidazole gingival ointment application (Fig. 4).
The clinical aspect after performing laser
decontamination and GBT decontamination protocol is presented in
Fig. 5. The clinical outcomes
after treatment in the 1st and 4th quadrants are presented in
Fig. 6. The patient was instructed
to use local mouthwash and application of gel containing 0.2%
chlorhexidine.
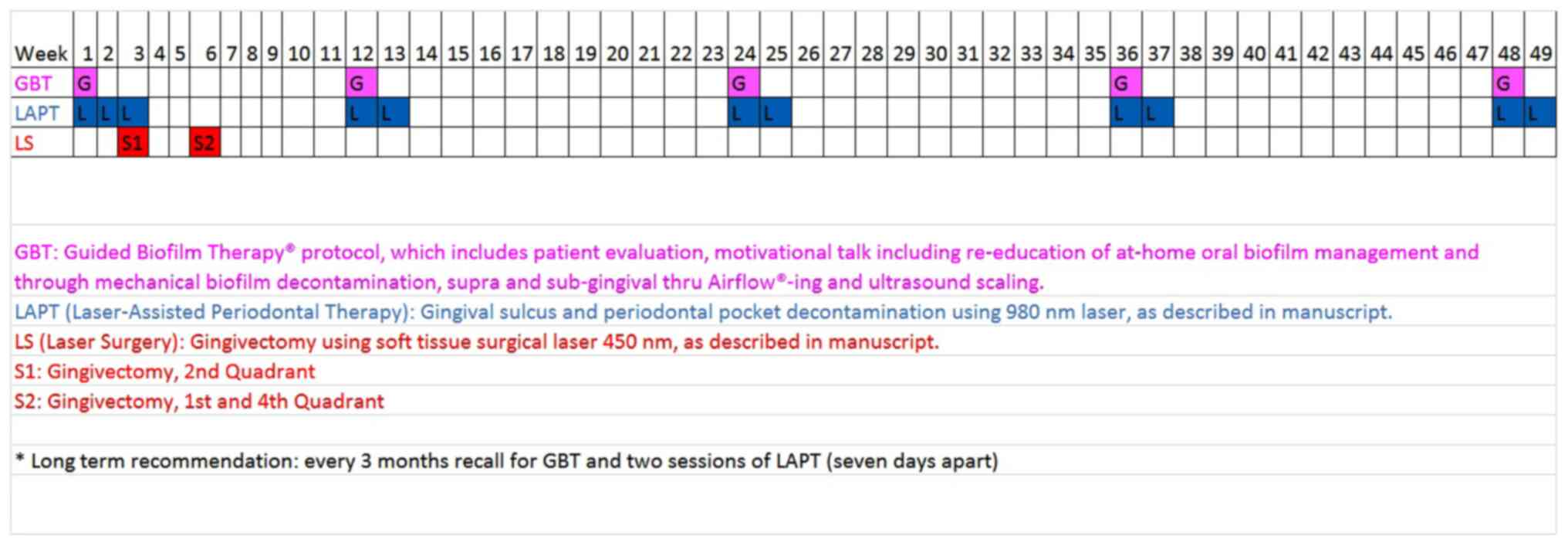
The treatment plan included recall for bacterial
decontamination using GBT protocol and laser decontamination and
biostimulation (two sessions 1 week apart) every 3 months. The
treatment plan chart is presented in Fig. 7.
The clinical aspect after 1 year (48 weeks) is
presented in Fig. 8. The remission
of gingival expansion was noted, with the gingiva displaying a pink
color, firm consistency, uniform borders and a healthy-looking
appearance.
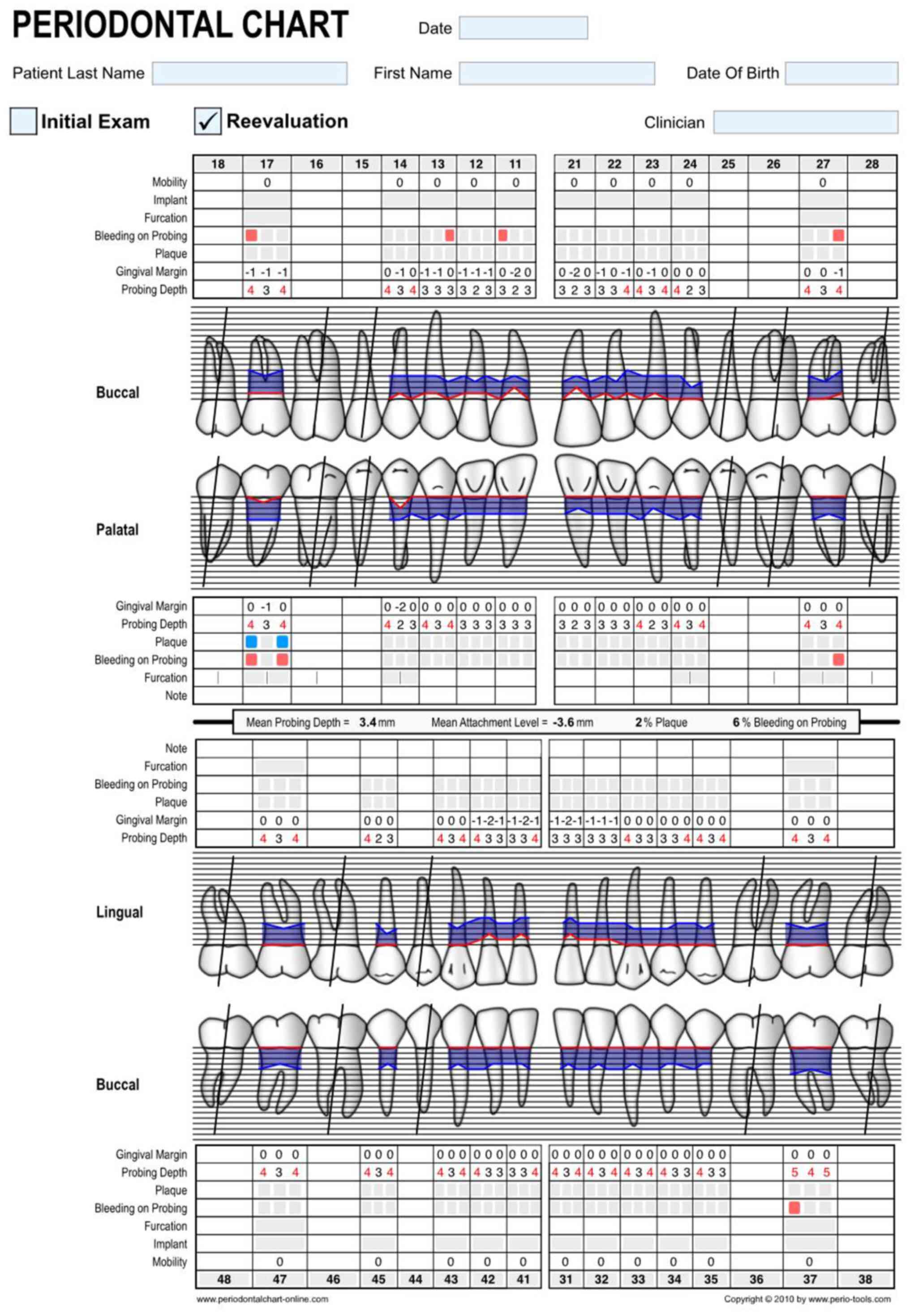
The periodontal chart of the patient is presented in
Fig. 9, initially and after
6-month and 1-year re-evaluations (Figs. 10 and 11). The model of periodontal chart used
was provided by (26).
Discussion
The first literature mention on the gingival
overgrowth induced by calcium channel blockers dates from 1984 when
Ramon et al (27) reported
a case series of five cases. The main risk factors for the extent
and severity of this disease are the drug variable, such as plasma
concentration of nifedipine, concomitant medication and the
periodontal status (presence of gingival inflammation and/or
plaque) (28). The mechanism of
drug segregation in the gingiva remains to be elucidated (29). A review article analyzed 293
publications of case reports and case series and found no
significant differences in the severity of lesions with different
doses (27). The treatment
modalities vary for each case and include changes of drug and
improved oral hygiene (30). In
addition, the diode laser at the wavelength of 445 nm blue light
showed improvement in a case-report on gingival growth due to
amlodipine intake (31).
The patient reported in the present article,
diagnosed with gingival overgrowth induced by nifedipine, was
referred to his cardiologist for analyzing the possibility of
changing the antihypertensive treatment. The thorough removal of
bacterial plaque in the dental clinic and a correct hygiene
protocol at home are essential in the positive evolution of all
periodontal diseases, including calcium channel blockers-influenced
gingival enlargement.
The removal of factors favoring the retention of
bacterial plaque (prosthetic works or marginally unfitted fillings)
plays an essential role. Using the laser for bacterial
decontamination is a valuable aid.
In the case of excision of gingival hyperplasia
induced by calcium channel blockers, the use of the 450-nm laser is
the least invasive method (minimum tissue necrosis in depth), with
the fastest and most comfortable healing for the patient and the
lowest recurrence rate.
The current report case limitations arise from the
lack of ability to broadly apply the findings and the decision to
publish a case with positive outcomes without balancing it with an
unsuccessful one.
The dentist, the periodontologist and the patient
all play important roles in gingival health. The clinical approach
of the presented case included mechanical decontamination according
to (GBT) protocol, laser decontamination (laser-assisted
nonsurgical periodontal pocket therapy) and 980-nm and 450-nm laser
surgical excision. At 12 months there were positive, stable
results, with an improvement in gingival status (no gingival
overgrowth in the area where all risk factors were eliminated and
minimal overgrowth in the area where old poorly marginally adapted
prosthodontics were kept in place and no/minimal signs of gingival
inflammation).
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
Conceptualization was by LM and IP. Methodology was
by AC and AB. Resources were the responsibility of AC and AB. Data
curation was by IP. LM and AC confirm the authenticity of all the
raw data. Writing of the original draft was by LM. Writing, review
and editing were performed by LM, AB and AC. Visualization was
performed by IP. Supervision and project administration were by LM.
All authors read and approved the final manuscript.
Ethics approval and consent to
participate
The present study was approved by the Ethical
Committee of the Titu Maiorescu University of Bucharest (approval
no. 23/2023).
Patient consent for publication
Written informed consent was obtained from the
patient.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Caton JG, Armitage G, Berglundh T, Chapple
ILC, Jepsen S, Kornman KS, Mealey BL, Papapanou PN, Sanz M and
Tonetti MS: A new classification scheme for periodontal and
peri-implant diseases and conditions-Introduction and key changes
from the 1999 classification. J Periodontol. 89 (Suppl 1):S1–S8.
2018.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Socransky SS: Relationship of bacteria to
the etiology of periodontal disease. J Dent Res. 49:203–222.
1970.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Angulo RS and Torre ACL: Gingival
enlargement resolution by means of non-surgical periodontal
therapy: Case report. Revista Odontológica Mexicana. 20:e246–e251.
2016.
|
|
4
|
Brown RS and Arany PR: Mechanism of
drug-induced gingival overgrowth revisited: A unifying hypothesis.
Oral Dis. 21:e51–61. 2015.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Tonsekar P and Tonsekar V:
Calcium-channel-blocker-influenced gingival enlargement: A
conundrum demystified. Oral. 1:236–249. 2021.
|
|
6
|
Devi P and Biradar B: Plaque Biofilm. In:
Gingival Diseases-Their Aetiology, Prevention and Treatment.
Panagakos FS and Davies RM (eds). InTech, 2011.
|
|
7
|
Donnet M, Fournier M, Schmidlin P and
Lussi A: A novel method shaping the future of oral hygiene.
Research Outreach, Stonehouse, 2022.
|
|
8
|
Bastendorf KD and Strafela-Bastendorf N:
Outcomes of clinical protocol - PZR, UPT, GBT. Quintessenz
Zahnmedizin. 71:1380–1389. 2020.(In German).
|
|
9
|
Ladiz MAR, Mirzaei A, Hendi SS,
Najafi-Vosough R, Hooshyarfard A and Gholami L: Effect of
photobiomodulation with 810 and 940 nm diode lasers on human
gingival fibroblasts. Dent Med Probl. 57:369–376. 2020.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Liu J, Wang X, Xue F, Zheng M and Luan Q:
Abnormal mitochondrial structure and function are retained in
gingival tissues and human gingival fibroblasts from patients with
chronic periodontitis. J Periodontal Res. 57:94–103.
2022.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Zhao P, Song X and Wang Q, Zhang P, Nie L,
Ding Y and Wang Q: Effect of adjunctive diode laser in the
non-surgical periodontal treatment in patients with diabetes
mellitus: A systematic review and meta-analysis. Lasers Med Sci.
36:939–950. 2021.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Lin Z, Strauss FJ, Lang NP, Sculean A,
Salvi GE and Stähli A: Efficacy of laser monotherapy or
non-surgical mechanical instrumentation in the management of
untreated periodontitis patients. A systematic review and
meta-analysis. Clin Oral Investig. 25:375–391. 2021.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Salvi GE, Stähli A, Schmidt JC, Ramseier
CA, Sculean A and Walter C: Adjunctive laser or antimicrobial
photodynamic therapy to non-surgical mechanical instrumentation in
patients with untreated periodontitis: A systematic review and
meta-analysis. J Clin Periodontol. 47 (Suppl 22):176–198.
2020.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Nammour S, El Mobadder M, Maalouf E,
Namour M, Namour A, Rey G, Matamba P, Matys J, Zeinoun T and
Grzech-Leśniak K: Clinical evaluation of diode (980 nm)
laser-assisted nonsurgical periodontal pocket therapy: A randomized
comparative clinical trial and bacteriological study. Photobiomodul
Photomed Laser Surg. 39:10–22. 2021.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Hanke A, Fimmers R, Frentzen M and Meister
J: Quantitative determination of cut efficiency during soft tissue
surgery using diode lasers in the wavelength range between 400 and
1,500 nm. Lasers Med Sci. 36:1633–1647. 2021.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Lazon Medical Laser: Advantages of 450nm
Blue Dental Diode Laser. https://www.lazonlaser.com/news/industry/20210816/1659.html.
Accessed February 17, 2023.
|
|
17
|
Palaia G, Pergolini D, D'Alessandro L,
Carletti R, Del Vecchio A, Tenore G, Di Gioia CRT and Romeo U:
Histological effects of an innovative 445 nm blue laser during oral
soft tissue biopsy. Int J Environ Res Public Health.
17(2651)2020.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Jiang DL, Yang Z, Liu GX, Wu K, Fan J, Wu
D, Li L, Wang X, Guo P, Mu L and He D: A novel 450-nm blue laser
system for surgical applications: Efficacy of specific laser-tissue
interactions in bladder soft tissue. Lasers Med Sci. 34:807–813.
2019.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Liu G, Jiang D, Ren M, Lu X, Chang Y, He
S, Ren Z, Fan H, Wu K and He D: High-power 450 nm blue diode laser
for endoscopic mucosal resection/endoscopic submucosal dissection
in the stomach: Preliminary results on a porcine model with a
modified flexible endoscope. Lasers Surg Med. 54:1002–1009.
2022.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Fornaini C, Fekrazad R, Rocca JP, Zhang S
and Merigo E: Use of blue and blue-violet lasers in dentistry: A
narrative review. J Lasers Med Sci. 12(e31)2021.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Fornaini C, Merigo E, Rocca JP, Lagori G,
Raybaud H, Selleri S and Cucinotta A: 450 nm blue laser and oral
surgery: Preliminary ex vivo study. J Contemp Dent Pract.
17:795–800. 2016.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Fornaini C, Rocca JP and Merigo E: 450 nm
diode laser: A new help in oral surgery. World J Clin Cases.
4:253–257. 2016.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Frentzen M, Kraus D, Reichelt J, Engelbach
C, Dehn C and Meister J: A novel blue light diode laser (445 nm)
for dental application Biomedical testing and clinical aspects.
laser, 2016. https://epaper.zwp-online.info/epaper/5105/export-article/6.
|
|
24
|
Amaral MB, de Ávila JM, Abreu MH and
Mesquita RA: Diode laser surgery versus scalpel surgery in the
treatment of fibrous hyperplasia: A randomized clinical trial. Int
J Oral Maxillofac Surg. 44:1383–1389. 2015.PubMed/NCBI View Article : Google Scholar
|
|
25
|
de Jesus AO, Matias MDP, de Arruda JAA,
Aires AV, Gomes IP, Souza LN, Abreu LG and Mesquita RA: Diode laser
surgery versus electrocautery in the treatment of inflammatory
fibrous hyperplasia: A randomized double-blind clinical trial. Clin
Oral Investig. 24:4325–4334. 2020.PubMed/NCBI View Article : Google Scholar
|
|
26
|
University Of Bern, Switzerland [Online].
2023 [accessed 2023 Feb 17]. Available from: https://www.periodontalchart-online.com/uk/.
|
|
27
|
Ramon Y, Behar S, Kishon Y and Engelberg
IS: Gingival hyperplasia caused by nifedipine-a preliminary report.
Int J Cardiol. 5:195–206. 1984.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Seymour RA, Ellis JS and Thomason JM: Risk
factors for drug-induced gingival overgrowth. J Clin Periodontol.
27:217–223. 2000.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Damdoum M, Varma SR, Nambiar M and
Venugopal A: Calcium channel blockers induced gingival overgrowth:
A comprehensive review from a dental perspective. J Int Soc Prev
Community Dent. 12:309–322. 2022.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Samudrala P, Chava VK, Chandana TS and
Suresh R: Drug-induced gingival overgrowth: A critical insight into
case reports from over two decades. J Indian Soc Periodontol.
20:496–502. 2016.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Okumuş ÖF: Treatment of gingival growth
due to amlodipine use with a 445-nm diode laser: A case report.
Cureus. 14(e32592)2022.PubMed/NCBI View Article : Google Scholar
|