Introduction
Degenerative lumbar diseases are caused by
degenerative changes in the lumbar spine and the surrounding
tissues. The older the patient, the more prone they are to changes
in the lumbar spine structure, causing back pain, spinal
dysfunction and other symptoms (1). With the accelerated aging of the
Chinese population, the proportion of diagnoses and treatments for
lumbar degeneration is increasing and the proportion of lumbar
spine surgeries is also increasing annually. Transforaminal lumbar
interbody fusion (TLIF) combined with pedicle screw internal
fixation is a therapeutic option for patients in whom conservative
treatment has failed (2). In
lumbar spine surgery, the pedicle screw internal fixation technique
can provide fixation of the anterior, middle and posterior columns
of the spine in various lumbar fusion procedures and has been
widely used in the surgical treatment of various lumbar spine
disorders to promote fusion and restore spinal stability. Since
Boucher (3) applied the pedicle
screw technique in 1959, it has become the standard internal
fixation method for the treatment of spinal fractures, degenerative
and infectious spinal lesions and spinal deformities. For patients
with osteoporosis, cemented reinforcement or cortical bone screws
can be used, while for those with cervical osteoporosis or
infection, anterior cervical bilateral pedicle screws can be used
to enhance stability (4,5). The open TLIF technique was first
introduced by Harms and Rolinger in 1982(6) and has been used since. After >40
years, TLIF has become one of the most commonly used surgical
procedures for lumbar degenerative diseases. Conventional TLIF uses
an intervertebral foraminal approach located on the lateral aspect
of the articular eminence, enabling stable intervertebral fusion
and effectively reducing the loss of pressure on the neural tissues
without the need to enter the spinal canal. This approach can
reduce the damage to the spinal dura mater and nerves and has the
advantages of easy operation, less trauma and quicker recovery
(7). However, extensive stripping
of the paravertebral muscles and prolonged pulling may lead to
muscle damage, resulting in medically induced muscle injury and
chronic postoperative low back pain (8). With the development of minimally
invasive concepts and channel technologies, endoscopic technology
and robot-assisted surgery have become a current research focus.
The minimally invasive TLIF (MIS-TLIF) is precisely used to solve
the shortcomings of open TLIF, effectively protecting the
attachment of paraspinal muscles to the bone and avoiding
interruption of the supraspinous and interspinous ligaments, thus
reducing bleeding and postoperative pain. MIS-TLIF, a minimally
invasive spinal technique introduced by Foley and Lefkowitz in the
early 2000s (9), has been widely
used in clinical practice. Common indications for MIS-TLIF and open
TLIF include severe degenerative disc disease, low-grade
spondylolisthesis (grades 1 and 2), pseudarthrosis and symptomatic
spondylolisthesis. Whereas recurrent disc herniation and obese
patients are more suited for MIS-TLIF, high-grade vertebral slips
(grades 3 and 4) and anatomical variations are more suited for open
TLIF and contraindications include extensive epidural scarring,
arachnoiditis, active infections, linking of the nerve roots (which
may impede access to the intervertebral disc space) and
osteoporosis in patients (10-12).
Studies have shown that, concerning single-stage surgery, MIS-TLIF
reduces intraoperative blood loss, shortens hospitalization and
recovery times, reduces complications and has the same clinical
outcomes and fusion rates as open TLIF (13,14).
However, for multi-segmental lumbar degenerative disease, it
remains unclear whether MIS-TLIF still has the advantage of a
single-stage surgery. Therefore, the present meta-analysis aimed to
explore the similarities and differences between single-stage and
multi-segmental treatments by comparing and evaluating the efficacy
of MIS-TLIF and open TLIF in treating multi-segmental lumbar
degenerative disease.
Materials and methods
Search strategy
The PubMed, Web of Science, Embase, CNKI, Wanfang
and VIP databases were searched to identify relevant studies for
inclusion. Data on the effectiveness and security of open TLIF and
MIS-TLIF for treating lumbar degenerative disorders were collected
from the inception of the databases to August 2023. The search
keywords used were TLIF, MIS-TLIF and lumbar degenerative diseases.
The retrieval strategy was (‘MIS-TLIF’ OR ‘minimally invasive
transforaminal lumbar interbody fusion’ OR ‘TLIF’ OR
‘transforaminal lumbar interbody fusion’) AND (‘degenerative
disease of the lumbar spine’).
Surgical techniques
MIS-TLIF: The patient was placed in the prone
position and the C-arm was used to determine the surgical plane
preoperatively. A longitudinal incision was made 5-10 mm outside
the upper and lower pedicles on the symptomatic side. The
latissimus dorsi fascia was incised and the space between the
longest and multifidus muscles (Wiltse approach) was separated from
the fingers. The muscles around the facet joints were bluntly
separated and a guide needle was placed. A stepwise sleeve was
placed to remove the upper and lower joints of the affected
intervertebral space and part of the lamina near the spinous
process. The intervertebral foramen was exposed, the annulus
fibrosus was incised, the nucleus pulposus was removed and the
endplate was cleaned. The cage was implanted according to the test
model and the bone particles made from the bone block were
implanted and compacted. The nerve root was explored and released;
no residual pressure or nerve root relaxation was observed. The
same decompression and intervertebral bone grafting methods were
performed on other segments. Finally, a titanium rod was installed
to connect the pedicle screws and a drainage tube was placed in the
incision.
TLIF: After general anesthesia, the patient was
placed in the prone position and the C-arm was used to locate the
surface projection of the fused segment's upper and lower vertebral
pedicles. According to the position of the upper and lower pedicles
of the fused segment, the median longitudinal incision was made,
the skin and lumbar fascia were cut, the paravertebral muscles on
both sides were separated, the bone structure behind the lamina was
fully exposed, the articular capsule of the upper and lower
non-fusion segments was not destroyed and pedicle screws were
placed. Decompression and intervertebral bone grafting were the
same as those used for MIS-TLIF. Titanium rods were installed,
pressurized and tightened and negative-pressure drainage tubes were
placed on both sides of the lamina.
Inclusion and exclusion criteria
The inclusion criteria were: i) Patients who
underwent open TLIF or MIS-TLIF for degenerative lumbar spine
disease; ii) two or more surgical segments; and iii) one of the
following reported in the literature: Operative time,
intraoperative blood loss, postoperative drainage volume, number of
intraoperative radiographs, bed rest time, hospital stay,
complications, fusion rate, Oswestry Disability Index (ODI) and
Visual Analog Scale (VAS) score (15-24).
The exclusion criteria were: i) Comorbidities, such as lumbar
infections, neoplastic diseases, or lumbar fractures; ii) history
of previous lumbar spine surgeries; iii) reviewed manuscripts,
conference papers, expert opinions, case reports and literature not
obtained in full text; and iv) animal experiments and biomechanical
studies.
Data extraction and literature quality
assessment
Articles were independently screened and identified
for study inclusion by two researchers through the title, abstract
and full text of the article. When there was a difference in
opinion regarding the study, it was discussed and resolved by two
authors. When necessary, a third researcher was consulted. The
quality of the included literature was assessed using the
Newcastle-Ottawa Scale (NOS) (25)
and categorized as low (<5 points), moderate (5-7 points) and
high (8-9 points) quality.
Statistical methods
Review Manager 5.4 (The Cochrane Collaboration) was
used to process the collected data. Continuous variables were
expressed as mean difference and 95% confidence interval (CI) and
dichotomous variables were expressed as odds ratios and 95%CI. The
heterogeneity of the included literature was determined using the
I2 statistic, with I2<50%
considered homogeneous studies with less heterogeneity using a
fixed-effects model and vice versa using a random-effects model.
The literature was removed individually to perform a sensitivity
analysis. When the number of included studies was ≥10, a funnel
plot or Egger's (Egger's test) test was used to assess for
publication bias. P<0.05 was considered to indicate a
statistically significant difference.
Results
Basic characteristics of the included
literature
In total, 1,608 relevant studies were obtained from
the databases based on the search formula and 168 relevant studies
were initially screened after excluding non-case controls,
duplicates and other irrelevant studies. Finally, the articles were
scrutinized; 158 papers with irrelevant content, inconsistent
outcome indicators and incomplete critical data were excluded and
10 articles were finally included. The literature screening process
and results are shown in Fig. 1
and the basic characteristics of the included studies are listed in
Table I.
 | Table IGeneral characteristics of included
studies. |
Table I
General characteristics of included
studies.
| First author(s).
year | Type of study | Country |
MIS-TLIF/OpenTLIF | Cases | Age (mean) | Sex (M/F) | Outcome | NOS scale | (Refs.) |
|---|
| Cao et al,
2022 | Retrospective | China | MIS-TLIF | 64 | 61.80±8.83 | 30/34 | ①②③⑤ | 6 | (15) |
| | | | OpenTLIF | 62 | 60.96±8.48 | 28/34 | ⑥⑨⑩ | | |
| Du et al,
2017 | Retrospective | China | MIS-TLIF | 16 | 47.62±13.57 | 5/8 | ①②⑥⑦⑨ | 6 | (16) |
| | | | OpenTLIF | 16 | 54.38±10.53 | 5/8 | | | |
| Gu et al,
2014 | Prospective | China | MIS-TLIF | 44 | 66.4±6.7 | 19/25 | ①②⑥⑦⑧ | 8 | (17) |
| | | | OpenTLIF | 38 | 64.1±7.8 | 15/23 | ⑨⑩ | | |
| Hu et al,
2022 | Retrospective | China | MIS-TLIF | 52 | 64.18±8.17 | 28/24 | ①②③④⑤⑦ | 8 | (18) |
| | | | OpenTLIF | 60 | 66.24±7.16 | 34/26 | ⑧⑨⑩ | | |
| Lee et al,
2015 | Retrospective | Korea | MIS-TLIF | 27 | 60.55±13.61 | 8/19 | ①②⑥⑦⑧⑨ | 7 | (19) |
| | | | OpenTLIF | 43 | 65.06±6.81 | 16/27 | | | |
| Modi et al,
2021 | Retrospective | India | MIS-TLIF | 24 | 51.2±12.2 | NA | ①②⑥ | 6 | (20) |
| | | | OpenTLIF | 42 | 51.5±14.0 | NA | | | |
| Wang et al,
2019 | Retrospective | China | MIS-TLIF | 67 | 64.77±7.07 | 33/34 | ①②③⑤⑥⑦ | 7 | (21) |
| | | | OpenTLIF | 59 | 64.92±6.74 | 25/34 | ⑧⑨⑩ | | |
| Wang et al,
2021 | Retrospective | China | MIS-TLIF | 32 | 63.3±11.3 | 15/17 | ⑦⑧⑨⑩ | 7 | (22) |
| | | | OpenTLIF | 30 | 66.0±8.4 | 13/17 | | | |
| Wang et al,
2022 | Retrospective | China | MIS-TLIF | 51 | 64.67±6.17 | 28/23 | ①②③④⑤⑥ | 8 | (23) |
| | | | OpenTLIF | 55 | 64.35±5.62 | 32/23 | ⑦⑨ | | |
| Zhang et al,
2022 | Retrospective | China | MIS-TLIF | 45 | 59.9±6.9 | 25/20 | ①②⑦⑧⑨ | 7 | (24) |
| | | | OpenTLIF | 37 | 61.8±5.6 | 21/16 | | | |
Quality assessment of included
articles
The present study included 10 articles, including
zero randomized controlled studies, one prospective study and nine
retrospective studies. A total of 864 patients were included: 422
underwent MIS-TLIF and 442 underwent open TLIF. The NOS score table
was used for quality evaluation, including three, four and three
studies with eight, seven and six points, respectively; three
high-quality and seven medium-quality studies. A total of nine
studies reported the operation time and intraoperative drainage;
however, one article did not report perioperative data because of
long-term efficacy. Among them, seven articles involved 2-segment
lumbar fusion and two included 2- or 3-segment lumbar fusion.
Outcomes. Perioperative
indicators
Perioperative indicators included operation time,
blood loss, postoperative drainage volume and fluoroscopy
frequency. A total of nine studies compared the time spent
performing MIS-TLIF with open TLIF during multi-segmental surgery.
The heterogeneity test showed that the heterogeneity of each study
was significant (I2=97%) and a random-effects
model was used for analysis. The results showed no significant
difference in operation time between MIS-TLIF and open TLIF in the
treatment of multi-segment lumbar degenerative diseases and the
difference was not statistically significant (95%CI: -26.92,20.03;
P=0.77; Fig. 2). A total of nine
studies compared intraoperative blood loss; the heterogeneity test
showed significant heterogeneity (I2=92%) and
continued to use the random effect model, demonstrating that the
intraoperative blood loss was considerably lower in the MIS-TLIF
group compared with the open TLIF group (95%CI: -254.33,-157.86;
P<0.00001; Fig. 3). A total of
four studies compared the postoperative drainage volume and the
heterogeneity test showed significant heterogeneity in each study
(I2=99%); therefore, the random-effects model was
used. The results showed no significant difference in postoperative
drainage between the MIS-TLIF and open TLIF surgery groups (95%CI:
-259.91,8.58; P=0.07; Fig. 4).
Only two articles compared the frequency of fluoroscopy; the
heterogeneity of the two studies was apparent
(I2=92%) and the random-effects model was used.
The results showed that the fluoroscopy frequency in the MIS-TLIF
group was significantly higher than that in the open TLIF group and
the difference was statistically significant (95%CI: 2.07,6.12;
P<0.0001; Fig. 5). The results
showed that in the perioperative indices of multi-segment lumbar
spine surgery, the bleeding in the MIS-TLIF group was less than
that in the open TLIF group, while the number of radiations was
higher than that in the open group and the difference was
statistically significant; the operative time and postoperative
drainage did not differ significantly.
Postoperative bedtime and hospitalization
time. A total of four studies compared postoperative bedtime
and the heterogeneity test showed I2=78%. After
sensitivity analysis, one study was excluded; the heterogeneity
test result was I2=0% and the fixed-effects model
was used. The results suggested a statistically significant
difference between the postoperative bed rest times in the MIS-TLIF
and open TLIF surgery groups (95%CI: -3.49,-2.76; P<0.00001;
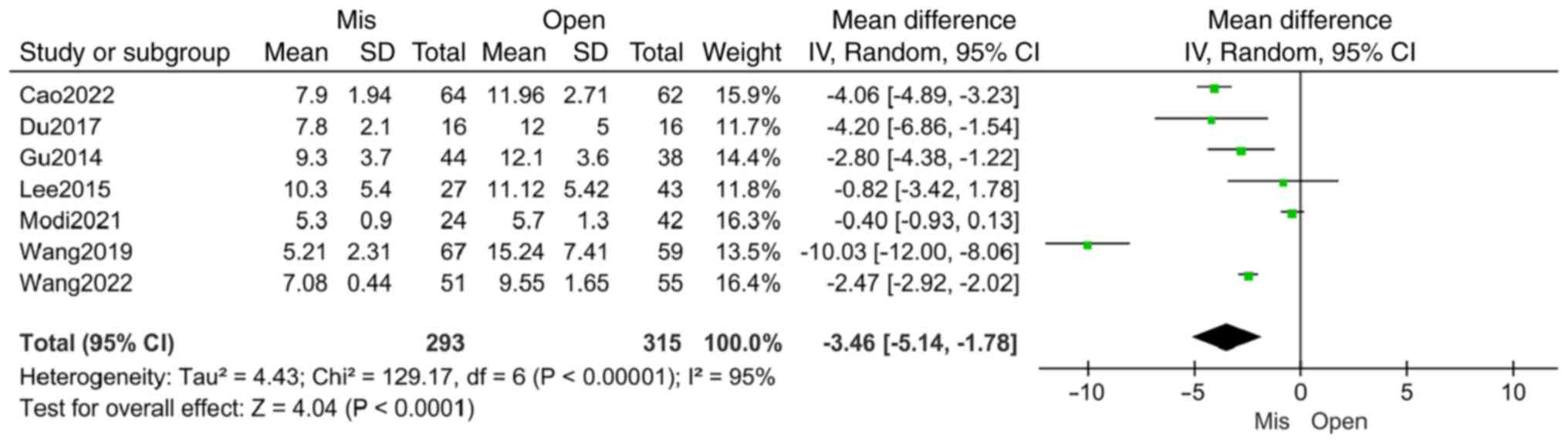
Fig. 6). A total of seven studies
compared the length of hospitalization time and the heterogeneity
of each study was significant (I2=95%) using a
random effect model, showing that the postoperative hospitalization
time in the MIS-TLIF group was significantly shorter than that in
the open TLIF group (95%CI: -5.14,-1.78; P<0.0001; Fig. 7). The outcomes indicated that the
postoperative bed and hospitalization times in the MIS-TLIF group
were significantly shorter than those in the open TLIF group. This
indicated that minimally invasive surgery causes less tissue damage
and patients recover more quickly postoperatively.
Postoperative complications. A total of eight
studies compared the postoperative complications of MIS-TLIF and
open TLIF for multi-segment lumbar degenerative diseases. The
heterogeneity of each study was low (I2=48%) and
a fixed-effects model was used. The results showed no significant
difference in postoperative complications between MIS-TLIF and open
TLIF (95%CI: 0.41,1.14; P=0.15; Fig.
8). The MIS-TLIF and open TLIF groups did not differ
significantly in the incidence of postoperative complications in
multi-segmental lumbar degenerative disease.
Fusion rate. A total of six studies reported
the fusion rate, of which four studies divided the fusion situation
into four grades according to the Bridwell criterion (26): grades I and II were fusion and
grades III and IV were non-fusion. Subgroup analysis was performed
for Bridwell grades I and II. The heterogeneity test results
(I2=0%) indicated that heterogeneity was small
and a fixed-effects model was used. The findings revealed no
discernible difference between open TLIF and MIS-TLIF regarding the
fusion rate (95%CI: 0.77,1.32; P=0.96; Fig. 9). Two articles only reported the
overall fusion rate. Heterogeneity in each study was low
(I2=0%). A fixed-effects model was used. The
results showed no significant difference in the overall fusion rate
between the two groups and the statistics did not support the
difference (95%CI: 0.60,2.62; P=0.54) (Fig. 10). The results demonstrated that
MIS-TLIF and open TLIF can provide excellent fusion results for
multi-segmental lumbar spine diseases.
Postoperative functional score. Postoperative
functional scores included the ODI and VAS scores. A total of nine
studies compared ODI scores based on the last follow-up. The
overall heterogeneity test was high (I2=89%) and
a random-effects model was used. The results showed no significant
difference in postoperative ODI scores between the two groups
(95%CI: -2.05,-0.24; P=0.12; Fig.
11). The MIS-TLIF and open TLIF groups did not differ
significantly in postoperative dysfunction index scores and both
procedures resulted in excellent decompression. The six papers
(15,17,18,21,22,24)
returned the reported results of postoperative VAS scores, but
because the results of one of them were expressed as mean and
maximum-minimum and could not be calculated for conversion to
standardized data, this article was discarded; with the exclusion
of postoperative VAS scores for low back pain from one study
(I2=35%) and overall (I2=47%),
using a fixed-effects model, the findings revealed a statistically
significant difference between the postoperative VAS values for leg
pain in the MIS-TLIF and open TLIF groups (95%CI: -0.27,-0.13;
P<0.00001; Fig. 12). The
MIS-TLIF and open TLIF groups showed no significant differences in
postoperative lower back pain; however, there was a difference in
postoperative leg pain, with lower VAS scores for postoperative leg
pain in the MIS-TLIF group.
Publication bias and sensitivity
analysis
Publication bias and sensitivity of intraoperative
operative time, blood loss, postoperative drainage volume,
fluoroscopy frequency, postoperative bedtime, hospitalization time,
complications, fusion rate and ODI and VAS scores were assessed
using Review Manager 5.4. The funnel plots of the items were mostly
symmetrical, indicating no overt publication bias and that the data
were consistent and dependable (Fig.
13). Studies with (I2>50%) were analyzed
for sensitivity and we found that (I2=78%) became
(I2=0%) by excluding one of the studies on
bedtime; (I2=74%) became
(I2=35%) after excluding one of the studies
related to the VAS score of postoperative low back pain. The
heterogeneity of the rest of the studies did not change
significantly after excluding the literature one by one, indicating
the stability of the results.
 | Figure 13Funnel plots created to assess
publication bias for (A) operation time, (B) intraoperative blood
loss, (C) postoperative drainage volume, (D) fluoroscopy frequency,
(E) postoperative in-bed time, (F) hospitalization time, (G)
postoperative complications, (H) fusion rate, (I) overall fusion
rate, (J) Oswestry Disability Index scores, (K) Visual Analog Scale
scores. SE, standard error; MD, mean difference; CI, confidence
interval. |
Discussion
Lumbar degenerative diseases are prevalent in older
individuals and multi-segmental lumbar degenerative diseases are
common in clinical practice. Patients with ineffective conservative
treatment and severe neurological symptoms require surgical
treatment to restore the original stable structure of the lumbar
spine and decompress the compressed spinal cord and nerve roots. A
number of surgical methods exist, including posterior LIF (PLIF),
TLIF, oblique LIF, extreme lateral LIF and various minimally
invasive methods. TLIF, a mature technique, is a common surgical
method for treating lumbar degenerative diseases (27). Compared to PLIF, TLIF causes less
disturbance to the dural sac and nerve root, less chance of injury
and less damage to the ligamentous complex, which is conducive to
spinal stability (28). However,
traditional TLIF still has the common problem of requiring open
surgery. Due to the large skin incision, hooks pulling the soft
tissue during the operation may cause liquefaction and necrosis of
the soft tissue, leading to postoperative low back pain. MIS-TLIF
uses spinal surgical channel technology, which causes less surgical
trauma to the muscle of the patient and can achieve unilateral and
bilateral decompression, less stimulation to soft tissue, less
inflammatory response than open surgery and faster functional
recovery. Current trends in surgery favor minimally invasive
procedures. The ongoing development of various procedures aims to
achieve improved clinical outcomes and fewer postoperative
complications.
There was no significant difference in the operative
time between the two groups in this meta-analysis, probably because
minimally invasive surgery requires numerous fluoroscopies to
determine the location of anatomical structures such as pedicles
and articular eminences of the responsible segment and requires
multiple intraoperative adjustments of the access and direction,
making the operation process more complicated and the instruments
used more complex. Previous studies found that the operative time
was longer in the MIS-TLIF group than in the open TLIF group
(29,30). However, a significant correlation
exists between operative time and operator proficiency. Garcia
et al (31) concluded that
the operator needs to perform at least 58 procedures to become
proficient in MIS-TLIF and then the operative time decreases
gradually. MIS-TLIF requires the operator to be experienced in open
surgery and proficient in using minimally invasive surgical
instruments, which explains the longer and steeper learning curve
of the MIS-TLIF procedure (32).
There was no significant difference in the postoperative drainage
volume. Blood loss was lower in the MIS-TLIF group compared with
the open TLIF group. This may be because MIS-TLIF adopts the
intermuscular approach, using the working sleeve to expand
step-by-step without extensive soft tissue separation and with less
damage to muscle fibers. By comparison, open TLIF involves a large
incision and more tissue damage, resulting in increased
intraoperative bleeding. There was no significant difference in the
fusion rates in the present study. There was no difference between
the two groups regarding Bridwell grades I and II or overall fusion
rate. The fusion rate is an important index for testing the effect
of surgery, which shows whether open TLIF or MIS-TLIF, complete
nerve decompression and stable fusion of surgical segments can be
achieved in two-segment lumbar surgery. This is similar to the
results of the single-stage surgery (33). It has also been suggested that open
surgery has a higher fusion rate than minimally invasive surgery,
arguing that open surgery provides cleaner handling of the disc
tissue under direct vision, adequate handling of the implant bed
and more bone grafting (34).
There were no significant differences in postoperative
complications in the present study, suggesting that minimally
invasive maneuvers in two-segment lumbar spine surgery did not
reduce postoperative complications. This may be related to the long
duration and high risk of injury associated with multi-segmental
surgery. According to one investigation, MIS-TLIF has a higher rate
of postoperative complications in multiple segments than in single
segments (35). MIS-TLIF also has
the disadvantage of requiring a significantly higher number of
intraoperative radiations compared with the open TLIF group.
MIS-TLIF requires multiple intraoperative fluoroscopies to locate
the channel and reposition surgical segments. The increase in the
number or duration of fluoroscopy prolongs the duration of the
procedure and increases radiation exposure to the patient, which
was confirmed in a study by Qin et al (36). A study found that the fluoroscopy
time increased by 22.9 sec compared with the open TLIF group. By
detecting the exposure dose used by the physician, it was found
that the radiation dose in the MIS-TLIF group was 30 µSv higher
than that in the open TLIF group (37). In the present study, the bed and
hospitalization times of the MIS-TLIF group were shorter than those
of the open-TLIF group, indicating that patients undergoing
MIS-TLIF left bed and were able to be discharged from the hospital
earlier. This also indirectly reflects the theoretical advantage of
reduced soft tissue injury in the MIS-TLIF group. A more direct
manifestation of this is lower hospitalization costs. Regarding
postoperative functional indicators, the postoperative ODI and low
back pain VAS scores were not statistically significant; only the
postoperative leg pain VAS score was significant. Although both
groups demonstrated effectively reduced postoperative symptoms, the
minimally invasive group outperformed the open group regarding the
postoperative leg pain VAS score. As for postoperative pain scores,
postoperative opioid use may affect postoperative pain scores;
however, Claus et al (38)
showed that low-dose ketochromic acid and opioid use can achieve
the same analgesic effect. Only Wang et al (22) studied the long-term efficacy. The
ODI and VAS scores were similar between the minimally invasive and
open surgery groups at 24 months and the final follow-up. This is
similar to single-stage surgery, with both procedures achieving
equally safe and satisfactory results while overall favoring
MIS-TLIF (39). Although there are
a number of articles related to open TLIF and MIS-TLIF surgeries,
they all compared single-stage fusion and there are no
meta-analyses on multiple segments. The common limitations of these
studies include the lack of long-term follow-up, the fact that the
majority of the research countries are concentrated in China and
the lack of comparison between multi-segmental surgery (14,40);
regarding single-stage surgery, MIS-TLIF is superior to open TLIF
concerning intraoperative blood loss, shortened hospitalization and
recovery times and reduced complications. However, multi-segmental
surgery has no clear conclusion, which remains controversial. The
present study focused on multi-segmental surgery and is the first
meta-analysis to analyze the efficacy of minimally invasive open
TLIF in treating multi-segmental lumbar degenerative diseases.
The present study discovered that patients with
multi-segmental lumbar degenerative disorders can achieve effective
relief of their postoperative symptoms, regardless of whether they
undergo open-TLIF or MIS-TLIF. MIS-TLIF has the advantages of less
intraoperative blood loss, shorter bedtime and shorter
hospitalization time in multi-segment surgery; however, it had a
significantly higher frequency of fluoroscopic surgery than open
surgery. In the postoperative ODI and VAS scores, the VAS score of
leg pain after MIS-TLIF was superior than that of open TLIF. There
was no difference in the operative time and fusion rate. Therefore,
for patients with lumbar degenerative disorders requiring
multi-segment fusion surgery, MIS-TLIF is preferable to open
TLIF.
The limitations of the present study included: i)
The literature included in the present study lacked randomized
controlled studies and high-quality articles; ii) the follow-up
time of the included studies was inconsistent, which may have
impacted the results and caused a lack of long-term follow-up; iii)
the minimum number of included studies in the outcome indicators
was two, which may have introduced some bias; iv) the countries of
the researchers were relatively concentrated, with most studies
conducted in China and a few studies in Europe, America and other
countries; therefore, it is unknown whether the conclusion applies
to other countries. Due to the quality of the articles and the high
heterogeneity of some of the indicators, the results of the present
study may be somewhat different from the actual results.
Nevertheless, the results of the present study provide some
clinical references in this field; however, more randomized
controlled trials with larger sample sizes are needed to obtain
more reliable results.
Acknowledgements
Not applicable.
Funding
Funding: The present study was supported by the Changzhi City
Science and Technology Bureau Fund Project (grant no. 2022sy008)
and the Heping Hospital Affiliated to Changzhi Medical College
Youth Start-up Fund Project.
Availability of data and materials
The data generated in the present study may be
requested from the corresponding author.
Authors' contributions
WJZ and ZKW were accountable for the design of the
present study and both performed the statistical analyses. WJZ and
ZKW confirm the authenticity of all the raw data. HLL and SLQ
conducted the study and collected important background information.
PFH and YFX drafted the manuscript and performed the interpretation
of data. All authors read and approved the final manuscript.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Machino M, Nakashima H, Ito K, Tsushima M,
Ando K, Kobayashi K and Imagama S: Influence of age and gender on
intervertebral disk degeneration and height in the thoracolumbar
spine. Spine Surg Relat Res. 6:379–387. 2021.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Patel J, Osburn I, Wanaselja A and Nobles
R: Optimal treatment for lumbar spinal stenosis: An update. Curr
Opin Anaesthesiol. 30:598–603. 2017.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Boucher HH: A method of spinal fusion. J
Bone Joint Surg Br. 41-B:248–259. 1959.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Zhang YW, Deng L, Zhang XX, Yu XL, Ai ZZ,
Mei YX, He F, Yu H, Zhang L, Xiao X, et al: Three-dimensional
printing-assisted cervical anterior bilateral pedicle screw
fixation of artificial vertebral body for cervical tuberculosis.
World Neurosurg. 127:25–30. 2019.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Zhang YW, Zeng T, Gao WC, Xiao X, Xiao Y,
Chen X, Zhang SL and Deng L: Progress of the anterior
transpedicular screw in lower cervical spine: A review. Med Sci
Monit. 25:6281–6290. 2019.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Harms J and Rolinger H: A one-stager
procedure in operative treatment of spondylolistheses: Dorsal
traction-reposition and anterior fusion (author's transl). Z Orthop
Ihre Grenzgeb. 120:343–347. 1982.PubMed/NCBI View Article : Google Scholar : (In German).
|
|
7
|
Reid PC, Morr S and Kaiser MG: State of
the union: A review of lumbar fusion indications and techniques for
degenerative spine disease. J Neurosurg Spine. 31:1–14.
2019.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Kumaran Y, Shah A, Katragadda A,
Padgaonkar A, Zavatsky J, McGuire R, Serhan H, Elgafy H and Goel
VK: Iatrogenic muscle damage in transforaminal lumbar interbody
fusion and adjacent segment degeneration: A comparative finite
element analysis of open and minimally invasive surgeries. Eur
Spine J. 30:2622–2630. 2021.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Foley KT and Lefkowitz MA: Advances in
minimally invasive spine surgery. Clin Neurosurg. 49:499–517.
2002.PubMed/NCBI
|
|
10
|
Bovonratwet P, Samuel AM, Mok JK, Vaishnav
AS, Morse KW, Song J, Steinhaus ME, Jordan YJ, Gang CH and Qureshi
SA: Minimally invasive lumbar decompression versus minimally
invasive transforaminal lumbar interbody fusion for treatment of
low-grade lumbar degenerative spondylolisthesis. Spine (Phila Pa
1976). 47:1505–1514. 2022.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Garg B and Mehta N: Minimally invasive
transforaminal lumbar interbody fusion (MI-TLIF): A review of
indications, technique, results and complications. J Clin Orthop
Trauma. 10 (Suppl 1):S156–S162. 2019.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Mobbs RJ, Phan K, Malham G, Seex K and Rao
PJ: Lumbar interbody fusion: Techniques, indications and comparison
of interbody fusion options including PLIF, TLIF, MI-TLIF,
OLIF/ATP, LLIF and ALIF. J Spine Surg. 1:2–18. 2015.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Jover-Mendiola AD, Lopez-Prats FA,
Lizaur-Utrilla A and Vizcaya-Moreno MF: Patient-reported outcomes
of minimally invasive versus open transforaminal lumbar interbody
fusion for degenerative lumbar disc disease: A prospective
comparative cohort study. Clin Orthop Surg. 15:257–264.
2023.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Xue J, Song Y, Liu H, Liu L, Li T and Gong
Q: Minimally invasive versus open transforaminal lumbar interbody
fusion for single segmental lumbar disc herniation: A
meta-analysis. J Back Musculoskelet Rehabil. 35:505–516.
2022.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Cao Y, Li X, Chen ZG, Li LD and Lv SJ:
Minimally invasive transforaminal approach and conventional
transforaminal approach for lumbar fusion treatment. J Nantong Univ
(Med Sci). 42:544–547. 2022.(In Chinese).
|
|
16
|
Du YB, Zhang ZD, Liu YM, Wang SS and Ma L:
Comparison of effects between MIS-TLIF and TLIF in the treatment of
L4 ~ S1 lumbar stenosis. J Clin Orthop. 20:289–292. 2017.(In
Chinese).
|
|
17
|
Gu G, Zhang H, Fan G, He S, Cai X, Shen X,
Guan X and Zhou X: Comparison of minimally invasive versus open
transforaminal lumbar interbody fusion in two-level degenerative
lumbar disease. Int Orthop. 38:817–824. 2014.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Hu W, Yang G, Wang H, Wu X, Ma H, Zhang K
and Gao Y: Which is better in clinical and radiological outcomes
for lumbar degenerative disease of two segments: MIS-TLIF or
OPEN-TLIF? J Pers Med. 12(1977)2022.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Lee WC, Park JY, Kim KH, Kuh SU, Chin DK,
Kim KS and Cho YE: Minimally invasive transforaminal lumbar
interbody fusion in multilevel: Comparison with conventional
transforaminal interbody fusion. World Neurosurg. 85:236–243.
2016.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Modi HN and Shrestha U: Comparison of
clinical outcome and radiologic parameters in open TLIF versus
MIS-TLIF in single- or double-level lumbar surgeries. Int J Spine
Surg. 15:962–970. 2021.PubMed/NCBI View
Article : Google Scholar
|
|
21
|
Wang L: The Clinical Outcomes Comparison
Between Minimally Invasive (Zista Channel) and Open Surgery for the
Treatment of Multi-Level Lumbar Degenerative Disease. Dalian Med
Univ. 2019.(In Chinese).
|
|
22
|
Wang X, Liu Y, Du Y, Qi J, Li C, Zheng K
and Yu X: Clinical outcomes of minimally invasive transforaminal
lumbar interbody fusion fordouble-segment lumbar spinal stenosis at
mid- and long-term follow-up. J Pract Med. 37:149–153. 2021.(In
Chinese).
|
|
23
|
Wang HH, Liu J, Xu YY, Zhang Y, Sun Y and
Wang GH: Short and medium term efficacy of microscope-assisted
MIS-TLIF versus open-TLIF for two-segment lumbar spinal stenosis. J
Pract Med. 38:1373–1377. 2022.(In Chinese).
|
|
24
|
Zhang Y, Zhou T, Gu Y, Che W, Zhang L and
Wang Y: Contralateral bridge fixation of freehand minimally
invasive pedicle screws combined with unilateral MIS-TLIF vs. open
TLIF in the treatment of multi-segmental lumbar degenerative
diseases: A five years retrospective study and finite element
analysis. Front Surg. 9(1049260)2022.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Stang A: Critical evaluation of the
Newcastle-Ottawa scale for the assessment of the quality of
nonrandomized studies in meta-analyses. Eur J Epidemiol.
25:603–605. 2010.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Bridwell KH, Lenke LG, McEnery KW, Baldus
C and Blanke K: Anterior fresh frozen structural allografts in the
thoracic and lumbar spine. Do they work if combined with posterior
fusion and instrumentation in adult patients with kyphosis or
anterior column defects? Spine (Phila Pa 1976). 20:1410–1418.
1995.PubMed/NCBI
|
|
27
|
Kang YN, Ho YW, Chu W, Chou WS and Cheng
SH: Effects and safety of lumbar fusion techniques in lumbar
spondylolisthesis: A network meta-analysis of randomized controlled
trials. Global Spine J. 12:493–502. 2022.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Cheng X, Zhang K, Sun X, Zhao C, Li H, Ni
B and Zhao J: Clinical and radiographic outcomes of bilateral
decompression via a unilateral approach with transforaminal lumbar
interbody fusion for degenerative lumbar spondylolisthesis with
stenosis. Spine J. 17:1127–1133. 2017.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Parrish JM, Jenkins NW, Brundage TS,
Hrynewycz NM, Podnar J, Buvanendran A and Singh K: Outpatient
minimally invasive lumbar fusion using multimodal analgesic
management in the ambulatory surgery setting. Int J Spine Surg.
14:970–981. 2020.PubMed/NCBI View
Article : Google Scholar
|
|
30
|
Ge DH, Stekas ND, Varlotta CG, Fischer CR,
Petrizzo A, Protopsaltis TS, Passias PG, Errico TJ and Buckland AJ:
comparative analysis of two transforaminal lumbar interbody fusion
techniques: Open TLIF versus wiltse MIS TLIF. Spine (Phila Pa
1976). 44:E555–E560. 2019.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Garcia D, Sousa-Pinto B, De Biase G,
Ruiz-Garcia H, Akinduro OO, Dholakia R, Borah B, Fox WC, Nottmeier
E, Deen HG, et al: Minimally invasive transforaminal lumbar
interbody fusion: Cost of a surgeon's learning curve. World
Neurosurg. 162:e1–e7. 2022.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Kovari VZ, Kuti A, Konya K, Szel I,
Szekely AK and Szalay K: Comparison of single-level open and
minimally invasive transforaminal lumbar interbody fusions
presenting a learning curve. Biomed Res Int.
2020(3798537)2020.PubMed/NCBI View Article : Google Scholar
|
|
33
|
Kim CH, Easley K, Lee JS, Hong JY, Virk M,
Hsieh PC and Yoon ST: Comparison of minimally invasive versus open
transforaminal interbody lumbar fusion. Global Spine J. 10 (2
Suppl):143S–150S. 2020.PubMed/NCBI View Article : Google Scholar
|
|
34
|
Deng QX, Ou YS, Zhu Y, Zhao ZH and Huang
Q: Risk factors of cage subsidence after single level
transforaminal lumbar interbody fusion. Chin J Orthop. 38:156–163.
2018.(In Chinese).
|
|
35
|
Huang J, Rabin EE, Stricsek GP and Swong
KN: Outcomes and complications of minimally invasive transforaminal
lumbar interbody fusion in the elderly: A systematic review and
meta-analysis. J Neurosurg Spine. 36:741–752. 2022.PubMed/NCBI View Article : Google Scholar
|
|
36
|
Qin R, Wu T, Liu H, Zhou B, Zhou P and
Zhang X: Minimally invasive versus traditional open transforaminal
lumbar interbody fusion for the treatment of low-grade degenerative
spondylolisthesis: A retrospective study. Sci Rep.
10(21851)2020.PubMed/NCBI View Article : Google Scholar
|
|
37
|
Arif S, Brady Z, Enchev Y, Peev N and
Encheva E: Minimising radiation exposure to the surgeon in
minimally invasive spine surgeries: A systematic review of 15
studies. Orthop Traumatol Surg Res. 107(102795)2021.PubMed/NCBI View Article : Google Scholar
|
|
38
|
Claus CF, Lytle E, Lawless M, Tong D,
Sigler D, Garmo L, Slavnic D, Jasinski J, McCabe RW, Kaufmann A, et
al: The effect of ketorolac on posterior minimally invasive
transforaminal lumbar interbody fusion: An interim analysis from a
randomized, double-blinded, placebo-controlled trial. Spine J.
22:8–18. 2022.PubMed/NCBI View Article : Google Scholar
|
|
39
|
Kunadt M, Barleben L and Büttner-Janz K:
One-level open vs minimally invasive transforaminal lumbar
interbody fusion: A systematic review and advanced meta-analytic
assessment of prospective studies with at least two years
follow-up. Eur Spine J. 31:2557–2571. 2022.PubMed/NCBI View Article : Google Scholar
|
|
40
|
Miller LE, Bhattacharyya S and Pracyk J:
Minimally invasive versus open transforaminal lumbar interbody
fusion for single-level degenerative disease: A systematic review
and meta-analysis of randomized controlled trials. World Neurosurg.
133:358–365.e4. 2020.PubMed/NCBI View Article : Google Scholar
|