Introduction
Intrauterine adhesions (IUAs), also known as
Asherman syndrome, is a common gynecological disease in clinical
practice that is accompanied by several symptoms, such as pain,
menstrual disturbance and subfertility (1). The majority of IUA cases are
associated with trauma to the endometrial basalis layer caused by
curettage, hysteroscopy, intrauterine infections and genital
tuberculosis (2). The incidence
and prevalence of IUAs vary in different studies. A review article
by Yu et al (3) reported
that the incidence of IUAs in 2,981 patients was 770/2,981 in
Israel, 456/2,981 in Greece and 445/2,981 in South America. Another
study indicated that the incidence of IUAs was 16-19%, as verified
by hysteroscopy after miscarriage curettage. Additionally, this
study also reported that the risk of IUAs was notably increased by
40% after repeated curettage (4).
It is widely accepted that hysteroscopy is the most
accurate method for the diagnosis and treatment of IUAs. It has
been also reported that hysteroscopic lysis performed using
hysteroscopic scissors without electrosurgery provides protection
to the endometrium (5-7).
Due to the high rate of adhesion reformation (21.0-41.9%) (8), the prevention of IUA recurrence
following operation is crucial for the therapeutic outcome. Several
types of precautions can be taken to achieve this purpose,
including the application of crosslinked hyaluronic acid gels,
balloon catheters, intrauterine devices (IUDs), estrogen, aspirin
and stem cell treatment (1,8-10).
The insertion of an IUD to separate the endometrial layers after
the hysteroscopic lysis of IUAs has been applied for several years.
However, due to their inflammatory-promoting properties,
copper-containing IUDs are not recommended. However, when
non-copper IUDs were removed from the market (3), the use of copper-containing IUDs
after hysteroscopy is likely to increase in clinical practice.
Nevertheless, the data regarding subsequent fertility and obstetric
outcomes after the use of copper-containing IUDs following
hysteroscopy are limited. Therefore, the present prospective,
randomized controlled trial (RCT) was carried out to investigate
the efficacy of copper-containing IUDs on reproductive outcomes
after hysteroscopic adhesiolysis in women treated for IUAs.
Subjects and methods
Subjects
This present study was approved by the Medical
Ethics Committee of the Affiliated Jinhua Hospital of Wenzhou
Medical University (approval no. IRB-2020028-R; Jinhua, China) and
was conducted at the same hospital between January 2020 and June
2021. The inclusion criteria were as follows: i) Patients who met
the diagnostic criteria for IUAs by hysteroscopy; ii) patients who
were willing to participate in the study and signed the informed
consent form; iii) female patients aged 23-50 years (11-13);
iv) patients who suffered from mild to severe IUAs, according to
the American Fertility Society (AFS) classification system
(3); and v) patients who wished to
become pregnant. The exclusion criteria were the following: i)
Patients who had contraindications for estrogen-progesterone
therapy and hysteroscopy, including severe coagulation disorders,
severe heart, liver and kidney diseases or mental disorders; ii)
patients who suffered from female genital tuberculosis, endometrial
polyps, submucous myoma and endometrial carcinoma; and iii) women
with postmenopausal status.
Sample size calculation
In the present research, it was hypothesized that
the live birth rates were 50% in patients with IUDs and 20% in
patients without any barrier device, as indicated in previous
literature (1-3).
By accepting a type I error (α) of 0.05 and a type II error (β) of
0.1, the number of patients with IUAs required for each group was
54. Estimating a drop-out rate of 30%, a total of 140 subjects were
required.
Patient grouping
Patients who fulfilled the inclusion criteria and
signed informed consent to participate in the study were randomized
into the treatment or control groups using a computer randomization
method. After completing the procedure of hysteroscopic
adhesiolysis during the follicular period, patients in the
treatment group used copper-containing IUDs, while those in the
control group did not use any barrier device. The hysteroscopic
adhesiolysis procedure was repeated (2-3 times) until the uterine
cavity was recovered, as verified by two experienced gynecologists
(PX and BY).
Treatment
Patients without history of allergies received
antibiotic prophylaxis with intravenous injection of 1.5 g
cefuroxime 30 min prior to surgery. Once IUA was assessed and
verified, patients underwent hysteroscopy with a 5.0 mm outer
diameter hysteroscopy (Richard Wolf GmbH) to divide the adhesions
using hysteroscopic scissors without electrosurgery under local
anesthesia. The intrauterine pressure was maintained at 120 mmHg
and normal saline was used as a distension medium. Transabdominal
ultrasonography was applied throughout the operation. Each patient
was orally administrated with 4 mg/day estradiol (dydrogesterone
tablets) for the first 14 days and 20 mg/day complex packing
estradiol tablets/estradiol and dydrogesterone tablets (2 mg/2 mg
and 10 mg; Abbott Biologicals B.V.) for the last 7 days after
hysteroscopy. During the interval between operations (4 weeks), all
patients also received low-dose aspirin (75 mg/day). The IUDs
remained in the uterine cavity for 4 weeks. The second look
hysteroscopic therapy was carried out ~4 weeks after the first
surgery. In addition, if a patient suffered from severe adhesion
recurrence, the third hysteroscopic procedure was usually performed
at ~4 weeks after the second surgery. After the completion of the
aforementioned treatment, the patient underwent natural conception
or assisted reproduction, followed up bimonthly for 1.5 years, and
the fertility outcome was recorded. The data of the present study
were collected and managed by the electronic medical record system
of the Affiliated Jinhua Hospital of Wenzhou Medical
University.
Pregnancy definition
Pregnancy was verified by detecting fetal cardiac
activity using transvaginal ultrasound. Live birth was defined as
≥28 completed weeks of live birth gestation, while preterm birth
was defined as ≥28 completed weeks, but prior 37 completed weeks of
live birth gestation. Placenta accreta spectrum or adherent
placenta disorders were diagnosed using ultrasound, nuclear
magnetic resonance imaging or during surgery.
Statistical analysis
All statistical analyses were performed using SPSS
version 25 software (IBM Corp.). The continuous variables of the
clinical characteristics are presented as the mean ± SD or the
median (P25, P75). The differences between the groups were compared
using independent-sample Student's t-test or Wilcoxon rank-sum
test. Dichotomous variables are presented as n (%) and were
analyzed using χ2 test. P<0.05 was considered to
indicate a statistically significant difference.
Results
Patient characteristics
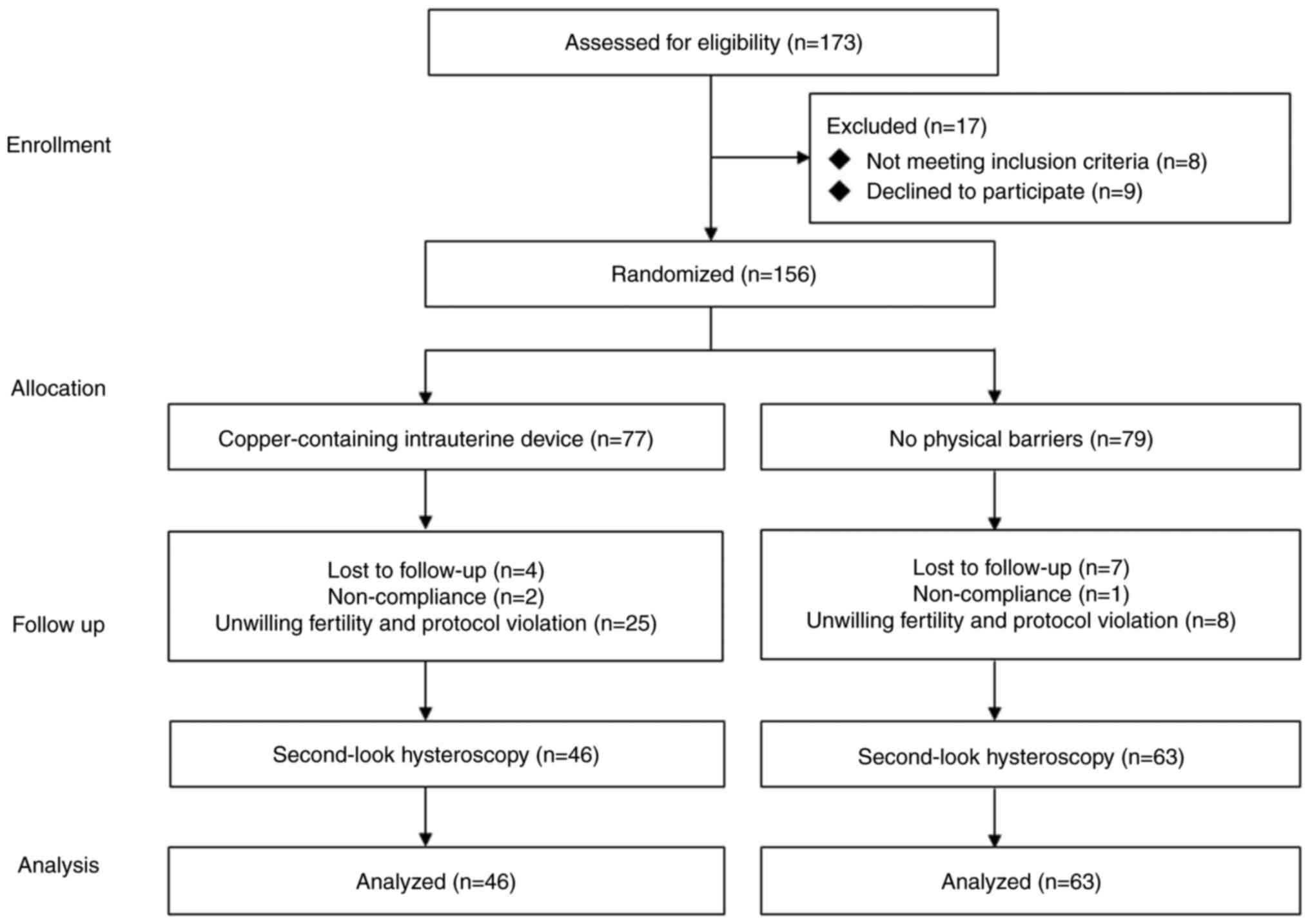
The flow chart of subject recruitment, randomization
and follow-up is shown in Fig. 1.
Of the 173 women that were originally recruited, a total of 17
patients were excluded and the remaining 156 were randomly
allocated into the treatment (n=77) and control (n=79) groups.
Finally, 109 patients completed the study and final analysis. After
the first operation, a total of 33 patients changed the treatment
plan and did not try to conceive during the follow-up period, which
included 25 patients in the treatment group and 8 patients in the
control group. A total of 11 patients were lost to follow-up, 4
patients in the treatment group and 7 patients in the control
group. A total of 3 patients were reluctant to continue the study,
2 patients in the treatment group and 1 patient in the control
group. The basic characteristics, including age, body mass index,
parity, miscarriage times and AFS scores were compared between the
two groups. As shown in Table I
there were no statistically significant differences between the two
groups. By contrast, hysteroscopy frequency was significantly
higher in the treatment group compared with the control group.
 | Table IComparison of the clinical
characteristics of patients between the treatment and control
groups after hysteroscopy. |
Table I
Comparison of the clinical
characteristics of patients between the treatment and control
groups after hysteroscopy.
| Characteristic | Treatment group
(n=46) | Control group
(n=63) | P-value | t/z value |
|---|
| Age,
yearsa,b | 33.88±0.71 | 33.36±0.69 | 0.605 | 0.519 |
| BMI,
kg/m2a,b | 22.32±0.45 | 23.18±0.44 | 0.178 | 1.358 |
| Parityc,d | 0 (0,1) | 0 (0,1) | 0.486 | 0.696 |
|
Miscarriagesc,d | 1 (1,2) | 2 (1,2) | 0.860 | 0.177 |
| AFS
scorea,d | 6.20±0.23 | 5.74±0.14 | 0.094 | 1.694 |
|
Hysteroscopya,b | 2.10±0.09 | 1.31±0.08 | <0.001 | 6.458 |
Pregnancy and live birth rates after
hysteroscopy
As previously stated, a total of 109 patients were
eligible and tried to get pregnant. Among them, 38/46 (82.6%)
patients in the treatment group and 55/63 (87.3%) in the control
group underwent in vitro fertilization and embryo transfer
using artificial reproductive techniques. No statistically
significant difference was observed between the two groups
(Table II). The comparison of
pregnancy rates between the two groups after hysteroscopy are shown
in Table III. The pregnancy rate
in the treatment group (60.9%) was lower compared with that in the
control group (66.7%). However, statistical significance was not
reached (P>0.05). Furthermore, the live birth rate after
hysteroscopy in the treatment group (41.3%) was lower compared with
that in the control group (55.6%). However, again, no statistically
significant differences were obtained between the two groups
(P>0.05; Table III).
 | Table IIComparison of pregnancy methods
between the treatment and control groups after hysteroscopy. |
Table II
Comparison of pregnancy methods
between the treatment and control groups after hysteroscopy.
| | χ2
test |
|---|
| Group | Patient number | IVF-ET, n (%) | Natural conception, n
(%) | D-value and 95%
confidence interval | χ2
value | P-value |
|---|
| Treatment group | 46 | 38 (82.6) | 8 (17.4) | 4.7
(-7.9-19.5) | 0.468 | 0.494 |
| Control group | 63 | 55 (87.3) | 8 (12.7) | | | |
 | Table IIIComparison of pregnancy rates and live
birth rates between the treatment and control groups after
hysteroscopy. |
Table III
Comparison of pregnancy rates and live
birth rates between the treatment and control groups after
hysteroscopy.
| A, Pregnancy
rate |
|---|
| | χ2
test |
|---|
| Group | Patient number | Pregnancy, n (%) | No pregnancy, n
(%) | D-value and 95%
confidence interval | χ2
value | P-value |
|---|
| Treatment group | 46 | 28 (60.9) | 18 (39.1) | 5.8
(-12.5-24.1) | 0.39 | >0.05 |
| Control group | 63 | 42 (66.7) | 21 (33.3) | | | |
| B, Live birth
rate |
| | χ2
test |
| Group | Patient number | Pregnancy, n (%) | No pregnancy, n
(%) | D-value and 95%
confidence interval | χ2
value | P-value |
| Treatment
group | 46 | 19 (41.3) | 27 (58.7) | 14.3
(-4.5-33.1) | 2.16 | >0.05 |
| Control group | 63 | 35 (55.6) | 28 (44.4) | | | |
Obstetric outcomes after
hysteroscopy
The obstetric outcomes between the two groups were
compared as shown in Table IV.
Among all patients included in the present study, 54/109 (49.54%)
had at least one live birth, while 8/54 gave twin live birth. In
addition, 36/54 (66.67%) women underwent cesarean delivery, 10/54
(18.82%) had adherent placenta and placenta accreta, while 3/54
(5.56%) received blood transfusion. Additionally, 2/54 patients
(3.70%) underwent abdominal hysterectomy and 5/54 (9.26%) gave
premature birth. No neonatal deaths were recorded.
 | Table IVObstetric outcomes from live births
in the treatment and control groups after hysteroscopy. |
Table IV
Obstetric outcomes from live births
in the treatment and control groups after hysteroscopy.
| Outcome | Number (%) |
|---|
| Live births | 54 (49.54) |
| Cesarean
delivery | 36 (66.67) |
| In vitro
fertilization and embryo transfer after hysteroscopy | 93 (85.30) |
| Adherent placenta
and placenta accreta spectrum | 10 (18.82) |
| Blood
transfusion | 3 (5.56) |
| Postpartum
hysterectomy | 2 (3.70) |
| Twin live
birth | 8 (14.81) |
| Premature
birth | 5 (9.26) |
| Neonatal
deaths | 0 (0.00) |
Discussion
Hysteroscopic lysis of adhesions is an effective and
standard approach for the diagnosis and treatment of IUAs. Due to
the high rate of adhesion reformation after primary hysteroscopy,
preventing the recurrence of IUAs after operation is of important
for their cure. IUDs and other mechanical barriers have been widely
used to separate the endometrial layers for endometrial
regeneration. The use of IUDs has been considered as a standard
approach for maintaining uterine cavity (7). Due to the induction of inflammatory
responses, the application of copper-containing IUDs is not
recommended. However, the use of copper-containing IUDs after
hysteroscopy is likely to increase in clinical practice when
non-copper IUDs are withdrawn from the market. There are limited
data regarding subsequent fertility and obstetric outcomes in
patients using copper-containing IUDs (1). Therefore, a prospective RCT was
conducted in the present study to investigate the reproductive
outcomes of patients using copper-containing IUDs. A major
limitation of the present study was that a control arm, involving
patients treated with IUDs without copper, was not included.
In the current study, the reproductive outcomes in
patients treated for IUAs between the copper-containing IUD
(treatment group) and the no-barrier device (control group) groups
following hysteroscopic lysis were compared. The live birth rate is
considered to be the most significant clinical outcome in women
with IUAs who wish to become pregnant (3). In the present study, a 60.9 and 66.7%
pregnancy rate was recorded in the treatment and control group,
respectively. The pregnancy rates in both the treatment and control
groups in the present study were higher than those reported by
Pabuccu et al (11) (30 and
47.2%, respectively) and similar to those recorded in the study by
Huang et al (12) (58.9%)
in 2020. However, no significant differences were observed in both
pregnancy and live birth rates between the two groups. With a live
birth rate of 41.3% in the treatment group and 55.6% in the control
group, a total of 49.54% of patients gave at least one live birth.
The aforementioned results were consistent with those reported by
Huang et al (12). In the
prospective RTC by Huang et al (12), 171 patients were randomly allocated
into the balloon insertion and contraceptive IUDs plus Foley
catheter groups. No statistically significant differences were
recorded in the pregnancy and live birth rates between the two
groups (12).
Notably, the pregnancy and live birth rates in the
control group were higher than those expected. As the control group
didn't use any barrier device, the recurrence rate of adhesion
should be higher, but the pregnancy rate of the patients in the
control group was not significantly decreased compared with the
treatment group through repeated hysteroscopic treatment according
to the findings of the present study. This finding was further
supported by the study by Deans et al (13). In the aforementioned retrospective
study, including a total of 154 female patients, the pregnancy and
live birth rates were 79.0 and 63.7%, respectively, following
repeated hysteroscopic procedures until cavity restoration, without
the use of any mechanical barriers (13). The higher pregnancy rate recorded
in the control group compared with the treatment group in the
present study could be possibly due to the optimization of
endometrial proliferation and endometrial receptivity (14). A functional endometrium and an
adequate uterine cavity are closely associated with a successful
pregnancy (9,10). Although the success rate is
associated with the severity of adhesions (15,16),
early second-look hysteroscopy and appropriate adjuvant therapy can
exert satisfactory effects. A previous RCT has demonstrated that
the pregnancy rate in patients with moderate to severe IUAs is
improved by adjuvant therapy (5 mg/day transdermal estrogen and 100
mg/day aspirin) after hysteroscopic lysis (17). In the prospective trial by Pabuçcu
et al (11) the pregnancy
and live birth rates were compared between patients who underwent a
second-look hysteroscopy at 1 week and a third-look hysteroscopy at
2 months after the first hysteroscopy (Group A) and those who were
treated with second-look hysteroscopy 2 months later after the
first hysteroscopy (Group B). The results showed that both the
pregnancy and live birth rates were higher in Group A compared with
those recorded in Group B. However, statistical significance was
not reached (11). Therefore, this
study suggested that early second-look hysteroscopy may improve the
reproductive outcomes of patients with severe IUAs.
Τhe lower live birth rate in the copper-containing
IUD group could be due to the following two reasons: Firstly, it
has been reported that copper IUDs can induce an inflammatory
response in the endometrium (3).
Secondly, in the present study, 25 patients in the treatment group
and 8 patients in the control group changed their desire for
pregnancy after the first hysteroscopy. These patients were not
included in the statistical analysis. According to the AFS
classification of IUAs (18), a
range of live birth rate of 25-50% and a range of pregnancy rate of
50-75% is expected to be achieved in the copper IUD group.
Copper-containing IUDs could be an acceptable alternative approach
for preventing the recurrence of IUAs, when non-copper IUDs are not
available. However, no positive effects on pregnancy and live birth
rates were observed. Performing embryo transfer as soon as possible
could be a more effective strategy to achieve higher pregnancy and
live birth rates after hysteroscopy without the use of barrier
devices.
Only a limited number of studies have reported the
obstetric outcomes in patients with moderate to severe IUA treated
with hysteroscopy (13). In the
present study, the placental-related complication rate was 18.82%
(10/54). A total of 2 patients (2/54) underwent postpartum
hysterectomy due to postpartum hemorrhage caused by placenta
accreta spectrum. In addition, twin live birth, premature birth and
cesarean section rates of 14.81% (8/54), 9.26% (5/54) and 66.67%
(36/54), respectively, were recorded. The aforementioned results
were consistent with those reported by Deans et al (13). The aforementioned findings
suggested that the severity of IUAs could be positively associated
with obstetric outcomes. The 2 patients suffering from severe IUAs
eventually had their uterus removed.
In conclusion, the results of the current study
indicated that copper-containing IUDs had no positive effect on
pregnancy and live birth rates in patients with mild to severe IUAs
after hysteroscopic adhesiolysis.
Acknowledgements
We would like to thank Professor Zhenwei Xie for her
guidance throughout the study and Miss Zifei Zhou for her
contributions to the follow-up work of the present study (Women's
Hospital, School of Medicine, Zhejiang University, Hangzhou,
Zhejiang 310006, China).
Funding
Funding: This study was supported by the Science and Technology
Bureau Foundation of Jinhua (grant no. 2021-4-300).
Availability of data and materials
The data used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
PX, YS, JL and BY were responsible for study
conception and design, data analysis and first draft revision. HX
and QL were responsible for writing the first draft of the article,
data analysis and review. SL and EH contributed to data collection
and analysis and follow-up. All authors read and approved the final
manuscript. PX and BY confirm the authenticity of all the raw
data.
Ethics approval and consent to
participate
The study was approved by the Medical Ethics
Committee of the Affiliated Jinhua Hospital of Wenzhou Medical
University (approval no. IRB-20200028-R; Jinhua, China). All
patients signed an informed consent form.
Patient consent for publication
All patients provided written informed consent for
the publication of their data.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
AAGL Elevating Gynecologic Surgery. AAGL
practice report: Practice guidelines on intrauterine adhesions
developed in collaboration with the European society of
gynaecological endoscopy (ESGE). J Minim Invasive Gynecol.
24:695–705. 2017.PubMed/NCBI View Article : Google Scholar
|
|
2
|
March CM: Asherman's syndrome. Semin
Reprod Med. 29:83–94. 2011.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Yu D, Wong YM, Cheong Y, Xia E and Li TC:
Asherman syndrome-one century later. Fertil Steril. 89:759–779.
2008.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Rein DT, Schmidt T, Hess AP, Volkmer A,
Schöndorf T and Breidenbach M: Hysteroscopic management of residual
trophoblastic tissue is superior to ultrasound-guided curettage. J
Minim Invasive Gynecol. 18:774–748. 2011.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Lin XN, Zhou F, Wei ML, Yang Y, Li Y, Li
TC and Zhang SY: Randomized, controlled trial comparing the
efficacy of intrauterine balloon and intrauterine contraceptive
device in the prevention of adhesion reformation after
hysteroscopic adhesiolysis. Fertil Steril. 104:235–240.
2015.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Hanstede MM, van der Meij E, Goedemans L
and Emanuel MH: Results of centralized Asherman surgery, 2003-2013.
Fertil Steril. 104:1561–1568. 2015.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Khan Z and Goldberg JM: Hysteroscopic
management of Asherman's syndrome. J Minim Invasive Gynecol.
25:218–228. 2018.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Dreisler E and Kjer JJ: Asherman's
syndrome: Current perspectives on diagnosis and management. Int J
Womens Health. 11:191–198. 2019.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Lee WL, Liu CH, Cheng M, Chang WH, Liu WM
and Wang PH: Focus on the primary prevention of intrauterine
adhesions: Current concept and vision. Int J Mol Sci.
22(5175)2021.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Di Guardo F, Corte LD, Vilos GA, Carugno
J, Török P, Giampaolino P, Manchanda R and Vitale SG: Evaluation
and treatment of infertile women with Asherman syndrome: An updated
review focusing on the role of hysteroscopy. Reprod Biomed Online.
41:55–61. 2020.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Pabuccu R, Onalan G, Kaya C, Selam B,
Ceyhan T, Ornek T and Kuzudisli E: Efficiency and pregnancy outcome
of serial intrauterine device-guided hysteroscopic adhesiolysis of
intrauterine synechiae. Fertil Steril. 90:1973–1977.
2008.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Huang XW, Lin MM, Zhao HQ, Powell M, Wang
YQ, Zheng RR, Ellis LB, Xia WT and Lin F: A prospective randomized
controlled trial comparing two different treatments of intrauterine
adhesions. Reprod Biomed Online. 40:835–841. 2020.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Deans R, Vancaillie T, Ledger W, Liu J and
Abbott JA: Live birth rate and obstetric complications following
the hysteroscopic management of intrauterine adhesions including
Asherman syndrome. Hum Reprod. 33:1847–1853. 2018.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Konci R, Caminsky N, Tulandi T and Dahan
MH: Supplements to conventional treatment after hysteroscopic lysis
of intrauterine adhesions: A systematic review. J Obstet Gynaecol
Can. 42:984–1000. 2020.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Valle RF and Sciarra JJ: Intrauterine
adhesions: Hysteroscopic diagnosis, classification, treatment, and
reproductive outcome. Am J Obstet Gynecol. 158:1459–1470.
1988.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Pabuçcu R, Atay V, Orhon E, Urman B and
Ergün A: Hysteroscopic treatment of intrauterine adhesions is safe
and effective in the restoration of normal menstruation and
fertility. Fertil Steril. 68:1141–1143. 1997.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Chi Y, He P, Lei L, Lan Y, Hu J, Meng Y
and Hu L: Transdermal estrogen gel and oral aspirin combination
therapy improves fertility prognosis via the promotion of
endometrial receptivity in moderate to severe intrauterine
adhesion. Mol Med Rep. 17:6337–6344. 2018.PubMed/NCBI View Article : Google Scholar
|
|
18
|
The American Fertility Society. The
American fertility society classifications of adnexal adhesions,
distal tubal occlusion, tubal occlusion secondary to tubal
ligation, tubal pregnancies, müllerian anomalies and intrauterine
adhesions. Fertil Steril. 49:944–955. 1988.PubMed/NCBI View Article : Google Scholar
|