Introduction
Clinical treatment of post-traumatic chronic
osteomyelitis is challenging and complex. The therapeutic options
for this condition include the rational use of antibiotics,
excision of infected bones and the surrounding tissues,
reconstruction of soft tissues, bone stabilization and correction
of associated deformities (1). In
particular, the two-stage treatment approach of chronic
osteomyelitis described by Cierny and Mader has been accepted and
clinically used for >40 years (2). Osteomyelitis can be successfully
treated with debridement, but this typically results in bone and
soft tissue defects (3). The
induced membrane technique, also termed the Masquelet technique,
and distraction osteogenesis methods such as the Ilizarov technique
are widely used after debridement for the reconstruction of bone
defects (4,5).
The induced membrane technique is a two-stage
procedure, the first of which involves the implantation of a bone
cement spacer into the bone defect and surrounding area to induce
membrane formation. The second stage involves excision of the
spacer and the placement of autologous bone grafts. However, as it
is necessary to control infection and reconstruction during the
second stage, external fixation of the bone is not the optimal
choice, because it is bulky, uncomfortable and cumbersome to the
patients, causing inconvenience in day-to-day activities and
hindering ambulation. Therefore, although the external fixation
device used during the first stage may be retained during the
reconstruction of the bone defect, internal fixation may be used
instead (6,7). However, there is currently no
consensus on the optimum approach.
The application of the non-contact locking plate
technique, using locking plates as a unilateral external fixator by
percutaneous pinning, for bone defect reconstruction following
chronic osteomyelitis debridement has gradually increased (8,9). A
major advantage of the locking plate is that it provides angular
stability, which effectively promotes bone union by providing
optimal biological and mechanical environments. In addition, due to
this being a non-contact technique, the blood supply to the bone is
protected. Furthermore, the screws can be fixed to the locking
plate through the skin and soft tissues, which avoids bacterial
colonization and subsequent biofilm formation. The non-contact
locking plate technique has been used in the second-stage treatment
of post-traumatic tibial osteomyelitis since 2017 at the Department
of Orthopedics of Jinling Hospital (Nanjing, China). Based on these
cases at the Department of Orthopedics of Jinling Hospital, the aim
of the present study was to determine whether the non-contact
locking plate technique is a safe and feasible approach for the
surgical reconstruction of tibial segment defects.
Materials and methods
Patient selection
The present study was approved by The Ethics
Committee for Retrospective Research of Jinling Hospital (Nanjing,
China; approval no. 2021NZKY-030-07). All patients with
post-traumatic tibial osteomyelitis who underwent surgical
treatment using the two-stage treatment approach at Jinling
Hospital between January 2017 and September 2020 were included in
the study. The patients were divided into three groups according to
the method of fixation, namely the external fixation (EX), locking
plate (LP) and internal fixation (IX) groups. A total of 22
patients who retained unilateral external fixation during the
second stage were assigned to the EX group, 20 patients who changed
to non-contact locking fixation were assigned to the LP group, and
13 patients who changed to internal fixation were assigned to the
IX group. The inclusion criteria were as follows: i) Patients aged
18-70 years; ii) patients with osteomyelitis initially caused by
trauma or surgery; iii) patients with osteomyelitis graded as
IIIA/B or IVA/B according to the Cierny-Mader grading system
(10); and iv) patients with
>4-cm bone defects caused by radical debridement in the first
stage of treatment. The exclusion criteria were as follows: i)
Patients with osteomyelitis without tibial bone defects; ii)
patients with bone defects caused by factors other than trauma or
surgery, such as congenital defects, bone tumor resection and
simple aseptic non-union; iii) patients with bone defects that
required transarticular fixation; iv) patients with serious
comorbidities such as septic shock or uncontrolled infections; v)
patients who refused surgery; and vi) patients without follow-up
data. Based on the bone defects classification proposed by
Tetsworth et al (11), the
bone segment defects were classified as moderate (2-4 cm), major
(4-8 cm) and massive (≥8 cm). In the present study, patients with
moderate bone defects were not included according to the inclusion
criteria.
Treatment procedures
All patients with tibial chronic osteomyelitis
underwent the two-stage surgical procedure. In the first stage,
surgical debridement was performed to entirely clean the wound bed
until bleeding tissue was reached, ensuring that all the foci of
infection were removed. Then, antibiotic-impregnated cement spacers
were placed in the bone defect area and conventional external
fixators were used to stabilize the bone defects. In the second
stage, according to the condition of the soft tissue, the bone
defect location, the preference of the surgeon and the choice of
the patient, the external fixators were either retained or changed
to non-contact locking plates or internal plates.
After removal of the cement spacers, granulation
tissues were collected for microbial culture, and the bone defects
were filled with autogenous cancellous bone grafts. Depending on
the outcome of the bacterial culture, corresponding intravenous and
oral antibiotics were administered for 2-4 weeks to prevent the
recurrence of infection. Other patients with negative bacterial
culture were treated with an empirical choice of antibiotics in the
perioperative period to prevent infection for 3 days.
Clinical signs were observed and blood tests,
including C-reactive protein (CRP) and erythrocyte sedimentation
rate (ESR) tests, were conducted to assess the infection status of
the patient. The limbs were elevated after surgery, and the sutures
were removed 2-3 weeks later. Short-term non-weight-bearing
exercise was initiated on the second post-operative day while the
patient remained in a state of bedrest. Toe-touch weight-bearing
exercise with two crutches was initiated at 4-6 weeks post-surgery,
once X-rays indicated that the continuous callus passing through
the fracture line had become blurred. The exercise intensity and
duration were progressively increased until full weight-bearing
recanalization of the medullary cavity was accomplished.
Clinical data collection
The primary observational indices included bone
healing time and complications, while the secondary observational
indices were laboratory results and anxiety assessment. Baseline
data, including patient demographics, wound healing conditions,
bacterial culture results, complications, CRP levels and the ESR
before and 3 days post-surgery were collected. Imaging data,
including plain anteroposterior and lateral radiographs of the
involved limbs were also obtained. X-ray imaging was used to
monitor bone consolidation at 1.5, 3, 6, 9 and 12 months
post-surgery. Two surgeons prospectively evaluated the X-rays for
each patient. The duration of bone defect malunion and degrees of
deformity were also recorded. Clinical union was defined as
full-weight bearing ability without pain, and radiological union
was defined as the presence of a bridging callus of two cortices
visible in two plain X-ray views. The radiographical parameters
were assessed using lower leg radiographs obtained at the final
follow-up. The mechanical axis deviation, medial proximal tibial
angle, lateral distal tibial angle and limb length discrepancy were
also assessed. Manual goniometric measurements of the
radiographical parameters were performed for patients who were
examined by X-ray during the final follow-up at Jinling Hospital,
using Healthcare-Centricity RIS CE V3.0 (GE Healthcare) software.
For patients who underwent final follow-up X-rays at other
hospitals, the radiographical parameters were measured using
conventional radiographical hard images by two orthopedic surgeons
blinded to patient information. These measurements were performed
using a goniometer and repeated three times, with the average value
being recorded as the final result to avoid measurement errors.
The Hospital for Special Surgery Knee score
(12) and the American Orthopedic
Foot and Ankle Score (13) were
used to evaluate lower limb joint functions following second-stage
surgery, and scores >80 were considered to indicate normal
function. The Self-Rating Anxiety Scale (SAS) was also assessed
during follow-up (14).
Statistical analysis
SPSS software (version 22.0; IBM Corp.) and JMP
software (version 14.2; SAS Institute, Inc.) were used the perform
the statistical analyses. Data are presented as the median and
interquartile range (IQR) for continuous variables and as
percentages for dichotomous variables. The CRP/ESR values and time
to union in each group were compared using Kruskal-Wallis analysis.
Subsequently, Steel-Dwass post hoc tests were performed to evaluate
differences between specific pairs of groups. The χ2 or
Fishers' exact tests were used to analyze dichotomous variables and
the estimated P-values after these tests were adjusted by
Bonferroni correction. P<0.05 was considered to indicate a
statistically significant result.
Results
Patient information
A total of 55 eligible patients were included in the
study, including 44 (80.0%) males and 11 (20.0%) females (average
age, 50 years). Clinical information for all patients is provided
in Table SI. In the second
treatment stage, patients exhibited no symptoms of infection,
including pain, draining sinuses, swelling, local warmth, erythema
at the involved site, or necrosis of the wound edge. Furthermore,
levels of the inflammatory markers ESR and CRP were normal. The
average tibial bone defect of the patients was 5.6 (4.2-12.3) cm
and differences in initial bone defects among the groups were not
significant (Table I). A total of
41 patients had major defects, while 14 patients had massive
defects.
 | Table IUnion time and complications in the
follow-up interval. |
Table I
Union time and complications in the
follow-up interval.
| | Fixation type |
|---|
| Parameters | EX (n=22) | IX (n=13) | LP (n=20) | P-value |
|---|
| Defect size before
surgery, cm, median (IQR) | 4.5 (4.0-8.0) | 5.0 (4.2-8.0) | 4.6 (4.2-6.7) | >0.05 |
| Time to union,
months, median (IQR) | 13.1 (10.0-16.0) | 13.1 (12.0-15.0) | 12.3 (9.0-14.0) | >0.05 |
| Non-union, n (%) | 2 (9.1) | 1 (7.7) | 1 (5.0) | >0.05 |
| Pin-tract infection,
n (%) | 5 (22.7) | 0 (0.0) | 2 (10.0) | 0.003a, 0.005b |
| Pin or screw
loosening, n (%) | 3 (13.6) | 0 (0.0) | 1 (5.0) | 0.014a, 0.032b |
| Infection recurrence,
n (%) | 3 (13.6) | 2 (15.4) | 3 (15.0) | >0.05 |
Laboratory results
Prior to the second stage of treatment, no
differences in CRP levels were observed among the three groups and
the ESR levels in the IX group were higher than those in the EX
group (Table II). Furthermore,
the ESR levels after the second-stage surgery were significantly
higher in the IX group compared with the EX group (P=0.001;
Table II). Following the removal
of the cement spacers during surgery, granulation tissues were
collected from all patients for microbial culture.
Staphylococcus aureus was detected in 22.7, 30.8 and 20% of
patients in the EX, IX and LP groups, respectively. Other bacteria
were detected in 18.2, 7.7 and 15% of patients in the EX, IX and LP
groups, respectively.
 | Table IIMicrobes and inflammatory markers in
the second stage of treatment. |
Table II
Microbes and inflammatory markers in
the second stage of treatment.
| | Fixation type | |
|---|
| Parameters | EX (n=22) | IX (n=13) | LP (n=20) | P-value |
|---|
| Organisms cultured
after surgery, n (%) | | | | |
|
None | 13 (59.1) | 8 (61.5) | 13 (65.0) | >0.05 |
|
S.
aureus | 5 (22.7) | 4 (30.8) | 4 (20.0) | >0.05 |
|
Others | 4 (18.2) | 1 (7.7) | 3 (15.0) | >0.05 |
| Before surgery,
median (IQR) | | | | |
|
CRP,
mg/l | 4.1 (0.7-17.2) | 4.0 (0.7-10.5) | 3.6 (0.5-5.6) | >0.05 |
|
ESR,
mm/h | 4.9 (2.0-8.0) | 8.6 (2.4-34.3) | 7.5 (4.0-11.4) | 0.019a |
| Day 3 after surgery,
median (IQR) | | | | |
|
CRP,
mg/l | 15.2 (4.4-46.0) | 18.6 (2.7-92.7) | 9.4 (1.7-43.1) | >0.05 |
|
ESR,
mm/h | 10.8 (8.4-15.6) | 16.4 (10.2-34.3) | 12.3 (9.3-19.3) | 0.001a; 0.016b |
Clinical outcomes and
complications
In the EX group during follow-up, 20 patients
(90.9%) showed evidence of bone healing and had a median time to
union of 13.1 months (Table I).
However, 3 patients (13.6%) in this group had infection recurrence,
which exhibited as oozing pus in wounds and elevated inflammatory
cytokine levels. Also, 5 patients (22.7%) had pin-tract infections,
2 patients (9.1%) had non-union after 12 months of follow-up, and 3
patients (13.6%) had loosened pins (Table I). In addition, 8 patients had
shortened limbs and deformed tibia. A total of 5 out of 8 patients
had malformations causing limb shortening, with a mean
postoperative limb shortening length of 3.2 cm (IQR, 1.5-6 cm). Of
these patients, 3 patients also presented with tibial deformity.
One patient with limb shortening of 6 cm underwent the Ilizarov
procedure, while the other 4 patients did not undergo surgery. The
other 3 patients exhibited only tibial deformity. All 6 patients
with deformity, including 3 patients with concurrent shortened
limbs, had varus or valgus malalignment >2˚. One of these 6
patients had a distal tibial recurvatum of 11˚ but underwent no
further surgery. The proportion of cases with satisfactory
functional status, which was assessed based on the scores for knee
and ankle joint functions of the affected lower limb, were 81.8%
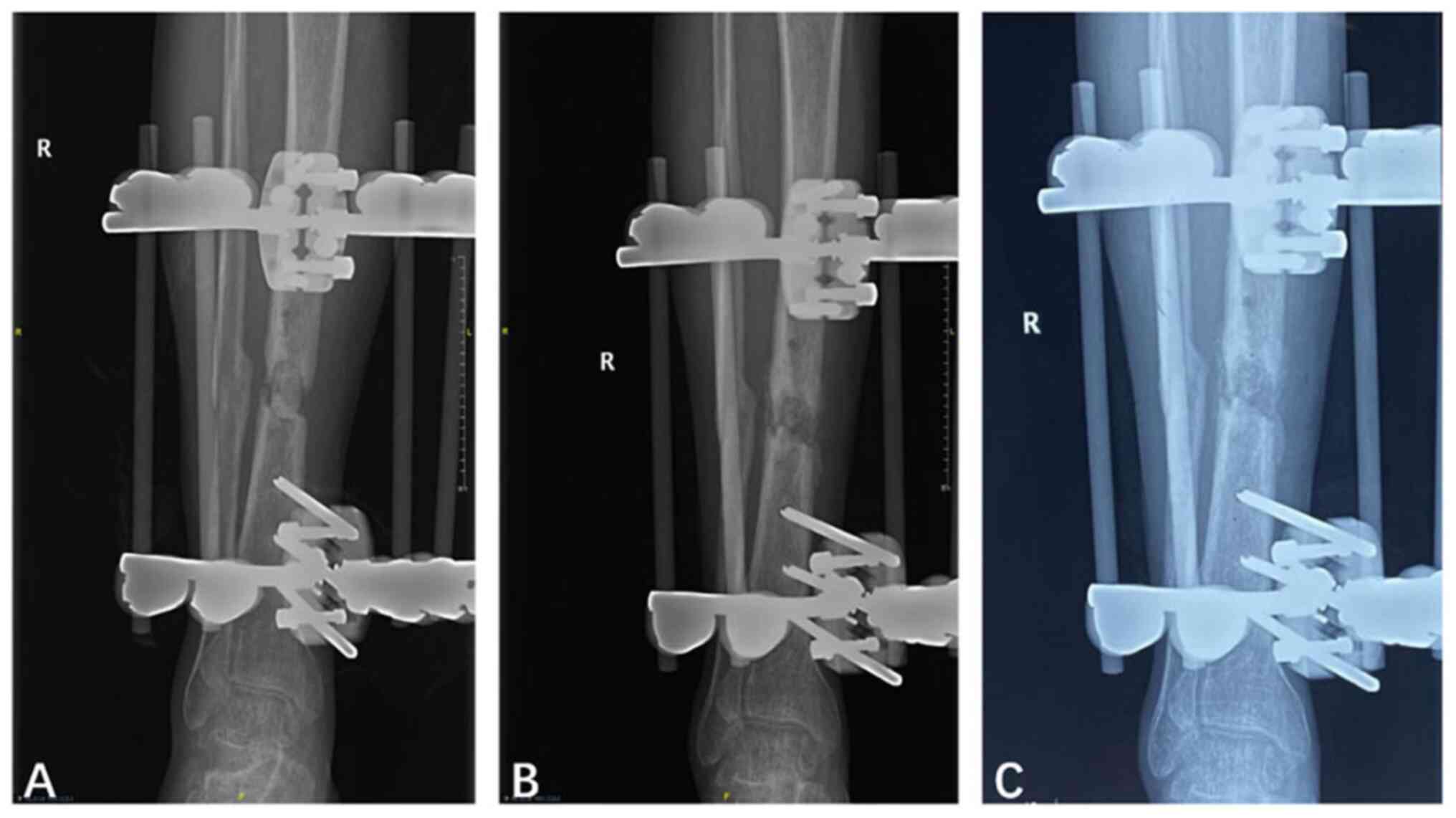
before surgery and 86.4% after surgery (Table III). Representative follow-up
X-ray images of patients who underwent bone grafting with retained
unilateral external fixation are shown in Fig. 1.
 | Table IIIFunctional and SAS assessment of the
enrolled patients. |
Table III
Functional and SAS assessment of the
enrolled patients.
| | Fixation type | |
|---|
| Parameters | EX (n=22) | IX (n=13) | LP (n=20) | P-value |
|---|
| Satisfactory
functional status, n (%) | | | | |
|
Before
surgery | 18 (81.8) | 11 (84.6) | 15 (75.0) | >0.05 |
|
After
surgery | 19 (86.4) | 12 (92.3) | 19 (95.0) | 0.034a, 0.046b |
| SAS assessment, n
(%) | | | | |
|
Mild
anxiety | 4 (18.2) | 5 (38.5) | 11 (55.0) | >0.05 |
|
Moderate
anxiety | 15 (68.2) | 7 (53.8) | 9 (45.0) | 0.028a, 0.017b |
|
Severe
anxiety | 3 (13.6) | 1 (7.7) | 0 (0.0) | 0.021a, 0.023b |
In the IX group, 12 patients achieved bone union
(92.3%), with a median union time of 13.1 months (Table I), while 1 patient had bone
non-union. Only 2 patients (15.4%) in this group had infection
recurrence. In addition, 1 patient had 9˚ malrotation of the
affected limb but did not undergo further surgery and 3 patients
had postoperative leg shortening (1.0-2.3 cm), while no patients
had a tibial varus of >2˚. The proportion of patients in the IX
group with a satisfactory functional status following surgery was
92.3%, which was significantly higher than that in the EX group
(P=0.034; Table III).
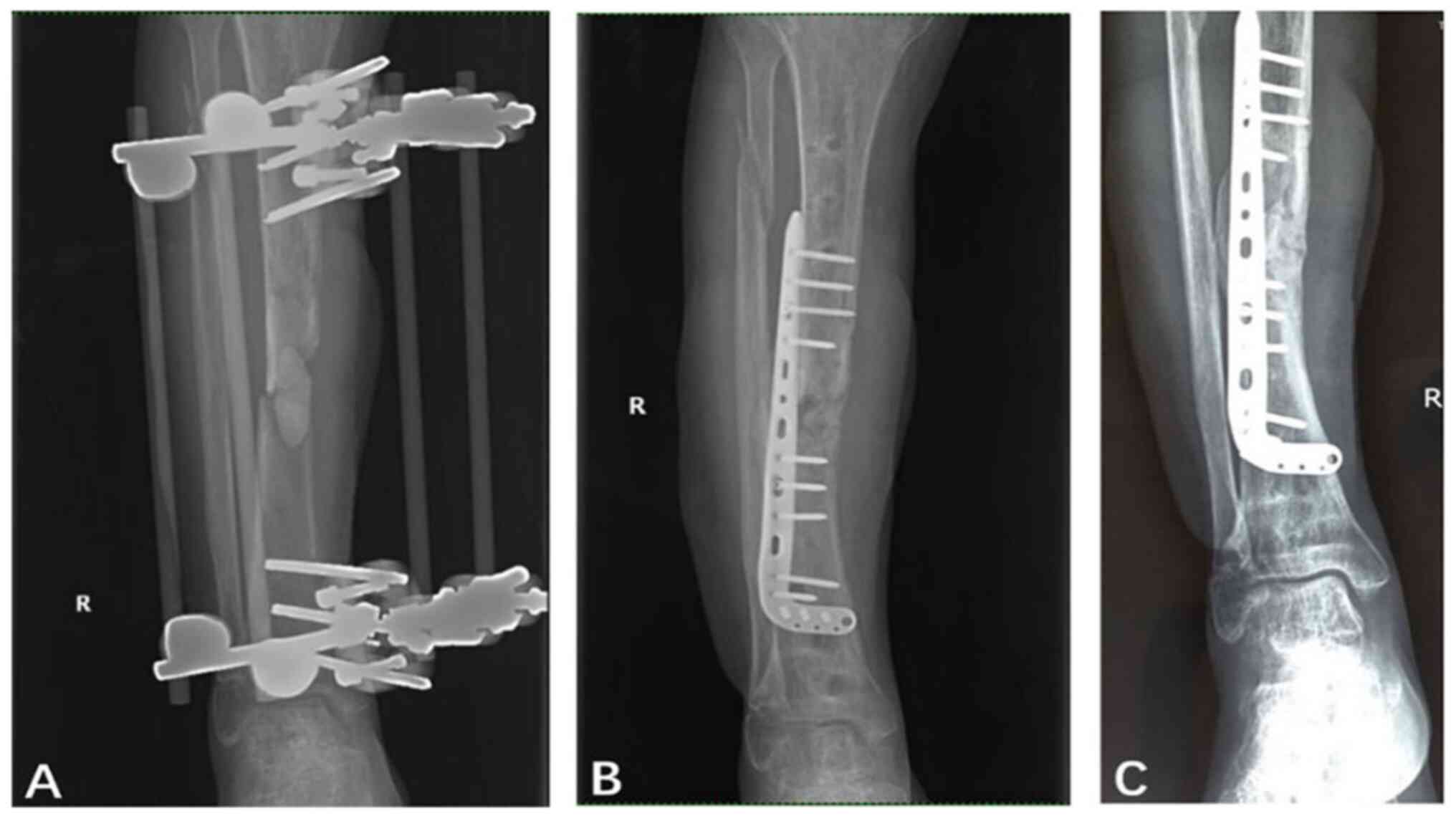
Representative follow-up X-ray images of patients who underwent
bone grafting and changed to internal fixation are shown in
Fig. 2.
In the LP group, 3 patients (15%) had infection
recurrence. In addition, 2 patients (10%) had pin-tract infection,
which was a significantly lower proportion than that in the EX
group (P=0.005; Table I).
Furthermore, 1 patient had a loosened screw and was not subjected
to any additional surgery. The patients in the LP group had a
median union time of 12.3 months (Table I). However, at the 12-month
follow-up, 1 patient exhibited non-union. A total of 3 patients
experienced tibial shortening, which included a 5˚ mild equinus
deformity in one case. In addition, a patient with a 15˚ tibial
procurvatum deformity at 2 years post-surgery was treated with
internal fixation. The proportion of patients in the LP group with
a satisfactory functional status post-surgery was improved to 95%
compared with that pre-surgery (75%). Notably, the proportion of
patients with a satisfactory functional status after surgery was
significantly higher in the LP group compared with the EX group
(P=0.046; Table III).
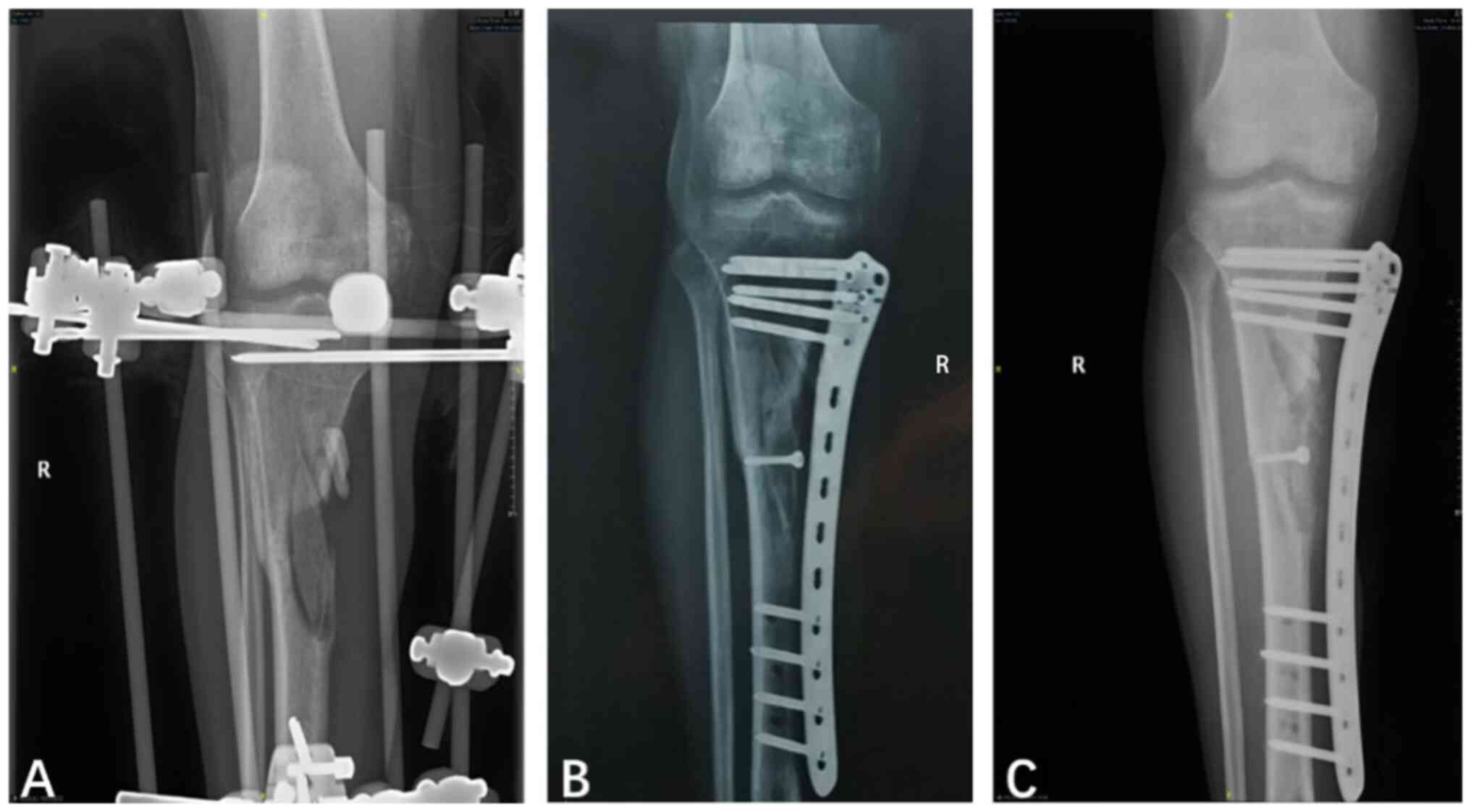
Representative follow-up X-ray images of patients who underwent
bone grafting and changed to non-contact locking plate fixation are
shown in Fig. 3.
SAS assessment
The SAS assessment demonstrated that the proportions
of patients with mild, moderate or severe anxiety were 38.5, 53.8
and 7.7% in the IX group, respectively; 55.0, 45.0 and 0.0% in the
LP group, respectively; and 18.2, 68.2 and 13.6% in the EX group,
respectively (Table III). The
proportion of patients with moderate or severe anxiety was lowest
in the LP group (45.0%). However, 81.8% of patients in the EX group
experienced moderate to severe anxiety.
Discussion
The tibia is the site where infected non-union and
chronic post-traumatic osteomyelitis most commonly occurs (15). Furthermore, the repair and
reconstruction approaches for infected tibial bone defects are
complex and require prolonged treatment and recovery (16). External fixation is widely used for
debridement during the first stage of the treatment of
post-traumatic tibial osteomyelitis. Compared with conventional
internal fixation, external fixation has less impact on soft tissue
and markedly reduces bacterial biofilm colonization. However,
external fixation is associated with certain risks, including pin
infection, deformity, joint stiffness, activity limitation,
pin-tract loosening and psychological disorders (17). The AO plate was designed according
to the concept and principles of the Association for the Study of
Internal Fixation, which is also referred to as the
Arbeitsgemeinschaft für Osteosynthesefragen (AO). Marti and van der
Werken (18) first proposed the
AO-plate method as an alternative to the use of conventional
external fixators. In addition, Apivatthakakul and Sananpanich
(19) reported the case of a large
distal tibial defect treated using a locking compression plate
(LCP) as an external fixator. The external locking plate has been
widely used to manage open fractures and infected non-unions
(8,9,18,19).
Thus, we hypothesized that the use of non-contact locking plates in
the second-stage treatment of tibial osteomyelitis combines the
advantages of conventional external and internal fixation.
In the present study, the use of the non-contact
locking plate technique provided similar fixation endurance and
time to bone-healing as were observed in the EX and IX groups.
Furthermore, the differences in the time to bone union and
recurrence rates of infection among the three groups were not
statistically significant. The SAS scores indicated that the
proportions of patients who had moderate or severe anxiety levels
were significantly reduced and the functional status after surgery
was significantly higher in the LP group compared with the EX
group. This difference may be due to the non-contact locking plate
technique improving compliance by the patient, since it is less
bulky and the device is lighter in weight compared with that used
for external fixation. However, following the one-stage debridement
surgery and the antibiotic treatment, the IX and LP groups
exhibited similar infection rates. In addition, angular malunion
occurred more frequently in the LP group compared with the IX
group. There may be two reasons for this, specifically selection
bias and different outcomes in the tibial force line. In the
present study, internal fixation was chosen for patients with
greater skin and soft-tissue resolution, which may have outweighed
the strengths of the non-contact locking plate technique in
infection prevention. In non-contact locking plate surgery, a good
reduction of the ends of the bone defect (restoration of the tibial
line and correction of the angulation, shortening and deformity)
before screw insertion is important but challenging to achieve.
Internal fixation provides additional biomechanical advantages
compared with fixation with an external locking plate. Therefore,
the non-contact locking plate technique should only be performed
when patients meet the surgical indications, but it is not
universally suitable.
Compared with internal fixation, the LCP technique
has several inherent advantages. First, for patients who require
removal of the plate after bone healing, the screws and LCP can be
removed in an outpatient setting under local anesthesia, which
avoids secondary cut-down surgery. Second, the non-contact plate
reduces compression of the periosteum and destruction of the local
blood circulation, providing an optimal environment for the bone
defect. Third, tibial soft tissue readily forms scars after trauma
or defects, resulting in a limited implant volume, which may not
provide an effective and complete coverage for internal fixation.
In the case of high skin tension after suturing, an external
locking plate is more appropriate. Fourth, load-sharing during
weight bearing may stimulate the development of calluses until bone
union occurs. In patients receiving an LCP, controlled stress
distribution or dynamization by removal of the screws closest to
the bone graft site is possible, which can provide a certain
measure of control of the load-sharing process (20).
There is a risk of secondary infection in external
fixation, including the use of conventional external fixators and
non-contact locking plates, in which bacterial infection extends
from the screws to the tibia. However, the majority of pin-tract
infections are superficial and only ~4% of cases present with deep
soft tissue infections and osteomyelitis (21). Furthermore, most pin-tract
infections can be eradicated by wound care and short-term oral
antibiotics. In the present study, 5 patients in the EX group,
including the patient shown in Fig.
1 who had an external fixator for >1 year, had pin-tract
infections, all of which were resolved by the use of dressings and
oral antibiotics. In the LP group, only 2 patients had a pin-tract
infection, which was a significantly lower incidence compared with
that in the EX group. We hypothesize that this may be due to the
following: i) Compared with the partially threaded screws of the
conventional external fixators, the fully threaded screws of the
LCP may attach more easily to subcutaneous tissue and skin; ii) the
LCP screws are shorter; and iii) the screw-loosening rate was
slightly lower in the LP group. Therefore, the risk of secondary
infection caused by biofilms extending from the screws may not be a
major issue if frequent daily care of the screws is performed.
However, due to concerns regarding the biomechanical
strength of the LCP, the application of this technology is limited.
Similar to the biomechanical principle of external fixation,
locking screws can directly lock into the plate to provide a stable
connection instead of relying on the compressive force provided by
the screw head against the plate and the friction between the plate
and bone. The length of the plate, the number of screws and the
distance from the plate to the bone surface are the main factors
affecting locking plate stiffness (22). Liu et al (23) conducted a biomechanical comparison
study and demonstrated that when an external fixator is used in the
treatment of distal tibia fracture, a distal femur LCP is preferred
over a distal tibial LCP. In the present study, when non-contact
locking plates were used to treat infectious bone defects of the
tibia, femoral plates with matching width screws were selected as
external fixators. No bending or breakage of plates was observed
for any of the patients in the LP group.
Kanchanomai and Phiphobmongkol (24) designed a biomechanical test for
tibial fractures externally fixed with an LCP, and reported that an
increased distance between the bone and the implant significantly
reduced construct stability. The authors recommended that the
distance between the bone and the plate should be 2 cm. However,
all models in the test were cyclically loaded with >500,000
cycles and did not exhibit any plate failure, indicating that
failure of the LCP is not a critical issue in clinical cases. The
angular stable interface between the screws and the plate is
designed to allow for placement of the plate without contact with
the bone, thus preserving periosteal blood supply and bone
perfusion, which may not be possible with internal fixation.
Notably, once the locking screws are placed on both sides of the
defect, it is not possible to adjust the plate as the adjustment
may increase the incidence of deformity and non-union (25,26).
In the present study, to achieve improved bone-matching, the plate
was temporarily secured using two Kirschner wires to provide
bicortical fixation and local stabilization. With regards to the
anatomy of the tibia and its relationship with peripheral nerves
and vessels, the medial tibia is a safe site at which to place the
locking screws. Intraoperative fluoroscopy is required to check
whether the locking screws penetrate through the joints when bone
defects are close to the joints.
There are several limitations associated with the
present study. First, this was a retrospective, single-center study
and the sample size was small due to the limited availability of
patients, which reduced the credibility of the experimental data
(type II error). Second, after measurements were repeated three
times the average value was determined to avoid measurement errors.
However, it may be more reliable to determine the average value
after removing the highest and lowest values of five measurements.
Third, this was not a randomized trial and selection bias may have
occurred. For example, the lower rate of complications in the IX
group was likely due to the selection of patients with good soft
tissue coverage for internal fixation treatment. Therefore, it is
important for the orthopedic surgeon to clearly understand the
operative indications when selecting the appropriate fixation
modality. Indeed, the selection of an external fixator, internal
plate or external non-contact locking plate depends on the
inclination of the surgeon and the preference of the patient, which
may be influenced by economic factors. The soft-tissue condition
and the location of the bone defect are important factors to be
considered when selecting the method of surgical reconstruction. In
the present study, an external non-contact locking plate was often
applied for bone defects in the middle segment of the tibia, while
an external fixator or internal plate was considered for bone
defects at the end of the tibia. However, there are other criteria
that were considered. For example, for patients with soft tissue
defects or a poor soft tissue condition, the external fixator was
retained after surgery. For patients with specific requirements
regarding the appearance and functionality of their limb, the
internal plate or external non-contact locking plate were selected.
In summary, the choice of fixation is based on the combined effects
of multiple factors, and it is challenging to identify the most
appropriate treatment for each patient. The fourth limitation of
the present study was that the IX group was defined as patients
receiving internal locking plate fixation, and several patients
with intramedullary nail fixation in the second-stage treatment
were not included. However, patients undergoing such treatment will
be evaluated in follow-up studies. Finally, the biomechanical
differences between the three groups were not analyzed, and this
merits further investigation.
In conclusion, the present study indicated that in
the second-stage treatment of post-traumatic tibial osteomyelitis,
the use of non-contact locking plate technology to treat >4-cm
bone defects achieved stable fixation, and reduced pin-tract
infections, pin loosening and the risk of biofilm formation.
Furthermore, the locking plate lowered the psychological anxiety of
the patients. Therefore, the non-contact locking plate technique is
a viable alternative for the second-stage treatment of
post-traumatic tibial osteomyelitis.
Supplementary Material
General characteristics of 55 patients
with post-traumatic tibial osteomyelitis.
Acknowledgements
Not applicable.
Funding
Funding: This study was supported by Jiangsu Commission of
Health Project (grant no. M2022070).
Availability of data and materials
Datasets of this study are not publicly available
due to study participants not giving their consent but may be
requested from the corresponding author upon request.
Authors' contributions
YZ participated in the inclusion of patients,
research design, collection of data, statistical analysis of the
results, and writing and revising the manuscript. PJ contributed to
researching the data and writing the discussion. ZH participated in
the inclusion of patients, collection of data, statistical analysis
of the results, writing and revising the manuscript, and the online
submission. HQ contributed to research design, writing and revising
the manuscript, online submission and funding acquisition. YZ, PJ,
ZH and HQ confirm the authenticity of the raw data. All authors
read and approved the final version of the manuscript.
Ethics approval and consent to
participate
The present retrospective analysis was approved by
The Ethics Committee for Retrospective Research of Jinling Hospital
(Nanjing, China; approval no. 2021NZKY-030-07) and completed in
accordance with the Declaration of Helsinki. All patients provided
written informed consent to participate.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Patzakis MJ and Zalavras CG: Chronic
posttraumatic osteomyelitis and infected nonunion of the tibia:
Current management concepts. J Am Acad Orthop Surg. 13:417–427.
2005.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Cierny G and Mader JT: Adult chronic
osteomyelitis. Orthopedics. 7:1557–1564. 1984.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Qin C, Xu L, Liao J, Fang J and Hu Y:
Management of osteomyelitis-induced massive tibial bone defect by
monolateral external fixator combined with antibiotics-impregnated
calcium sulphate: A retrospective study. Biomed Res Int.
2018(9070216)2018.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Feng D, Zhang Y, Jia H, Xu G, Wu W, Yang
F, Ding J, Li D, Wang K, Luo Y, et al: Complications analysis of
Ilizarov bone transport technique in the treatment of tibial bone
defects-a retrospective study of 199 cases. BMC Musculoskelet
Disord. 24(864)2023.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Wang X, Luo F, Huang K and Xie Z: Induced
membrane technique for the treatment of bone defects due to
post-traumatic osteomyelitis. Bone Joint Res. 5:101–105.
2016.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Pesch S, Hanschen M, Greve F, Zyskowski M,
Seidl F, Kirchhoff C, Biberthaler P and Huber-Wagner S: Treatment
of fracture-related infection of the lower extremity with
antibiotic-eluting ceramic bone substitutes: Case series of 35
patients and literature review. Infection. 48:333–344.
2020.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Mathieu L, Tossou-Odjo L, de l'Escalopier
N, Demoures T, Baus A, Brachet M and Masquelet A: Induced membrane
technique with sequential internal fixation: Use of a reinforced
spacer for reconstruction of infected bone defects. Int Orthop.
44:1647–1653. 2020.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Tulner S, Strackee S and Kloen P:
Metaphyseal locking compression plate as an external fixator for
the distal tibia. Int Orthop. 36:1923–1927. 2012.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Blažević D, Kodvanj J, Adamović P, Vidović
D, Trobonjača Z and Sabalić S: Comparison between external locking
plate fixation and conventional external fixation for
extraarticular proximal tibial fractures: A finite element
analysis. J Orthop Surg Res. 17(16)2022.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Cierny G III, Mader JT and Penninck JJ: A
clinical staging system for adult osteomyelitis. Clin Orthop Relat
Res. 7–24. 2003.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Tetsworth K, Burnand H, Hohmann E and
Glatt V: Classification of bone defects: An extension of the
orthopaedic trauma association open fracture classification. J
Orthop Trauma. 35:71–76. 2021.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Kubiak G and Fabiś J: To compare the
results of knee evaluation after meniscus repair and anterior
cruciate ligament reconstruction on the basis of Lysholm, HSS and
IKDC scoring systems. Pol Orthop Traumatol. 77:127–131.
2012.PubMed/NCBI
|
|
13
|
Shazadeh Safavi P, Janney C, Jupiter D,
Kunzler D, Bui R and Panchbhavi V: A systematic review of the
outcome evaluation tools for the foot and ankle. Foot Ankle Spec.
12:461–470. 2019.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Olatunji BO, Deacon BJ, Abramowitz JS and
Tolin DF: Dimensionality of somatic complaints: Factor structure
and psychometric properties of the self-rating anxiety scale. J
Anxiety Disord. 20:543–561. 2006.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Patzakis MJ, Abdollahi K, Sherman R,
Holtom PD and Wilkins J: Treatment of chronic osteomyelitis with
muscle flaps. Orthop Clin North Am. 24:505–509. 1993.PubMed/NCBI
|
|
16
|
Tetsworth K and Cierny G III:
Osteomyelitis debridement techniques. Clin Orthop Relat Res. 87–96.
1999.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Abulaiti A, Yilihamu Y, Yasheng T, Alike Y
and Yusufu A: The psychological impact of external fixation using
the Ilizarov or Orthofix LRS method to treat tibial osteomyelitis
with a bone defect. Injury. 48:2842–2846. 2017.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Marti R and van der Werken C: The AO-plate
for external fixation in 12 cases. Acta Orthop Scand. 62:60–62.
1991.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Apivatthakakul T and Sananpanich K: The
locking compression plate as an external fixator for bone transport
in the treatment of a large distal tibial defect: A case report.
Injury. 38:1318–1325. 2007.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Woon YL, Wong MK and Howe TS: LCP external
fixation-external application of an internal fixator: Two cases and
a review of the literature. J Orthop Surg Res. 5(19)2010.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Parameswaran AD, Roberts CS, Seligson D
and Voor M: Pin tract infection with contemporary external
fixation: How much of a problem? J Orthop Trauma. 17:503–507.
2003.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Stoffel K, Dieter U, Stachowiak G, Gächter
A and Kuster M: Biomechanical testing of the LCP-how can stability
in locked internal fixators be controlled? Injury. 34 (Suppl
2):B11–B19. 2003.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Liu W, Yang L, Kong X, An L, Hong G, Guo Z
and Zang L: Stiffness of the locking compression plate as an
external fixator for treating distal tibial fractures: A
biomechanics study. BMC Musculoskelet Disord. 18(26)2017.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Kanchanomai C and Phiphobmongkol V:
Biomechanical evaluation of fractured tibia externally fixed with
an LCP. J Appl Biomech. 28:587–592. 2012.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Röderer G, Abouelsoud M, Gebhard F,
Böckers TM and Kinzl L: Minimally invasive application of the
non-contact-bridging (NCB) plate to the proximal humerus: An
anatomical study. J Orthop Trauma. 21:621–627. 2007.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Alemdar C, Azboy I, Atiç R, Özkul E, Gem M
and Kapukaya A: Management of infectious fractures with
‘Non-Contact Plate’ (NCP) method. Acta Orthop Belg. 81:523–529.
2015.PubMed/NCBI
|