Introduction
The rates of caesarean section (CS) have increased
globally from 7% in 1990 to 21% in 2023(1), and are particularly high in
developing countries (30-35%) (2-4).
Numerous studies have revealed that previous CS is associated with
an increased risk of infections and postpartum haemorrhage, as well
as an increased incidence of obstetric complications, such as
abnormal placentation and risk of uterine rupture, in subsequent
pregnancies (5). Additionally,
42-58% of women who underwent CS reported post-caesarean scar
defects (PCSD), such as isthmocele (an iatrogenic defect in the
myometrium at the site of a previous caesarean scar due to
defective tissue healing) (6).
While the incidence of PCSD is 61% in women who have had one
previous CS, it reaches 100% in women who have had at least three
CS (5,7).
Correlation between previous CS, fertility and other
pregnancy outcomes is still not clear. While a previous study
reported reduced fertility and live birth rates subsequent to
previous CS (8), another study
claimed that previous CS has only marginal impact on future
fertility and that clinical and societal factors, leading to higher
CS rates, may have a greater impact on reproductive health than CS
itself (9). Since the use of
assisted reproductive technology (ART) continues to rise globally
(10), there is an increasing need
to understand the implications of previous CS for maternal and
fetal health. A previous study suggested that previous CS is
correlated with lower subsequent clinical pregnancy rates (CPR) and
longer time to conceive compared with natural vaginal delivery
(NVD) (11). However, the true
impact of previous CS on subsequent pregnancies remains unclear.
The latest meta-analysis exploring the same research topic by Zhao
et al (12) (2021),
included just seven studies and lacks a comprehensive analysis of
maternal and neonatal outcomes. Thus, in the present systematic
review and meta-analysis the effects of previous CS compared with
normal vaginal delivery (NVD) were analysed with regard to the
following: i) The reproductive outcomes such as live birth rate
(LBR), biochemical pregnancy rate (BPR), clinical pregnancy rates
(CPR), implantation rate (IR) and ectopic pregnancy rate (EPR); ii)
pregnancy outcomes including preterm birth rate (PBR), still birth
rate (SBR), miscarriage rate (MR), birth defects (BD), birth weight
(BW) and multiple pregnancy rate (MPR); and iii) other outcomes
such as endometrial thickness (EMT) and difficult transfer rate
(DTR).
The present systematic review and meta-analysis
aimed to summarize and analyse data of all reproductive, pregnancy
and perinatal outcomes in women who underwent ART treatment after
previous CS.
Patients and methods
Protocol registration and methodology. The
present study was registered at PROSPERO (an international database
of systematic review protocols; no. CRD42023468689). The latest
(2020) ‘Preferred Reporting Items for Systematic Reviews and
Meta-Analyses (PRISMA)’ framework was used to report the findings
of the present study (13).
Ethical approval was not obtained, since only information that was
freely available across various databases was utilized.
Inclusion criteria. Studies that included the
following were selected: i) Studies reporting on pregnant women who
underwent ART; ii) studies reporting on women with previous CS and
ART; iii) studies reporting on women with previous NVD and ART; iv)
studies reporting various reproductive, pregnancy and neonatal
outcomes; and v) analytical studies including cross sectional,
prospective and retrospective observational, as well as case
control studies.
Exclusion criteria. Studies with the
following characteristics were excluded: i) Studies without a
control group of patients who underwent vaginal birth; and ii)
studies without follow-up records, with inadequate data, not
peer-reviewed, and grey literature (policy reports, newsletters and
working papers). In addition, only articles published in the
English language across Medline (https://pubmed.ncbi.nlm.nih.gov), Google Scholar
(https://scholar.google.com) and Science
Direct (https://www.sciencedirect.com)
databases, from inception until October 2023 were included.
Search strategy. Medical Subject Heading
terms such as: ‘Previous C section’ OR ‘Previous Caesarean section’
AND ‘Previous Vaginal delivery’ AND ‘In vitro fertilisation’
OR ‘Assisted reproductive techniques’ OR ‘Embryo transfer’ AND
‘Observational studies’ OR ‘Cohort studies’ OR ‘Prospective
studies’ were utilized to search in the three aforementioned
databases. No geographical limitations were considered.
Additionally, studies that were missed by computerised searches
were examined by searching the reference lists of all qualifying
articles and were included if found eligible. Two primary
investigators (DC and LC) independently conducted the search and
assessed the quality of individual studies. All cases of
disagreements were resolved by consensus. The detailed search
strategy is presented in Table
SI.
Outcome parameters and operational
definitions. The primary outcomes of interest were:
Reproductive outcomes such as CPR, defined as the presence of an
intrauterine gestational sac through ultrasound confirmation; LBR,
defined as the birth of a live fetus 24 weeks after conception;
EPR, defined as the presence of an extrauterine gestational sac
through ultrasound confirmation; MR, defined as pregnancy loss
before 12 weeks of gestation; BPR, defined as an elevated serum
level of β-human chorionic gonadotropin [>5 IU/l] after 14 days;
SBR, defined as the delivery of a fetus with no signs of
viability/after 28 weeks; and IR. Secondary outcomes of interest
were: PBR, defined as the delivery of a live fetus before 37
completed weeks; as well as EMT, BW, MPR, DTR and BD.
Data extraction and management. Relevant
information such as the details of the authors, study design,
duration, sample size, geographical location, inclusion criteria,
embryo transfer type and relevant primary and secondary outcomes
were extracted and entered in the data documentation sheet.
Statistical analysis. The extracted data were
analysed using Stata 14.2 (StataCorp LLC). Each data entry was
double-checked by the investigators. The effect across studies was
pooled for binary outcomes through the inverse variance method
using risk ratios (RR) with a 95% confidence interval (CI), and
continuous outcomes as a mean difference with a 95% CI. In case of
missing data, efforts were made to contact the author for necessary
information, such as data pertaining to the study period, mean age
distribution of cases and controls and other information necessary
for assessing the quality of the studies. In all cases where it was
not possible to obtain the necessary data, it was considered not
reported. Pooled effect sizes were graphically represented as
forest plots and publication bias was graphically represented as
funnel plots and was statistically tested using Egger's test
(14). P<0.05 was considered to
indicate a statistically significant difference.
Assessment of heterogeneity. The
I2 statistic and the Chi-square heterogeneity test were
used to examine the between-study variability. Three levels of
heterogeneity were identified: Mild (I2<25%),
moderate (I2=25-75%) and considerable
(I2>75%).
Quality of the included studies. Quality of
the included studies was assessed using the Newcastle Ottawa Scale
(NOS) (15). The scale assesses
the quality of studies using three criteria: Ascertainment of
outcome, selection and comparability of the study groups. A study
may receive a maximum of one star for each numbered item in the
selection and outcome categories. For comparability, a maximum of
two stars may be assigned. Thus, the maximum NOS score is nine.
Results
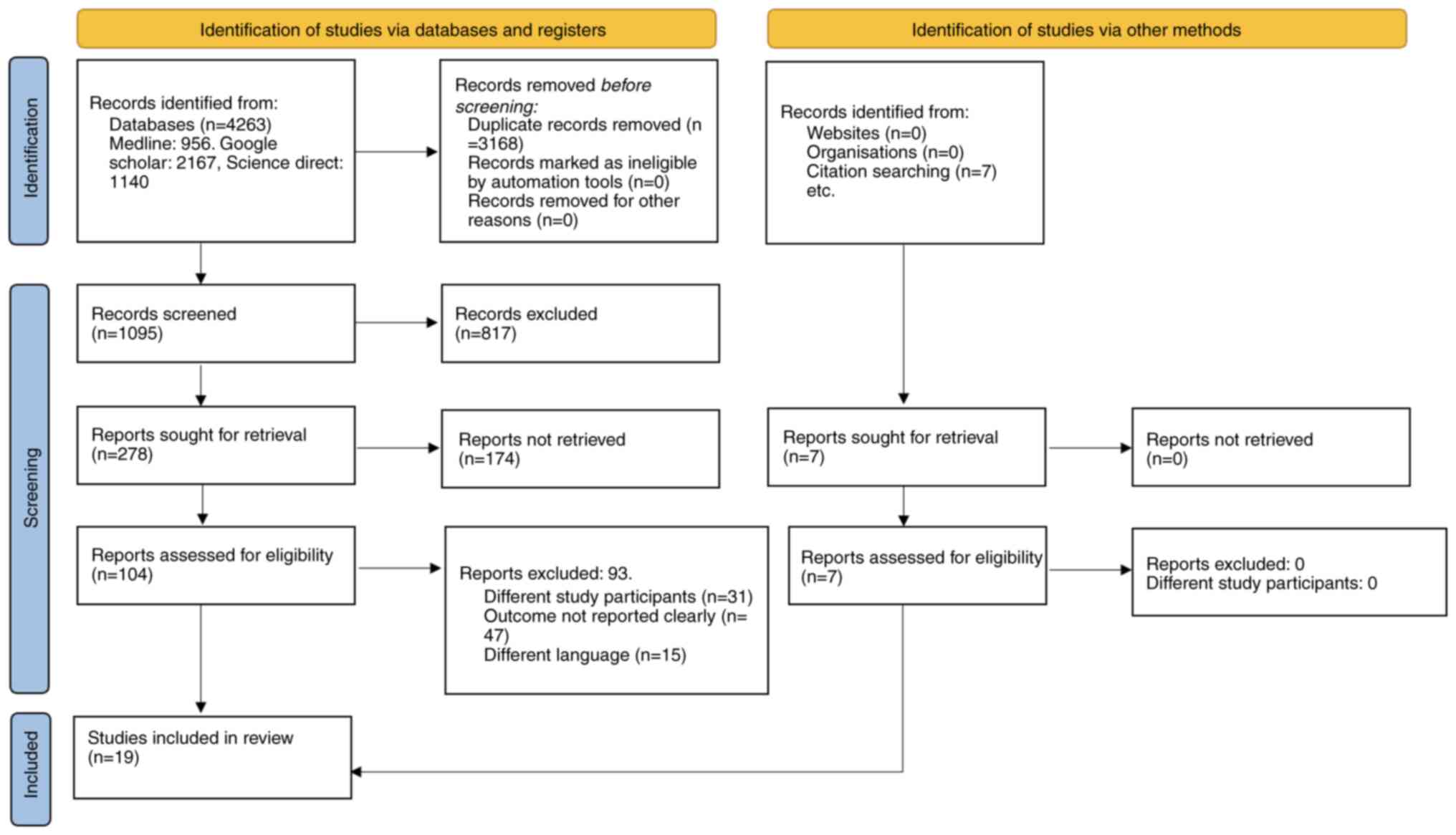
Study selection. A total of 4,263 articles
were identified by the literature search across the databases. Of
these, 3,168 were removed as duplicates. Another 817 articles were
excluded after screening the title and abstract. From the remaining
278 studies, 104 free full text articles were retrieved. Finally, a
total of 19 articles that met eligibility criteria, were selected
for the present systematic review and meta-analysis (16-34).
In total, 18 studies reported on the LBR (16-33),
17 reported on the CPR (16-32),
17 on the MR (16-29,31-33),
16 on the EPR (16-29,31,32),
13 on the BPR (16-21,23-25,27,29,32,33),
nine on the PBR (19,20,22,24,25,28,29,32,34),
eight studies on the EMT (16,17,19,20,22,24,30,33),
seven each on the MPR (16,19,20,23,25,28,32),
SPR (19,20,22,24,26,29,32)
and IR (16,19,20,24,27,32,33),
five on the BW (19,20,24,31,32),
three on the DTR (17,19,24)
and two on the BD (20,32) respectively. The PRISMA 2020 flow
diagram is explained in Fig.
1.
Characteristics of the included studies.
General characteristics of the included studies are detailed in
Table I. Of the 19 studies
included, 11 were from China, two were from the Netherlands and the
USA, and one study each from Turkey, Canada, Germany and UAE. All
studies reported results in English. The sample size of the
included studies ranged between 150 to 9,124. Most (17/19) studies
were retrospective cohort studies, one was a prospective cohort
study and one was a retrospective case control study.
 | Table ICharacteristics of the 19 included
studies. |
Table I
Characteristics of the 19 included
studies.
| First author,
year | Country | Sample size | Study type | Study duration | Eligibility | Age (median and
range/mean SD) | Outcomes | Quality of study
(NOS) | (Refs.) |
|---|
| Gale et al,
2022 | Canada | 962 | Retrospective
cohort | January 1, 2013 to
September 1, 2019 | Cases: Patients
with at least one prior delivery beyond 20 weeks' gestation who
underwent their first ET after a delivery; patients in the
caesarean delivery group had a history of one or more caesarean
deliveries, regardless of prior VD history | Cases:
35.2±4.2 | CPR, EPR, LBR, MR
and SBR | 7 | (26) |
| | | | | | Controls: Infertile
women with only one previous VD; the first fresh ET | Controls:
34.9±4.1 | | | |
| Cai et al,
2022 | China | 8,494 | Retrospective
cohort | January 2014 to
July 2020 | Cases: Women
undergoing IVF/ICSI with a previous CS | Cases:
36.49±4.19 | CPR, EPR, LBR, MR,
BPR and IR | 9 | (27) |
| | | | | | Controls: Women
undergoing IVF/ICSI with a previous VD | Controls:
37.32±4.86 | | | |
| Wang et al,
2022 | China | 4,158 | Retrospective
cohort | January 2015 to
April 2019 | Cases: Patients
included in this study at least one previous delivery (including CS
and VD) | Cases:
35.52±4.71 | CPR, EPR, LBR, MR,
BPR, PBR and SBR | 8 | (29) |
| | | | | | Controls: Women
undergoing IVF/ICSI with a previous VD | Controls:
36.81±5.00 | | | |
| Zhang et al,
2022 | China | 993 | Retrospective
cohort | January 2014 to
January 2020 | Cases: Women who
received their first FET cycle after a freeze-all policy, had a
history of only one parturition (after 28 weeks of pregnancy) and
were aged <40 years with previous CS | Cases:
33.5±3.7 | CPR, EPR, LBR, MR,
PBR and MPR | 7 | (28) |
| | | | | | Controls: Women
undergoing IVF/ICSI with a previous VD | Controls:
33.8±3.9 | | | |
| Bayram et
al, 2022 | Germany | 412 | Retrospective
cohort | March 2017 to
October 2019 | Cases: Patients
with secondary infertility and at least one previous caesarean
delivery | Cases: 35.0
(4.6) | CPR, LBR and
ET | 8 | (30) |
| | | | | | Controls: Women
undergoing IVF/ICSI with a previous VD | Controls: 34.1
(5.0) | | | |
| Diao et al,
2021 | China | 760 | Retrospective
cohort | January 2015 to
December 2019 | Cases: All women
with secondary infertility and a history of delivery who underwent
IVF/ICSI-ET treatment (patients having a history of a previous
delivery beyond 5 months gestation; on treatment with either a long
mid-luteal GnRH antagonist or GnRH antagonist ovarian stimulation
protocol; undergoing a first fresh ET) | Cases:
35.11±3.97 | CPR, EPR, LBR, MR
and BW | 8 | (31) |
| | | | | | Controls: Women
undergoing IVF/ICSI with a previous VD | Controls:
35.05±4.51 | | | |
| Asoglu et
al, 2021 | Turkey | 150 | Retrospective
cohort | 2017-2018 | Cases: Women
undergoing IVF/ICSI with a previous CS | Cases: 34.5±5 | CPR, EPR, LBR, MR,
BPR and MPR | 8 | (23) |
| | | | | | Controls: Women
undergoing IVF/ICSI with a previous VD | Controls:
34.6±4.8 | | | |
| Chen et al,
2021 | China | 5,479 | Retrospective
cohort | 2014-2017 | Cases: All women
with secondary infertility and a history of delivery who underwent
IVF/ICSI-ETtreatment with at least one good embryo; FSH ≤10 mIU/ml;
BMI ≤30 kg/m2; endometrial thickness of ET day ≥8
mm] | Not reported | CPR, EPR, LBR, MR,
BPR, PBR and MPR | 7 | (25) |
| | | | | | Controls: Women
undergoing IVF/ICSI with a previous VD | | | | |
| Wang et al,
2020 | China | 1,076 | Retrospective
cohort | January 2015 to
December 2016 | Cases: Women
undergoing IVF/ICSI with a previous CS | Cases:
35.4±4.5 | CPR, EPR, LBR, MR,
PBR, SBR, ET and IR | 8 | (22) |
| | | | | | Controls: Women
undergoing IVF/ICSI with a previous VD | Controls:
37.4±5.2 | | | |
| Huang et al,
2020 | China | 2,046 | Retrospective
cohort | January 2013 to
December 2018 | Cases: Infertile
women with a prior live birth delivery and undergoing their first
FET cycles after a freeze-all policy | Cases:
37.2±5.5 | CPR, EPR, LBR, MR,
BPR, MPR, ET and IR | 8 | (16) |
| | | | | | Controls: Infertile
women with history of VD only | Controls:
36.2±5 | | | |
| Vissers et
al, 2020 | Netherlands | 1,317 | Retrospective
cohort | 2006 to 2016 | Cases: Infertile
women with only one previous CS; the first | Cases:
36.6±3.6 | CPR, EPR, LBR, MR,
BPR,PBR, SBR,ET,BW, IR and DTR | 8 | (24) |
| | | | | | Controls: Infertile
women with only one previous VD; the first fresh ET first fresh
ET | Controls:
36.2±3.8 | | | |
| Lawrenz et
al, 2020 | UAE | 495 | Retrospective
cohort | 2018-2019 | Cases: Infertile
women with only one previous CS; the first fresh ET | Cases:
37.1±3.6 | CPR, EPR, LBR, MR
and BPR | 8 | (21) |
| | | | | | Controls: Infertile
women with only one previous VD; the first fresh ET | Controls:
38.4±3.2 | | | |
| Jacob et al,
2019 | China | 1,793 | Retrospective
cohort | 2015-2016 | Cases: Infertile
women with only one previous CS; the first fresh ET | Cases:
35.4±3.3 | CPR, EPR, LBR, MR,
BPR, PBR, MPR, SBR, BD and BW | 7 | (32) |
| | | | | | Controls: Infertile
women with only one previous VD; the first fresh ET | Controls:
36.1±3.7 | | | |
| Van den Tweel et
al, 2022 | Netherlands | 530 | Retrospective
cohort | January 2005 to
June 2016 | Cases: Subfertile
women with previous CS undergoing IVF/ICSI (with a previous live
birth who tried for a second child using IVF/ICSI and had at least
one ET) | Cases:
34.5±3.8 | CPR, EPR, LBR, MR
and BPR | 7 | (18) |
| | | | | | Controls:
Subfertile women with previous VD receiving IVF/ICSI | Controls:
34.4±3.9 | | | |
| Wang et al,
2017 | China | 310 | Retrospective case
control | January 2013 to
December 2015 | Cases: Subfertile
women with prior CS undergoing IVF/ICSC and fresh ET | Cases:
33.9±3.1 | CPR, EPR, LBR, MR,
BPR, MPR, SBR, IR, ET, BW and DTR | 8 | (19) |
| | | | | | Controls: Infertile
women with only one previous VD and undergoing IVF-ET | Controls:
34.1±3.1 | | | |
| Patounakis et
al, 2016 | USA | 194 | Prospective
cohort | March 2008 to May
2014 | Cases: Infertile
women with single or multiple previous CS (women with a history of
a previous delivery beyond 20 weeks of gestation) | Cases:
35.3±4.2 | CPR, EPR, LBR, MR,
BPR, ET and DTR | 9 | (17) |
| | | | | | Controls: Infertile
women with previous VD | Controls:
35.6±4.3 | | | |
| Zhang et al,
2016 | China | 231 | Retrospective
cohort | January 2012 to
September 2014 | Cases: Infertile
women with previous CS undergoing IVF-ET | Cases:
33.5±3.7 | CPR, EPR, LBR, MR,
BPR, PBR, MPR, SBR, ET,BD, IR and BW | 8 | (20) |
| | | | | | Controls: Infertile
women with previous VD undergoing IVF-ET | Controls:
33.8±3.8 | | | |
| Friedenthal et
al, 2021 | USA | 525 | Retrospective
cohort | 2012 to 2020 | Cases: Subfertile
women with prior CS undergoing IVF-ET | Cases:
37.4±3.6 | ET, IR, PBR, MR and
LBR | 8 | (33) |
| | | | | | Controls: Infertile
women with only one previous VD undergoing IVF-ET | Controls:
36.9±3.9 | | | |
| Lin et al,
2022 | China | 9,124 | Retrospective
cohort | April 2014 to April
2020 | Cases: Subfertile
women with prior CS undergoing IVF-ET | Not reported | PBR | 7 | (34) |
| | | | | | Controls: Infertile
women with only one previous VD undergoing IVF-ET | | | | |
Excluded studies. Of the 104 full-text
articles extracted, 93 studies were excluded during secondary
screening. Specifically, 31 were excluded as they had mixed study
participants groups, 47 did not report the outcome clearly and 15
were published in languages other than English.
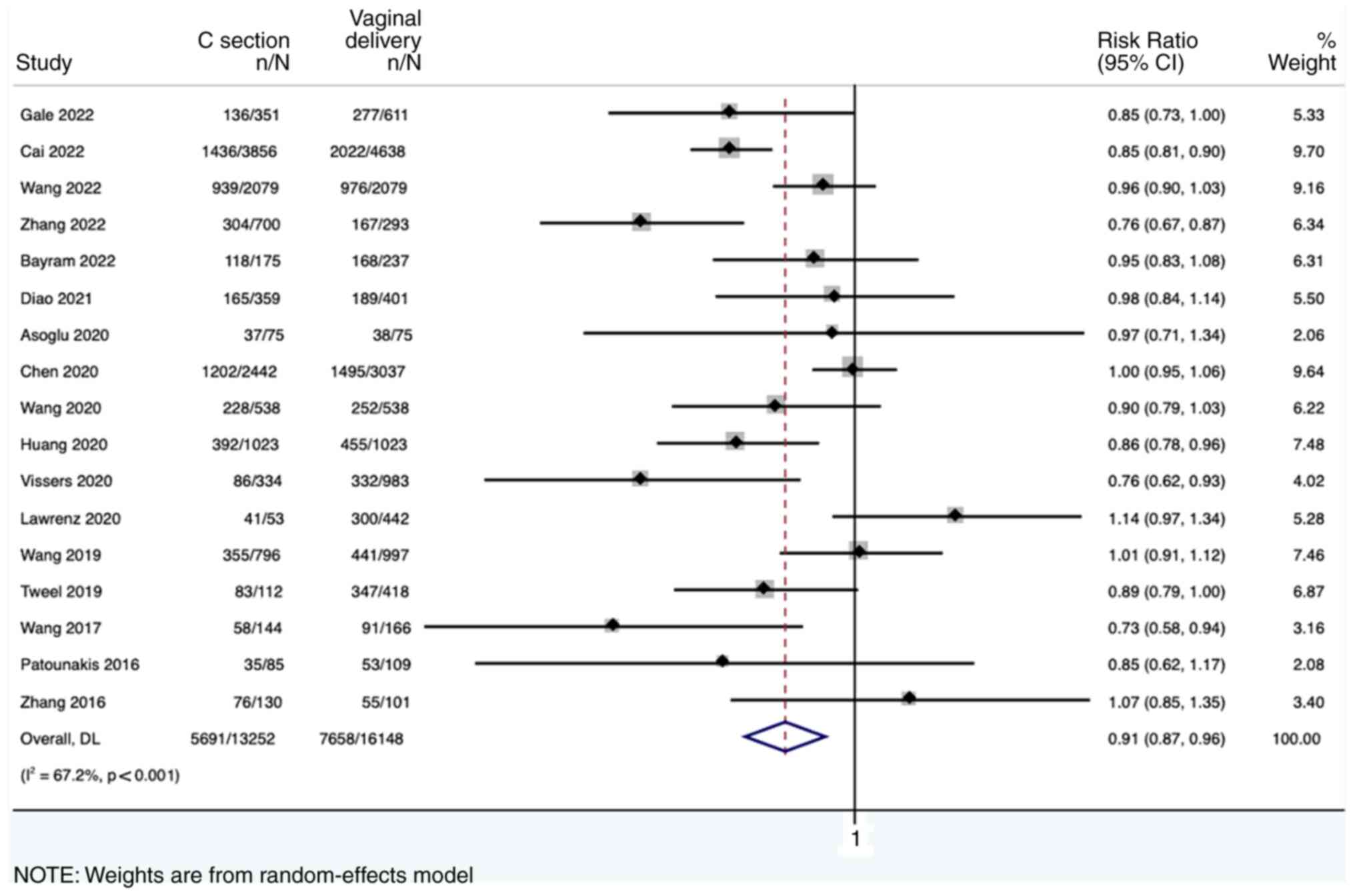
Reproductive outcomes across the study
groups. A total of 17 studies (n=29,400; CS=13,252 and
NVD=16,148) reported on the CPR. It was observed that women with
previous CS had a 9% lower CPR compared with women who had previous
NVD (pooled RR of 0.91, 95% CI: 0.87-0.96, with high heterogeneity
I2=67.2; P<0.001) (Fig.
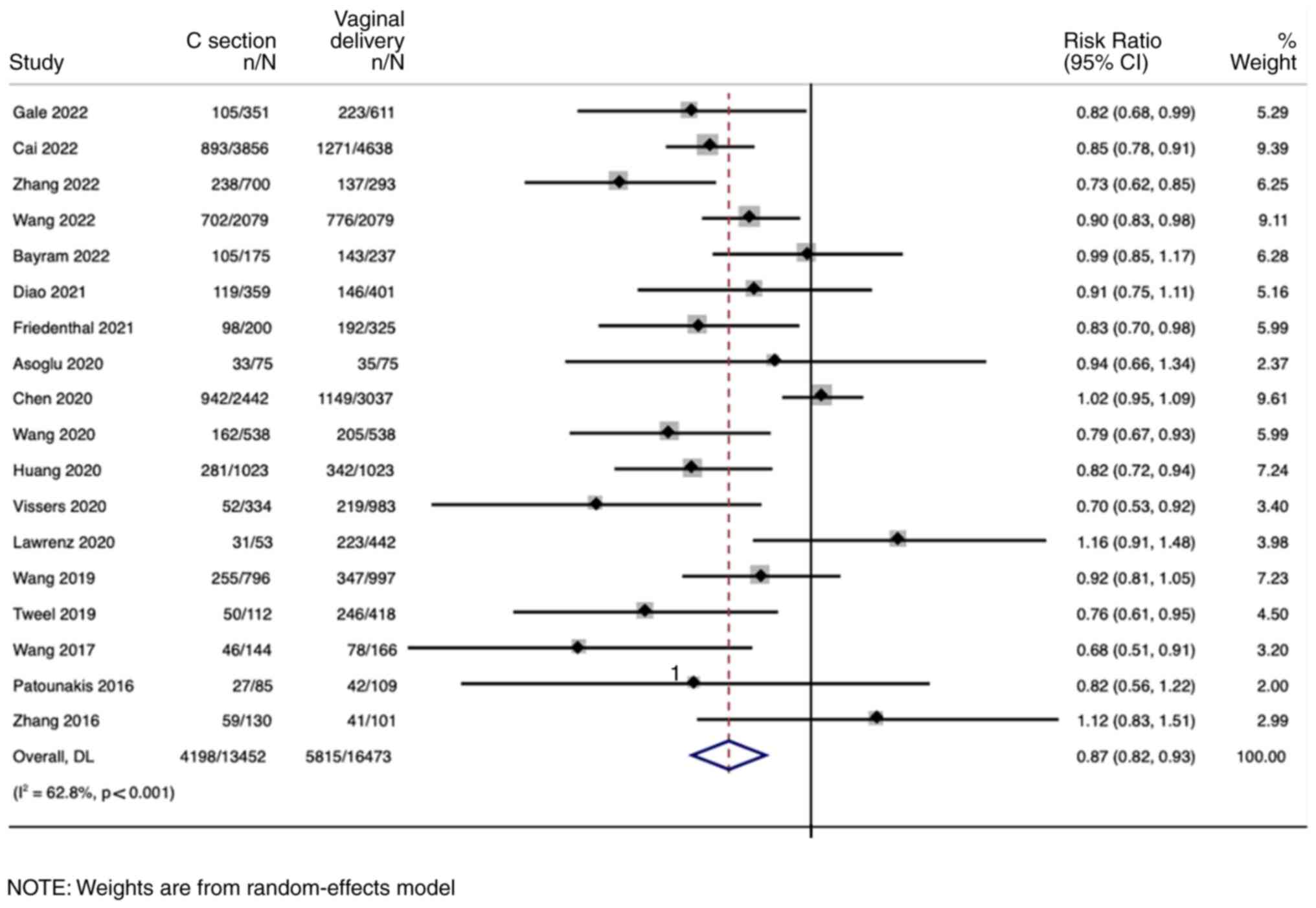
2). Furthermore, 18 studies (n=29,925; CS=13,452 and
NVD=16,473) reported on the LBR. It was observed that women with
previous CS had a 13% lower LBR compared with women who had
previous NVD (pooled RR of 0.87, 95% CI: 0.82-0.93, with high
heterogeneity I2=62.8; P<0.001) (Fig. 3). Next, seven studies (n=21,439;
CS=9,299 and NVD=12,140) reported on the IR. Women with previous CS
had an 11% lower IR compared with women with previous NVD (pooled
RR of 0.89, 95% CI: 0.81-0.99, with high heterogeneity
I2=76.1; P<0.001) (Fig.
S1). However, there was no significant difference in the EPR
(pooled RR of 1.15, 95% CI: 0.87-1.51, with no heterogeneity
I2=0; P=0.850) (Fig.
S2) and BPR (pooled RR of 0.95, 95% CI: 0.84-1.07, with high
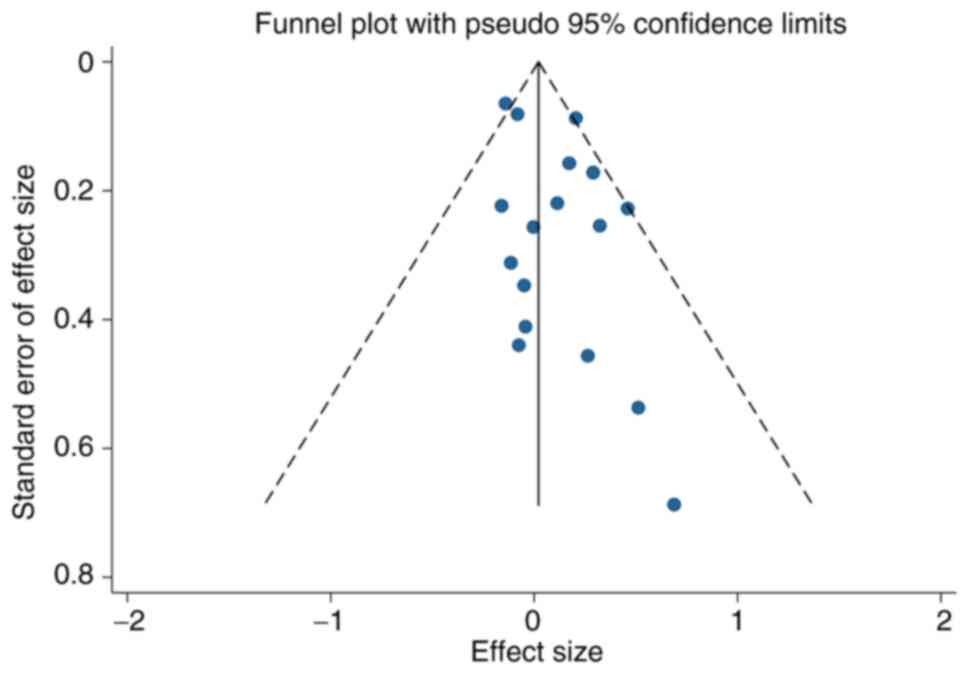
heterogeneity I2=94.2; P<0.001) (Fig. S3). Publication bias was assessed
only for four of the reproductive outcomes (BPR, CPR, EPR and LBR)
that were reported by >10 studies. No publication bias was
reported for outcomes such as CPR (Egger coefficient, 0.42; P=0.63)
(Fig. S4), LBR (Egger
coefficient, 1.03; P=0.20) (Fig.
S5), BPR (Egger coefficient, -1.0; P=0.66) (Fig. S6) and EPR (Egger coefficient,
0.41; P=0.30) (Fig. S7).
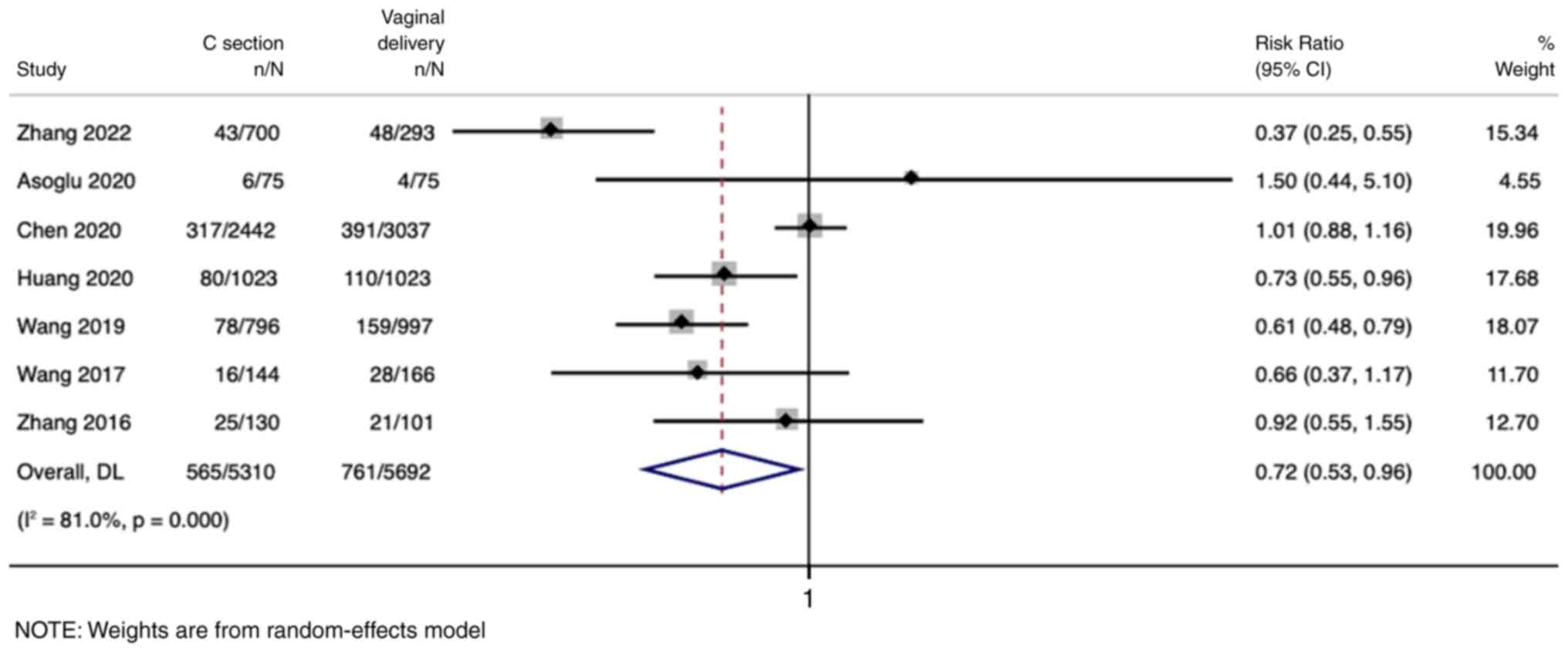
Secondary pregnancy outcomes across the study
groups. A total of seven studies (n=11,002; CS=5,310 and
NVD=5,692) reported on the MPR. Women with previous CS had a 28%
lower MPR compared with women who had previous NVD (pooled RR of
0.72, 95% CI: 0.53-0.96, with high heterogeneity
I2=81.0; P<0.001) (Fig.
4). Furthermore, eight studies (n=6,111; CS=2,629 and
NVD=3,482) reported on the EMT. Women with previous CS had -0.14
lower EMT compared with women who had previous NVD (pooled WMD of
-0.14, 95% CI: -0.26 to -0.01, with no heterogeneity
I2=0%; P=0.745) (Fig.
S8). DTRs were reported by three studies that showed that women
with previous CS had an 8-fold higher DTR compared with women with
NVD (pooled RR of 8.02, 95% CI: 4.54-14.16, with no heterogeneity
I2=0%; P=0.600) (Fig.
S9). However, no significant difference was detected in terms
of the PBR (pooled RR of 1.08, 95% CI: 0.82-1.42, with high
heterogeneity I2=79.3%; P<0.001) (Fig. S10), MR (pooled RR of 1.08, 95%
CI: 0.96-1.20, with moderate heterogeneity I2=32.2;
P=0.098) (Fig. S11), SBR (pooled
RR of 0.82, 95% CI: 0.31-2.21, with low heterogeneity
I2=11.1; P=0.342) (Fig.
S12), BW (pooled WMD of 17.41, 95% CI: -74 to 108.8, with
moderate heterogeneity I2=59.4; P=0.043) (Fig. S13) and BD (pooled RR of 1.72, 95%
CI: 0.49-5.97, with no heterogeneity I2=0%; P=0.440)
(Fig. S14). Publication bias was
assessed only for the MR, among the secondary pregnancy outcomes,
as it had >10 studies reporting it. The absence of publication
bias for the MR was noted (Egger coefficient, 0.84; P=0.08)
(Fig. 5).
Risk of bias in the included studies.
Table I summarizes the data on the
risk of bias in the included studies, as assessed by NOS. Based on
the 9-item scoring system, it was revealed that 11 studies had a
score of 8, six had a score of 7 and the remaining two studies had
a score of 9.
Discussion
The present meta-analysis included 19 studies that
reported 13 different reproductive and pregnancy outcomes in women
who underwent ART with and without a previous history of CS. The
results demonstrated that women with a previous history of CS had
9, 13, 11 and 28% lower probability of CPR, LBR, IR and MPR,
respectively. Additionally, previous CS was associated with an
8-fold higher DTR than previous NVD. These findings offer valuable
insights into the clinical management of this unique patient
population.
The rates of CS are on the rise worldwide (35), which in turn suggests that an
increasing number of women with a history of previous CS will be
receiving ART treatment. Previous studies showed that having a
previous CS may increase the likelihood of infertility and prolong
the time required to conceive (36,37).
Murphy et al (10),
hypothesized that this reduction in fertility might be linked to
increased rates of infections, adhesions, disruption of the
placental bed or other non-medical factors associated with CS, in
addition to socioeconomical and cultural differences.
The results of the present study revealed a 9% lower
CPR and 13% lower LBR in women with previous CS, which is
consistent with the work of Zhao et al (12). It may be speculated that this
effect may be explained by several possible mechanisms. The
endometrium at the CS scar site has fewer blood vessels in the
endometrial stroma, less leukocyte infiltration and delayed
endometrial maturation as compared with the endometrium after
vaginal delivery (38,39). Additionally, women with previous CS
tend to have increased rates of posterior placentas during
subsequent conception (40). CS
also impacts the integrity of the endometrial muscle layer junction
zone (41,42). In addition, a previous study
discovered that in frozen-thawed embryo transfer cycles, a previous
CS was linked to a lower LBR and increased MR (16).
However, it is important to note that the present
analysis did not reveal significant differences in EPR, MR and BPR
between women with previous CS and NVD. The results were comparable
to findings by Riemma et al (43). It was observed that previous CS was
associated with an 11% reduction in IR and an 8-fold higher DTR.
These findings are similar to findings from previous studies
(44,45) and may be explained by an anterior
diverticulum, which gathers fluid and old blood developing in the
lower uterus as a result of a CS incision (45). Blood that enters the uterus may
prevent successful implantation (44).
The present study had several clinical implications.
The findings of the present study may aid clinicians in counselling
women with previous CS about the potential impact on their
prospects of achieving a clinical pregnancy and live birth through
ART. In addition, the findings of the present study warrant a
thorough uterine anatomy evaluation before initiating ART,
especially in women with previous CS, for early identification of
uterine scars, adhesions and other possible complications. The
findings of the present study also emphasize the importance of
optimizing embryo transfer techniques in women with previous CS to
enhance successful implantation.
The present review is among the very few attempts
that have evaluated the impact of previous CS on a comprehensive
list of reproductive and pregnancy outcomes among women with ART.
The increased power of the present review due to the large sample
size is another major strength.
Despite these strengths, the present study has
certain limitations. One limitation is the moderate to high
heterogeneity between the studies. This heterogeneity may be
explained by methodological differences such as the study design,
differences in treatment protocols, embryo transfer techniques and
types of CS. In addition, the possibility of language bias could
not be excluded as only studies published in English were included.
Moreover, most included studies were historical cohorts. Therefore,
it was not possible to adjust for some potential confounders such
as smoking status, embryo quality, body mass index or ovarian
stimulation protocols.
In conclusion, the present systematic review and
meta-analysis provided comprehensive insights into the impact of
previous CS on reproductive and pregnancy outcomes in women
undergoing ART. The findings indicated that women with previous CS
may face decreased chances of CPR, LBR and successful embryo
implantation during ART. These results underscore the need for
tailored counselling and management strategies for this patient
population.
Supplementary Material
Forest plot showing the implantation
rate across study groups. CI, confidence interval.
Forest plot showing the ectopic
pregnancy rate across study groups. CI, confidence interval.
Forest plot showing the biochemical
pregnancy rate across study groups. CI, confidence interval.
Funnel plot describing publication
bias for studies reporting on the clinical pregnancy rate.
Funnel plot describing publication
bias for studies reporting on the live birth rate.
Funnel plot describing publication
bias for studies reporting on the biochemical pregnancy rate.
Funnel plot describing publication
bias for studies reporting on the ectopic pregnancy rate.
Forest plot showing the endometrial
thickness across study groups. SD, standard deviation; WMD,
weighted mean difference; CI, confidence interval.
Forest plot showing the difficult
transfer rate across study groups. CI, confidence interval.
Forest plot showing the preterm birth
rate across study groups. CI, confidence interval.
Forest plot showing the miscarriage
rate across study groups. CI, confidence interval.
Forest plot showing the still birth
rate across study groups. CI, confidence interval.
Forest plot showing the birth weight
across study groups. SD, standard deviation; WMD, weighted mean
difference; CI, confidence interval.
Forest plot showing the incidence of
birth defects across study groups. CI, confidence interval.
Search strategy.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The data generated in the present study may be
requested from the corresponding author.
Authors' contributions
DC conceived and designed the study. DC and LC
collected the data and performed the literature search. DC was
involved in the writing of the manuscript. All authors have read
and approved the final manuscript. DC and LC confirm the
authenticity of all the raw data.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests
References
|
1
|
Angolile CM, Max BL, Mushemba J and
Mashauri HL: Global increased cesarean section rates and public
health implications: A call to action. Health Sci Rep.
6(e1274)2023.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Spong CY, Berghella V, Wenstrom KD, Mercer
BM and Saade GR: Preventing the first cesarean delivery: Summary of
a joint eunice kennedy shriver national institute of child health
and human development, society for maternal-fetal medicine, and
American college of obstetricians and gynecologists workshop.
Obstet Gynecol. 120:1181–1193. 2012.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Li HT, Luo S, Trasande L, Hellerstein S,
Kang C, Li JX, Zhang Y, Liu JM and Blustein J: Geographic
variations and temporal trends in cesarean delivery rates in China,
2008-2014. JAMA. 317:69–76. 2017.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Rajaa S, Sujiv A and Kar SS: Risk factors
for cesarean section in women of urban Puducherry, India: A matched
case-control study. Int J Popul Stud. 7:66–72. 2022.
|
|
5
|
Clark EAS and Silver RM: Long-term
maternal morbidity associated with repeat cesarean delivery. Am J
Obstet Gynecol. 205 (Suppl):S2–S10. 2011.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Wang CB, Chiu WW, Lee CY, Sun YL, Lin YH
and Tseng CJ: Cesarean scar defect: Correlation between cesarean
section number, defect size, clinical symptoms and uterine
position. Ultrasound Obstet Gynecol. 34:85–89. 2009.PubMed/NCBI View
Article : Google Scholar
|
|
7
|
Diaz SD, Jones JE, Seryakov M and Mann WJ:
Uterine rupture and dehiscence: Ten-year review and case-control
study. South Med J. 95:431–435. 2002.PubMed/NCBI
|
|
8
|
Kjerulff KH, Zhu J, Weisman CS and Ananth
CV: First birth caesarean section and subsequent fertility: A
population-based study in the USA, 2000-2008. Hum Reprod.
28:3349–3357. 2013.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Gurol-Urganci I, Cromwell DA, Mahmood TA,
van der Meulen JH and Templeton A: A population-based cohort study
of the effect of caesarean section on subsequent fertility. Hum
Reprod. 29:1320–1326. 2014.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Murphy DJ, Stirrat GM and Heron J: ALSPAC
Study Team. The relationship between caesarean section and
subfertility in a population-based sample of 14 541 pregnancies.
Hum Reprod. 17:1914–1917. 2002.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Tollånes MC, Melve KK, Irgens LM and
Skjaerven R: Reduced fertility after cesarean delivery: A maternal
choice. Obstet Gynecol. 110:1256–1263. 2007.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Zhao J, Hao J, Xu B, Wang Y and Li Y:
Impact of previous caesarean section on reproductive outcomes after
assisted reproductive technology: Systematic review and
meta-analyses. Reprod Biomed Online. 43:197–204. 2021.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Page MJ, McKenzie JE, Bossuyt PM, Boutron
I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Akl EA, Brennan
SE, et al: The PRISMA 2020 statement: An updated guideline for
reporting systematic reviews. BMJ. 372(n71)2021.PubMed/NCBI View
Article : Google Scholar
|
|
14
|
Egger M, Davey Smith G, Schneider M and
Minder C: Bias in meta-analysis detected by a simple, graphical
test. BMJ. 315:629–634. 1997.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Lo CK, Mertz D and Loeb M:
Newcastle-ottawa scale: Comparing reviewers' to authors'
assessments. BMC Med Res Methodol. 14(45)2014.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Huang J, Lin J, Cai R, Lu X, Song N, Gao
H, Zhu J and Kuang Y: Effect of a prior cesarean delivery on
pregnancy outcomes of frozen-thawed embryo transfer: A
retrospective cohort study in a freeze-all setting. Acta Obstet
Gynecol Scand. 99:1303–1310. 2020.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Patounakis G, Ozcan MC, Chason RJ, Norian
JM, Payson M, DeCherney AH and Yauger BJ: Impact of a prior
cesarean delivery on embryo transfer: A prospective study. Fertil
Steril. 106:311–316. 2016.PubMed/NCBI View Article : Google Scholar
|
|
18
|
van den Tweel MM, Klijn NF, Diaz de Pool
JDN, van der Westerlaken LAJ and Louwe LA: Previous caesarean
section is associated with lower subsequent in vitro fertilization
live birth rates. Hum Fertil (Camb). 25:93–98. 2022.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Wang YQ, Yin TL, Xu WM, Qi QR, Wang XC and
Yang J: Reproductive outcomes in women with prior cesarean section
undergoing in vitro fertilization: A retrospective case-control
study. J Huazhong Univ Sci Technolog Med Sci. 37:922–927.
2017.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Zhang N, Chen H, Xu Z, Wang B, Sun H and
Hu Y: Pregnancy, delivery, and neonatal outcomes of in vitro
fertilization-embryo transfer in patient with previous cesarean
scar. Med Sci Monit. 22:3288–3295. 2016.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Lawrenz B, Melado L, Garrido N, Coughlan
C, Markova D and Fatemi H: Isthmocele and ovarian stimulation for
IVF: Considerations for a reproductive medicine specialist. Hum
Reprod. 35:89–99. 2020.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Wang L, Yao W, Tang X, Yao H, Wei S, Huang
J, Mol BWJ, Jin L, Yue J and Wang R: Fertility outcomes of IVF/ICSI
after caesarean section: A cohort study. Reprod Biomed Online.
40:719–728. 2020.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Asoglu MR, Celik C, Ozturk E, Cavkaytar S
and Bahceci M: Impact of isthmocele on assisted reproductive
treatment outcomes: An age-matched retrospective study. J Minim
Invasive Gynecol. 28:1113–1120. 2021.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Vissers J, Sluckin TC, van Driel-Delprat
CCR, Schats R, Groot CJM, Lambalk CB, Twisk JWR and Huirne JAF:
Reduced pregnancy and live birth rates after in vitro fertilization
in women with previous caesarean section: A retrospective cohort
study. Hum Reprod. 35:595–604. 2020.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Chen T, Li B, Shi H, Bu ZQ, Zhang FQ and
Su YC: Reproductive outcomes of single embryo transfer in women
with previous cesarean section. Reprod Sci. 28:1049–1059.
2021.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Gale J, Corran B, Bacal V, Haebe J, Nguyen
V and Shmorgun D: Reduced live birth rates after embryo transfer in
patients with prior cesarean delivery: A retrospective cohort
study. Eur J Obstet Gynecol Reprod Biol. 271:250–254.
2022.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Cai M, Pan X, Xia W, Liang X and Yang X:
Intra-cavitary fluid resulted from caesarean section but not
isthmocele compromised clinical pregnancy after IVF/ICSI treatment.
Arch Gynecol Obstet. 306:229–237. 2022.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Zhang Y, de Ziegler D, Hu X, Tai X, Han Y,
Ma J, Zhang Y and Luo H: Previous caesarean delivery and the
presence of caesarean scar defects could affect pregnancy outcomes
after in vitro fertilization frozen-thawed embryo transfer: A
retrospective cohort study. BMC Pregnancy Childbirth.
22(769)2022.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Wang L, Wang J, Lu N, Liu J and Diao F:
Pregnancy and perinatal outcomes of patients with prior cesarean
section after a single embryo transfer in IVF/ICSI: A retrospective
cohort study. Front Endocrinol (Lausanne).
13(851213)2022.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Bayram A, Elkhatib I, Abdala A, Nogueira
D, Melado L, Fatemi HM and Lawrenz B: ART outcome after euploid
frozen embryo transfer is not affected by previous cesarean section
delivery in the absence of intracavitary fluid. J Assist Reprod
Genet. 39:2529–2537. 2022.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Diao J, Gao G, Zhang Y, Wang X, Zhang Y,
Han Y, Du A and Luo H: Caesarean section defects may affect
pregnancy outcomes after in vitro fertilization-embryo transfer: A
retrospective study. BMC Pregnancy Childbirth.
21(487)2021.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Jacob L, Weber K, Sechet I, Macharey G,
Kostev K and Ziller V: Caesarean section and its impact on
fertility and time to a subsequent pregnancy in Germany: A database
analysis in gynecological practices. Arch Gynecol Obstet.
294:1005–1010. 2016.PubMed/NCBI View Article : Google Scholar
|
|
33
|
Friedenthal J, Alkon-Meadows T,
Hernandez-Nieto C, Gounko D, Lee JA, Copperman A and Buyuk E: The
association between prior cesarean delivery and subsequent in vitro
fertilization outcomes in women undergoing autologous,
frozen-thawed single euploid embryo transfer. Am J Obstet Gynecol.
225:287.e1–287.e8. 2021.PubMed/NCBI View Article : Google Scholar
|
|
34
|
Lin Y, Chen Q, Huang X, Wang Z, Chen C,
Chen H and Jin F: Obstetric and perinatal outcomes after assisted
reproductive technology in women with cesarean scar. Front Physiol.
13(808079)2022.PubMed/NCBI View Article : Google Scholar
|
|
35
|
Rietveld AL, van Exel NJA, Cohen de Lara
MC, de Groot CJM and Teunissen PW: Giving birth after caesarean:
Identifying shared preferences among pregnant women using Q
methodology. Women Birth. 33:273–279. 2020.PubMed/NCBI View Article : Google Scholar
|
|
36
|
Hemminki E: Impact of caesarean section on
future pregnancy-a review of cohort studies. Paediatr Perinat
Epidemiol. 10:366–379. 1996.PubMed/NCBI View Article : Google Scholar
|
|
37
|
O'Neill SM, Kearney PM, Kenny LC,
Henriksen TB, Lutomski JE, Greene RA and Khashan AS: Caesarean
delivery and subsequent pregnancy interval: A systematic review and
meta-analysis. BMC Pregnancy Childbirth. 13(165)2013.PubMed/NCBI View Article : Google Scholar
|
|
38
|
Rosa F, Perugin G, Schettini D, Romano N,
Romeo S, Podestà R, Guastavino A, Casaleggio A and Gandolfo N:
Imaging findings of cesarean delivery complications: Cesarean scar
disease and much more. Insights Imaging. 10(98)2019.PubMed/NCBI View Article : Google Scholar
|
|
39
|
Ananias P, Luenam K, Melo JP, Jose AM,
Yaqub S, Turkistani A, Shah A and Mohammed L: Cesarean section: A
potential and forgotten risk for abdominal wall endometriosis.
Cureus. 13(e17410)2021.PubMed/NCBI View Article : Google Scholar
|
|
40
|
Tinari S, Buca D, Cali G, Timor-Tritsch I,
Palacios-Jaraquemada J, Rizzo G, Lucidi A, Di Mascio D, Liberati M
and D'Antonio F: Risk factors, histopathology and diagnostic
accuracy in posterior placenta accreta spectrum disorders:
Systematic review and meta-analysis. Ultrasound Obstet Gynecol.
57:903–909. 2021.PubMed/NCBI View Article : Google Scholar
|
|
41
|
Ben-Nagi J, Walker A, Jurkovic D, Yazbek J
and Aplin JD: Effect of cesarean delivery on the endometrium. Int J
Gynaecol Obstet. 106:30–34. 2009.PubMed/NCBI View Article : Google Scholar
|
|
42
|
Naji O, Daemen A, Smith A, Abdallah Y,
Bradburn E, Giggens R, Chan DC, Stalder C, Ghaem-Maghami S,
Timmerman D and Bourne T: Does the presence of a cesarean section
scar influence the site of placental implantation and subsequent
migration in future pregnancies: A prospective case-control study.
Ultrasound Obstet Gynecol. 40:557–561. 2012.PubMed/NCBI View Article : Google Scholar
|
|
43
|
Riemma G, De Franciscis P, Torella M,
Narciso G, La Verde M, Morlando M, Cobellis L and Colacurci N:
Reproductive and pregnancy outcomes following embryo transfer in
women with previous cesarean section: A systematic review and
meta-analysis. Acta Obstet Gynecol Scand. 100:1949–1960.
2021.PubMed/NCBI View Article : Google Scholar
|
|
44
|
Tanimura S, Funamoto H, Hosono T, Shitano
Y, Nakashima M, Ametani Y and Nakano T: New diagnostic criteria and
operative strategy for cesarean scar syndrome: Endoscopic repair
for secondary infertility caused by cesarean scar defect. J Obstet
Gynaecol Res. 41:1363–1369. 2015.PubMed/NCBI View Article : Google Scholar
|
|
45
|
Tower AM and Frishman GN: Cesarean scar
defects: An underrecognized cause of abnormal uterine bleeding and
other gynecologic complications. J Minim Invasive Gynecol.
20:562–572. 2013.PubMed/NCBI View Article : Google Scholar
|