Introduction
A choledochal cyst (CC) is a congenital biliary
malformation characterized by cystic dilation of the biliary duct
(1); it is more common in Asian
countries than in Western countries and has an estimated incidence
ranging from 1/100,000 to 1/1,000 (1,2).
Approximately 80% of patients with CCs experience symptoms
including abdominal pain, jaundice, or abdominal mass before the
age of 10 years (3). Total CC
excision with Roux-en-Y hepaticojejunostomy (RYHJ) is currently
recommended for patients to avoid potential complications such as
hepatic fibrosis, pancreatitis, perforation and biliary malignancy
(4,5).
Minimally invasively surgery (MIS) procedures are
increasingly being applied in pediatric surgeries (6), including esophageal repair (7), duodenoduodenostomy (8,9) and
hepatobiliary surgeries (10,11),
and have exhibited benefits for children and even newborns
(7,8,10,12).
In the past two decades, laparoscopic-assisted surgery has been the
most popular procedure for CCs, because it is associated with less
postoperative pain, decreased complications and better cosmesis
than open surgery (3,5,12,13).
The majority of laparoscopic surgeries for CCs involve laparoscopic
procedures and extracorporeal Roux-en-Y construction (1,2).
However, there are relatively few reports on totally laparoscopic
surgery for CCs (TLCCs), due to the limited space in the pediatric
abdominal cavity and the operative difficulty. During the last 3
years, some patients with CCs at the Department of Pediatric
Surgery, Second Affiliated Hospital of Xi'an Jiaotong University
(Xi'an, China) have undergone TLCCs due to the pursuit of their
parents for better cosmesis and quality of life for these pediatric
patients. In the present study, a retrospective analysis of TLCCs
at the aforementioned hospital was conducted to evaluate its
efficacy and explore how TLCCs can be performed safely in a
pediatric population.
Patients and methods
Patients
TLCCs were performed in 28 out of 71 patients with
CCs at the Department of Pediatric Surgery, Second Affiliated
Hospital of Xi'an Jiaotong University (Xi'an, China) between June
2020 and June 2023. The enrolled patients consisted of 8 boys and
20 girls with a sex ratio of 1:2.5. The decision for whether or not
to undertake the TLCC approach was made preoperatively based on the
preferences of the parents and the surgeon. All surgeries were
completed by the same experienced pediatric surgeon. Written
informed consent was provided by the parents of the children before
surgery. The present retrospective study was approved by the Ethics
Committee of the Second Affiliated Hospital of Xi'an Jiaotong
University (approval no. 2022274; Xi'an, China).
Methods
Clinical data including demographic characteristics,
history of illness, laboratory test results and imaging findings,
operative data and postoperative outcomes were collected from the
electronic medical records and subjected to retrospective analysis.
All laboratory test results analyzed in the study were obtained
within 1 week before surgery. Operative data were acquired from the
documentation recording the surgery, anesthesia and intraoperative
care. Postoperative follow-up data were based on clinical records
and telephone enquiries. Data are presented as the mean value ±
standard deviation, which were calculated by Excel 2016 (Microsoft
Corporation).
Operative procedures
All of patients were intubated under general
anesthesia in the supine position and underwent TLCCs in the
reverse Trendelenburg position. In step 1, a 5-mm umbilical trocar
was inserted using the open method and fixed. The CO2
pneumoperitoneum pressure was maintained at 8-12 mmHg based on the
age and weight of the patient (1,14).
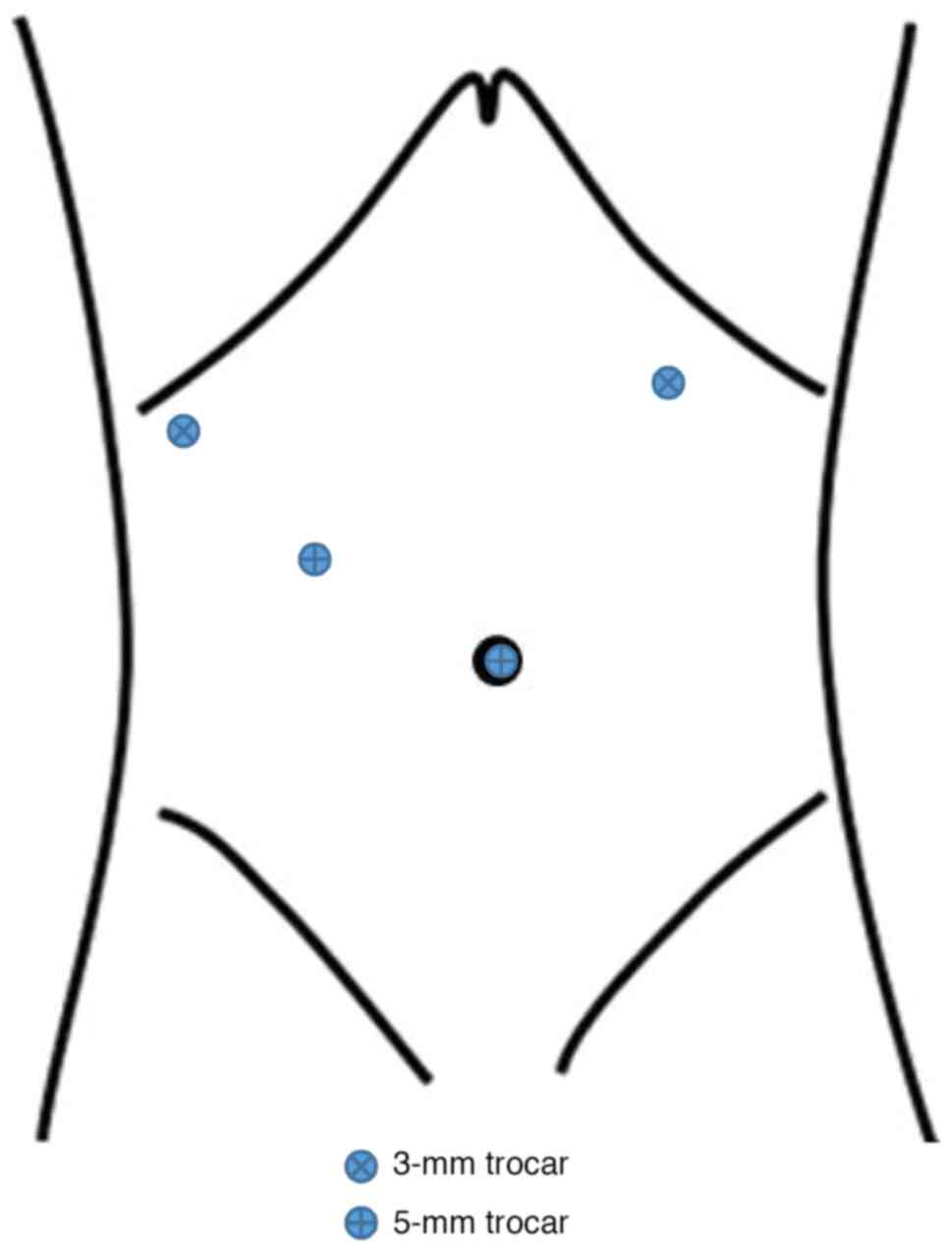
Another 5-mm trocar and two 3-mm trocars were inserted at the right
upper abdomen, and the right and left subcostal margins under the
laparoscopic view, respectively (Fig.
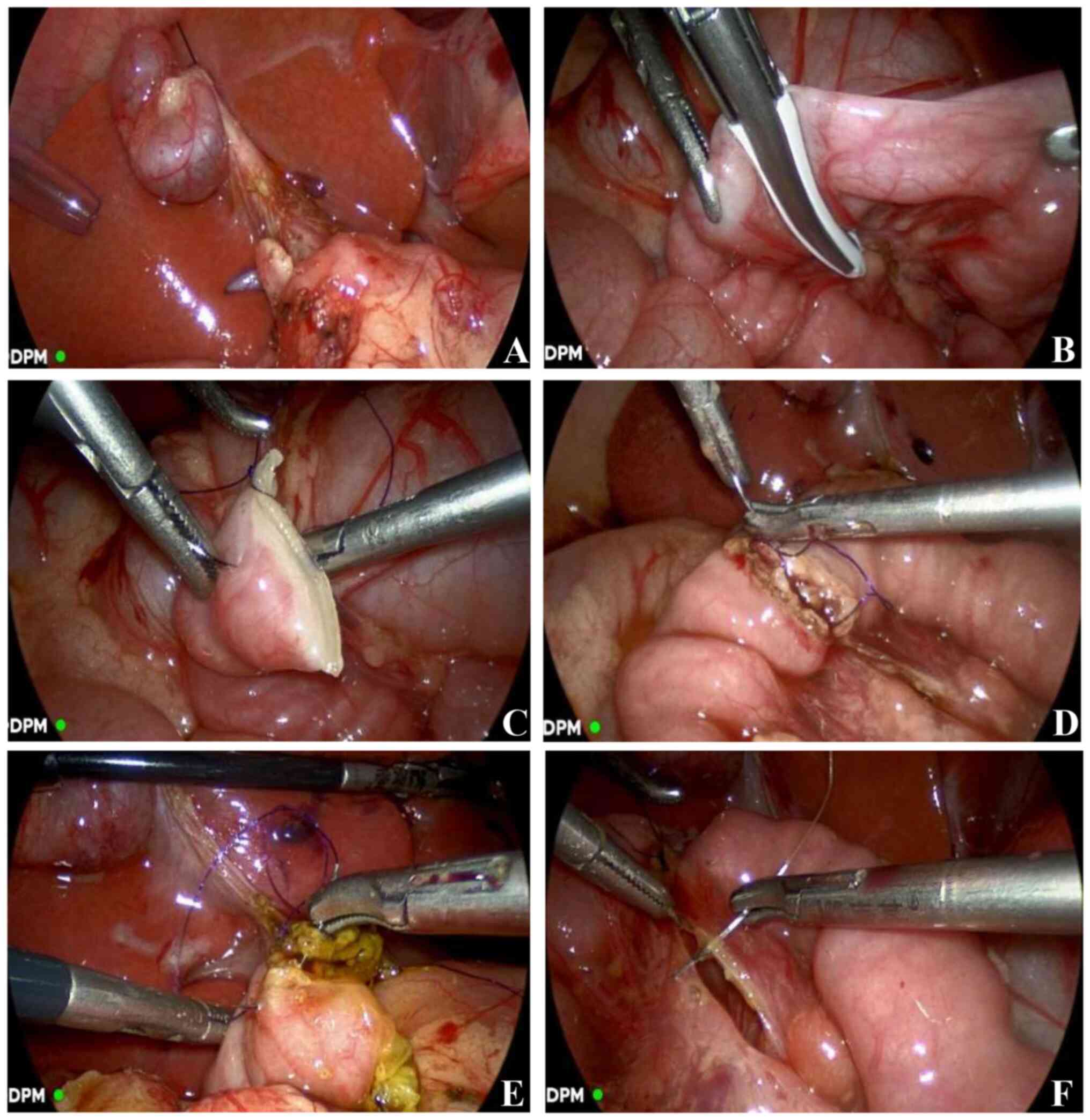
1). In step 2, a stay suture was placed at the neck of the
gallbladder (Fig. 2A) to suspend
the liver for splaying of the liver hilum and dissection of the
cyst. Meanwhile, the duodenum was constricted downward using
laparoscopic forceps by an assistant. The proximal end of the CC
was dissected at the level of the common hepatic duct and removed,
leaving a stump at ~5 mm from the bifurcation of the common hepatic
duct. Bile, protein plugs, or calculi within the cyst were
suctioned and washed out. The CC was dissected down to the distal
end using a monopolar electrocautery hook and ligated. The total
cyst was then removed. In step 3, the Treitz ligament was
identified under laparoscopy and the jejunum was cut transversely
using a LigaSure (Covidien LLC; Medtronic, Inc.) at 10-20 cm distal
to the ligament (Fig. 2B) with
management of the mesenteric vascular arch. The distal section of
the jejunum was closed using 5-0 polydioxanone (PDS) continuous
sutures (Fig. 2C). The Roux-en-Y
limb reached the liver hilum in a tensionless manner through a
window in the transverse mesocolon. A hand-sewn end-to-side
jejunojejunostomy (Fig. 2D),
consisting of an all-layer suture with a continuous locking method
in the posterior wall and continuous sutures on the seromuscular
layer in the anterior wall, was performed laparoscopically. In step
4, an end-to-side hepaticojejunostomy (Fig. 2E) was performed with 5-0 PDS
continuous sutures. Mesenteric defects in the jejunum and
transverse colon were closed with 5-0 absorbable sutures (Fig. 2F). In step 5, the gallbladder was
dissected and removed from its bed. Finally, a drainage tube was
placed through the right subcostal trocar incision.
Postoperative management
The urinary catheter was removed on the day after
surgery upon normal output of urine. Water intake was commenced at
24 h after surgery and gradually increased every 2-3 h. The
nasogastric tube was removed on the following day of onset of water
intake if the patient had no abdominal bloating or vomiting. A
liquid diet was started on the evidence of recovery of bowel
motility. The drainage tube was removed at 5-7 days after surgery
when the abdominal ultrasound was negative. Hospital discharge was
considered when patients ate normally without any discomfort.
Results
A total of 28 patients with CCs, including Todani
types I and IV, underwent TLCCs at our institution. The
characteristics of the patients are revealed in Table I. The ratio of male to female
patients was 1:2.5. The mean age at operation was 4.2 years (range,
1 month to 12.3 years) and the mean weight was 15.9 kg (range,
4.6-43 kg). Intermittent abdominal pain was the most frequent
symptom followed by jaundice, nausea and vomiting. A total of 6
patients were asymptomatic, including 4 patients diagnosed on
prenatal ultrasonography and 2 cases discovered accidentally. There
was also an uncommon case involving an 11-year-old girl from a
remote area who had undergone extrahepatic bile duct drainage for
10 years and visited the aforementioned hospital for further
treatment.
 | Table IClinical characteristics of patients
with choledochal cysts (n=28). |
Table I
Clinical characteristics of patients
with choledochal cysts (n=28).
| Variables | Value |
|---|
| Sex
(male/female) | 8/20 |
| Age at surgery,
yearsa | 4.2 (1 month-12.3
years) |
| Weight,
kga | 15.9 (4.6-43) |
| Symptoms, n | |
|
Abdominal
pain | 16 |
|
Nausea and
vomiting | 5 |
|
Jaundice | 5 |
|
Prenatal
discovery | 4 |
|
Unexpected
discovery | 2 |
| White blood cells, n
x109/l | 7.67±2.46 |
| Neutrophils, % | 34.42±13.06 |
| Alanine transferase,
IU/l | 56.74±37.93 |
| Aspartic
aminotransferase, IU/l | 43.95±36.45 |
| Direct bilirubin,
µmol/l | 14.2±24.81 |
| Indirect bilirubin,
µmol/l | 13.53±14.49 |
| Diameter of cyst,
cm | 1.74±0.76 |
| Length of cyst,
cm | 3.85±1.25 |
Prior to surgery, 3 children had hyperbilirubinemia
and 5 had elevated transaminase levels. Ultrasound was the first
choice to identify CCs in all patients, and magnetic resonance
cholangiopancreatography was performed preoperatively to obtain
further information. On imaging, the mean cyst diameter and length
were 1.74±0.76 cm and 3.85±1.25 cm, respectively.
As presented in Table
II, TLCCs were performed through four operative ports with a
mean intraoperative blood loss of 21.0±20.4 ml and a mean operative
time of 214±43.8 min. The urethral catheter and nasogastric tube
were removed at 1.02±0.70 days and 2.08±1.24 days after surgery,
respectively. The mean time to intake of an oral diet was 2.89±1.23
days after surgery. The drainage tube was left for a mean period of
6.25±2.32 days.
 | Table IIIntraoperative and postoperative data
of patients with choledochal cysts (n=28). |
Table II
Intraoperative and postoperative data
of patients with choledochal cysts (n=28).
| Variables | Value |
|---|
| Operative duration,
min | 214±43.8 |
| Blood loss during
operation, ml | 21.0±20.4 |
| Transfusions in
surgery, n | 0 |
| Placement of
nasogastric tube, days | 2.08±1.24 |
| Placement of
drainage, days | 6.25±2.32 |
| Retained urinary
catheter, days | 1.02±0.70 |
| Time to water intake,
days | 1.81±0.65 |
| Time to liquid diet,
days | 2.89±1.23 |
| Complications, n | |
|
Wound
infection | 1 |
|
Bile
leakage | 1 |
|
Pancreatitis | 0 |
|
Bowel
obstruction | 0 |
|
Other | 0 |
| Reoperation, n | 0 |
| Hospital stay after
surgery, days | 6.82±2.12 |
Bile leakage occurred in a 4.5-year-old girl on
postoperative day 4 and the patient was treated conservatively by
drainage and parenteral nutrition for 9 days. A 5-year-old girl
experienced an infection in the incision where the drainage tube
was placed, which was cured by wound care and antibiotics. The
other 26 patients had an uneventful recovery after surgery. The
mean hospital stay for postoperative recovery after TLCCs was
6.82±2.12 days. No further complications occurred during a median
follow-up period of 18 months (range, 4-42 months) based on clinic
visits and telephone enquiries.
Discussion
CCs are more common in Asian countries than in
Western countries, and arise through congenital anomalous
development of the biliary system (2). Currently, the most common surgical
procedure for CCs is performed with laparoscopic assistance, and
the Roux-en-Y anastomosis is performed extracorporeally (3,5).
With recent advances in laparoscopic techniques and instruments,
TLCCs has been reported as an MIS procedure associated with rapid
recovery of gastrointestinal function and reduced hospital stay
(1). However, the intracorporeal
jejunojejunostomy was completed using an Endo-GIA instrument
(1,11,15-18)
with an additional 12-mm port (1,11,17,18)
and increased hospitalization costs (1). Given the rich experience with
laparoscopic surgery in pediatric patients at the institution of
the authors, the technique of laparoscopic duodenoduodenostomy was
applied for the jejunojejunal anastomosis in TLCCs. In the present
study, the hand-sewn jejunojejunal anastomosis under laparoscopy
was performed intracorporeally based on sophisticated laparoscopic
techniques. As well as the advantages of laparoscopic surgery
aforementioned, TLCCs are associated with less trauma and smaller
incisions without significantly increased costs, and also meets the
expectations of the children and their parents for MIS.
During the intracorporeal jejunojejunostomy, the
intestine can remain relaxed in the natural position without
extracorporeal exposure during the anastomosis. This can reduce
intestinal stretching and avoid the possibility of mesenteric
vessels being incarcerated by the incision. Consequently, the risk
of intestinal injury and postoperative adhesions is theoretically
decreased and the recovery of intestine motility can benefit from
this approach (1). Compared with
previous reports on TLCCs, a running hand-sewn approach was used at
the Second Affiliated Hospital of Xi'an Jiaotong University instead
of a mechanical anastomosis (endo-GIA) and was applied
intracorporeally during the jejunojejunostomy procedure. The
present study demonstrated improved results than previous studies
regarding operative time, time until oral intake and postoperative
hospital stay (Table III). As
revealed in Table III,
complications including intestinal obstruction and necrosis were
reported in 0-7% of cases and were caused by herniation of the
distal biliary jejunum into the defect in the transverse mesocolon
(1,11), while bile leakage and wound
infection occurred in 2 of the patients without bowel
obstruction.
 | Table IIIPrevious studies of totally
laparoscopic surgery for choledochal cysts. |
Table III
Previous studies of totally
laparoscopic surgery for choledochal cysts.
| First author,
year | Cases | Operative age,
years | Ports, mm | Intestinal
anastomosis | Operative time,
min | Time to oral
intake, days | Postoperative
hospital days | Complications | (Refs.) |
|---|
| Jang et al,
2006 | 13 | 37.3±13.1 | 5-11 | Mechanical | 228±51 | 3 | 5.8±1.2 | Bile leakage,
subphrenic fluid collection | (18) |
| Ahn et al,
2009 | 6 | 0.3-7 | 3-11 | Mechanical | 275±58 | 3 | 6a | No | (17) |
| Gander et
al, 2010 | 13 | 5b (1-16) | 5-12 |
Mechanical/hand-sewn | 240b (130-325) | 1b (1-4) | 5b (4-8) | Bowel
obstruction | (11) |
| Urushihara et
al, 2011 | 8 | 4.1 (1.6-7) | 5-12 | Mechanical | 390a (310-460) | NA | 8.4a (7-14) | NA | (15) |
| Liu et al,
2020 | 30 | 4.31±0.46 | 5-12 | Mechanical | NA | 3.57±0.19 | 5.50±0.28 | Bowel obstruction
andnecrosis, adhesive intestinal obstruction | (1) |
| Murakami et
al, 2021 | 1 | 0.2 | 3-10 | Mechanical | 502 | NA | NA | No | (16) |
| Present study | 28 | 4.2a (0.1-12.3) | 3-5 | Hand-sewn | 214±43.8 | 2.89±1.23 | 6.82±2.12 | Bile leakage, wound
infection | - |
In gastrointestinal surgery, mechanical anastomosis
with a stapler has been widely used in adult populations (1,11,15,19,20)
but rarely used in pediatric populations (15,17,18).
Compared with the hand-sewn method, use of a stapler significantly
reduced the operative time in digestive anastomoses (20), but some shortcomings other than
high cost (20) should be noted,
especially in children. It was reported that adverse events
associated with stapler use occurred in up to 17.3% of cases,
including leakage or dehiscence, bleeding and infection (19), while serosal laceration of the
stomach was found in 46% of cases in animal experiments on pigs
(21). An additional 12-mm trocar
is always required when introducing a stapler device, and it is
difficult to operate in the limited space of the pediatric
abdominal cavity, thus increasing the trauma to the abdomen and the
expense of hospitalization (1,15,16).
On the contrary, laparoscopic manual continuous
sutures have been safely used for digestive anastomoses (1,11,22,23),
including intestinal anastomoses (11,22),
which have been applied in RYHJ (1,11),
and require less time than interrupted sutures (8). Moreover, the hand-sewn method has
been used to close the hole after side-to-side anastomosis with the
use of a stapler and repair the mesenteric defects to prevent
intestinal obstruction due to internal herniation (1,11).
Nevertheless, it should be considered that manual laparoscopic
anastomosis is technically challenging and may increase the
operative duration (11,17).
The following methods were selected to minimize the
complications of TLCCs in the pediatric patients. First, the length
of the Roux-en-Y limb was measured from the hepatic hilum to the
umbilicus to avoid a redundant loop. Second, the transverse cut of
the jejunum was performed using a LigaSure device, which can
achieve temporary closure of the jejunal stoma and reduce
contamination of the abdominal cavity (Fig. 2B and C). Third, single-layered continuous
sutures were used to close the distal stoma and complete the
end-to-side jejunojejunostomy and hepaticojejunostomy. The
technique has been applied in bowel anastomosis with lower
incidence of anastomotic leak, reduced time duration and lower
costs compared with double-layered sutures (24). Fourth, it was important to provide
proper tension while suturing and tightening the stitches through
an assistant (Fig. 2D), because
the jejunum is mobile.
To the best of the authors' knowledge, the present
study included the largest number of pediatric patients who
underwent TLCCs with manual sutures reported to date. However, the
limitations of the retrospective review and the lack of a
comparison with conventional laparoscopic surgery for CCs must be
acknowledged. Controlled prospective studies will be necessary to
determine the safety and superiority of this approach for pediatric
CCs.
In summary, TLCCs were safely performed in a cohort
of patients with congenital CCs. The intracorporeal jejunojejunal
anastomosis was anatomically natural and improved the recovery of
bowel function compared with the conventional laparoscopic surgery
approach for CCs, moreover, it was associated with less trauma and
improved esthetic outcomes. The laparoscopic hand-sewn method was
reliable and cost-effective. Therefore, TLCCs with manual sutures
may be considered as an option for MIS in pediatric patients with
CCs.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The data generated in the present study may be
requested from the corresponding author.
Authors' contributions
QL and JF participated in the study design and data
collection, carried out the initial analyses and drafted the
article. QY and PL participated in the study conception and design,
analysis and interpretation of the data, and critical revisions of
the article. QL and JF confirm the authenticity of all the raw
data. All authors read and approved the final version of the
manuscript and agree to be accountable for all aspects of the
work.
Ethics approval and consent to
participate
Ethics approval (approval no. 2022274) was obtained
from the Ethics Committee of the Second Affiliated Hospital of
Xi'an Jiaotong University (Xi'an, China). Written informed consent
was provided from the parents of all the children who participated
in the present study.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Liu F, Xu X, Lan M, Tao B, Li L, Wu Q,
Chai C and Zeng J: Total versus conventional laparoscopic cyst
excision and Roux-en-Y hepaticojejunostomy in children with
choledochal cysts: A case-control study. BMC Surg.
20(243)2020.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Wen Z, Liang H, Liang J, Liang Q and Xia
H: Evaluation of the learning curve of laparoscopic choledochal
cyst excision and Roux-en-Y hepaticojejunostomy in children: CUSUM
analysis of a single surgeon's experience. Surg Endosc. 31:778–787.
2017.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Xie X, Li K, Wang J, Wang C and Xiang B:
Comparison of pediatric choledochal cyst excisions with open
procedures, laparoscopic procedures and robot-assisted procedures:
A retrospective study. Surg Endosc. 34:3223–3231. 2020.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Guan X, Li J, Wang Z, Zeng J, Zhong W and
Yu J: Timing of operation in children with a prenatal diagnosis of
choledochal cyst: A single-center retrospective study. J
Hepatobiliary Pancreat Sci. 29:1308–1315. 2022.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Section of Laparoscopic&Endoscopic
Surgery; Branch of Pediatric Surgery; Chinese Medical Association.
Guideline for laparoscopic hepatojejunostomy for choledochal cyst
in children (2017). Chin J Pediatr Surg. 38:485–494. 2017.
|
|
6
|
Gil LA, Asti L, Apfeld JC, Sebastião YV,
Deans KJ and Minneci PC: Perioperative outcomes in
minimally-invasive versus open surgery in infants undergoing repair
of congenital anomalies. J Pediatr Surg. 57:755–762.
2022.PubMed/NCBI View Article : Google Scholar
|
|
7
|
van Lennep M, Singendonk MMJ, Dall'Oglio
L, Gottrand F, Krishnan U, Terheggen-Lagro SWJ, Omari TI, Benninga
MA and van Wijk MP: Oesophageal atresia. Nat Rev Dis Primer.
5(26)2019.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Oh C, Lee S, Lee SK and Seo JM:
Laparoscopic duodenoduodenostomy with parallel anastomosis for
duodenal atresia. Surg Endosc. 31:2406–2410. 2017.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Chung PHY, Wong CWY, Ip DKM, Tam PKH and
Wong KKY: Is laparoscopic surgery better than open surgery for the
repair of congenital duodenal obstruction? A review of the current
evidences. J Pediatr Surg. 52:498–503. 2017.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Kwon H, Lee JY, Cho YJ, Kim DY, Kim SC and
Namgoong JM: How to safely perform laparoscopic liver resection for
children: A case series of 19 patients. J Pediatr Surg.
54:2579–2584. 2019.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Gander JW, Cowles RA, Gross ER, Reichstein
AR, Chin A, Zitsman JL, Middlesworth W and Rothenberg SS:
Laparoscopic excision of choledochal cysts with total
intracorporeal reconstruction. J Laparoendosc Adv Surg Tech A.
20:877–881. 2010.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Soares KC, Goldstein SD, Ghaseb MA, Kamel
I, Hackam DJ and Pawlik TM: Pediatric choledochal cysts: Diagnosis
and current management. Pediatr Surg Int. 33:637–650.
2017.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Yin T, Chen S, Li Q, Huang T, Li L and
Diao M: Comparison of outcomes and safety of laparoscopic and
robotic-assisted cyst excision and hepaticojejunostomy for
choledochal cysts: A systematic review and meta-analysis. Ann Med
Surg (Lond). 75(103412)2022.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Liu Q, Fu J, Yu Q, Gong W, Li P and Guo X:
Laparoscopic surgery of intra-abdominal lymphatic malformation in
children. Exp Ther Med. 24(581)2022.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Urushihara N, Fukuzawa H, Fukumoto K,
Sugiyama A, Nagae H, Watanabe K, Mitsunaga M and Miyake H: Totally
laparoscopic management of choledochal cyst: Roux-en-Y
Jejunojejunostomy and wide hepaticojejunostomy with hilar
ductoplasty. J Laparoendosc Adv Surg Tech A. 21:361–366.
2011.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Murakami M, Kaji T, Nagano A, Matsui M,
Onishi S, Yamada K and Ieiri S: Complete laparoscopic choledochal
cyst excision and hepaticojejunostomy with laparoscopic Roux-Y
reconstruction using a 5-mm stapler: A case of a 2-month-old
infant. Asian J Endosc Surg. 14:824–827. 2021.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Ahn SM, Jun JY, Lee WJ, Oh JT, Han SJ,
Choi SH and Hwang EH: Laparoscopic total intracorporeal correction
of choledochal cyst in pediatric population. J Laparoendosc Adv
Surg Tech A. 19:683–686. 2009.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Jang JY, Kim SW, Han HS, Yoon YS, Han SS
and Park YH: Totally laparoscopic management of choledochal cysts
using a four-hole method. Surg Endosc. 20:1762–1765.
2006.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Kuthe A, Haemmerle A, Ludwig K, Falck S,
Hiller W, Mainik F, Freys S, Dubovoy L, Jaehne J and Oldhafer K:
Multicenter prospective evaluation of a new articulating 5-mm
endoscopic linear stapler. Surg Endosc. 30:1883–1893.
2016.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Korolija D: The current evidence on
stapled versus hand-sewn anastomoses in the digestive tract. Minim
Invasive Ther Allied Technol. 17:151–154. 2008.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Hasegawa S, Nakayama S, Hida K, Kawada K
and Sakai Y: Effect of tri-staple technology and slow firing on
secure stapling using an endoscopic linear stapler. Dig Surg.
32:353–360. 2015.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Mentessidou A and Saxena AK: Laparoscopic
repair of duodenal atresia: Systematic review and meta-analysis.
World J Surg. 41:2178–2184. 2017.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Qin R, Kendrick ML, Wolfgang CL, Edil BH,
Palanivelu C, Parks RW, Yang Y, He J, Zhang T, Mou Y, et al:
International expert consensus on laparoscopic
pancreaticoduodenectomy. Hepatobiliary Surg Nutr. 9:464–483.
2020.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Aniruthan D, Pranavi AR, Sreenath GS and
Kate V: Efficacy of single layered intestinal anastomosis over
double layered intestinal anastomosis-an open labelled, randomized
controlled trial. Int J Surg. 78:173–178. 2020.PubMed/NCBI View Article : Google Scholar
|