Introduction
Delicate nickel-titanium instruments are essential
in root canal therapy. However, when the operation of the surgeon
is not standard or the morphology of the root canal is too complex,
the force applied to the instrument exceeds the antifatigue
strength, and the instrument is likely to fracture in the root
canal (1). It has been previously
reported that the worldwide probability of instrument fracturing
during root canal treatment ranges from 0.7 to 7.4%, which is
difficult to avoid even by experienced dentists and endodontists
(2-4).
Fatigue separation accounts for 50-90% of instrument separations
worldwide (5). During the process
of root canal preparation, tensile and compressive stresses are
repeatedly applied to the instrument, resulting in microcracks on
its surface. When the instrument works in the curved or narrow
parts of the root canal, the cracks are easily broken, resulting in
separation. The retention of fractured instruments (FIs) in the
root canal makes disinfection of the root canal, a critical factor
in the success of root canal therapy outcomes, difficult to achieve
effectively, thus reducing the success rate of treatment (6).
From the perspective of the patient, residual FIs
may trigger anxiety as they may be viewed as treatment failure or
even medical malpractice. Any problems the patient encounters in
the future may be attributed to this. Therefore, with the
popularization and availability of dental microscopy, ultrasonic
equipment and professional tools for removing FIs, the removal of
FIs is becoming the first-choice strategy for clinicians (7). However, since the majority of
separations occur during the treatment of root canals with poor
surgical fields and small, curved and severely calcified root
canals, not all files can be effectively removed. During the
process of establishing a straight path in the root canal, varying
degrees of tooth tissue are removed, increasing the risk of lateral
perforation and root fracture (8).
Therefore, bypass techniques, which consist of retaining and
bypassing the FI to seal the apical stop, should be considered.
However, the success rate of bypass techniques remains a topic of
debate in the field of root canal therapy. This report attempts to
explore the feasibility of bypass technique for FIs by comparing
the postoperative outcomes of removal and bypass techniques for the
same tooth.
Case report
The present case involved a 41-year-old female
patient who was conscious with no underlying disease. The patient
complained of pain in the left upper posterior tooth for 6 months,
which intensified in the last 3 days before presentation. The
patient reported that the affected tooth had been treated in
another hospital due to pain 2 years prior, but the discomfort
persisted after treatment. A sudden onset of pain 6 months prior to
admittance to hospital, which was not treated, had occurred
intermittently since then. However, 3 days prior to admittance to
hospital, the pain worsened and was only slightly relieved by
anti-inflammatory drugs. In addition, 2 days prior to admittance to
hospital, the patient was treated at another hospital, which
suggested implant restoration after extraction of the affected
tooth. In September 2021, after studying the medical history, the
implantologist at Xi'an International Medical Center Hospital in
Xi'an, China referred the patient to the endodontist for further
evaluation of the retention value of the affected tooth.
Intraoral examination revealed a large area of
defects on the distal proximal surface of tooth no. 26, with
partial loss of white filling material and secondary caries at the
edge of the material. The affected tooth experienced severe pain on
percussion, but no discomfort from cold stimulation or probing. The
extent of loosening was I˚. The buccal vestibular sulcus of the
affected tooth was swollen and painful to press. A fistula was
observed in the mucosa of the buccal apical region. Periodontal
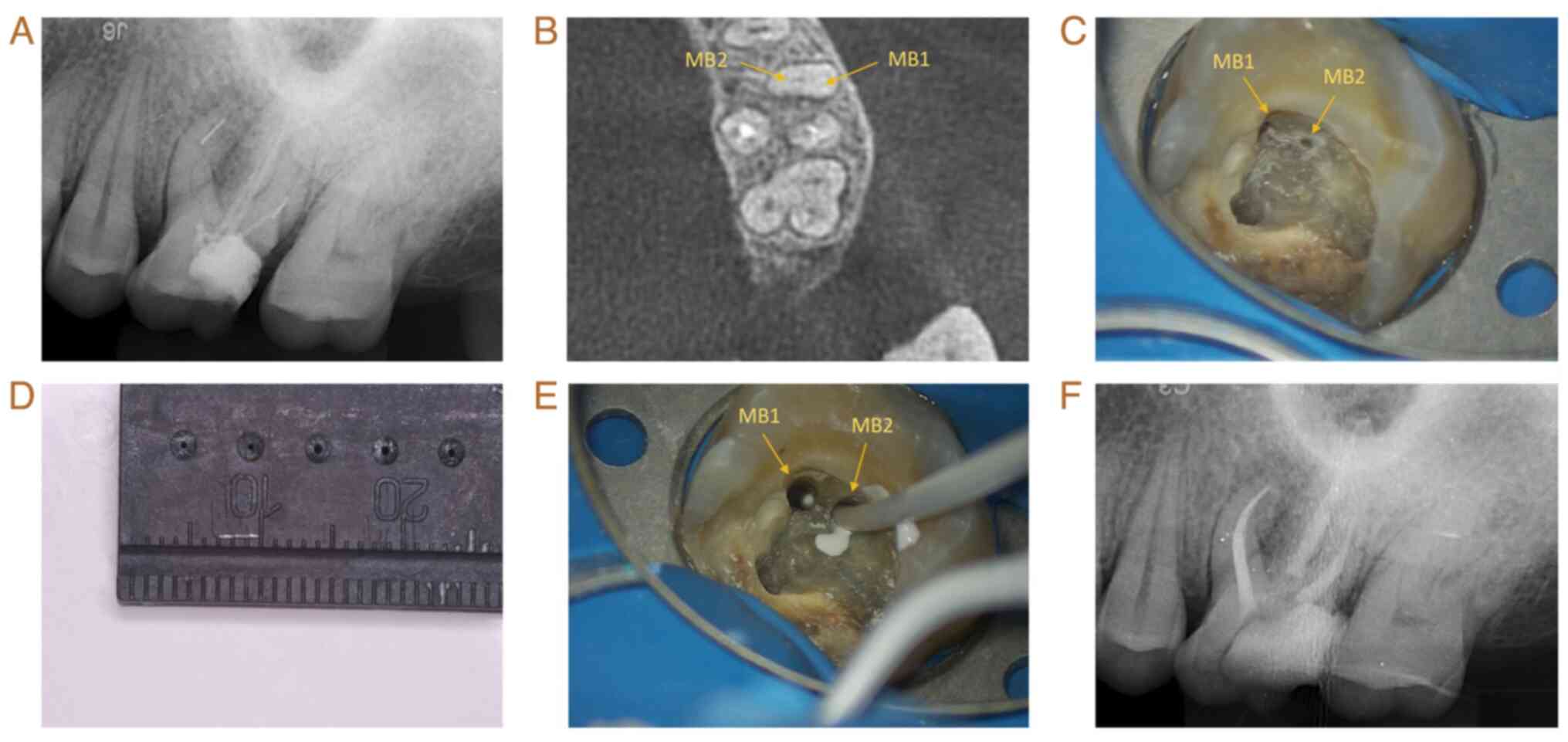
probing revealed no significant attachment loss. Diagnostic X-ray
revealed that tooth no. 26 had been endodontically treated
(Fig. 1A). There were suspected
FIs in the apical segment of the mesiobuccal (MB) root and the
middle segment of the distal buccal (DB) root; the palatal (P)
canal filling was underfilled, and there was also a large hypodense
area surrounding the periapex of the three aforementioned roots
(Fig. 1A). Cone-beam CT (CBCT)
revealed that the MB root was suspected of having two canals, where
the FI was present in the first MB canal (MB1) but there was no
obvious filling in the MB2 (Fig.
1B). On the basis of these observations, a diagnosis of chronic
apical periodontitis was made for tooth no. 26. Since the patient
expressed a desire to retain the affected tooth, root canal
retreatment of tooth no. 26 was planned after communication with
the patient. Specifically, the intended protocol involved removing
the FI at the middle of the DB canal, establishing a bypass through
the MB2 canal for treating the MB root and then retreating the P
root.
The original filling was removed via a diamond bur,
after a rubber dam was used to isolate the affected tooth. Under a
dental operating microscope (OMS 2380; Zumax Medical Co., Ltd.),
two root canal orifices, MB1 and MB2, could be observed in the MB
root (Fig. 1C). The FIs in the DB
canal were removed (Fig. 1D) via
the ET20 and ET25 working tips with an ultrasonic therapeutic
instrument (P5 Newtron XS; Satelec; Acteon). A mechanical
endodontic retreatment file (PROTAPER A1412; Dentsply Sirona, Inc.)
was used to remove the filling material in the P canal. The initial
working length of the root canals was measured via diagnostic X-ray
and an apex locator (PROPEX II; Dentsply Sirona, Inc.).
Subsequently, no. 8 and no. 10 K files (K-FILES; Mani, Inc.) were
used to dredge the canals. The root canals were prepared using an
X-SMART endodontic micromotor (X-SMART PLUS; Dentsply Sirona,
Inc.). During preparation, the root canals were irrigated
repeatedly with 20 ml of 1% sodium hypochlorite (NaClO) solution
and 5 ml of 17% ethylenediaminetetraacetic acid (EDTA) solution.
The DB, MB1 and MB2 canals were prepared with a #25/0.04 taper,
whereas the P canal was prepared with a #35/0.04 taper. After
repeated irrigation using an ultrasonic therapeutic instrument,
sterile paper tips were used to dry the root canals, and calcium
hydroxide paste (ApexCal; Ivoclar Vivadent) was inserted into the
root canals. Upon inserting the paste into the MB2 root canal
orifice, it was observed that the paste flowed upwards from the MB1
root foramen (Fig. 1E), supporting
the suspicions that the MB1 canal fused with MB2 to form a single
canal at the apical segment. A sterile cotton pellet was placed in
the pulp chamber before the access cavity was sealed via temporary
sealing paste (Cavit-G; 3M ESPE).
At 2 weeks after the procedure, the affected tooth
had no percussion pain or abnormal mobility. The apical segments of
the MB2, DB and P canals were filled with large taper gutta-perchas
(RECIPROC; VDW GmbH) and injectable root canal sealers (iRoot SP;
Innovative BioCeramix, Inc.) via the vertical compression
technique. The middle and coronal segments of the four root canals
were filled with warm gutta-percha via a gutta-percha heating
system (WL-B1; B&L Biotech). After filling, X-ray imaging
revealed that all the root apexes were fully filled (Fig. 1F).
At 1 week later, the affected tooth demonstrated no
percussion pain, no abnormal mobility and no obvious abnormalities
in the buccal or lingual mucosa. The tooth was restored with an
onlay.
At 9 months after surgery, CBCT revealed that the
hypodense area surrounding the DB, MB and P root apex had
significantly diminished (Fig. 2).
At 27 months after surgery, CBCT revealed that the hypodense areas
surrounding the DB, MB and P root apex almost completely
disappeared (Fig. 2).
 | Figure 2Follow-up observation of tooth no. 26
via X-ray. (A) Sagittal X-ray of the MB root. the first was taken
before the operation, the second was taken 9 months after the
operation and the third was taken 27 months after the operation.
(B) Coronal X-ray of the MB root. The first was taken before the
operation, the second was taken 9 months after the operation and
the third was taken 27 months after the operation. (C) Sagittal
X-ray of the DB root. The first was taken before the operation, the
second was taken 9 months after the operation and the third was
taken 27 months after the operation. (D) Coronal X-ray of the DB
root. The first was taken before the operation, the second was
taken 9 months after the operation and the third was taken 27
months after the operation. (E) Sagittal X-ray of the P root. The
first was taken before the operation, the second was taken 9 months
after the operation and the third was taken 27 months after the
operation. (F) Coronal X-ray of the P root. The first was taken
before the operation, the second was taken 9 months after the
operation and the third was taken 27 months after the operation.
(G) Cross-sectional X-ray of the three types of roots. The first
was taken before the operation, the second was taken 9 months after
the operation and the third was taken 27 months after the
operation. MB, mesiobuccal; FI, fractured instrument; DB, distal
buccal; P, palatal. |
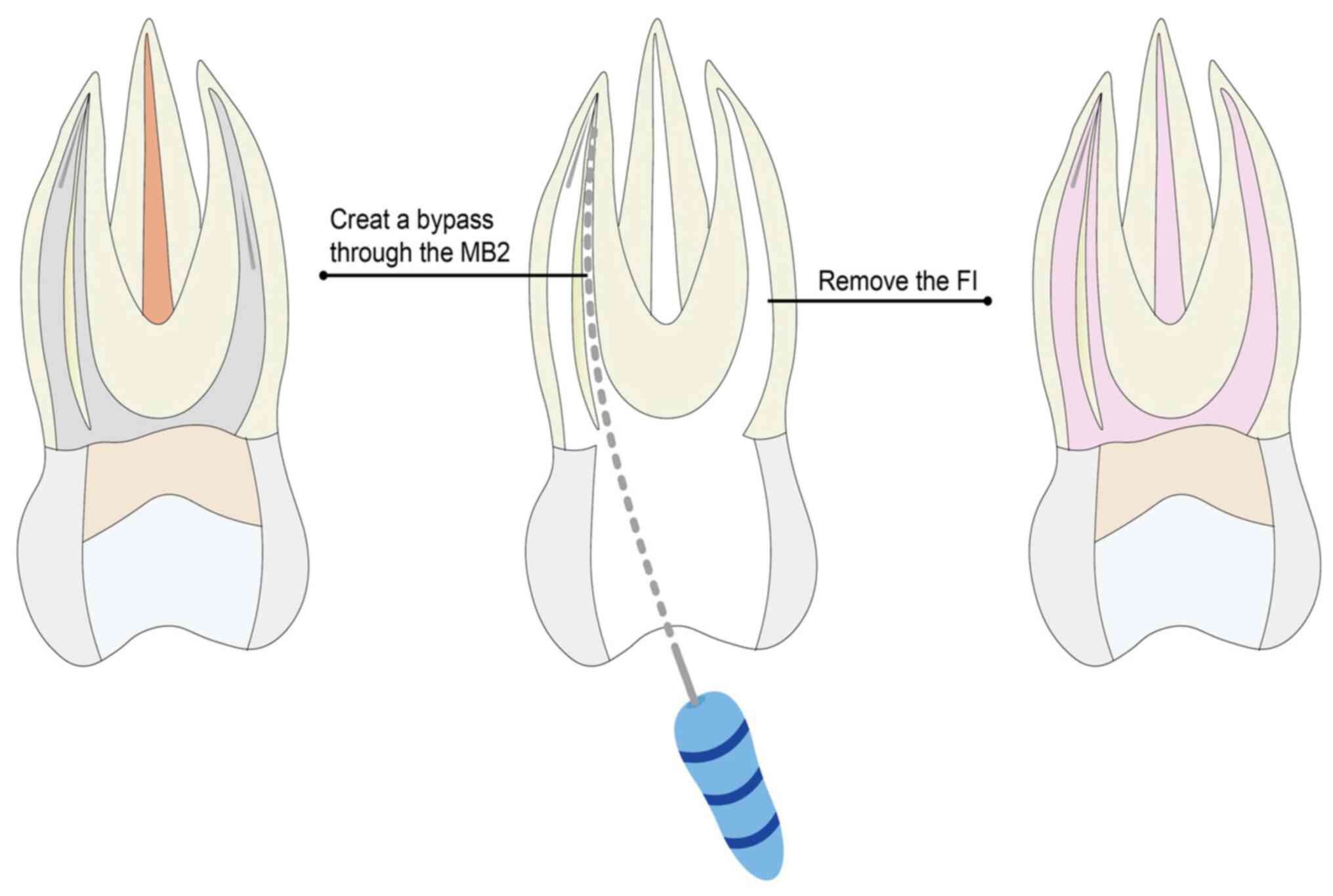
In the present case, FIs were successfully removed
from the middle third of the DB canal under an oral microscope with
the use of ultrasonic equipment. If attempts were made to remove
the FI in the MB root, regardless of success, then a large amount
of tooth tissue would have to be removed, increasing the risk of
para-perforation and root fracture. In addition, preoperative CBCT
revealed that the MB root had two canals, MB1 and MB2, which were
suspected to have fused into one canal at the apical segment.
Furthermore, the incidence of 2-into-1 canal when two canals are
present in the MB root of the maxillary first molar is ~60%
(9). Therefore, filling the apical
foramen of the MB root by establishing a bypass through MB2 was
planned before the operation, and was successfully implemented
(Fig. 3).
At 9 months after surgery, the periapical hypodense
areas surrounding the MB, DB and P roots markedly decreased, and
the periapical tissue had almost completely recovered at 27 months
after surgery.
The present report compared the postoperative
outcomes of removal and bypass techniques for the same tooth. The
bypass technique should therefore be considered a nonsurgical
treatment if the FIs in the root canal are difficult to remove or
if the post-removal risks become unacceptable.
Discussion
To the best of our knowledge, universal guidelines
for the management of root canals with FIs remain elusive. A
previous retrospective study suggested that the ability of a
physician to make a balanced decision by combining clinical
experience with the specific condition of the affected tooth is
important (7). During the
preoperative planning of the present case, the location of the FIs,
the anatomical characteristics of the root canals and the risk of
removal were considered. The final decision was made to remove the
FI in the middle of the DB canal and to treat the FI in the MB
canal by bypass. This allowed for the observation of differences in
the therapeutic outcomes between the removal technique and the
bypass technique. At 9 and 27 months of follow-up, the periapical
inflammation in both roots was markedly improved and the treated
tooth became asymptomatic. The results demonstrated that as long as
the root canal system was disinfected as much as possible, the
pathogens remaining on the FI surface of the root canal could be
effectively removed and the disinfected FIs would not cause
secondary infection of the root canal. When FIs are used as part of
the filling process, the root canal is tightly filled to prevent
the invasion of foreign pathogens and an ideal retreatment effect
can be achieved. Overall, as long as the infection in the root
canal is removed as much as possible and the root canal is tightly
filled, successful treatment can be performed. In the present case,
this was successfully achieved by using the bypass technique.
The removal of FIs has been considered the ideal
treatment after instrument separation (8). Widely accepted removal techniques
include the Endo Extractor system, the wire loop technique, the
Masserann kit and ultrasonication (10). In previous years, several reports
have proposed endodontic templates for guiding trephines (11), computer-assisted methods (12), modified hollow tube-based extractor
systems (13) and innovative
low-cost device techniques (14).
Previous studies have shown that the success rate of removal is
85.5% when the FI is visible under an oral microscope, but only
47.7% when the FI is not visible (7,15).
Among numerous file removal methods, ultrasonic techniques have
been consistently reported as safe and successful (16). In the present case, the visible FI
from the middle segment of the DB canal was successfully removed
using an ultrasonic device under the microscope. Ultrasonic
equipment has been used in endodontics since 1957 and has been
constantly improved. Current handpieces operating at 1-8 kHz have
been documented to improve the success rate of FI removal because
of their low shear stresses and fewer changes on the canal surface
(17).
In a series of cases reported by Hindlekar et
al (18), FIs were
successfully removed via the Acteon Satelec P5 Neutron, the same
device used for the present case. The unit tips of the device move
back and forth in a linear piston-like manner, rendering them
suitable for endodontic treatment (19). However, notably, the heat generated
by the friction between the ultrasonic tips and the root canal wall
may lead to instrument fatigue and secondary fracture of the
fragment. Therefore, ultrasonic tips at low-power levels cannot be
operated for prolonged periods (20). Hashem (21) previously demonstrated that water
should not be used to cool the ultrasonic tip to maintain a good
surgical field of view, and the power of the device should be set
to moderate and used intermittently (21).
Madarati et al (7) have suggested that five factors can
affect the efficacy of the bypass technique: i) Severity of the
tooth symptoms; ii) whether the tooth can establish a smooth bypass
to reach the apical stop; iii) whether the infectious tissue
surrounding the periapex of the affected tooth can be effectively
removed; iv) whether the bypass can be tightly filled; and v)
whether the periodontal infection can be effectively controlled if
the affected teeth have periodontal symptoms. In addition, the
treatment success rate of teeth with pulpitis is considerably
higher compared with that of teeth with periapical inflammation
(22). Although there was severe
periapical inflammation in the MB root of the affected tooth in the
present case, the inflammation was effectively controlled after the
establishment of a smooth bypass, removal of as much apical
infectious tissue as possible and tight filling of the apical stop.
The treatment effect on the affected tooth was obvious. The
periapical hypodense areas surrounding the MB root apex had
significantly diminished at 9 months after treatment, and almost
completely disappeared at 27 months after treatment. And by now,
the affected tooth has not experienced any discomfort.
Recently, with the upgrading of dental instruments
and the accumulation of research data, the type of FI and the
degree of canal curvature have also become important factors
affecting bypass therapy outcomes (23). It has been reported that the
success rate of bypassing RaCe is higher compared with that of K3
and Hero 642 rotary nickel-titanium files (23). By contrast, the success rate of the
bypass technique is improved for instruments that fractured in the
anterior part of the curved canal (23). In addition, compared with normal
root canals, the success rate of excessively curved canals is
markedly reduced (23).
Kalogeropoulos et al (24) suggested that preoperative CBCT
examination plays an important role in decision making prior to the
management of FI. In the present case, preoperative CBCT
examination revealed that the MB canal where the FI was located was
fused with the MB2 at the apical segment, justifying the bypass
technique instead of the removal technique on the basis of clinical
experience. For the effective removal of the smear layer and
infectious tissues in the root canal, Sinha et al (25) previously demonstrated that the use
of both EDTA and NaClO with the ultrasonic system appears to be the
most effective combination of flushing fluid. Liu et al
(26) reported that
laser-activated irrigation (LAI) and LAI combined with the
photon-induced photoacoustic streaming technique results in
increased vaporized bubble kinetics and superior cleaning efficacy
in the apical area, even in the presence of FIs. In addition, the
filling of bypass canals is one of the key factors for the success
of root canal therapy. Vadachkoria et al (27) demonstrated that thermoplastic
GuttaMaster and GuttaFusion show superior adhesion to the walls.
The heated gutta-percha has good fluidity and plasticity. The
vertical condensation technique used in the filling process can
fill the hot gutta-percha into all corners of the bypass canal,
achieving a satisfactory filling effect for some small curved
irregular gaps between the FI and the root canal wall. The cooled
gutta-percha and FIs then form a dense whole in the root canal that
is close to the root canal wall, achieving an ideal
three-dimensional root canal filling effect, tightly sealing the
root canal system and improving the success rate of root canal
treatment (28).
In conclusion, the present case suggested that the
bypass technique can be considered an alternative treatment if
removing FIs from root canals is considered too difficult and/or
risky. Clinicians should combine their clinical experience and the
specific FI conditions to make further decisions. However, there
are certain limitations to the present report. The results observed
in only one case are not sufficiently convincing and more samples
and data should be collected in follow-up research. In a follow-up
study, a total of 60 teeth that were removed during orthodontic
treatment will be selected and the nickel-titanium instruments in
the root apical segment will be broken. One group will be treated
by the removal technique, and the other group will be treated by
the bypass technique. The success rates of the two groups will be
recorded and the data will be statistically analysed. The results
will be used to further validate the current conclusions.
Acknowledgements
Not applicable.
Funding
Funding: The present study was supported by Natural Science
Foundation of Shaanxi Province (grant no. 022JM-447).
Availability of data and materials
The data generated in the present study may be
requested from the corresponding author.
Authors' contributions
AZ and RM performed the treatment. XJ collected
data, RC analyzed data and wrote the manuscript. EY and QZ made
contributions to the study's conception and design. AZ conceived
the study and provided financial support. AZ and RC confirm the
authenticity of all the raw data. All authors read and approved the
final manuscript.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
The patient involved in the present study provided
written informed consent for publication of their data and
images.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Wycoff RC and Berzins DW: An in vitro
comparison of torsional stress properties of three different rotary
nickel-titanium files with a similar cross-sectional design. J
Endod. 38:1118–1120. 2012.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Spili P, Parashos P and Messer HH: The
impact of instrument fracture on outcome of endodontic treatment. J
Endod. 31:845–850. 2005.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Khasnis SA, Kar PP, Kamal A and Patil JD:
Rotary science and its impact on instrument separation: A focused
review. J Conserv Dent. 21:116–124. 2018.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Parashos P and Messer HH: Rotary NiTi
instrument fracture and its consequences. J Endod. 32:1031–1043.
2006.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Plotino G, Costanzo A, Grande NM, Petrovic
R, Testarelli L and Gambarini G: Experimental evaluation on the
influence of autoclave sterilization on the cyclic fatigue of new
nickel-titanium rotary instruments. J Endod. 38:222–225.
2012.PubMed/NCBI View Article : Google Scholar
|
|
6
|
McGuigan MB, Louca C and Duncan HF:
Clinical decision-making after endodontic instrument fracture. Br
Dent J. 214:395–400. 2013.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Madarati AA, Hunter MJ and Dummer PM:
Management of intracanal separated instruments. J Endod.
39:569–581. 2013.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Tikhonova S, Booij L, D'Souza V, Crosara
KTB, Siqueira WL and Emami E: Investigating the association between
stress, saliva and dental caries: A scoping review. BMC Oral
Health. 18(41)2018.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Cleghorn BM, Christie WH and Dong CC: Root
and root canal morphology of the human permanent maxillary first
molar: A literature review. J Endod. 32:813–821. 2006.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Chhina H, Hans MK and Chander S:
Ultrasonics: A novel approach for retrieval of separated
instruments. J Clin Diagn Res. 9:ZD18–ZD20. 2015.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Bordone A, Ciaschetti M, Perez C and
Couvrechel C: Guided endodontics in the management of intracanal
separated instruments: A case report. J Contemp Dent Pract.
23:853–856. 2022.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Pradhan B, Gao Y, Gao Y, Guo T, Cao Y and
He J: Broken instrument removal from mandibular first molar with
conebeam computed tomography based pre-operative computer-assisted
simulation: A case report. JNMA J Nepal Med Assoc. 59:795–798.
2021.PubMed/NCBI View Article : Google Scholar
|
|
13
|
AlRahabi MK and Ghabbani HM: Removal of a
separated endodontic instrument by using the modified hollow
tube-based extractor system: A case report. SAGE Open Med Case Rep.
8(2050313X20907822)2020.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Monteiro JC, Kuga MC, Dantas AA,
Jordao-Basso KC, Keine KC, Ruchaya PJ, Faria G and Leonardo Rde T:
A method for retrieving endodontic or atypical nonendodontic
separated instruments from the root canal: A report of two cases. J
Contemp Dent Pract. 15:770–774. 2014.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Nevares G, Cunha RS, Zuolo ML and Bueno
CE: Success rates for removing or bypassing fractured instruments:
A prospective clinical study. J Endod. 38:442–444. 2012.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Fu M, Huang X, Zhang K and Hou B: Effects
of ultrasonic removal of fractured files from the middle third of
root canals on the resistance to vertical root fracture. J Endod.
45:1365–1370. 2019.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Lea SC, Walmsley AD, Lumley PJ and Landini
G: A new insight into the oscillation characteristics of endosonic
files used in dentistry. Phys Med Biol. 49:2095–2102.
2004.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Hindlekar A, Kaur G, Kashikar R and
Kotadia P: Retrieval of separated intracanal endodontic
instruments: A series of four case reports. Cureus.
15(e35694)2023.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Cuje J, Bargholz C and Hulsmann M: The
outcome of retained instrument removal in a specialist practice.
Int Endod J. 43:545–554. 2010.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Madarati AA, Qualtrough AJ and Watts DC:
Factors affecting temperature rise on the external root surface
during ultrasonic retrieval of intracanal separated files. J Endod.
34:1089–1092. 2008.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Hashem AA: Ultrasonic vibration:
Temperature rise on external root surface during broken instrument
removal. J Endod. 33:1070–1073. 2007.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Sjogren U, Figdor D, Persson S and
Sundqvist G: Influence of infection at the time of root filling on
the outcome of endodontic treatment of teeth with apical
periodontitis. Int Endod J. 30:297–306. 1997.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Arshadifar E, Shahabinejad H, Fereidooni
R, Shahravan A and Kamyabi H: Possibility of bypassing three
fractured rotary NiTi files and its correlation with the degree of
root canal curvature and location of the fractured file: An in
vitro study. Iran Endod J. 17:62–66. 2022.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Kalogeropoulos K, Xiropotamou A, Koletsi D
and Tzanetakis GN: The effect of cone-beam computed tomography
(CBCT) evaluation on treatment planning after endodontic instrument
fracture. Int J Environ Res Public Health. 19(4088)2022.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Sinha S, Barua AND, Rana KS, Singh K,
Kumar S and Saini R: Comparison of efficacy of various intracanal
irrigants with ultrasonic bypass system. J Pharm Bioallied Sci. 13
(Suppl 2):S1390–S1393. 2021.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Liu J, Watanabe S, Mochizuki S, Kouno A
and Okiji T: Comparison of vapor bubble kinetics and cleaning
efficacy of different root canal irrigation techniques in the
apical area beyond the fractured instrument. J Dent Sci.
18:1141–1147. 2023.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Vadachkoria O, Mamaladze M, Jalabadze N,
Chumburidze T and Vadachkoria D: Evaluation of three obturation
techniques in the apical part of root canal. Georgian Med News.
17-21:2019.PubMed/NCBI
|
|
28
|
Ho ES, Chang JW and Cheung GS: Quality of
root canal fillings using three gutta-percha obturation techniques.
Restor Dent Endod. 41:22–28. 2016.PubMed/NCBI View Article : Google Scholar
|